Rural Social Participation through Osekkai during the COVID-19 Pandemic
Highlights
- The traditional Japanese behavior of creating a helping culture, termed ‘Osekkai’, is associated with increased social participation in rural communities during the COVID-19 pandemic.
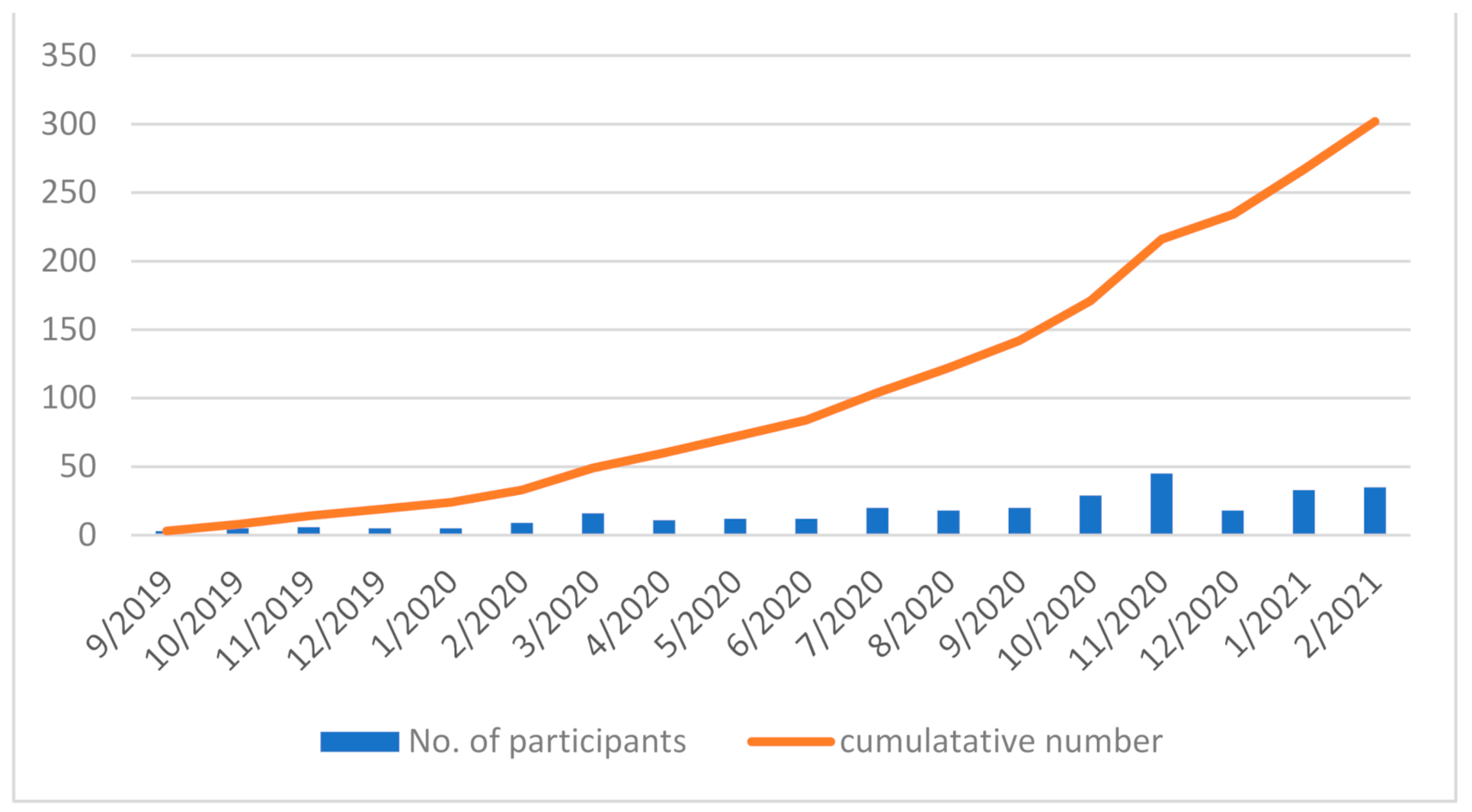
- During the COVID-19 pandemic, the number of participants involved in the activities regarding Osekkai has gradually increased.
- The participants have realized the positive effect that involvement in Osekkai has on their social participation.
- Involvement in Osekkai can improve social participation in rural communities.
- The continuity of the traditional activities with creating a helping culture can increase social participation.
- Rural traditional activities can lead to the sustainability of rural communities during the COVID-19 pandemic.
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Osekkai Conferences
2.3. Participants
2.4. Measurements
2.5. Analysis
2.6. Ethical Consideration
3. Results
3.1. Osekkai Conference Provisions
3.2. Demographics of the Participants
3.3. Relationship between Osekkai Participation and Social Participation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mehrabi, F.; Béland, F. Frailty as a Moderator of the Relationship between Social Isolation and Health Outcomes in Community-Dwelling Older Adults. Int. J. Environ. Res. Public Health 2021, 18, 1675. [Google Scholar] [CrossRef]
- Luo, Y.; Hawkley, L.C.; Waite, L.J.; Cacioppo, J.T. Loneliness, Health, and Mortality in Old Age: A National Longitudinal Study. Soc. Sci. Med. 2012, 74, 907–914. [Google Scholar] [CrossRef]
- Luanaigh, C.O.; Lawlor, B.A. Loneliness and the Health of Older People. Int. J. Geriatr. Psychiatry 2008, 23, 1213–1221. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Kitayuguchi, J.; Gomi, T.; Katsube, T. Challenges and Solutions in the Continuity of Home Care for Rural Older People: A Thematic Analysis. Home Health Care Serv. Q. 2020, 39, 126–139. [Google Scholar] [CrossRef]
- Pan, H. Social Capital and Life Satisfaction across Older Rural Chinese Groups: Does Age Matter? Soc. Work 2018, 63, 75–84. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Kitayuguchi, J.; Sano, C.; Könings, K.D. Educational Intervention to Improve Citizen’s Healthcare Participation Perception in Rural Japanese Communities: A Pilot Study. Int. J. Environ. Res. Public Health 2021, 18, 1782. [Google Scholar] [CrossRef]
- Grenade, L.; Boldy, D. Social Isolation and Loneliness among Older People: Issues and Future Challenges in Community and Residential Settings. Aust. Health Rev. 2008, 32, 468–478. [Google Scholar] [CrossRef]
- Yu, J.; Choe, K.; Kang, Y. Anxiety of Older Persons Living Alone in the Community. Healthcare 2020, 8, 287. [Google Scholar] [CrossRef]
- Herron, R.V.; Newall, N.E.G.; Lawrence, B.C.; Ramsey, D.; Waddell, C.M.; Dauphinais, J. Conversations in Times of Isolation: Exploring Rural-Dwelling Older Adults’ Experiences of Isolation and Loneliness during the COVID-19 Pandemic in Manitoba, Canada. Int. J. Environ. Res. Public Health 2021, 18, 3028. [Google Scholar] [CrossRef]
- Lo Coco, G.; Gentile, A.; Bosnar, K.; Milovanović, I.; Bianco, A.; Drid, P.; Pišot, S. A Cross-Country Examination on the Fear of COVID-19 and the Sense of Loneliness During the First Wave of COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2021, 18, 2586. [Google Scholar] [CrossRef]
- Banerjee, D.; Rai, M. Social Isolation in Covid-19: The Impact of Loneliness. Int. J. Soc. Psychiatry 2020, 66, 525–527. [Google Scholar] [CrossRef]
- Smith, B.J.; Lim, M.H. How the COVID-19 Pandemic Is Focusing Attention on Loneliness and Social Isolation. Public Health Res. Pract. 2020, 30, 3022008. [Google Scholar] [CrossRef]
- Segrin, C.; Domschke, T. Social Support, Loneliness, Recuperative Processes, and Their Direct and Indirect Effects on Health. Health Commun. 2011, 26, 221–232. [Google Scholar] [CrossRef]
- Victor, C.R.; Burholt, V.; Martin, W. Loneliness and Ethnic Minority Elders in Great Britain: An Exploratory Study. J. Cross Cult. Gerontol. 2012, 27, 65–78. [Google Scholar] [CrossRef]
- Wright-St Clair, V.A.; Neville, S.; Forsyth, V.; White, L.; Napier, S. Integrative Review of Older Adult Loneliness and Social Isolation in Aotearoa/New Zealand. Australas. J. Ageing 2017, 36, 114–123. [Google Scholar] [CrossRef]
- Ohta, R.; Yata, A. The Revitalization of ‘Osekkai’: How the COVID-19 Pandemic Has Emphasized the Importance of Japanese Voluntary Social Work. Qual. Soc. Work 2021, 20, 423–432. [Google Scholar] [CrossRef]
- Holt-Lunstad, J.; Smith, T.B.; Baker, M.; Harris, T.; Stephenson, D. Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Perspect. Psychol. Sci. 2015, 10, 227–237. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Cacioppo, S. The Growing Problem of Loneliness. Lancet 2018, 391, 426. [Google Scholar] [CrossRef]
- Harden, S.M.; Smith, M.L.; Ory, M.G.; Smith-Ray, R.L.; Estabrooks, P.A.; Glasgow, R.E. RE-AIM in Clinical, Community, and Corporate Settings: Perspectives, Strategies, and Recommendations to Enhance Public Health Impact. Front. Public Health 2018, 6, 71. [Google Scholar] [CrossRef]
- Ohta, R.; Ryu, Y.; Kataoka, D.; Sano, C. Effectiveness and Challenges in Local Self-Governance: Multifunctional Autonomy in Japan. Int. J. Environ. Res. Public Health 2021, 18, 574. [Google Scholar] [CrossRef]
- Ide, K.; Tsuji, T.; Kanamori, S.; Jeong, S.; Nagamine, Y.; Kondo, K. Social Participation and Functional Decline: A Comparative Study of Rural and Urban Older People, Using Japan Gerontological Evaluation Study Longitudinal Data. Int. J. Environ. Res. Public Health 2020, 17, 617. [Google Scholar] [CrossRef] [PubMed]
- Saito, T.; Cable, N.; Aida, J.; Shirai, K.; Saito, M.; Kondo, K. Validation Study on a Japanese Version of the Three-Item UCLA Loneliness Scale among Community-Dwelling Older Adults. Geriatr. Gerontol. Int. 2019, 19, 1068–1069. [Google Scholar] [CrossRef] [PubMed]
- Grande, S.W.; Faber, M.J.; Durand, M.A.; Thompson, R.; Elwyn, G. A Classification Model of Patient Engagement Methods and Assessment of Their Feasibility in Real-World Settings. Patient Educ. Couns. 2014, 95, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Mahase, E. Covid-19: What New Variants Are Emerging and How Are They Being Investigated? BMJ 2021, 372, n158. [Google Scholar] [CrossRef]
- Kreuter, M.W.; Lukwago, S.N.; Bucholtz, R.D.; Clark, E.M.; Sanders-Thompson, V. Achieving Cultural Appropriateness in Health Promotion Programs: Targeted and Tailored Approaches. Health Educ. Behav. 2003, 30, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Gregson, S.; Terceira, N.; Mushati, P.; Nyamukapa, C.; Campbell, C. Community Group Participation: Can It Help Young Women to Avoid HIV? An Exploratory Study of Social Capital and School Education in Rural Zimbabwe. Soc. Sci. Med. 2004, 58, 2119–2132. [Google Scholar] [CrossRef]
- Pronyk, P.M.; Harpham, T.; Busza, J.; Phetla, G.; Morison, L.A.; Hargreaves, J.R.; Kim, J.C.; Watts, C.H.; Porter, J.D. Can Social Capital Be Intentionally Generated? A Randomized Trial from Rural South Africa. Soc. Sci. Med. 2008, 67, 1559–1570. [Google Scholar] [CrossRef]
- Kamada, M.; Kitayuguchi, J.; Abe, T.; Taguri, M.; Inoue, S.; Ishikawa, Y.; Bauman, A.; Lee, I.M.; Miyachi, M.; Kawachi, I. Community-Wide Intervention and Population-Level Physical Activity: A 5-Year Cluster Randomized Trial. Int. J. Epidemiol. 2018, 47, 642–653. [Google Scholar] [CrossRef] [PubMed]
- Barcham, R.; Silas, E.; Irie, J. Health Promotion and Empowerment in Henganofi District, Papua New Guinea. Rural Remote Health 2016, 16, 3553. [Google Scholar] [CrossRef]
- Ocloo, J.; Matthews, R. From Tokenism to Empowerment: Progressing Patient and Public Involvement in Healthcare Improvement. BMJ Qual. Saf. 2016, 25, 626–632. [Google Scholar] [CrossRef]
- Brodsky, A.E.; Cattaneo, L.B. A Transconceptual Model of Empowerment and Resilience: Divergence, Convergence and Interactions in Kindred Community Concepts. Am. J. Commun. Psychol. 2013, 52, 333–346. [Google Scholar] [CrossRef] [PubMed]
- Masi, C.M.; Chen, H.Y.; Hawkley, L.C.; Cacioppo, J.T. A Meta-Analysis of Interventions to Reduce Loneliness. Pers. Soc. Psychol. Rev. 2011, 15, 219–266. [Google Scholar] [CrossRef] [PubMed]
- Andersson, L. Loneliness Research and Interventions: A Review of the Literature. Aging Ment. Health 1998, 2, 264–274. [Google Scholar] [CrossRef]
- Looi, M.K. Covid-19: Japan Ends State of Emergency but Warns of ‘new normal’. BMJ 2020, 369, m2100. [Google Scholar] [CrossRef]
- De Koning, J.; Richards, S.H.; Wood, G.E.R.; Stathi, A. Profiles of Loneliness and Social Isolation in Physically Active and Inactive Older Adults in Rural England. Int. J. Environ. Res. Public Health 2021, 18, 3971. [Google Scholar] [CrossRef]
- Bessaha, M.L.; Sabbath, E.L.; Morris, Z.; Malik, S.; Scheinfeld, L.; Saragossi, J. A Systematic Review of Loneliness Interventions among Non-Elderly Adults. Clin. Soc. Work J. 2020, 48, 110–125. [Google Scholar] [CrossRef]
- Jeste, D.V.; Lee, E.E.; Cacioppo, S. Battling the Modern Behavioral Epidemic of Loneliness: Suggestions for Research and Interventions. JAMA Psychiatry 2020, 77, 553–554. [Google Scholar] [CrossRef] [PubMed]
- Margalit, M.; Efrati, M. Loneliness, Coherence and Companionship among Children with Learning Disorders. Educ. Psychol. 1996, 16, 69–79. [Google Scholar] [CrossRef]
- Jia, F.; Soucie, K.; Matsuba, K.; Pratt, M.W. Meaning in Life Mediates the Association between Environmental Engagement and Loneliness. Int. J. Environ. Res. Public Health 2021, 18, 2897. [Google Scholar] [CrossRef]
- Pu, B.; Zhang, L.; Tang, Z.; Qiu, Y. The Relationship between Health Consciousness and Home-Based Exercise in China during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 5693. [Google Scholar] [CrossRef]
- Bermejo-Martins, E.; Luis, E.O.; Sarrionandia, A.; Martínez, M.; Garcés, M.S.; Oliveros, E.Y.; Cortés-Rivera, C.; Belintxon, M.; Fernández-Berrocal, P. Different Responses to Stress, Health Practices, and Self-Care during COVID-19 Lockdown: A Stratified Analysis. Int. J. Environ. Res. Public Health 2021, 18, 2253. [Google Scholar] [CrossRef] [PubMed]
| Participation in Osekkai | |||
|---|---|---|---|
| Factor | Exposure | Control | p-Value |
| N | 119 | 66 | |
| Age, men, mean (SD) | 44.34 (16.59) | 42.50 (19.75) | 0.5 |
| Sex (%) | |||
| Male | 76 (63.9) | 43 (65.2) | 0.874 |
| Female | 43 (36.1) | 23 (34.8) | |
| Education (%) | |||
| Low | 5 (4.2) | 1 (1.6) | 0.665 |
| High | 113 (95.8) | 60 (98.4) | |
| Socioeconomic status (%) | |||
| Low | 80 (67.2) | 50 (76.9) | 0.18 |
| High | 39 (32.8) | 15 (23.1) | |
| Habitual alcohol use (%) | 62 (52.5) | 28 (43.1) | 0.28 |
| Tobacco use (%) | 7 (6.0) | 4 (6.2) | 1 |
| Regular health check (%) | 73 (61.9) | 44 (68.8) | 0.419 |
| Living with family (%) | 93 (78.2) | 61 (93.8) | 0.006 |
| Living location (%) | |||
| Outside | 32 (27.1) | 14 (21.5) | 0.478 |
| Unnan City | 86 (72.9) | 51 (78.5) | |
| Social support (%) | |||
| High | 105 (89.0) | 56 (87.5) | 0.81 |
| Low | 13 (11.0) | 8 (12.5) | |
| Increasing frequency of meeting friends (%) | |||
| Yes | 64 (53.8) | 10 (15.2) | <0.001 |
| No | 55 (46.2) | 56 (84.8) | |
| Increasing timings of sharing joy (%) | |||
| Yes | 56 (47.1) | 7 (10.6) | <0.001 |
| No | 63 (52.9) | 59 (89.4) | |
| Frequency of Meeting | Number of Meetings | Loneliness | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Factor | AOR | 95% CI | p-Value | AOR | 95% CI | p-Value | AOR | 95% CI | p-Value |
| Osekkai | 3.64 | 1.67–7.93 | <0.001 | 2.05 | 1.01–4.17 | 0.048 | 0.76 | 0.37–1.55 | 0.44 |
| Age | 0.98 | 0.96–1.01 | 0.067 | 1.02 | 1.00–1.05 | 0.13 | 0.99 | 0.97–1.02 | 0.28 |
| Male | 0.73 | 0.34–1.56 | 0.42 | 0.61 | 0.30–1.26 | 0.18 | 1.2 | 0.58–2.50 | 0.62 |
| Higher education | 3.28 | 0.34–31.81 | 0.31 | 0.14 | 0.01–1.45 | 0.098 | 1.96 | 0.26–15.01 | 0.52 |
| High SES | 0.59 | 0.27–1.31 | 0.19 | 0.75 | 0.35–1.63 | 0.47 | 1.07 | 0.50–2.33 | 0.86 |
| Living with family | 1.48 | 0.59–3.68 | 0.4 | 0.88 | 0.35–2.23 | 0.79 | 0.42 | 0.16–1.08 | 0.07 |
| Residence | 1.11 | 0.49–2.54 | 0.81 | 0.52 | 0.23–1.19 | 0.12 | 0.86 | 0.38–1.98 | 0.72 |
| High SS | 1.88 | 0.57–6.16 | 0.3 | 0.57 | 0.18–1.87 | 0.35 | 17.2 | 1.98–150.01 | <0.001 |
| Habitual alcohol use | 1.31 | 0.65–2.66 | 0.45 | 0.63 | 0.32–1.26 | 0.19 | 0.93 | 0.47–1.85 | 0.83 |
| Health check | 1.7 | 0.79–3.70 | 0.18 | 0.41 | 0.19–0.88 | 0.021 | 1.49 | 0.70–3.16 | 0.3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ohta, R.; Yata, A.; Arakawa, Y.; Maiguma, K.; Sano, C. Rural Social Participation through Osekkai during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 5924. https://doi.org/10.3390/ijerph18115924
Ohta R, Yata A, Arakawa Y, Maiguma K, Sano C. Rural Social Participation through Osekkai during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(11):5924. https://doi.org/10.3390/ijerph18115924
Chicago/Turabian StyleOhta, Ryuichi, Akiko Yata, Yuki Arakawa, Koichi Maiguma, and Chiaki Sano. 2021. "Rural Social Participation through Osekkai during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 11: 5924. https://doi.org/10.3390/ijerph18115924
APA StyleOhta, R., Yata, A., Arakawa, Y., Maiguma, K., & Sano, C. (2021). Rural Social Participation through Osekkai during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(11), 5924. https://doi.org/10.3390/ijerph18115924







