A Comparative Analysis of Risky Sexual Behaviors, Self-Reported Sexually Transmitted Infections, Knowledge of Symptoms and Partner Notification Practices among Male and Female University Students in Pretoria, South Africa
Abstract
1. Introduction
2. Methods
2.1. Study Design and Population
2.2. Measures
2.3. Data Collection
2.4. Data Analysis
2.5. Ethical Considerations
3. Results
3.1. Characteristics of Students
3.2. Risky Sexual Behaviour
3.3. Perception of Risk and Preventive Practices on STIs
3.4. Knowledge of Selected STI Symptoms
3.5. Self-Reported STIs Symptoms and Partner Notification Practices
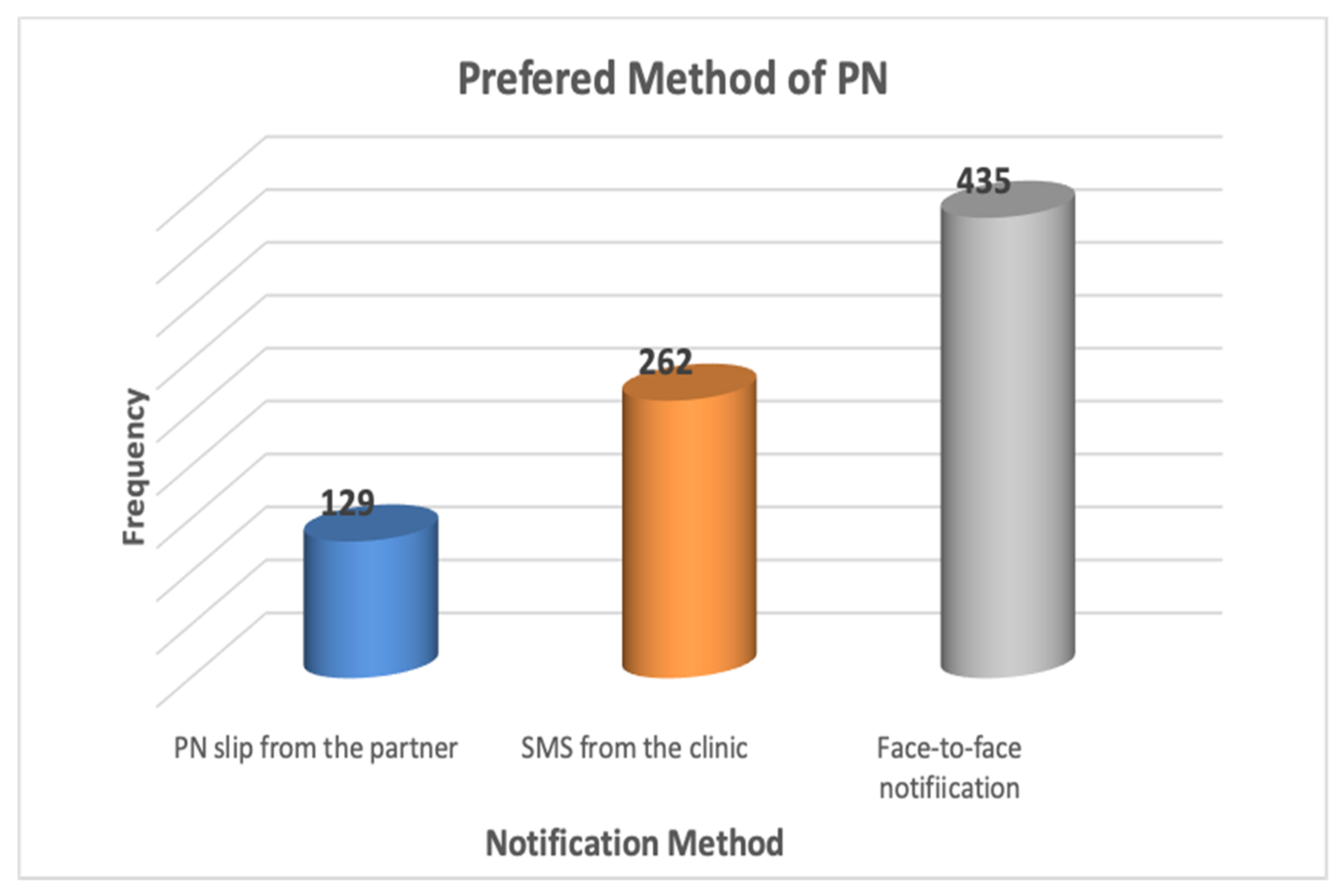
3.6. Partner Notification Intentions
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. More Than 1 Million New Curable Sexually Transmitted Infections Every Day; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- World Health Organization. Global Strategy for the Prevention and Control of Sexually Transmitted Infections: 2006–2015: Breaking the Chain of Transmission; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Francis, S.C.; Mthiyane, T.N.; Baisley, K.; Mchunu, S.L.; Ferguson, J.B.; Smit, T.; Crucitti, T.; Gareta, D.; Dlamini, S.; Mutevedzi, T. Prevalence of sexually transmitted infections among young people in South Africa: A nested survey in a health and demographic surveillance site. PLoS Med. 2018, 15, e1002512. [Google Scholar] [CrossRef]
- World Health Organization. Global Health Sector Strategy on Sexually Transmitted Infections 2016–2021: Toward Ending STIs; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Nubed, C.K.; Akoachere, J.-F.T.K. Knowledge, attitudes and practices regarding HIV/AIDS among senior secondary school students in Fako Division, South West Region, Cameroon. BMC Public Health 2016, 16, 1–10. [Google Scholar] [CrossRef]
- Somba, M.J.; Mbonile, M.; Obure, J.; Mahande, M.J. Sexual behaviour, contraceptive knowledge and use among female undergraduates’ students of Muhimbili and Dar es Salaam Universities, Tanzania: A cross-sectional study. BMC Women’s Health 2014, 14, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kassie, B.A.; Yenus, H.; Berhe, R.; Kassahun, E.A. Prevalence of sexually transmitted infections and associated factors among the University of Gondar students, Northwest Ethiopia: A cross-sectional study. Reprod. Health 2019, 16, 1–8. [Google Scholar] [CrossRef]
- Shiferaw, K.; Getahun, F.; Asres, G. Assessment of adolescents’ communication on sexual and reproductive health matters with parents and associated factors among secondary and preparatory schools’ students in Debremarkos town, North West Ethiopia. Reprod. Health 2014, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Tura, G.; Alemseged, F.; Dejene, S. Risky sexual behavior and predisposing factors among students of Jimma University, Ethiopia. Ethiop. J. Health Sci. 2012, 22, 170–180. [Google Scholar] [PubMed]
- Ngidi, N.D.; Moyo, S.; Zulu, T.; Adam, J.K.; Krishna, S.B.N. Qualitative evaluation of selected social factors that impact sexual risk-taking behaviour among African students in Kwazulu-Natal, South Africa. SAHARA J J. Soc. Asp. HIV AIDS 2016, 13, 96–105. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Talwar, P.; Abd Rahman, M.F.B. Assessment of HIV knowledge among university students using the HIV-KQ-18 scale: A cross-sectional study. South East Asia J. Public Health 2015, 5, 33–38. [Google Scholar] [CrossRef]
- Kebede, A.; Molla, B.; Gerensea, H. Assessment of risky sexual behavior and practice among Aksum University students, Shire Campus, Shire Town, Tigray, Ethiopia, 2017. BMC Res. Notes 2018, 11, 1–6. [Google Scholar] [CrossRef]
- Abera, M.; Ofori, K.; Opito, R.; Nanfuka, M.; Mugenyi, L.; Etukoit, M. Unprotected Sex and Associated Factors among Adolescent Students of Rift Valley University Jimma Campus, Jimma Town, South West Ethiopia: Institution Based Cross Sectional Study. Int. J. HIV AIDS Prev. Educ. Behav. Sci. 2019, 5, 1. [Google Scholar] [CrossRef]
- Blignaut, R.J.; Jacobs, J.; Vergnani, T. Trends in HIV risk behaviour of incoming first-year students at a South African university: 2007–2012. SAHARA J J. Soc. Asp. HIV AIDS 2015, 12, 39–50. [Google Scholar] [CrossRef]
- HEAIDS. Knowledge, Attitudes, and Behaviours of Students and Staff at South Africa’s Technical and Vocational Education and Training Colleges, 2014; Human Sciences Research Council (HSRC): Pretoria, South Africa, 2014; Available online: http://www.hsrc.ac.za/uploads (accessed on 12 April 2021).
- Akullian, A.; Bershteyn, A.; Klein, D.; Vandormael, A.; Bärnighausen, T.; Tanser, F. Sexual partnership age pairings and risk of HIV acquisition in rural South Africa. AIDS 2017, 31, 1755–1764. [Google Scholar] [CrossRef] [PubMed]
- Stoner, M.C.; Nguyen, N.; Kilburn, K.; Gómez-Olivé, F.X.; Edwards, J.K.; Selin, A.; Hughes, J.P.; Agyei, Y.; Macphail, C.; Kahn, K. Age-disparate partnerships and incident HIV infection in adolescent girls and young women in rural South Africa: An HPTN 068 analysis. AIDS 2019, 33, 83. [Google Scholar] [CrossRef] [PubMed]
- Subbarao, N.T.; Akhilesh, A. Knowledge and attitude about sexually transmitted infections other than HIV among college students. Indian J. Sex. Transm. Dis. AIDS 2017, 38, 10–14. [Google Scholar] [CrossRef]
- Molla, G.; Desalegn, A.; Tigu, F. Prevalence of Gonorrhea and Associated Knowledge, Attitude and Risky Behaviors and Preventive Practices Among High School Students: A Cross-Sectional Study. J. Community Health 2021, 46, 358–366. [Google Scholar] [CrossRef]
- Kaida, A.; Dietrich, J.J.; Laher, F.; Beksinska, M.; Jaggernath, M.; Bardsley, M.; Smith, P.; Cotton, L.; Chitneni, P.; Closson, K. A high burden of asymptomatic genital tract infections undermines the syndromic management approach among adolescents and young adults in South Africa: Implications for HIV prevention efforts. BMC Infect. Dis. 2018, 18, 1–11. [Google Scholar] [CrossRef]
- Garrett, N.J.; McGrath, N.; Mindel, A. Advancing STI Care in Low/Middle-Income Countries: Has STI Syndromic Management Reached Its Use-by Date? BMJ Publishing Group Ltd.: London, UK, 2017. [Google Scholar]
- Kalichman, S.C.; Mathews, C.; Kalichman, M.; Lurie, M.N.; Dewing, S. Perceived barriers to partner notification among sexually transmitted infection clinic patients, Cape Town, South Africa. J. Public Health 2017, 39, 407–414. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Alam, N.; Chamot, E.; Vermund, S.H.; Streatfield, K.; Kristensen, S. Partner notification for sexually transmitted infections in developing countries: A systematic review. BMC Public Health 2010, 10, 1–11. [Google Scholar] [CrossRef]
- Pellowski, J.; Mathews, C.; Kalichman, M.O.; Dewing, S.; Lurie, M.N.; Kalichman, S.C. Advancing partner notification through electronic communication technology: A review of acceptability and utilization research. J. Health Commun. 2016, 21, 629–637. [Google Scholar] [CrossRef] [PubMed]
- Levine, D.; Woodruff, A.J.; Mocello, A.R.; Lebrija, J.; Klausner, J.D. inSPOT: The first online STD partner notification system using electronic postcards. PLoS Med. 2008, 5, e213. [Google Scholar] [CrossRef]
- Hogben, M. Partner notification for sexually transmitted diseases. Clin. Infect. Dis. 2007, 44, S160–S174. [Google Scholar] [CrossRef] [PubMed]
- Mathews, C.; Kalichman, M.O.; Laubscher, R.; Hutchison, C.; Nkoko, K.; Lurie, M.; Kalichman, S.C. Sexual relationships, intimate partner violence and STI partner notification in Cape Town, South Africa: An observational study. Sex. Transm. Infect. 2018, 94, 144–150. [Google Scholar] [CrossRef]
- Cassidy, C.; Curran, J.; Steenbeek, A.; Langille, D. University students’ sexual health knowledge: A Scoping literature review. Can. J. Nurs. Res. Arch. 2015, 47, 18–38. [Google Scholar] [CrossRef]
- Lewis, D.A.; Chirwa, T.F.; Msimang, V.M.; Radebe, F.M.; Kamb, M.L.; Firnhaber, C.S. Urethritis/cervicitis pathogen prevalence and associated risk factors among asymptomatic HIV-infected patients in South Africa. Sex. Transm. Dis. 2012, 39, 531–536. [Google Scholar] [CrossRef]
- Madiba, S.; Mokgatle, M. Assessing risk perceptions, condom use, and sexual behaviour of student at Technical Vocational Education and Training colleges in Gauteng and North West Provinces in South Africa. PULA Botsw. J. Afr. Stud. 2016, 30, 150–165. [Google Scholar]
- Clark, J.L.; Long, C.M.; Giron, J.M.; Cuadros, J.A.; Caceres, C.F.; Coates, T.J.; Klausner, J.D. Partner notification for sexually transmitted diseases in Peru: Knowledge, attitudes, and practices in a high-risk community. Sex. Transm. Dis. 2007, 34, 309–313. [Google Scholar] [CrossRef]
- Folasayo, A.T.; Oluwasegun, A.J.; Samsudin, S.; Saudi, S.N.S.; Osman, M.; Hamat, R.A. Assessing the knowledge level, attitudes, risky behaviors and preventive practices on sexually transmitted diseases among university students as future healthcare providers in the central zone of Malaysia: A cross-sectional study. Int. J. Environ. Res. Public Health 2017, 14, 159. [Google Scholar] [CrossRef]
- Ayerdi Aguirrebengoa, O.; Vera Garcia, M.; Rueda Sanchez, M.; D’ Elia, G.; Chavero Méndez, B.; Alvargonzalez Arrancudiaga, M.; Bello León, S.; Puerta López, T.; Clavo Escribano, P.; Ballesteros Martín, J. Risk factors associated with sexually transmitted infections and HIV among adolescents in a reference clinic in Madrid. PLoS ONE 2020, 15, e0228998. [Google Scholar] [CrossRef] [PubMed]
- Abdul, R.; Gerritsen, A.A.; Mwangome, M.; Geubbels, E. Prevalence of self-reported symptoms of sexually transmitted infections, knowledge and sexual behaviour among youth in semi-rural Tanzania in the period of adolescent friendly health services strategy implementation. BMC Infect. Dis. 2018, 18, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Amu, E.; Adegun, P. Awareness and knowledge of sexually transmitted infections among secondary school adolescents in Ado Ekiti, South Western Nigeria. J. Sex. Transm. Dis. 2015, 2015, 1–7. [Google Scholar] [CrossRef]
- Fonte, V.R.F.d.; Spindola, T.; Francisco, M.T.R.; Sodré, C.P.; André, N.L.N.d.O.; Pinheiro, C.D. Young university students and the knowledge about sexually transmitted infections. Esc. Anna Nery 2018, 22, 22. [Google Scholar] [CrossRef]
- Oharume, I.M. Knowledge, sexual behaviours and risk perception of sexually transmitted infections among students of the polytechnic, Ibadan, Oyo state. Afr. Health Sci. 2020, 20, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Sham, F.; Yaakub, S.; Fawati, F.N.; Fatinni, S.J.; Azamuddin, A.A. Knowledge, attitudes, risk behaviours and preventive practices on sexually transmitted diseases among students in a public university in malaysia. Malays. J. Public Health Med. 2020, 20, 100–108. [Google Scholar] [CrossRef]
- Mokgatle, M.M.; Madiba, S. Risky sexual behaviour amidst predicament of acceptable sexually transmitted infection partner notification modalities: A cross-sectional survey amongst minibus taxi drivers in Gauteng Province, South Africa. S. Afr. Fam. Pract. 2020, 62, e1–e6. [Google Scholar] [CrossRef]
- Gezae, K.E.; Gebretsadik, L.G.; Abebe, H.T.; Meles, H.G.; Fisseha, M.A.; Gebremedhin, E.A.; Yetbarek, A.S. Unsafe sex practice and its associated factors among regular undergraduate students of Mekelle University, Ethiopia, 2019: A facility based cross-sectional study. Ethiop. J. Reprod. Health 2020, 12, 10. [Google Scholar]
- Gutu, B. Gender Difference in Risky Sexual Behaviour and Associated Factors among Undergraduate Students in Dambi Dollo University, Ethiopia. Ethiop. J. Reprod. Health 2020, 12, 11. [Google Scholar]
- Afriyie, J.; Essilfie, M.E. Association between risky sexual behaviour and HIV risk perception among in-school adolescents in a municipality in Ghana. Ghana Med. J. 2019, 53, 29–36. [Google Scholar] [CrossRef]
- Sychareun, V.; Thomsen, S.; Chaleunvong, K.; Faxelid, E. Risk perceptions of STIs/HIV and sexual risk behaviours among sexually experienced adolescents in the Northern part of Lao PDR. BMC Public Health 2013, 13, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Osingada, C.P.; Nabasirye, C.; Groves, S.; Ngabirano, T.D. Perceived risk of HIV infection and associated factors among secondary school students in Wakiso district, Uganda. Adv. Public Health 2016, 2016, 1–7. [Google Scholar] [CrossRef]
- Buchsbaum, A.; Gallo, M.F.; Whiteman, M.K.; Cwiak, C.; Goedken, P.; Kraft, J.M.; Jamieson, D.J.; Kottke, M. Sexually transmitted disease partner notification among African-American, adolescent women. Infect. Dis. Obstet. Gynecol. 2014, 2014, 619632. [Google Scholar] [CrossRef] [PubMed]
- Taleghani, S.; Joseph-Davey, D.; West, S.B.; Klausner, H.J.; Wynn, A.; Klausner, J.D. Acceptability and efficacy of partner notification for curable sexually transmitted infections in sub-Saharan Africa: A systematic review. Int. J. STD AIDS 2019, 30, 292–303. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Frequency (%) | |
|---|---|---|
| Sex (n = 915) | Female | 643 (70.3) |
| Male | 272 (29.7) | |
| 17–20 | 442 (48.6) | |
| 21–25 | 391 (42.9) | |
| >25 | 77 (8.5) | |
| Field of study (n = 911) | Bachelor of Pharmacy | 270 (29.6) |
| Bachelor Medicine | 161 (17.8) | |
| Bachelor Occupational Therapy | 111 (12.2) | |
| Bachelor of Science | 78 (8.6) | |
| Bachelor Nursing Science | 69 (7.6) | |
| Bachelor Diagnostic Radiography | 61 (6.7) | |
| Other | 162 (17.8) | |
| Year of study (n = 901) | First | 227 (25.2) |
| Second | 296 (32.8) | |
| Third | 222 (24.6) | |
| Fourth | 135 (15) | |
| Fifth to sixth | 22 (2.4) | |
| Place of residence (n = 889) | Campus | 455 (49.7) |
| Off-campus | 430 (46.9) | |
| Other | 31 (3.4) | |
| Sexually active | Yes | 459 (50.5) |
| No | 450 (49.5) | |
| Relationship status (n = 661) | Steady partner | 479 (72.5) |
| Casual partner | 160 (24.2) | |
| Married | 22 (3.3) | |
| Duration of the relationship (n = 540) | 1–11 months | 189 (35) |
| 1–3 years | 235 (43.5) | |
| 3–5 years | 77 (14.3) | |
| 5–10 years | 39 (7.2) | |
| Number of sexual partners in the previous 12 months (n = 583) | 1 | 421 (71.3) |
| 2 | 97 (16.1) | |
| >2 | 75 (12.6) | |
| Concurrent sexual partners (n = 257) | No | 413 (68.3) |
| Yes | 192 (31.7) | |
| Female | Male | p Value | |||
|---|---|---|---|---|---|
| Yes n (%) | No n (%) | Yes n (%) | No n (%) | ||
| Sexual relationships | |||||
| Sexually active | 301 (47.3) | 335 (52.7) | 146 (54.1) | 124 (45.9) | 0.063 |
| Had more than one sexual partner | 77 (14.1) | 470 (85.9) | 114 (46.0) | 134 (54.0) | <0.001 * |
| Transactional sex in past 12 months | 6 (1.0) | 565 (99.0) | 13 (5.3) | 234 (99.7) | <0.001 * |
| Had one-night stand in past 6 months | 22 (4.0) | 533 (96.0) | 68 (28.1) | 174 (71.9) | <0.001 * |
| Condom use | |||||
| Used condom the last sexual act | 248 (55.9) | 196 (44.1) | 166 (69.7) | 72 (30.3) | <0.001 * |
| Male condoms easily available on campus | 531 (92.0) | 46 (8.0) | 245 (90.7) | 25 (9.3) | 0.529 |
| Female condoms easily available on campus | 133 (23.3) | 437 (76.7) | 46 (20.4) | 180 (79.6) | 0.364 |
| Could purchase condoms without feeling embarrassed | 358 (63.7) | 204 (36.3) | 216 (80.6) | 52 (19.4) | <0.001 * |
| Could get condoms from a public place without feeling embarrassed | 272 (48.1) | 294 (51.9) | 175 (65.8) | 91 (34.2) | <0.001 * |
| Always carry a condom | 85 (16.3) | 436 (83.7) | 104 (40.9) | 150 (59.1) | <0.001 * |
| Ever used a female condom | 18 (3.2) | 551 (72.3) | 10 (4.5) | 211 (95.5) | 0.353 |
| Feel confident to suggest condom use with new partner | 478 (93.7) | 32 (6.3) | 237 (92.6) | 19 (7.4) | 0.548 |
| HIV testing and STI | |||||
| Has been tested for HIV in the last 12 months | 368 (59.8) | 247 (40.2) | 126 (47.0) | 142 (53.0) | <0.001 * |
| Know partner’s HIV status | 315 (60.7) | 204 (39.3) | 119 (48.4) | 127 (51.6) | 0.001 * |
| Had an STI in the last 12 months | 27 (4.5) | 573 (95.5) | 13 (5.6) | 239 (94.8) | 0.678 |
| Female | Male | p-Value | ||
|---|---|---|---|---|
| Chances of refusing sex if condom is not used | 0.000 * | |||
| Likely Unlikely | 425 (79.7) | 158 (61.2) | ||
| 108 (20.3) | 100 (38.8) | |||
| Chances of discussing HIV testing with partner | 0.001 * | |||
| Likely | 459 (78.5) | 178 (67.2) | ||
| Unlikely | 125 (21.5) | 87 (32.8) | ||
| Chances of asking partner to go for HIV test | ||||
| Likely | 439 (76.8) | 155 (59.4) | ||
| Unlikely | 133 (23.3) | 106 (40.6) | ||
| Perceived risk of being infected with HIV | 0.012 * | |||
| Very worried | 304 (49.2) | 144 (53.5) | ||
| Worried | 113 (18.3) | 63 (23.4) | ||
| Not worried | 201 (32.5) | 62 (23.1) | ||
| Perceived risk of contracting STIs | 0.265 | |||
| Likely | 78 (12.9) | 44 (16.8) | ||
| Unlikely | 525 (87.1) | 218 (83.2) | ||
| How important is it to the tell partner about STI infection? | 0.004 * | |||
| Not important | 12 (2.1) | 12 (2.1) | ||
| Important | 60 (30.3) | 37 (15.7) | ||
| Very important | 510 (87.6) | 187 (79.2) | ||
| Item | Female | Male | p-Value |
|---|---|---|---|
| Yes n (%) | Yes n (%) | ||
| Itching in genital area | 317 (49.3) | 121 (44.5) | 0.183 |
| Discharge | 329 (51.2) | 129 (47.4) | 0.301 |
| Pain during urination | 309 (48.1) | 138 (50.7) | 0.459 |
| Genital ulcers or open sores | 290 (45.1) | 104 (38.2) | 0.055 |
| Pain during intercourse | 229 (35.6) | 76 (27.9) | 0.024 * |
| A person can have an STI without symptoms | 421 (70.6) | 198 (77.0) | 0.054 |
| Frequency | Percent | |
|---|---|---|
| Ever diagnosed with STIs | ||
| No | 815 | 95.3 |
| Yes | 40 | 4.7 |
| STIs symptoms experienced | ||
| Itching in genital area | 9 | 34.6 |
| Discharge | 7 | 26.9 |
| Pain when urinating | 6 | 23.1 |
| Genital ulcers or open sores | 2 | 7.69 |
| Pain during intercourse | 2 | 7.69 |
| Informed sex partner of STI | ||
| No | 14 | 37.84 |
| Yes | 23 | 62.16 |
| Received PN slip during consultation for STI symptoms | ||
| No | 12 | 66.67 |
| Yes | 24 | 33.33 |
| Delivered PN slip to partner | ||
| No | 14 | 56 |
| Yes | 11 | 44 |
| Reasons for failing to tell | ||
| I would be embarrassed | 6 | 37.5 |
| Fear of losing partner | 4 | 25.00 |
| Partner would refuse to have sex | 2 | 12.50 |
| Partner would blame me | 1 | 6.25 |
| Could not locate partner | 1 | 6.25 |
| Informed of an STI by partner | ||
| No | 18 | 72.00 |
| Yes | 7 | 28.00 |
| Received PN slip from partner with STI | ||
| No | 13 | 52.00 |
| Yes | 12 | 48.00 |
| Statement | Female | Male | p-Value | OR(95%CI) | ||||
|---|---|---|---|---|---|---|---|---|
| No n (%) | Not Sure n (%) | Yes n (%) | No n (%) | Not Sure n (%) | Yes n (%) | |||
| If you have an STI, could you tell your partner about the infection? | 12 (2.1) | 60 (10.3) | 510 (87.6) | 12 (5.1) | 37 (15.7) | 187 (79.2) | 0.55 0.95 * | Ref Not sure 0.13 (0.75–1.17) Yes 1.38 (0.95–2.01) |
| If have an STI, would you deliver a PN slip to your partner? | 20 (3.4) | - | 573 (96.6) | 18 (7.4) | - | 226 (92.6) | 0.014 * | Ref Yes 0.43 (0.23–0.84) |
| If have an STI, would you deliver a PN slip to your ex-sexual partner? | 157 (26.8) | 174 (29.7) | 255 (43.5) | 55 (22.6) | 67 (27.6) | 121 (49.8) | 0.55 0.10 | Ref Not sure 0.14 (0.57–1.72) Yes 1.38 (0.95–2.01) |
| If your partner delivers a PN slip that request you for STI treatment, would you find that easy? | 80 (13.4) | 115 (19.5) | 395 (67.0) | 38 (15.9) | 47 (19.7) | 154 (64.4) | 0.54 0.34 | Ref Not sure 0.85 (0.51–1.42) Yes 0.81 (0.53–1.24) |
| How easy would it be deliver a PN slip to your partner? | 251 (42.8) | 101 (17.2) | 234 (39.9) | 124 (51.2) | 42 (17.4) | 76 (31.4) | 0.42 0.02 | Ref Not sure 0.84 (0.55–1.3) Yes 0.66 (0.47–0.92) |
| Would you prefer an SMS from a doctor sent to your partner to get STI treatment? | 184 (31.7) | 67 (11.5) | 330 (56.8) | 56 (23.3) | 26 (10.8) | 158 (65.8) | 0.19 0.02 * | No Ref Not sure 1.4 (0.85–2.23) Yes 1.5 (0.23–0.41) |
| Do you think an SMS would work better to notify partners to get STI treatment? | 202 (34.4) | 85(14.5) | 300 (51.1) | 62 (25.8) | 36 (15.0) | 142 (59.2) | 0.14 0.03 * | No Ref Not sure 0.86 (0.70–1.05) Yes 0.59 (0.36–0.96) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mokgatle, M.M.; Madiba, S.; Cele, L. A Comparative Analysis of Risky Sexual Behaviors, Self-Reported Sexually Transmitted Infections, Knowledge of Symptoms and Partner Notification Practices among Male and Female University Students in Pretoria, South Africa. Int. J. Environ. Res. Public Health 2021, 18, 5660. https://doi.org/10.3390/ijerph18115660
Mokgatle MM, Madiba S, Cele L. A Comparative Analysis of Risky Sexual Behaviors, Self-Reported Sexually Transmitted Infections, Knowledge of Symptoms and Partner Notification Practices among Male and Female University Students in Pretoria, South Africa. International Journal of Environmental Research and Public Health. 2021; 18(11):5660. https://doi.org/10.3390/ijerph18115660
Chicago/Turabian StyleMokgatle, Mathildah Mpata, Sphiwe Madiba, and Lindiwe Cele. 2021. "A Comparative Analysis of Risky Sexual Behaviors, Self-Reported Sexually Transmitted Infections, Knowledge of Symptoms and Partner Notification Practices among Male and Female University Students in Pretoria, South Africa" International Journal of Environmental Research and Public Health 18, no. 11: 5660. https://doi.org/10.3390/ijerph18115660
APA StyleMokgatle, M. M., Madiba, S., & Cele, L. (2021). A Comparative Analysis of Risky Sexual Behaviors, Self-Reported Sexually Transmitted Infections, Knowledge of Symptoms and Partner Notification Practices among Male and Female University Students in Pretoria, South Africa. International Journal of Environmental Research and Public Health, 18(11), 5660. https://doi.org/10.3390/ijerph18115660







