Risk Perception of SARS-CoV-2 Infection and Implementation of Various Protective Measures by Dentists Across Various Countries
Abstract
1. Introduction
1.1. Modes of Transmission
1.2. Transmission Risk in Dental Offices
1.3. The Current Scenario during the Second Wave
2. Methods
2.1. Site and Settings
2.2. Questionnaire
2.3. Subjects
2.4. Bias
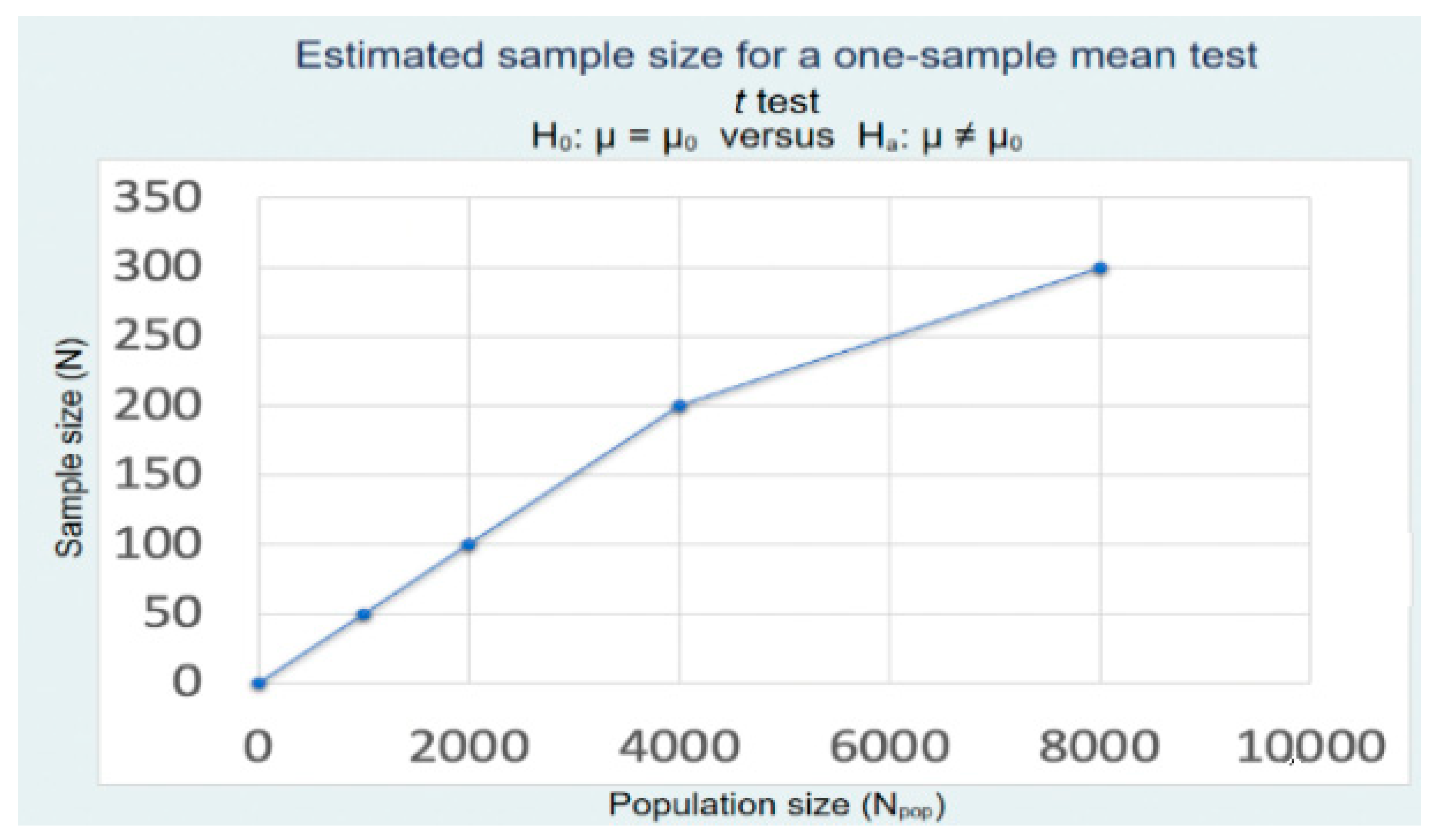
2.5. Statistics
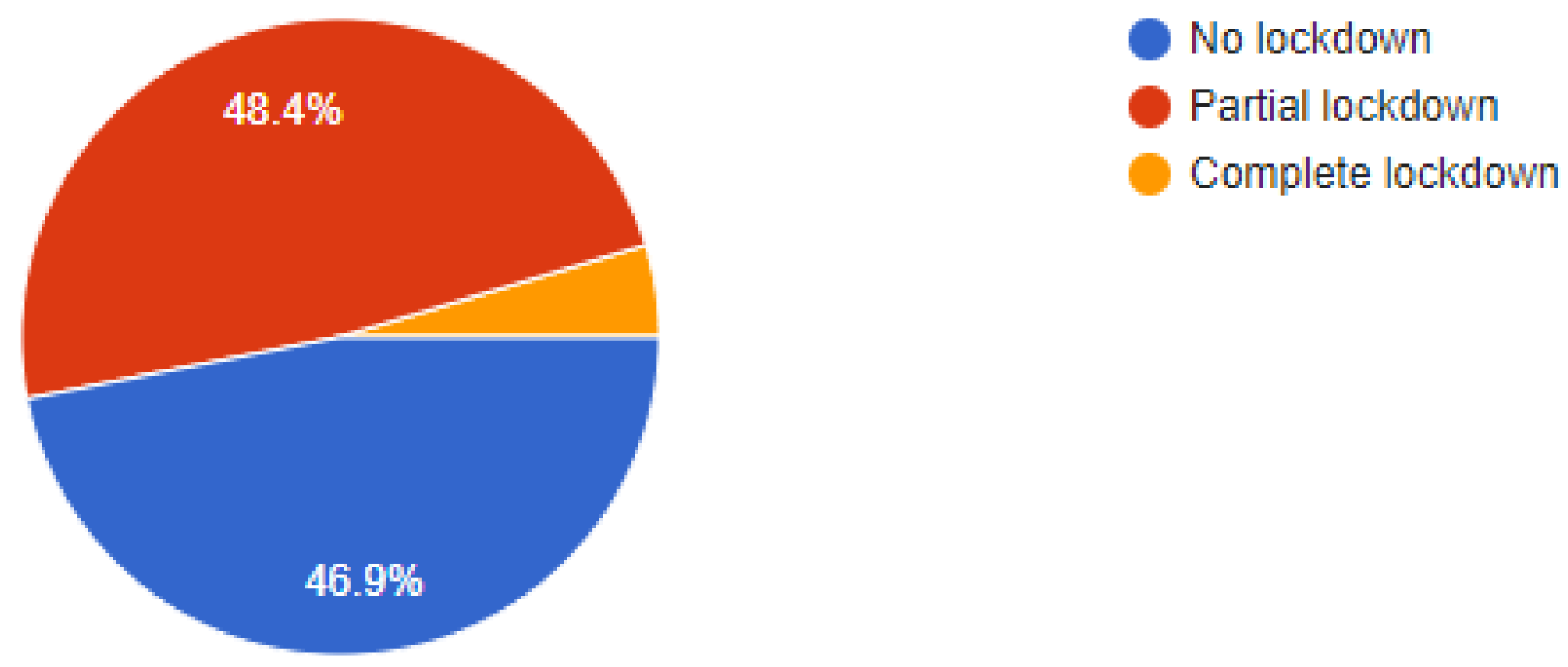
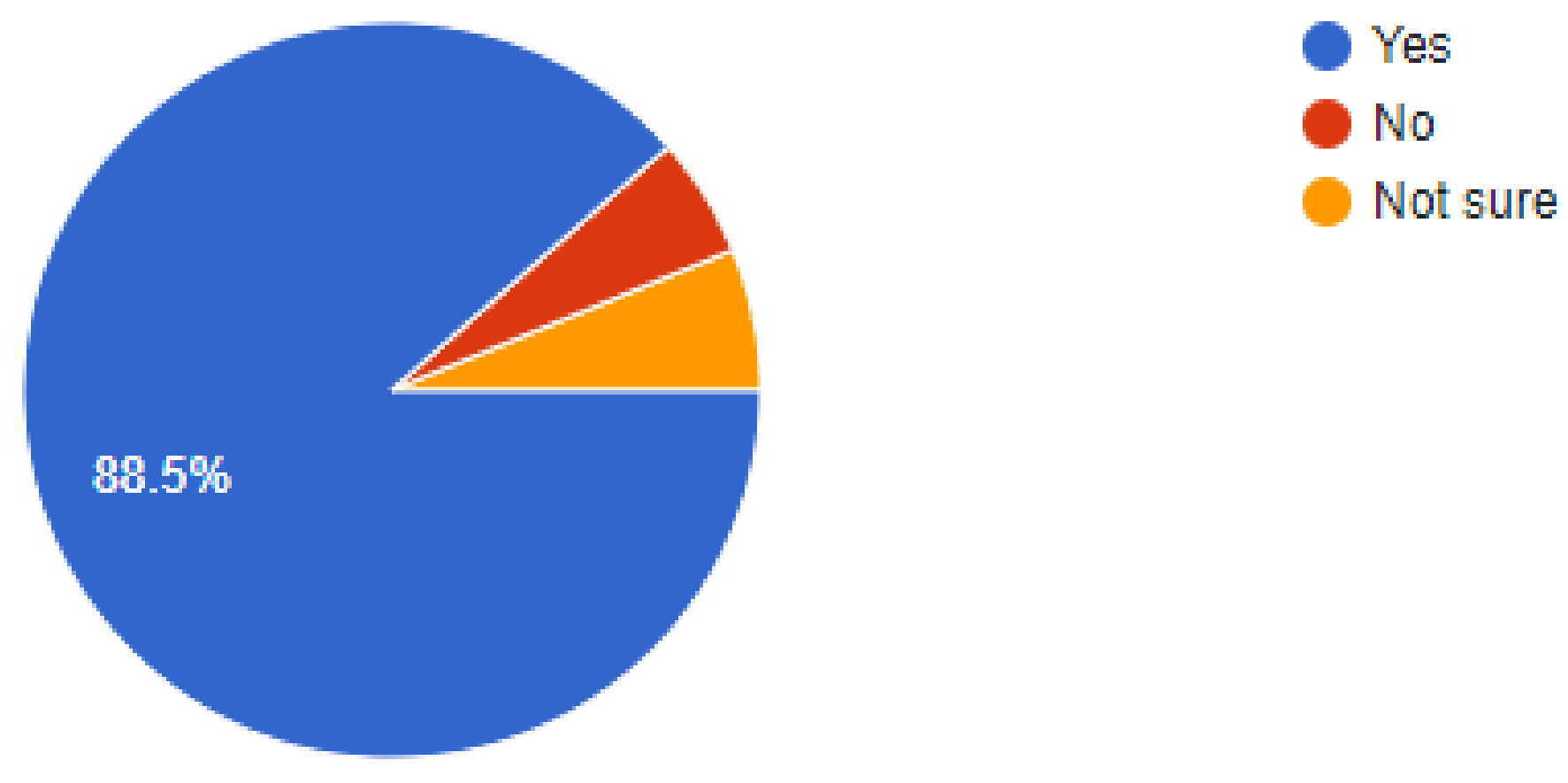
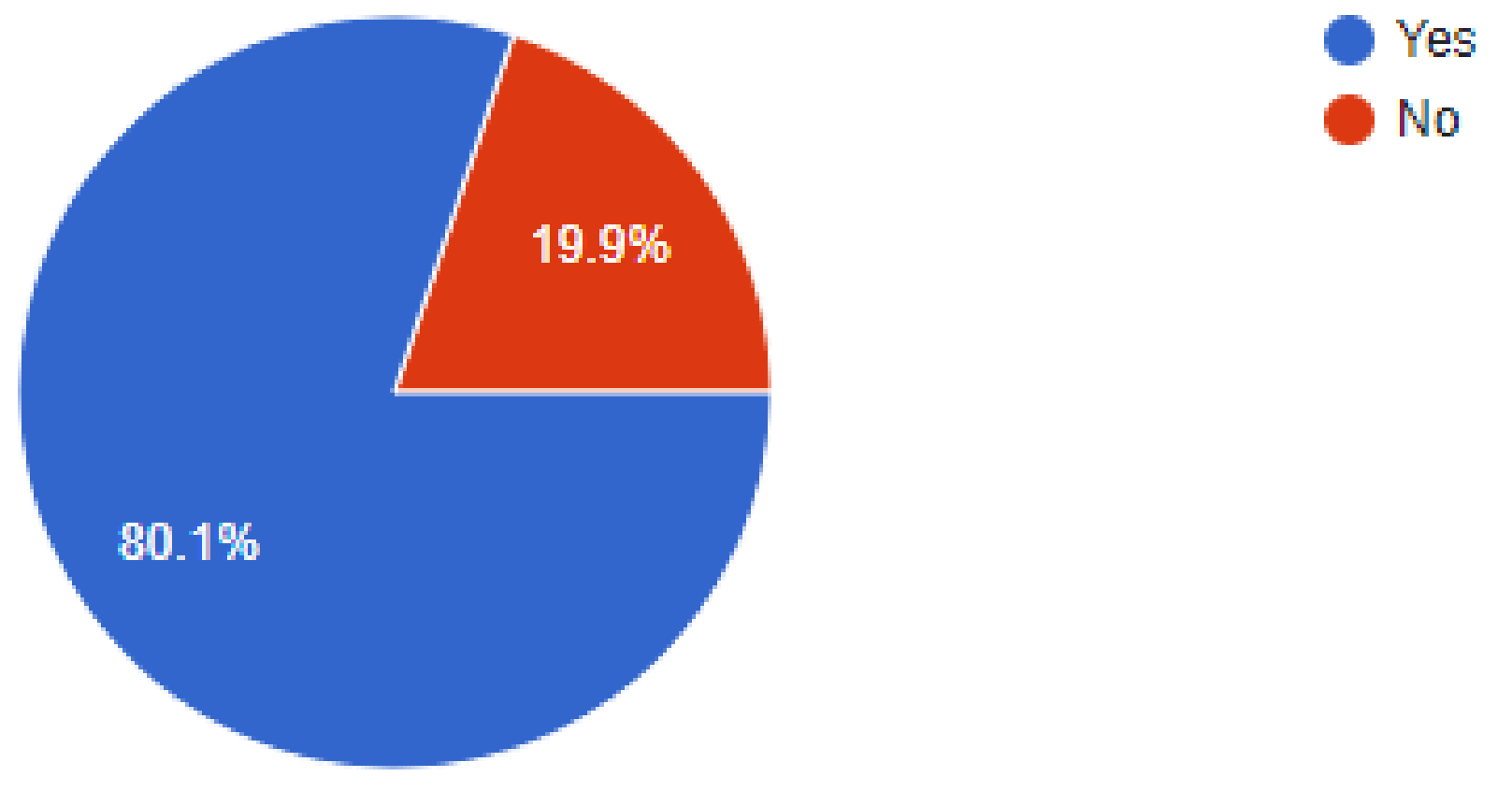
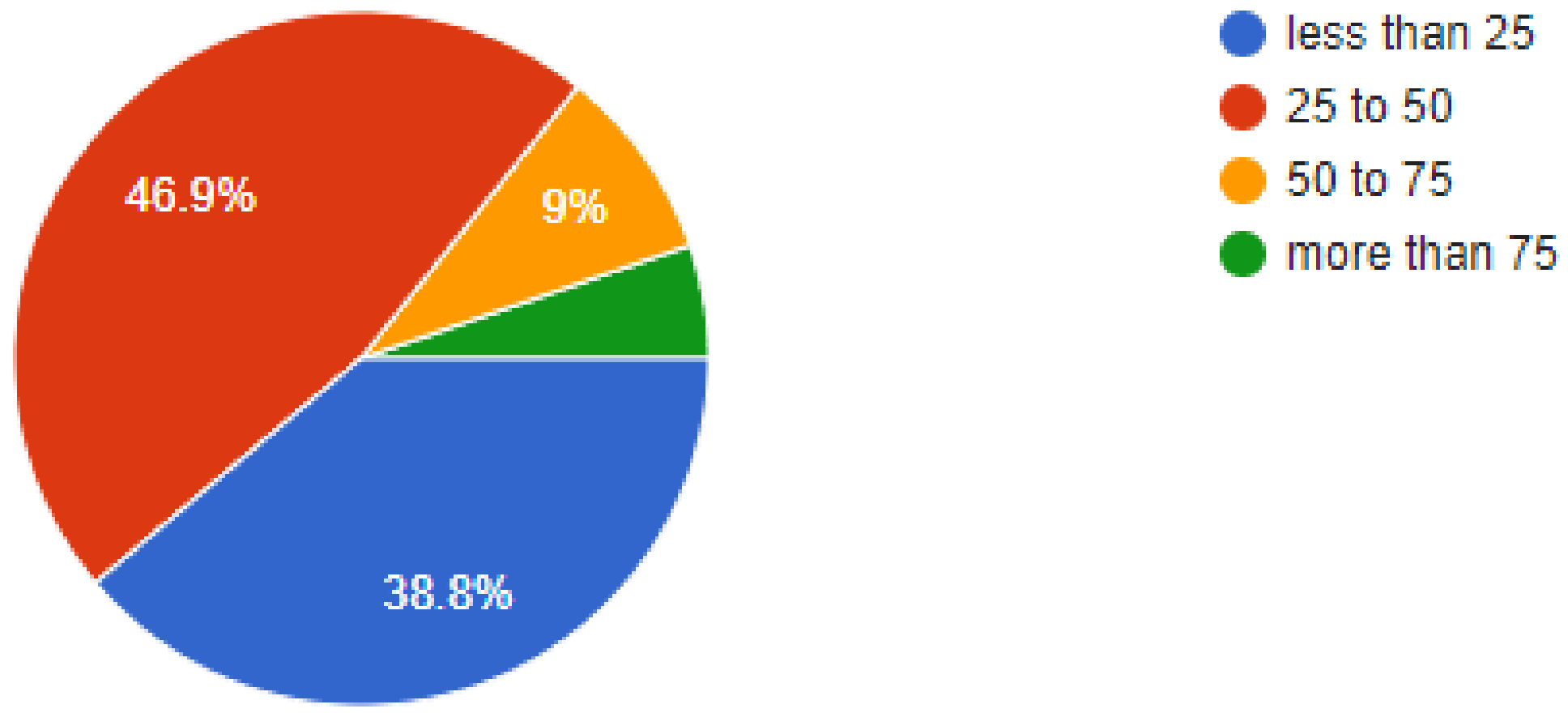
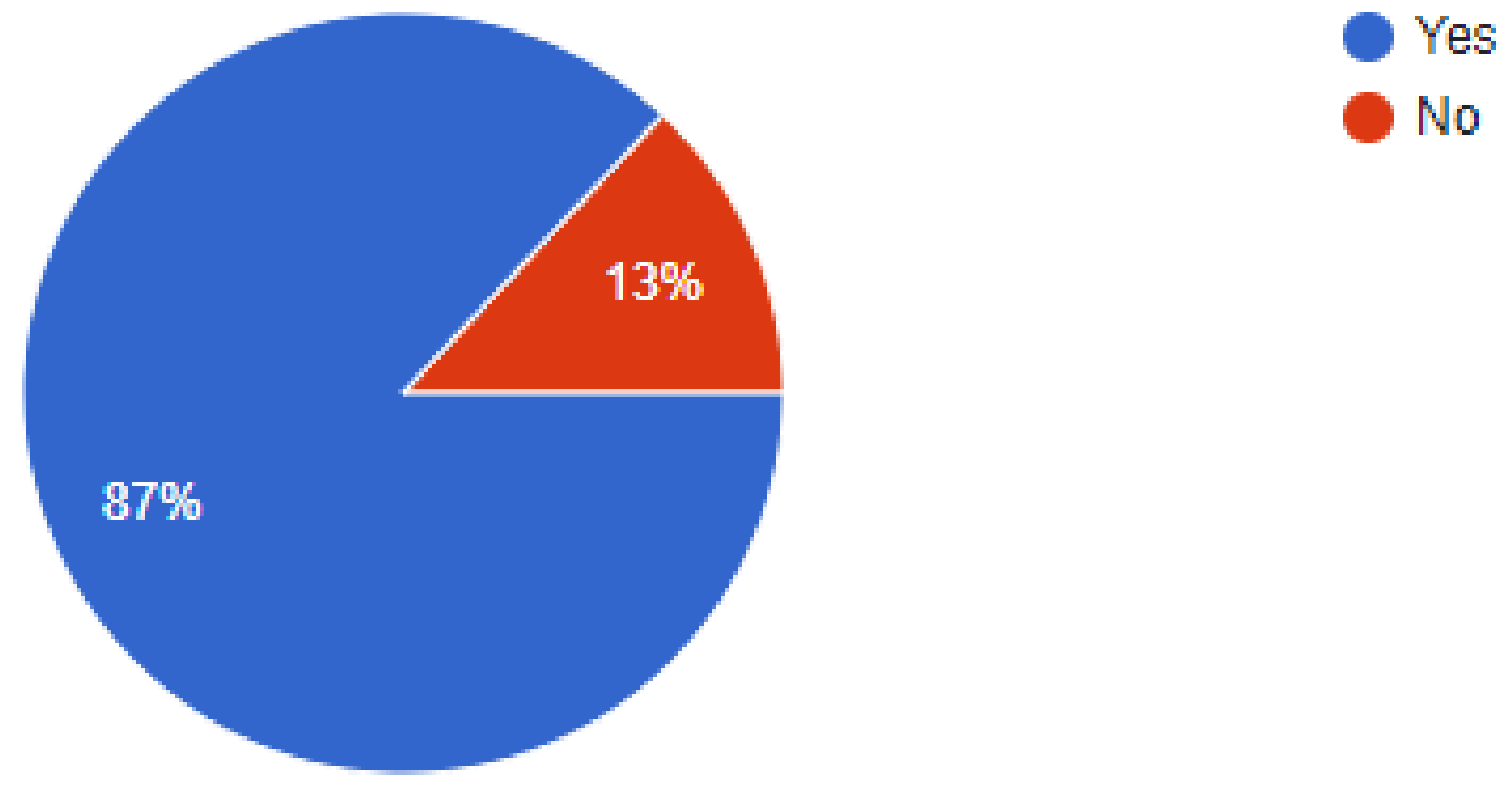
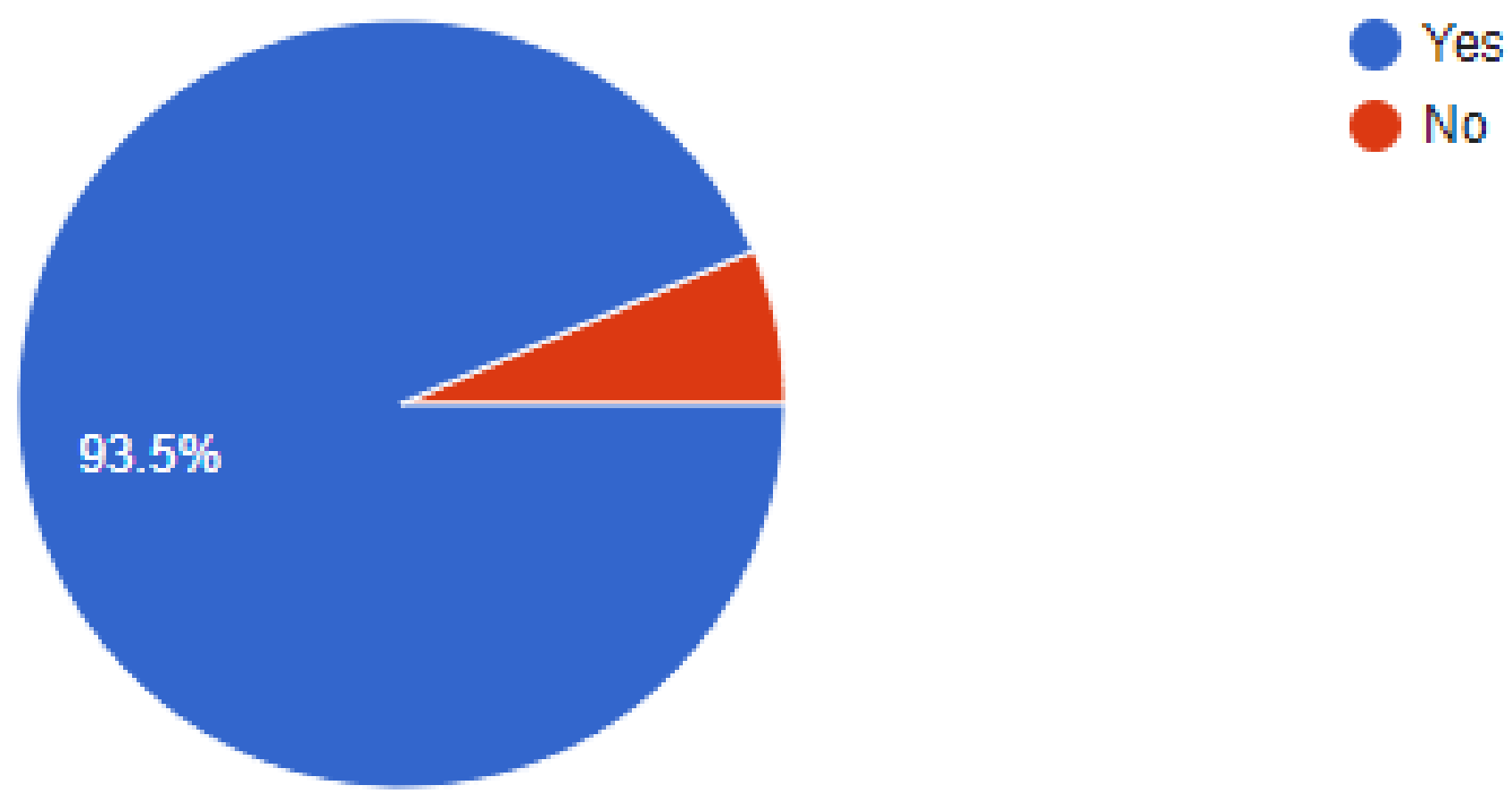
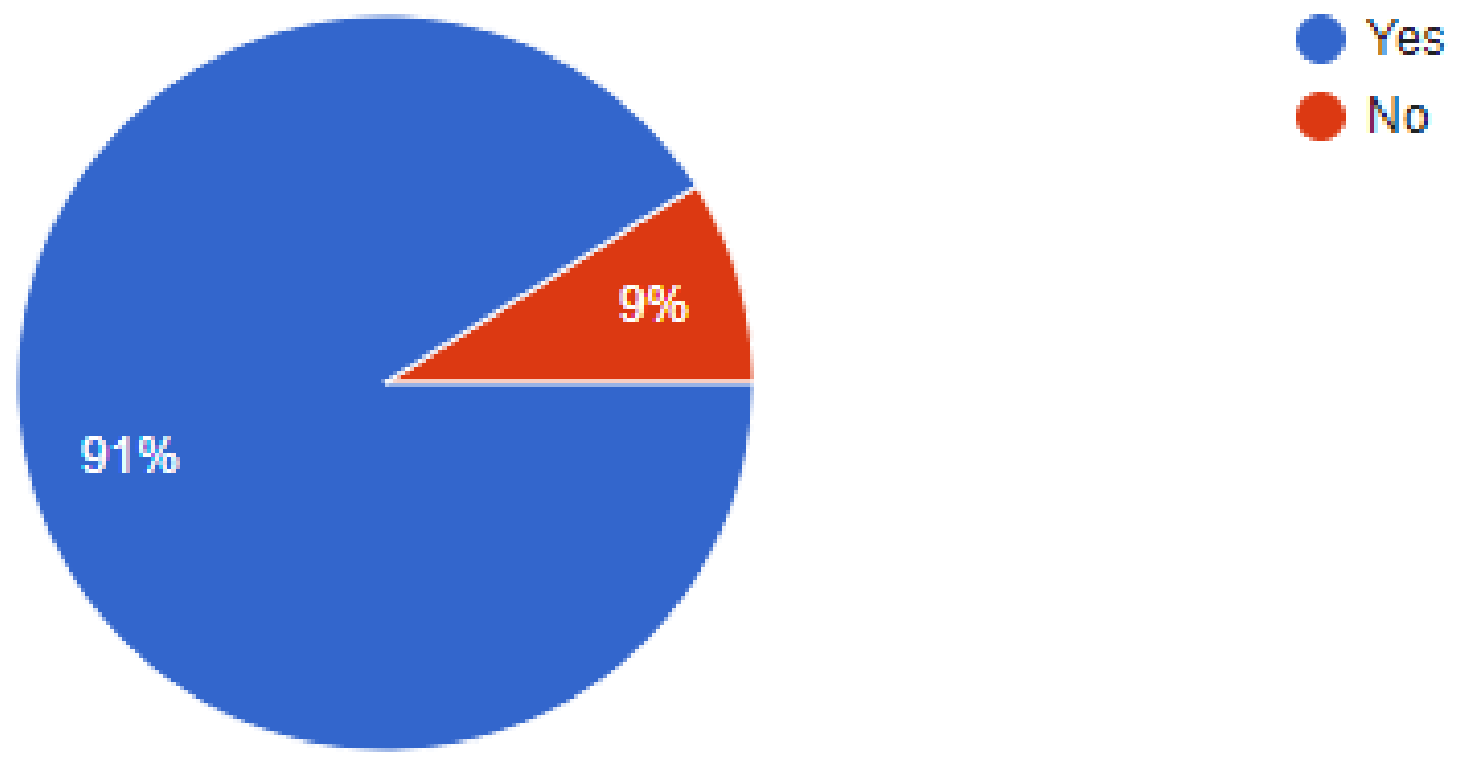
3. Results
4. Discussion
5. Conclusions
6. Limitations
7. Recommendations
- More efforts need to be directed at evidence-based clinical research to establish COVID-19 guidelines for each geographic location.
- The organization of educational programs for dentists to create more awareness about the infection risks in the clinics and preventive measures to adopt.
- Continuous evaluation of preventive measures to ensure that these are not adopted on a short-term basis and neglected thereafter.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Li, L.Q.; Huang, T.; Wang, Y.Q.; Wang, Z.P.; Liang, Y.; Huang, T.B.; Zhang, H.Y.; Sun, W.; Wang, Y. COVID-19 patients’ clinical characteristics, discharge rate, and fatality rate of meta-analysis. J. Med. Virol. 2020, 92, 577–583. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Naming the Coronavirus Disease (COVID-19) and the Virus that Causes It 2020. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019) (accessed on 11 February 2020).
- Izzetti, R.; Nisi, M.; Gabriele, M.; Graziani, F. COVID-19 Transmission in Dental Practice: Brief Review of Preventive Measures in Italy. J. Dent. Res. 2020, 99, 1030–1038. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. Scientific Brief 2020. Available online: https://www.who.int/publications-detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations (accessed on 29 March 2020).
- Bennett, A.M.; Fulford, M.R.; Walker, J.T.; Bradshaw, D.J.; Martin, M.V.; Marsh, P.D. Microbial aerosols in general dental practice. Br. Dent. J. 2000, 189, 664–677. [Google Scholar] [CrossRef]
- Ramesh, N.; Siddaiah, A.; Joseph, B. Tackling corona virus disease 2019 (COVID 19) in workplaces. Indian J. Occup. Environ. Med. 2020, 24, 16–18. [Google Scholar] [CrossRef]
- Dave, M.; Seoudi, N.; Coulthard, P. Urgent dental care for patients during the COVID-19 pandemic. Lancet 2020, 395, 1257. [Google Scholar] [CrossRef]
- O’Donnell, M.J.; Boyle, M.A.; Russell, R.J.; Coleman, D.C. Management of dental unit waterline biofilms in the 21st century. Future Microbiol. 2011, 6, 1209–1226. [Google Scholar] [CrossRef]
- Jain, M.; Mathur, A.; Mathur, A.; Mukhi, P.U.; Ahire, M.; Pingal, C. Qualitative and quantitative analysis of bacterial aerosols in dental clinical settings: Risk exposure towards dentist, auxiliary staff, and patients. J. Fam. Med. Prim. Care 2020, 9, 1003–1008. [Google Scholar] [CrossRef]
- James, R.; Mani, A. Dental aerosols: A silent hazard in dentistry. Int. J. Sci. Res. (Ahmedabad) 2016, 5, 1761–1763. [Google Scholar]
- Rothe, C.; Schunk, M.; Sothmann, P.; Bretzel, G.; Froeschl, G.; Wallrauch, C.; Zimmer, T.; Thiel, V.; Janke, C.; Guggemos, W.; et al. Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N. Engl. J. Med. 2020, 382, 970–971. [Google Scholar] [CrossRef]
- Prati, C.; Pelliccioni, G.; Sambri, V.; Chersoni, S.; Gandolfi, M.G. COVID-19: Its impact on dental schools in Italy, clinical problems in endodontic therapy and general considerations. Int. Endod. J. 2020, 53, 723–725. [Google Scholar] [CrossRef] [PubMed]
- Ammar, N.; Aly, N.M.; Folayan, M.O.; Mohebbi, S.Z.; Attia, S.; Howaldt, H.-P.; Boettger, S.; Khader, Y.; Maharani, D.A.; Rahardjo, A.; et al. Knowledge of dental academics about the COVID-19 pandemic: A multi-country online survey. BMC Med. Educ. 2020, 20, 399. [Google Scholar] [CrossRef] [PubMed]
- Gaffar, B.O.; El Tantawi, M.; Al-Ansari, A.A.; AlAgl, A.S.; Farooqi, F.A.; Almas, K.M. Knowledge and practices of dentists regarding MERS-CoV: A cross-sectional survey in Saudi Arabia. Saudi Med. J. 2019, 40, 714–720. [Google Scholar] [CrossRef]
- Callaway, E. Scores of coronavirus vaccines are in competition—How will scientists choose the best? Nature 2020. [Google Scholar] [CrossRef]
- Peditto, M.; Scapellato, S.; Marcianò, A.; Costa, P.; Oteri, G. Dentistry during the COVID-19 Epidemic: An Italian Workflow for the Management of Dental Practice. Int. J. Environ. Res. Public Health 2020, 17, 3325. [Google Scholar] [CrossRef] [PubMed]
- Peng, X.; Xu, X.; Li, Y.; Cheng, L.; Zhou, X.; Ren, B. Transmission routes of 2019-nCoV and controls in dental practice. Int. J. Oral Sci. 2020, 12, 9. [Google Scholar] [CrossRef] [PubMed]
- Nanda, K.D.; Nanda, J. Recommendations and management in dental practice during Corona Virus COVID-19. Open Dent. J. 2020, 14, 191–193. [Google Scholar] [CrossRef]
- Mateos Moreno, M.V.; Lenguas Silva, A.L.; Pastor Ramos, V.; García Ávila, I.; García Vázquez, M.T.; García Vicent, G.; Lamas Oliveira, M.; Rodríguez Alonso, E.; Tapias Perero, V.F.; Terán de Agustín, A.I.; et al. Odontología en entorno COVID-19. Adaptación de las Unidades de Salud Bucodental en los Centros de Salud de la Comunidad de Madrid. Rev. Esp. Salud Pública 2020, 94, e202011148. [Google Scholar] [PubMed]
- Terán, A.I.; Lenguas, A.L.; Pastor, V.; Lamas, M. Prevención de la COVID-19: Protección ocular. Recomendaciones para una actividad odontológica segura en la clínica dental. Maxillaris 2020, 245, 71–77. [Google Scholar]
- Liu, Y.; Ning, Z.; Chen, Y.; Guo, M.; Liu, Y.; Gali, N.K.; Sun, L.; Duan, Y.; Cai, J.; Westerdahl, D.; et al. Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature 2020, 582, 557–560. [Google Scholar] [CrossRef]
- Kujundzic, E.; Matalkah, F.; Howard, C.J.; Hernandez, M.; Miller, S.L. UV Air Cleaners and Upper-Room Air Ultraviolet Germicidal Irradiation for Controlling Airborne Bacteria and Fungal Spores. J. Occup. Environ. Hyg. 2006, 3, 536–546. [Google Scholar] [CrossRef]
- Reed, N.G. The History of Ultraviolet Germicidal Irradiation for Air Disinfection. Public Health Rep. 2010, 125, 15–27. [Google Scholar] [CrossRef] [PubMed]
- Liang, T. Handbook of COVID-19. Prevention and Treatment; School of Medicine, University of Zhejiang: Hangzhou, China, 2020. [Google Scholar]
- Ge, Z.; Yang, L.; Xia, J.; Fu, X.; Zhang, Y. Possible aerosol transmission of Covid-19 and special precautions in dentistry. J. Zhejiang Univ. Sci. 2020, 21, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Funkhouser, E.; Vellala, K.; Baltuck, C.; Cacciato, R.; Durand, E.; McEdward, D.; Sowell, E.; Theisen, S.E.; Gilbert, G.H. National Dental PBRN Collaborative Group. Survey methods to optimize response rate in the National Dental Practice-Based Research Network. Eval. Health Prof. 2017, 40, 332–358. [Google Scholar] [CrossRef] [PubMed]




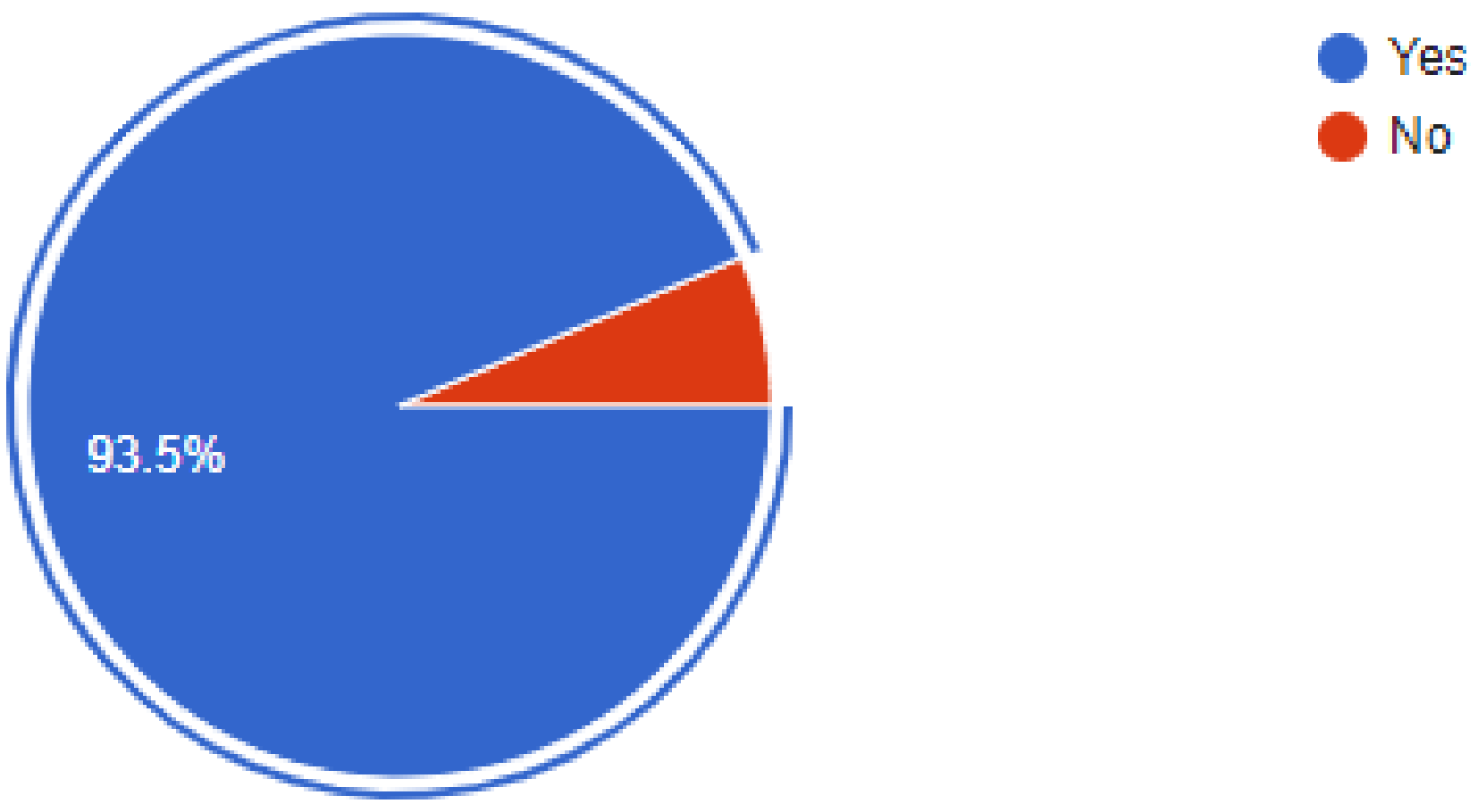
| Have You Added Any Measures for Disinfection? | None | Disposable | Autoclave | Total | One-Way ANOVA |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | ||
| Academician | 1 (1.8) | 32 (56.1) | 24 (42.1) | 57 (100.0) | 0.049 |
| General dentist | 5 (4.6) | 53 (49.1) | 50 (46.3) | 108 (100.0) | |
| Dental specialist | 2 (2.9) | 33 (48.5) | 33 (48.5) | 68 (100.0) |
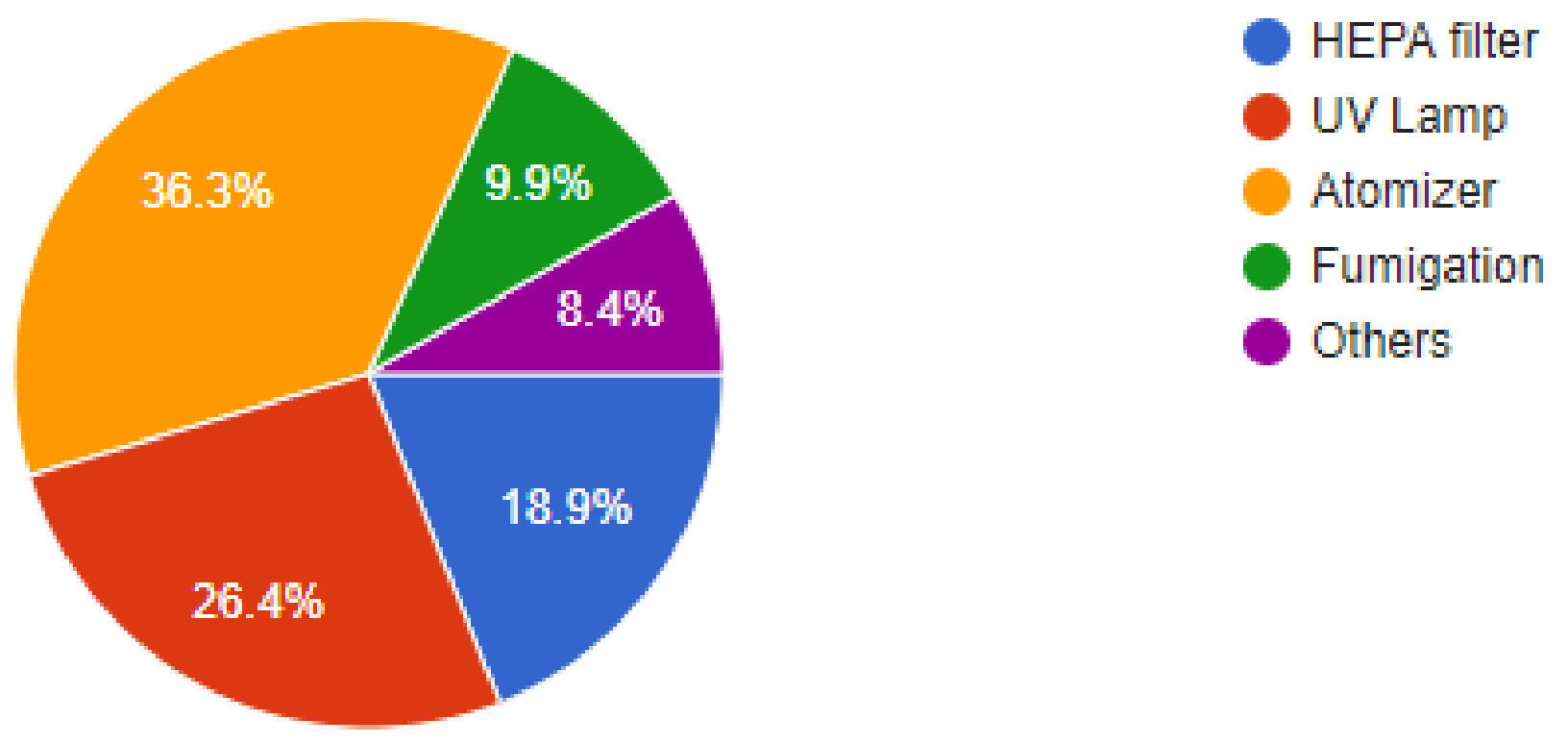
| Profession | HEPA Filter | UV Lamp | Atomizer | Fumigation | Total |
|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | |
| General dentist | 36 (25.4) b | 42 (29.6) a | 50 (35.2) b | 14 (9.9) b | 142 (100.0) |
| Dental specialist | 19 (21.8) b | 24 (27.6) a | 37 (37.9) b | 11 (12.6) b | 87 (100.0) |
| Academician | 6 (9.1) a | 19 (28.8) a | 34 (51.5) a | 7 (10.6) a | 66 (100) |
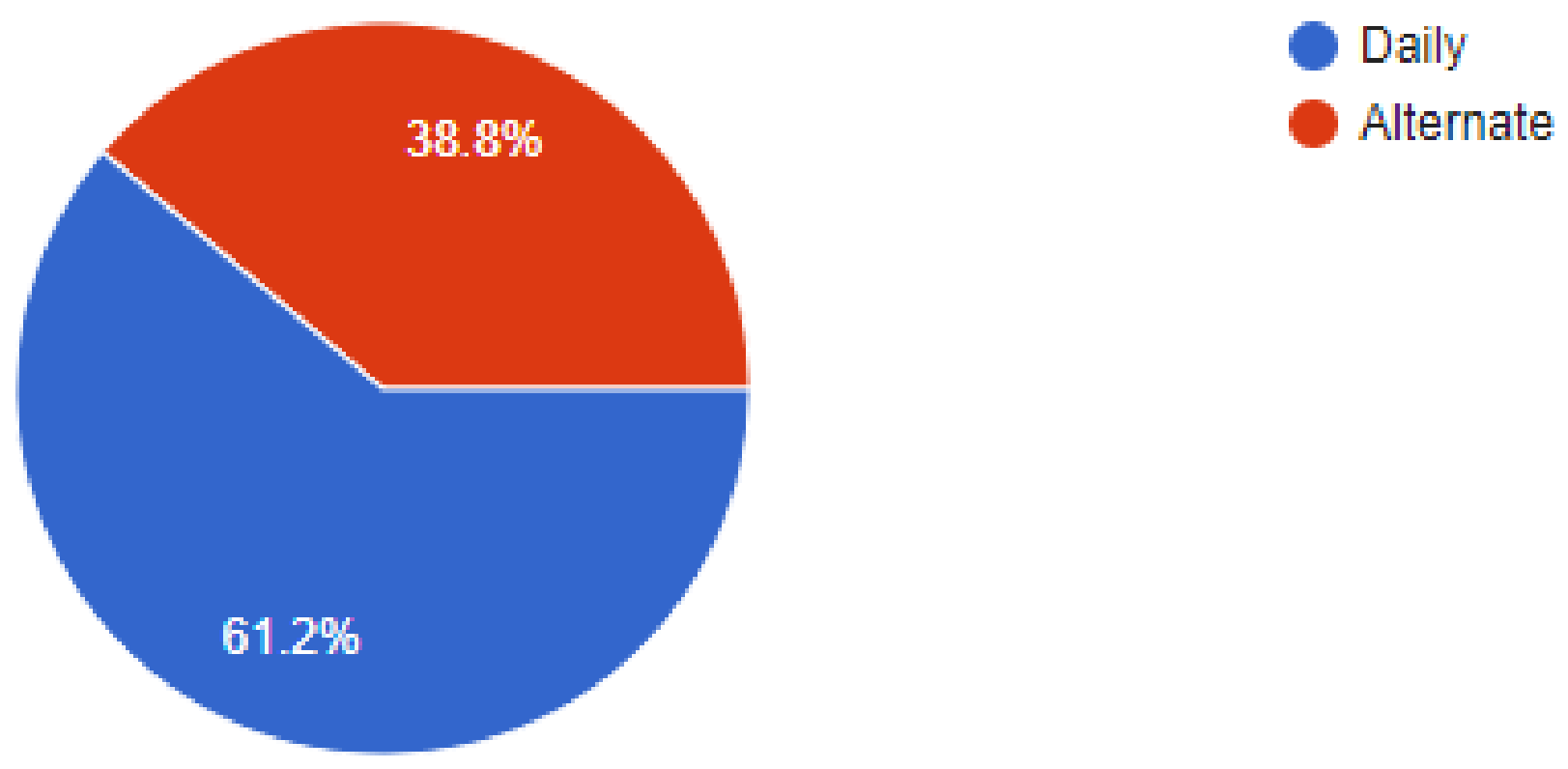
| 13. Have You Incorporated the 1-Meter Distance for Seating in Your Clinic? | Total | p-Value | ||||
|---|---|---|---|---|---|---|
| No | Yes | |||||
| 1. Location of Practice | Cambodia | n | 2 | 7 | 9 | 0.000 |
| % | 22.2% | 77.8% | 100.0% | |||
| India | n | 2 | 101 | 103 | ||
| % | 1.9% | 98.1% | 100.0% | |||
| Malaysia | n | 2 | 99 | 101 | ||
| % | 2.0% | 98.0% | 100.0% | |||
| Qatar | n | 12 | 25 | 37 | ||
| % | 32.4% | 67.6% | 100.0% | |||
| Saudi | n | 11 | 60 | 71 | ||
| % | 15.5% | 84.5% | 100.0% | |||
| Thailand | n | 0 | 1 | 1 | ||
| % | 0.0% | 100.0% | 100.0% | |||
| Italy | n | 0 | 50 | 50 | ||
| % | 0.0% | 100% | 100% | |||
| Total | n | 29 | 293 | 322 | ||
| % | 9.0% | 91.0% | 100.0% | |||
| Crosstab | p-Value | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| 14.Are You Using Any of the Following? | Total | ||||||||
| Atomizer | Fumigation | HEPA Filter | Others | UV Lamp | |||||
| 1. Location of Practice | Cambodia | n | 1 | 0 | 0 | 3 | 5 | 9 | 0.003 |
| % | 11.1% | 0.0% | 0.0% | 33.3% | 55.6% | 100.0% | |||
| India | n | 22 | 16 | 13 | 4 | 48 | 103 | ||
| % | 21.4% | 15.5% | 12.6% | 3.9% | 46.6% | 100.0% | |||
| Malaysia | n | 74 | 8 | 6 | 6 | 7 | 101 | ||
| % | 73.3% | 7.9% | 5.9% | 5.9% | 6.9% | 100.0% | |||
| Qatar | n | 5 | 0 | 22 | 2 | 8 | 37 | ||
| % | 13.5% | 0.0% | 59.5% | 5.4% | 21.6% | 100.0% | |||
| Saudi | n | 15 | 8 | 19 | 12 | 17 | 71 | ||
| % | 21.1% | 11.3% | 26.8% | 16.9% | 23.9% | 100.0% | |||
| Thailand | n | 0 | 0 | 1 | 0 | 0 | 1 | ||
| % | 0.0% | 0.0% | 100.0% | 0.0% | 0.0% | 100.0% | |||
| Italy | n | 5 | 0 | 20 | 15 | 10 | 50 | ||
| % | 10% | 0.0% | 40% | 30% | 20% | 100% | |||
| Total | n | 122 | 32 | 61 | 27 | 85 | 322 | ||
| % | 36.4% | 9.9% | 18.9% | 8.4% | 26.4% | 100.0% | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marya, A.; Karobari, M.I.; Selvaraj, S.; Adil, A.H.; Assiry, A.A.; Rabaan, A.A.; Horn, R.; Venugopal, A.; Messina, P.; Scardina, G.A. Risk Perception of SARS-CoV-2 Infection and Implementation of Various Protective Measures by Dentists Across Various Countries. Int. J. Environ. Res. Public Health 2021, 18, 5848. https://doi.org/10.3390/ijerph18115848
Marya A, Karobari MI, Selvaraj S, Adil AH, Assiry AA, Rabaan AA, Horn R, Venugopal A, Messina P, Scardina GA. Risk Perception of SARS-CoV-2 Infection and Implementation of Various Protective Measures by Dentists Across Various Countries. International Journal of Environmental Research and Public Health. 2021; 18(11):5848. https://doi.org/10.3390/ijerph18115848
Chicago/Turabian StyleMarya, Anand, Mohmed Isaqali Karobari, Siddharthan Selvaraj, Abdul Habeeb Adil, Ali A. Assiry, Ali A. Rabaan, Rithvitou Horn, Adith Venugopal, Pietro Messina, and Giuseppe Alessandro Scardina. 2021. "Risk Perception of SARS-CoV-2 Infection and Implementation of Various Protective Measures by Dentists Across Various Countries" International Journal of Environmental Research and Public Health 18, no. 11: 5848. https://doi.org/10.3390/ijerph18115848
APA StyleMarya, A., Karobari, M. I., Selvaraj, S., Adil, A. H., Assiry, A. A., Rabaan, A. A., Horn, R., Venugopal, A., Messina, P., & Scardina, G. A. (2021). Risk Perception of SARS-CoV-2 Infection and Implementation of Various Protective Measures by Dentists Across Various Countries. International Journal of Environmental Research and Public Health, 18(11), 5848. https://doi.org/10.3390/ijerph18115848










