An Agile Digital Platform to Support Population Health—A Case Study of a Digital Platform to Support Patients with Delirium Using IoT, NLP, and AI
Abstract
:1. Introduction
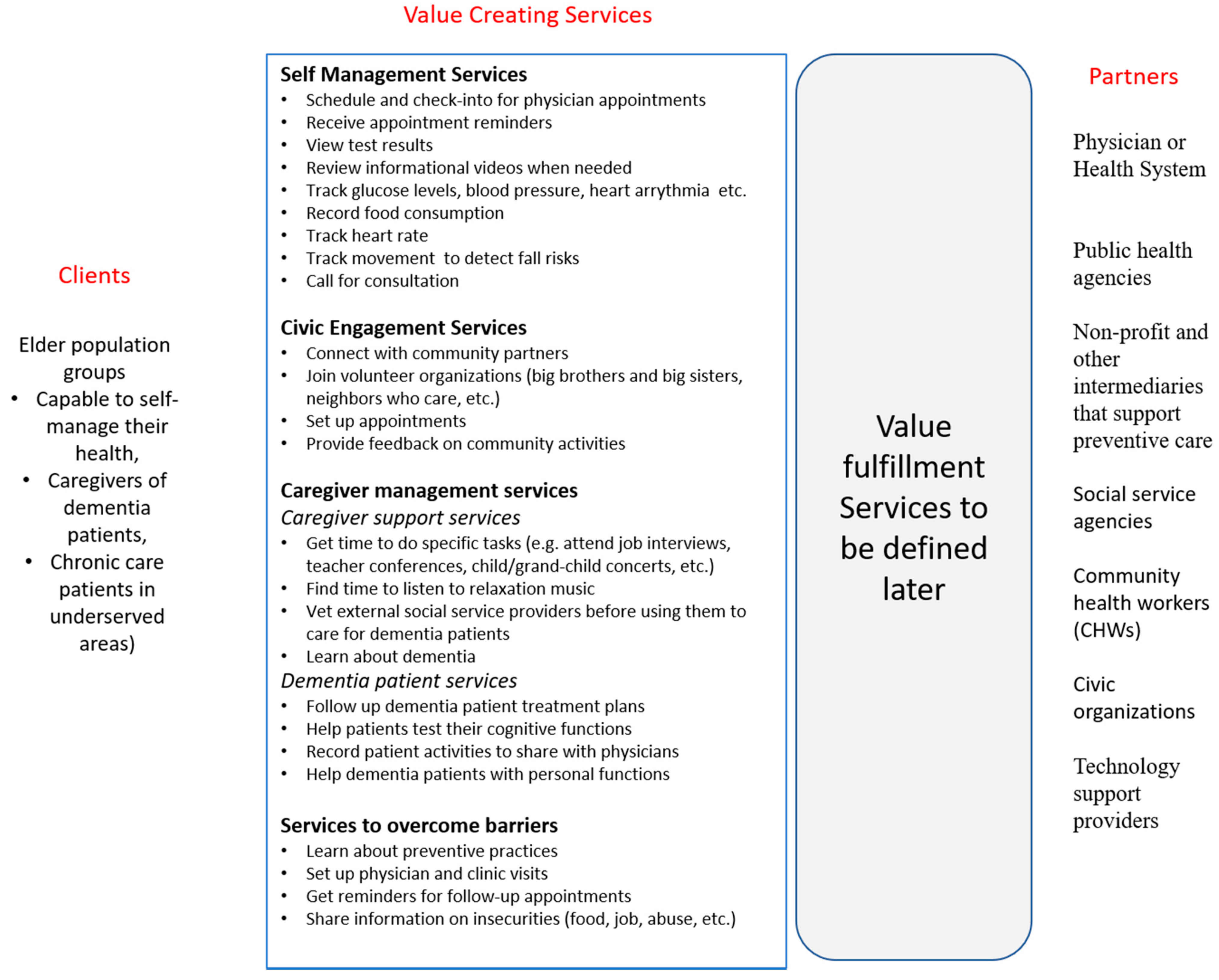
2. Research on Aging and Services to Create Value
2.1. Self-Health Management Services
2.2. Civic Engagement Services
2.3. Caregiver Engagement Services
2.4. Community Engagement Services
3. Designing a Digital Platform to Support Agility
3.1. Increase Value Cycle Frequency
3.2. Broaden the Scope of Value-in-Use Assessment
3.3. Broaden the Scale of Value-in-Use Assessment
3.4. Building an Agile Digital Platform
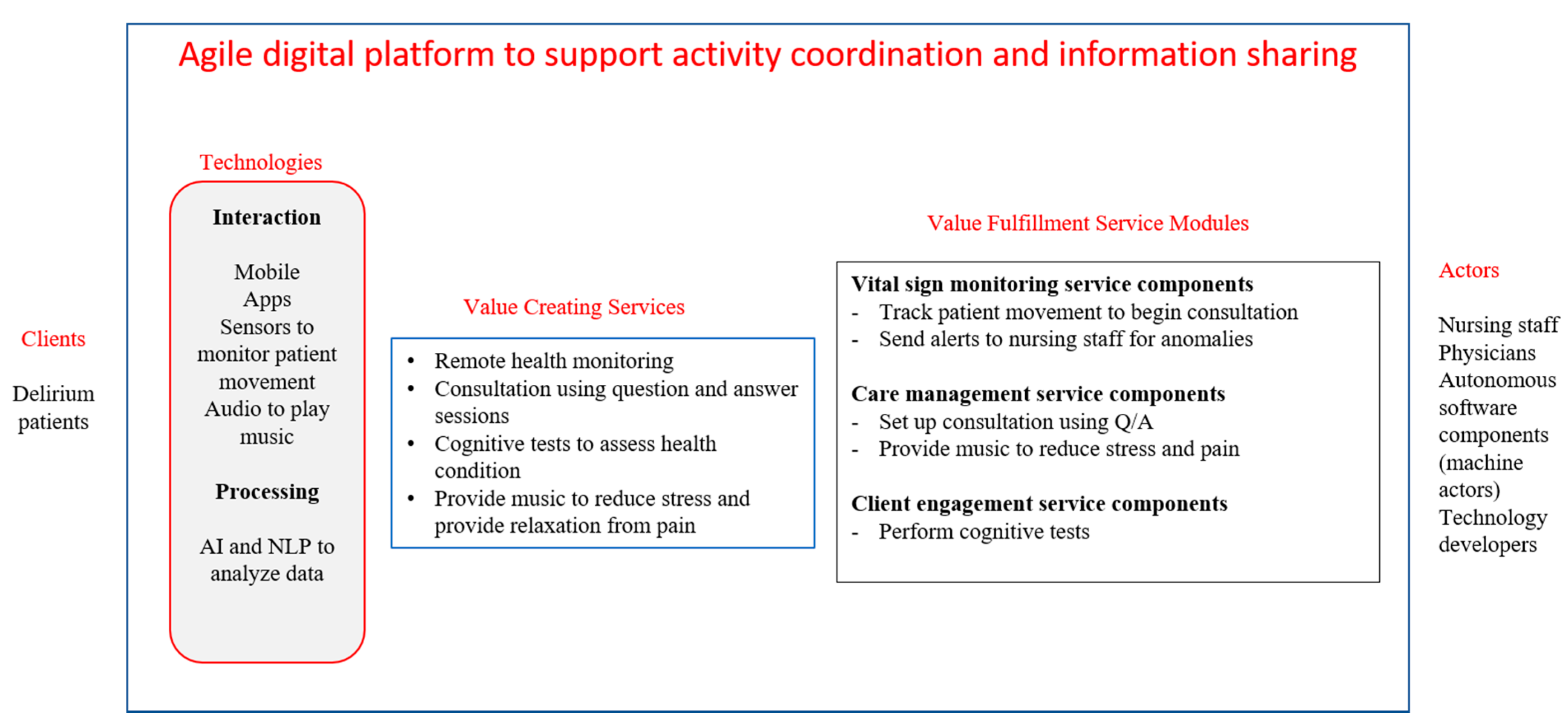
4. Digital Platform to Support Patients with Delirium
4.1. Clients
4.2. Technologies
4.3. Value Creating Services
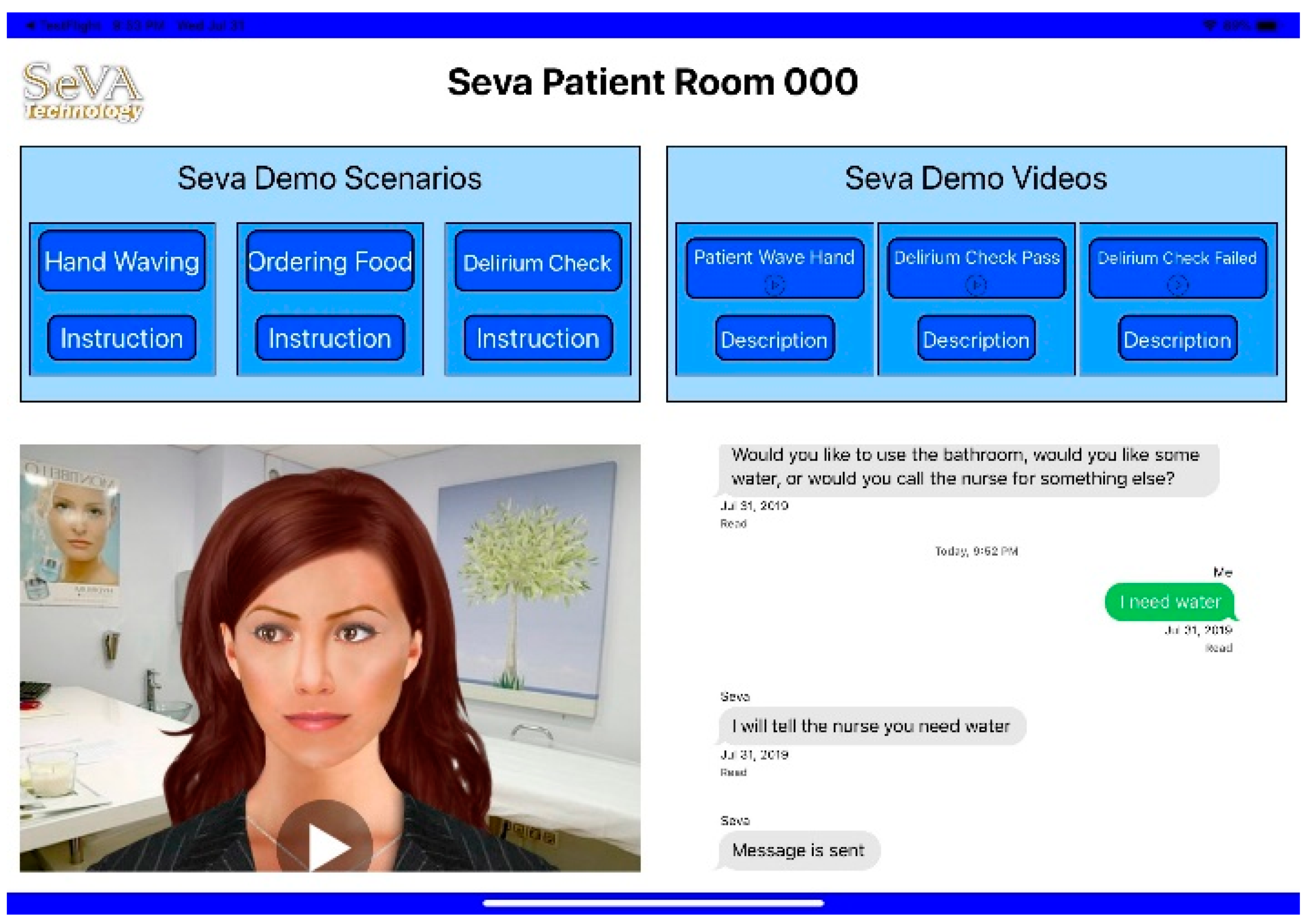
4.4. Value Fulfillment Service Modules
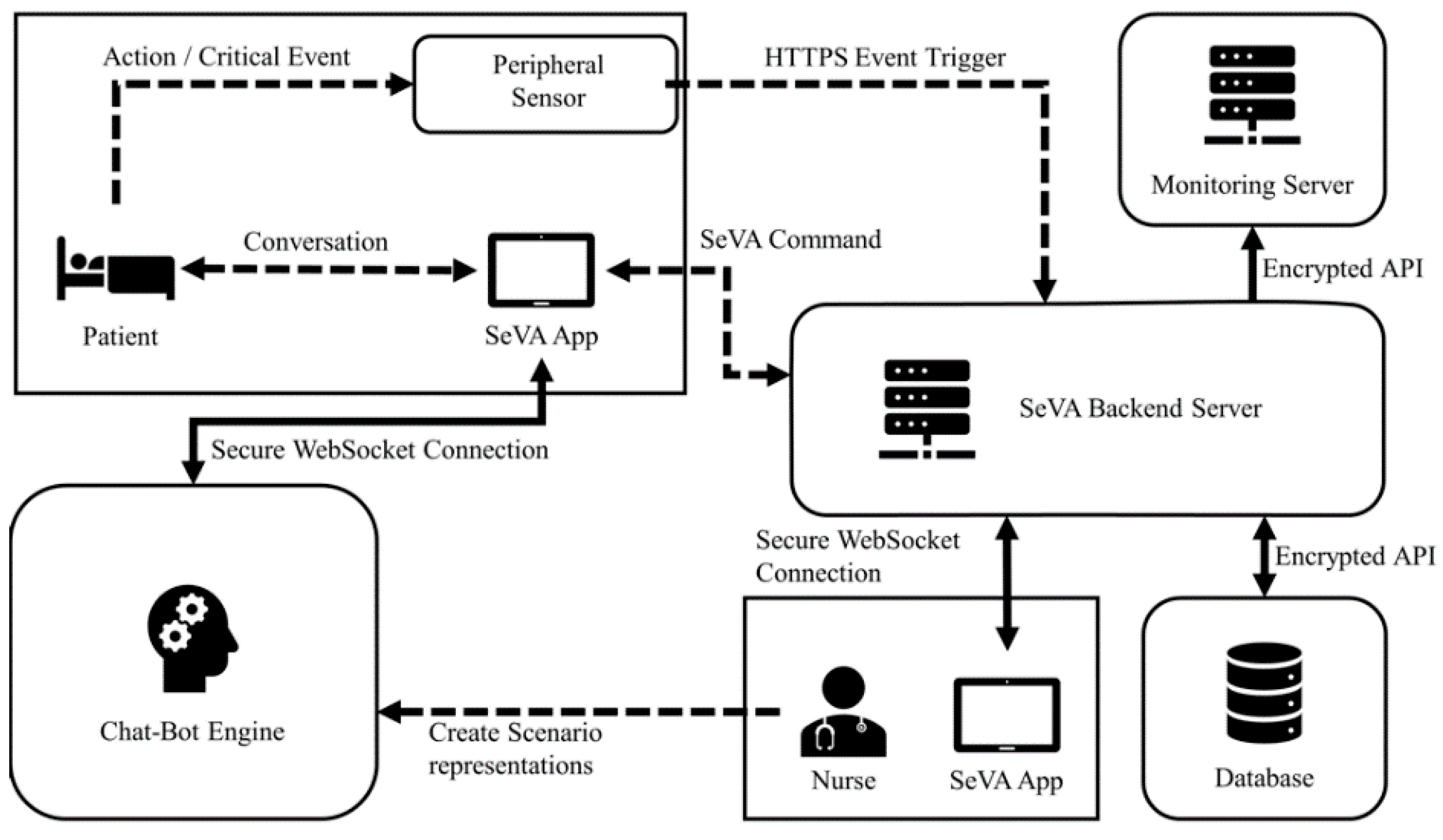
- A patient begins the scenario with an event, for example “waving hand.” When this patient request is received, the peripheral sensor recognizes the action and sends an hypertext transfer protocol secure (HTTPS) request to the SeVA backend server;
- The request is parsed to fetch the necessary information, such as the room number, from the database in order to trigger the chatbot engine to begin the conversation. The SeVA patient room application has a WebSocket connection with the chatbot engine so that the conversation can be executed;
- The conversation result is sent back to the SeVA backend server in the form of a SeVA command, and it is sent to the SeVA Master Control application in the nurse room;
- This leads to the nurse taking timely intervention if this is a critical event;
- The running status of the system is monitored continually by the monitoring server to ensure system reliability.
4.5. Agile Digital Platform to Support Activity Coordination among Actors
4.6. Agile Digital Platform to Support Information Sharing among Actors
5. Conclusions
6. Directions for Future Research
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
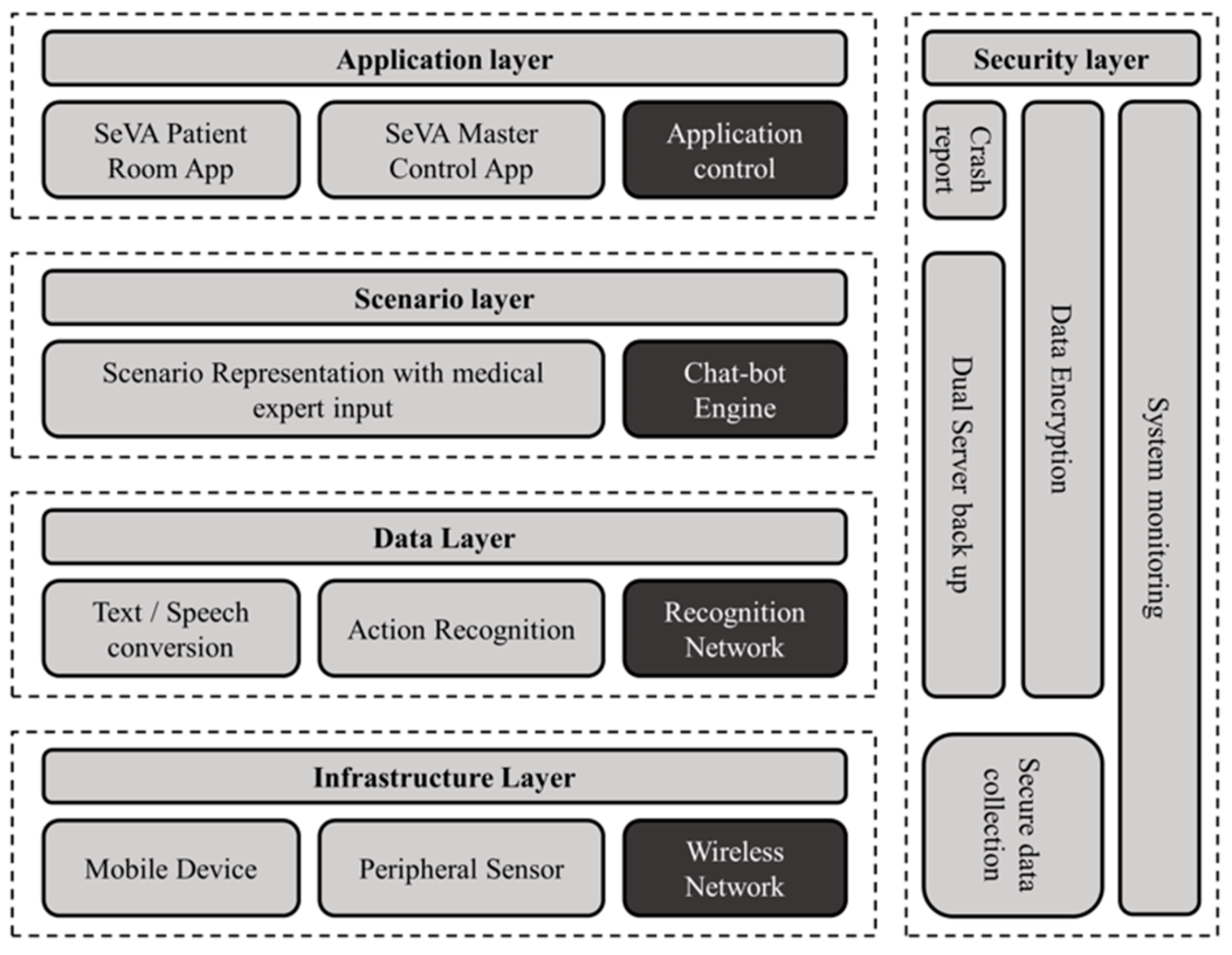
Appendix A
- The wireless network block works as a communication module for real-time data transmission;
- The mobile device, such as the tablet or cell phone, shows the user interface and conducts the conversation. The peripheral sensor collects patient movement data to infer the patient position status without infringing user privacy;
- The voice data and movement data will then be transferred to the upper layer.
References
- McKinsey Digital. Rethinking Customer Journeys with the Next-Generation Operating Model; McKinsey & Company: New York, NY, USA, 2018. [Google Scholar]
- Vargo, S.L.; Lusch, R.F. Why “service”? J. Acad. Mark. Sci. 2008, 36, 25–38. [Google Scholar] [CrossRef]
- Aghena, W.; De Smet, A.; Weerda, K. Agility: It Rhymes with Stability. McKinsey Quarterly. 2015. Available online: https://www.mckinsey.com/business-functions/organization/our-insights/agility-it-rhymes-with-stability (accessed on 1 December 2015).
- Saini, V.; Tanniru, M.; Liang, T.P. E-relationship strategies in digital age using value lens. In Proceedings of the 2020 International Conference on Service Science and Innovation, Hsinchu, Taiwan, 15–17 October 2020; p. 33. [Google Scholar]
- Bharadwaj, A.; El Sawy, O.A.; Pavlou, P.A.; Venkatraman, N. Digital business strategy: Toward a next generation of insights. MIS Q. 2013, 37, 471–482. [Google Scholar] [CrossRef]
- Trattner, A.; Hvam, L.; Forza, C.; Herbert-Hansen, Z.N.L. Product complexity and operational performance: A systematic literature review. CIRP J. Manuf. Sci. Technol. 2019, 25, 69–83. [Google Scholar] [CrossRef]
- Rodr´ Iguez, P.; Haghighatkhah, A.; Lwakatare, L.E.; Teppola, S.; Suomalainen, T.; Eskeli, J.; Karvonen, T.; Kuvaja, P.; Verner, J.M.; Oivo, M. Continuous deployment of software intensive products and services: A systematic mapping study. J. Syst. Softw. 2017, 123, 263–291. [Google Scholar] [CrossRef] [Green Version]
- Tanniru, M.; Khuntia, J.; Weiner, J. Hospital leadership in support of digital transformation. Pac. Asia J. Assoc. Inf. Syst. 2018, 10, 3. [Google Scholar] [CrossRef] [Green Version]
- Xu, B.; Xu, L.D.; Cai, H.; Xie, C.; Hu, J.; Bu, F. Ubiquitous data accessing method in IoT-Based information system for emergency medical services. IEEE Trans. Ind. Inform. 2014, 10, 1578–1586. [Google Scholar]
- Masoro, E.J. Are age-associated diseases an integral part of aging? In Handbook of the Biology of Aging; Masoro, E.J., Austad, S.N., Eds.; Academic Press: New York, NY, USA, 2006. [Google Scholar]
- Levy, B. Stereotype embodiment: A psychosocial approach to aging. Curr. Dir. Psychol. Sci. 2009, 18, 332–336. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- WHO World Health Organization. Active Ageing: A Policy Framework; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Doremus, B.L. The four R’s: Social diagnosis in health care. Health Soc. Work 1976, 1, 120–139. [Google Scholar] [CrossRef]
- Jarzabek, S.; Cheong, K.; Lim, Y.W.; Wong, J.C.M.; Kayanoth, R.K.; Teng, J.Y. CBT assistant platform: Web/mobile co-design solution for cognitive behavioral therapy. J. Hosp. Manag. Health Policy 2018, 2, 34. [Google Scholar] [CrossRef]
- Sendler, D.J. Combining standard psychiatric care with e-health follow up solutions—A viewpoint on making psychiatric care cost-effective for millions of patients and professionally satisfactory for providers. J. Hosp. Manag. Health Policy 2018, 2, 40. [Google Scholar] [CrossRef]
- Chiauzzi, E.; Rodarte, C.; DasMahapatra, P. Patient-centered activity monitoring in the self-management of chronic health conditions. BMC Med. 2015, 13, 77. [Google Scholar] [CrossRef] [Green Version]
- Khuntia, J.; Yim, D.; Tanniru, M.R.; Lim, S. Patient empowerment and engagement with a health infomediary. In Health Policy Technology; Elsevier: New York, NY, USA, 2017; Volume 6, pp. 40–50. [Google Scholar]
- Mulders, O.J. Employers’ age-related norms, stereotypes and ageist preferences in employment. Int. J. Manpow. 2019, 41, 523–534. [Google Scholar] [CrossRef] [Green Version]
- Serrat, R.; Warburton, J.; Petriwskyj, A.; Villar, F. Political participation and social exclusion in later life: What politically active seniors can teach us about barriers to inclusion and retention. Int. J. Ageing Later Life 2018, 12, 53–88. [Google Scholar] [CrossRef]
- Gagliardi, C.; Pillemer, K.; Gambella, E.; Piccinini, F.; Fabbietti, P. Benefits for older people engaged in environmental volunteering and socializing activities in city parks: Preliminary results of a program in Italy. Int. J. Environ. Res. Public Health 2020, 17, 3772. [Google Scholar] [CrossRef]
- WHO. Healthy Settings: Healthy Cities; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- WHO. Urban Green Spaces: A Brief for Action; WHO Regional Office for Europe: Copenhagen, Danmark, 2017. [Google Scholar]
- WHO. Physical Activity Strategy for the WHO European Region 2016–2025; WHO Regional Office for Europe: Copenhagen, Danmark, 2016. [Google Scholar]
- Foster, L.; Walker, A. Active and successful aging: A European policy perspective. Gerontologist 2015, 55, 83–90. [Google Scholar] [CrossRef]
- Serrat, R.; Scharf, T.; Villar, F.; Gómez, C. Fifty-five years of research into older people’s civic participation: Recent trends, future directions. Gerontologist 2020, 60, e38–e51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Principi, A.; Jensen, P.H.; Lamura, G. (Eds.) Active Ageing: Voluntary Work by Older People in Europe; The Policy Press: Bristol, UK, 2014. [Google Scholar]
- Walker, A. A strategy for active ageing. Int. Soc. Secur. Rev. 2002, 55, 121–139. [Google Scholar] [CrossRef]
- Darley, S. Learning as a process of personal-social transformation: Volunteering activity in health and social care charities. Mind Cult. Act. 2018, 25, 199–215. [Google Scholar] [CrossRef] [Green Version]
- Van Ingen, E.; Wilson, J. I Volunteer, Therefore I am? Factors Affecting Volunteer Role Identity. Nonprofit Volunt. Sect. Q. 2016, 46. [Google Scholar] [CrossRef]
- OECD. SMEs, Entrepreneurship and Innovation, 2010; OECD Publishing: Paris, France, 2010; pp. 185–215. [Google Scholar]
- Peredo, A.M.; McLean, M. Social entrepreneurship: A critical review of the concept. J. World Bus. 2006, 41, 56–65. [Google Scholar] [CrossRef]
- Relationship-Based Home Care: A Sustainable Solution for Europe’s Elder Care Crisis; Global Coalition on Aging: New York, NY, USA, 2018; pp. 1–36.
- Bom, J.; Bakx, P.; Schut, F.; van Doorslaer, E. The impact of informal caregiving for older adults on the health of various types of caregivers: A systematic Review. Gerontologist 2019, 59, e629–e642. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, E.Y.Y.; Gobat, N.; Kim, J.H.; Newnham, E.A.; Huang, Z.; Hung, H.; Dubois, C.; Hung, K.K.C.; Lai, Y.; Wong, E.; et al. Informal home care providers: The forgotten health-care workers during the COVID-19 pandemic. Lancet 2020, 395, 1957–1959. [Google Scholar] [CrossRef]
- Williams, F.; Moghaddam, N.; Ramsden, S.; de Boos, D. Interventions for reducing levels of burden amongst informal carers of persons with dementia in the community. A systematic review and meta-analysis of randomized controlled trials. Aging Ment. Health 2019, 23, 1629–1642. [Google Scholar] [CrossRef] [PubMed]
- Phillips, D.; Paul, G.; Fahy, M.; Dowling-Hetherington, L.; Kroll, T.; Moloney, B.; Duffy, C.; Fealy, G.; Lafferty, A. The invisible workforce during the COVID-19 pandemic: Family carers at the frontline. Hrb. Open Res. 2020, 3, 24. [Google Scholar] [CrossRef] [PubMed]
- Tur-Sinai, A.; Teti, A.; Rommel, A.; Hlebec, V.; Lamura, G. How many older informal caregivers are there in Europe? Comparison of estimates of their prevalence from three european surveys. Int. J. Environ. Res. Public Health 2020, 17, 9531. [Google Scholar] [CrossRef] [PubMed]
- Bryant, J.; Mansfield, E.; Boyes, A.W.; Waller, A.; Sanson-Fisher, R.; Regan, T. Involvement of informal caregivers in supporting patients with COPD: A review of intervention studies. Int. J. Chronic Obstr. Pulm. Dis. 2016, 11, 1587–1596. [Google Scholar] [CrossRef] [Green Version]
- Fiest, K.M.; McIntosh, C.J.; Demiantschuk, D.; Leigh, J.P.; Stelfox, H.T. Translating evidence to patient care through caregivers: A systematic review of caregiver-mediated interventions. BMC Med. 2018, 16, 105. [Google Scholar] [CrossRef]
- Kaschowitz, J.; Brandt, M. Health effects of informal caregiving across Europe: A longitudinal approach. Soc. Sci. Med. 2017, 173, 72–80. [Google Scholar] [CrossRef]
- Litwin, H.; Stoeckel, K.J.; Roll, A. Relationship status and depressive symptoms among older co-resident caregivers. Aging Ment. Health 2014, 18, 225–231. [Google Scholar] [CrossRef]
- Pinquart, M.; Sörensen, S. Spouses, adult children, and children-in-law as caregivers of older adults: A meta-analytic comparison. Psychol. Aging 2011, 26, 1–14. [Google Scholar] [CrossRef] [Green Version]
- Goll, J.C.; Charlesworth, G.; Scior, K.; Stott, J. Barriers to social participation among lonely older adults: The influence of social fears and identity. PLoS ONE 2015, 13, e0201510. [Google Scholar] [CrossRef] [Green Version]
- Biggs, S. Toward critical narrativity. Stories of aging in contemporary social policy. J. Aging Stud. 2011, 15, 303–316. [Google Scholar] [CrossRef]
- Plum, A.; Tanniru, M.; Khuntia, J. An Innovation Platform for Diffusing Public Health Practices across a Global Network; HICSS: Hawaii, HI, USA, 2019. [Google Scholar]
- Tanniru, M. Engagement leading to empowerment—Digital innovation strategies for patient care continuity. J. Hosp. Manag. Health Policy 2019, 3, 28. [Google Scholar] [CrossRef] [Green Version]
- HOPE. Available online: http://www.hopewarmingpontiac.org/ (accessed on 14 May 2021).
- Williams, D.R.; Costa, M.V.; Odunlami, A.O.; Mohammad, S.A. Moving upstream: How Interventions that address the social determinants of health can improve health and reduce disparities. J. Public Health Manag. Pract. 2008, 14, S8–S17. [Google Scholar] [CrossRef] [PubMed]
- Boccia, S.; Ricciardi, W.; Ioannidis, A.J.P. What other countries can learn from italy during the COVID-19 pandemic. JAMA Intern. Med. 2020, 180, 927–928. [Google Scholar] [CrossRef] [Green Version]
- Armitage, R.; Nellums, L.B. COVID-19 and the consequences of isolating the elderly. Lancet Public Health 2020, 5, e256. [Google Scholar] [CrossRef] [Green Version]
- Hwang, T.J.; Rabheru, K.; Peisah, C.; Reichman, W.; Ikeda, M. Loneliness and Social Isolation during the COVID-19 Pandemic. Int. Psychogeriatr. 2020, 32, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Rolandi, E.; Vaccaro, R.; Abbondanza, S.; Casanova, G.; Pettinato, L.; Colombo, M.; Guaita, A. Loneliness and social engagement in older adults based in lombardy during the COVID-19 lockdown: The long-term effects of a course on social networking sites use. Int. J. Environ. Res. Public Health 2020, 17, 7912. [Google Scholar] [CrossRef] [PubMed]
- Santini, Z.I.; Jose, P.E.; Cornwell, E.Y.; Koyanagi, A.; Nielsen, L.; Hinrichsen, C.; Meilstrup, C.; Madsen, K.R.; Koushede, V. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. Lancet Public Health 2020, 5, e62–e70. [Google Scholar] [CrossRef] [Green Version]
- Sala, E.; Gaia, A.; Cerati, G. The gray digital divide in social networking site use in Europe: Results from a quantitative study. Soc. Sci. Comput. Rev. 2020. [Google Scholar] [CrossRef]
- Yu, R.P.; Ellison, N.B.; McCammon, R.J.; Langa, K.M. Mapping the two levels of digital divide: Internet access and social network site adoption among older adults in the USA. Inf. Commun. Soc. 2016, 19, 1445–1464. [Google Scholar] [CrossRef]
- Meskó, B.Z.; Drobni, Z.; Bényei, E.; Gergely, B.; Győrffy, Z. Digital health is a cultural transformation of traditional healthcare. mHealth 2017, 3, 38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grant, R.W.; Wald, J.S.; Schnipper, J.L. Practicelinked online personal health records for type 2 diabetes mellitus: A randomized controlled trial. Arch. Intern. Med. 2008, 168, 1776–1782. [Google Scholar] [CrossRef] [Green Version]
- Tuil, W.S.; C M Verhaak, D.D.; de Vries Robbé, P.F.; Kremer, J.A.M. Empowering patients undergoing in vitro fertilization by providing Internet access to medical data. Fertil. Steril. 2007, 88, 361–368. [Google Scholar] [CrossRef]
- Wagner, P.; Dias, J.; Shalon, H.; Kintziger, K.W.; Hudson, M.F.; Seol, Y.H.; Sodomka, P. Personal health records and hypertension control: A randomized trial. J. Am. Med. Inform. Assoc. 2012, 19, 626–634. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- MHU. Mobile Clinic. Available online: https://publichealth.arizona.edu/outreach/primary-prevention-mobile-health-unit (accessed on 14 May 2021).
- Haggstrom, D.A.; Saleem, J.J.; Russ, A.L.; Jones, J.; Russell, S.A.; Chumbler, N.R. Lessons learned from usability testing of the VA’s personal health record. J. Am. Med. Inform. Assoc. 2011, 18, i13–i17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keefe, F.J.; Huling, D.A.; Coggins, M.J.; Keefe, D.F.; Rosenthal, M.Z.; Herr, N.R.; Hoffman, H.G. Virtual reality for persistent pain: A new direction for behavioral pain management. Pain 2012, 153, 2163–2166. [Google Scholar] [CrossRef] [PubMed]
- Mosadeghi, S.; Reid, M.W.; Martinez, B.; Rosen, B.T.; Spiegel, B.M.R. Feasibility of an immersive virtual reality intervention for hospitalized patients: An observational cohort study. JMIR Ment. Health 2016, 3, e28. [Google Scholar] [CrossRef]
- Fadel, K.; Brown, S.; Tanniru, M. A theoretical framework for knowledge transfer in process redesign. Data Base 2008, 39, 21–40. [Google Scholar] [CrossRef]
- Pwc. Available online: https://www.sleepreviewmag.com/uncategorized/pwc-research-resmeds-myair-significantly-improves-adherence-cpap-therapy/ (accessed on 14 May 2021).
- Timms, K.P.; Rivera, D.E.; Collins, L.M.; Piper, M.E. A dynamical systems approach to understanding self-regulation in smoking cessation behavior change. Nicotine Tob. Res. 2014, 16 (Suppl. 2), S159–S168. [Google Scholar] [CrossRef] [Green Version]
- Yu, K.-H.; Beam, A.L.; Kohane, I.S. Artificial intelligence in healthcare. Nat. Biomed. Eng. 2018, 2, 719–731. [Google Scholar] [CrossRef]
- Tanniru, M.; Jones, J.; Kazziha, S.; Hornberger, M. Strategies to address care transition—A methodology and a case study. J. Hosp. Adm. 2019, 8, 38. [Google Scholar]
- Khuntia, J.; Tanniru, M.; Weiner, J. Juggling digitization and technostress: The case of alert fatigues due to intelligent care system implementation at a hospital. Healthc. Policy Technol. 2015, 4, 364–377. [Google Scholar] [CrossRef]
- Agarwal, R.; Tanniru, M.; Wilemon, D. Assimilating information technology innovations: Strategies and moderating influences. IEEE Trans. Eng. Manag. 1997, 44, 358. [Google Scholar] [CrossRef]
- Khuntia, J.; Tanniru, M.; Fragoli, F.; Nawrocki, M. Mindfulness differences in hospital unit operations: Analysis of response to nurse call systems. Pac. Asia J. Assoc. Inf. Syst. 2016, 8, 33–36. [Google Scholar]
- McCradden, M.D.; Joshi, S.; Mazwi, M.; Anderson, J.A. Ethical Limitations of Algorithmic Fairness Solutions in Health Care Machine Learning; Elsevier: New York, NY, USA, 2020; Volume 2. [Google Scholar]
- Wenger, N.K. Cardiovascular disease: The female heart is vulnerable. A call to action from the 10Q Report. Clin. Cardiol. 2012, 35, 134–135. [Google Scholar] [CrossRef] [PubMed]
- Friedler, S.A.; Scheidegger, C.; Venkatasubramanian, S. On the (Im)possibility of Fairness. Available online: https://arxiv.org/pdf/1609.07236.pdf (accessed on 23 September 2019).
- Barocas, S.; Hardt, M.; Narayanan, A. Fairness and Machine Learning: Limitations and Opportunities. 2018. Available online: https://fairmlbook.org/ (accessed on 6 December 2019).
- Dearing, J.W.; Smith, D.K.; Larson, R.S.; Estabrooks, C.A. Designing for diffusion of a biomedical intervention. Am. J. Prev. Med. 2013, 44, S70–S76. [Google Scholar] [CrossRef]
- Endsley, M.R. Designing for Situation Awareness: An Approach to User-Centered Design, 2nd ed.; CRC Press, Inc.: Boca Raton, FL, USA, 2011. [Google Scholar]
- Agarwal, A.; Tanniru, M. Assessing organizational impacts of technology. Int. J. Technol. Manag. 1992, 7, 626–643. [Google Scholar] [CrossRef]
- Griffiths, F.; Watkins, J.A.; Huxley, C.; Harris, B.; Cave, J.; Pemba, S.; Chipwaza, B.; Lilford, R.; Ajisola, M.; Arvanitis, T.N.; et al. Mobile consulting (mConsulting) and its potential for providing access to quality healthcare for populations living in low-resource settings of low- and middle-income countries. Digit. Health 2020. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jansen, S.; Cusumano, M.A.; Popp, K.M. Managing software platforms and ecosystems. IEEE Softw. 2019, 36, 17–21. [Google Scholar] [CrossRef]
- Basole, R.C.; Park, H. Interfirm collaboration and firm value in software ecosystems: Evidence from cloud computing. IEEE Trans. Eng. Manag. 2019, 66, 368–380. [Google Scholar] [CrossRef]
- Basole, R.C.; Russell, M.G.; Huhtamaki, J.; Rubens, N.; Still, K.; Park, H. Understanding business ecosystem dynamics: A data-driven approach. ACM Trans. Manag. Inf. Syst. 2015, 6, 1–32. [Google Scholar] [CrossRef]
- Kumara, J.; Han, A.; Colman, W.; van den Heuvel, W.; Tamburri, D.A. Runtime evolution of multi-tenant service networks. In Proceedings of the Service Oriented and Cloud Computing—7th IFIP WG 2.14 European Conference; Proceedings, ser. Lecture Notes in Computer Science, ESOCC, Como, Italy, 12–14 September 2018; Kritikos, K., Plebani, P., Paoli, F.D., Eds.; Springer: New York, NY, USA, 2018; Volume 11116, pp. 33–48. [Google Scholar]
- de Vasconcelos Gomes, L.A.; Facin, A.L.F.; Salerno, M.S.; Ikenami, R.K. Unpacking the innovation ecosystem construct: Evolution, gaps and trends. Technol. Forecast. Soc. Chang. 2018, 136, 30–48. [Google Scholar] [CrossRef]
- Nguyen, L.H.; Thu, V.G.; Ha, G.H.; Nguyen, C.T.; Vu, H.M.; Nguyen, T.Q.; Tran, T.H.; Pham, K.T.H.; Latkin, C.A.; Tran, B.X.; et al. Fear of falling among older patients admitted to hospital after falls in vietnam: Prevalence, associated factors and correlation with impaired health-related quality of life. Int. J. Environ. Res. Public Health 2020, 17, 2493. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scheffer, A.C.; Schuurmans, M.J.; van Dijk, N.; van der Hooft, T.; de Rooij, S.E. Fear of falling: Measurement strategy, prevalence, risk factors and consequences among older persons. Age Aging 2006, 37, 19–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cumming, R.G.; Salkeld, G.; Thomas, M.; Szonyi, G. Prospective study of the impact of fear of falling on activities of daily living, SF-36 scores, and nursing home admission. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2000, 55, M299–M305. [Google Scholar] [CrossRef]
- Chamberlin, M.E.; Fulwider, B.D.; Sanders, S.I.; Medeiros, J.M. Does fear of falling influence spatial and temporal gait parameters in elderly persons beyond changes associated with normal aging? J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2005, 60, 1163–1167. [Google Scholar] [CrossRef]
- Deshpande, N.; Metter, E.J.; Bandinelli, S.; Lauretani, F.; Windham, B.G.; Ferrucci, L. Psychological, physical, and sensory correlates of fear of falling and consequent activity restriction in the elderly: The InCHIANTI study. Am. J. Phys. Med. Rehabil. 2008, 87, 354–362. [Google Scholar] [CrossRef] [Green Version]
- Chaccour, K.; Darazi, R.; Hassani, A.H.E.; Andres, E. From fall detection to fall prevention: A generic classification of fall-related systems. IEEE Sens. J. 2017, 17, 812–822. [Google Scholar] [CrossRef]
- Habib, M.; Mohktar, M.; Kamaruzzaman, S.; Lim, K.; Pin, T.; Ibrahim, F. Smartphone-based solutions for fall detection and prevention: Challenges and open issues. Sensors 2014, 14, 7181–7208. [Google Scholar] [CrossRef] [Green Version]
- Julayanont, P.; Phillips, N.; Chertkow, H.; Nasreddine, Z.S. Montreal Cognitive Assessment (MoCA): Concept and Clinical Review. In Cognitive Screening Instruments: A Practical Approach; Springer: London, UK, 2012; pp. 111–151. [Google Scholar]
- Shao, S.; Tunc, C.; Al-Shawi, A.; Hariri, S. Autonomic Author Identification in Internet Relay Chat (IRC). In Proceedings of the IEEE/ACS 15th International Conference on Computer Systems and Applications (AICCSA), Aqaba, Jordan, 28 October–1 November 2018. [Google Scholar]
- Ahmad, M.; Amin, M.; Hussain, S.; Kang, B.; Cheong, T.; Lee, S. Health fog: A novel framework for health and wellness applications. J. Supercomput. 2016, 72, 3677–3695. [Google Scholar] [CrossRef]
- Kumar, T.; Braeken, A.; Liyanage, M.; Ylianttila, M. Identity privacy preserving biometric based authentication scheme for Naked healthcare environment. In Proceedings of the IEEE International Conference on Communications (ICC), Paris, France, 21–25 May 2017. [Google Scholar]
- Pacheco, J.; Hariri, S. IoT security framework for smart cyber infrastructures. In Proceedings of the 2016 IEEE 1st International Workshops on Foundations and Applications of Self* Systems (FAS*W), Augsburg, Germany, 12–16 September 2016; pp. 242–247. [Google Scholar] [CrossRef]
- Gu, X.; Li, M.; Cao, Y.; Xiong, L. Supporting both range queries and frequency estimation with local differential privacy. In Proceedings of the 2019 IEEE Conference on Communications and Network Security (CNS), Washington, DC, USA, 10–12 June 2019. [Google Scholar]
- Tremblay, K. Healthcare @ The Speed of Thought: A digital world needs successful transformative leaders. Healthc. Manag. Forum. 2017, 30, 246–251. [Google Scholar] [CrossRef]
- Christensen, C.M.; Bohmer, R.; Kenagy, J. Will disruptive innovation cure healthcare? Harv. Bus. Rev. 2020, 78, 102–112. [Google Scholar]
- Schein Edgar, H. Coming to a new awareness of organizational culture. Sloan Manag. Rev. 1984, 25, 3. [Google Scholar]
- Uhl-Bien, M.; Marion, R.; McKelvey, B. Complexity leadership theory: Shifting leadership from the industrial age to the knowledge era. In Leadership, Gender, and Organization; Springer: New York, NY, USA, 2011; pp. 109–138. [Google Scholar]
- Cressman, D. A Brief Overview of Actor-Network Theory: Punctualization, Heterogeneous Engineering & Translation. 2009. Available online: https://www.semanticscholar.org/paper/A-Brief-Overview-of-Actor-Network-Theory%3A-%26-Cressman/09312181b176e8a32b1fc0cd7c1510cbcf98a57f (accessed on 7 April 2021).
- Fadhil, A.; Gabrielli, S. Addressing challenges in promoting healthy lifestyles. In Proceedings of the 11th EAI International Conference on Pervasive Computing Technologies for Healthcare, PervasiveHealth 17, Barcelona, Spain, 23–26 May 2017. [Google Scholar]
- Babylon Health. The Online Doctor and Prescription Services App, Babylon Health. 2019. Available online: https://www.babylonhealth.com (accessed on 5 August 2019).
- Buoy Health. Check Symptoms & Find the Right Care. Available online: https://www.buoyhealth.com/ (accessed on 7 April 2021).
- Chung, K.; Park, R.C. Chatbot-based healthcare service with a knowledge base for cloud computing. Clust. Comput. 2019, 22, 1925–1937. [Google Scholar] [CrossRef]
- Comendador, B.E.V.; Francisco, B.M.B.; Medenilla, J.S.; Nacion, S.M.T.; Serac, T.B.E. Pharmabot: A Pediatric Generic Medicine Consultant Chatbot. J. Autom. Control Eng. 2015, 3, 137–140. [Google Scholar] [CrossRef] [Green Version]
- Microsoft Health Bot Project. AI At Work for Your Patients, Microsoft Research. 2019. Available online: https://www.microsoft.com/en-us/research/project/health-bot/ (accessed on 7 April 2021).
- IBM Watson Health. AI Healthcare Solutions, IBM Watson Health. 2019. Available online: https://www.ibm.com/watson-health (accessed on 7 April 2021).


| Type | Skill | Story | Description |
|---|---|---|---|
| Movement Response | Sensor Response | Fall detection | Respond to patient and notify nurse by recognizing patient movement. |
| Wave | |||
| Regular Check | Hourly Rounding | Feeling check | Perform regular hourly check to fulfill patient needs actively. |
| Restroom check | |||
| Brace check | |||
| Heat pack check | |||
| Delirium Check | What day is today? | Perform regular delirium check to evaluate patient cognition. | |
| List weekdays in reversed order | |||
| Relaxations | Soothing Music | Play music | Use music, jokes, and small talk to improve patient’s mental state. |
| Small Talk | Random talk | ||
| Joke | Tell me a joke | ||
| More jokes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanniru, M.R.; Agarwal, N.; Sokan, A.; Hariri, S. An Agile Digital Platform to Support Population Health—A Case Study of a Digital Platform to Support Patients with Delirium Using IoT, NLP, and AI. Int. J. Environ. Res. Public Health 2021, 18, 5686. https://doi.org/10.3390/ijerph18115686
Tanniru MR, Agarwal N, Sokan A, Hariri S. An Agile Digital Platform to Support Population Health—A Case Study of a Digital Platform to Support Patients with Delirium Using IoT, NLP, and AI. International Journal of Environmental Research and Public Health. 2021; 18(11):5686. https://doi.org/10.3390/ijerph18115686
Chicago/Turabian StyleTanniru, Mohan R., Nimit Agarwal, Amanda Sokan, and Salim Hariri. 2021. "An Agile Digital Platform to Support Population Health—A Case Study of a Digital Platform to Support Patients with Delirium Using IoT, NLP, and AI" International Journal of Environmental Research and Public Health 18, no. 11: 5686. https://doi.org/10.3390/ijerph18115686
APA StyleTanniru, M. R., Agarwal, N., Sokan, A., & Hariri, S. (2021). An Agile Digital Platform to Support Population Health—A Case Study of a Digital Platform to Support Patients with Delirium Using IoT, NLP, and AI. International Journal of Environmental Research and Public Health, 18(11), 5686. https://doi.org/10.3390/ijerph18115686





