Use of Coronary Computed Tomography Angiography to Screen Hospital Employees with Cardiovascular Risk Factors
Abstract
1. Introduction
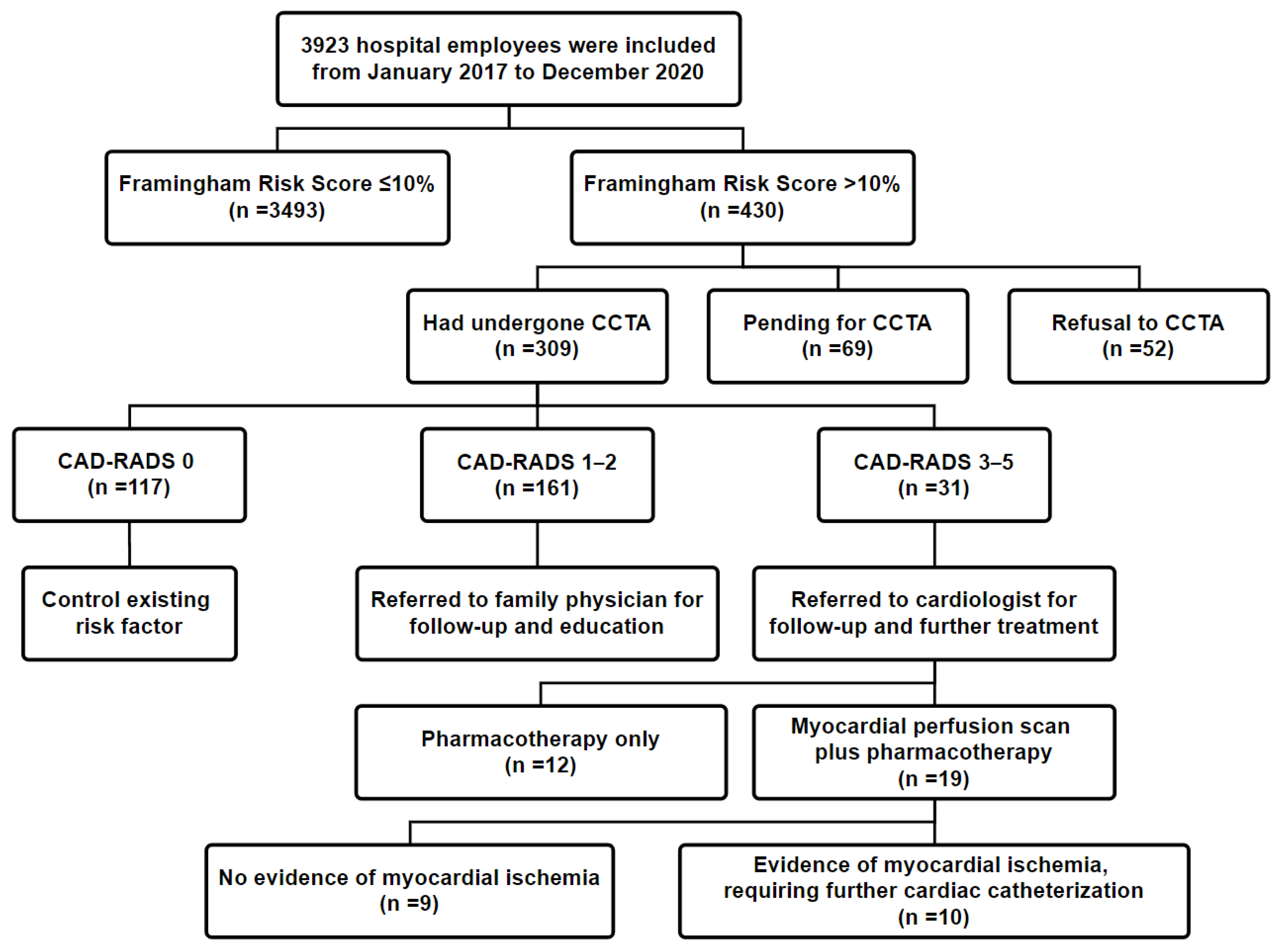
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Welfare, M.H. Available online: https://www.mohw.gov.tw/cp-16-54482-1.html (accessed on 15 August 2020).
- Murphy, S.L.; Xu, J.; Kochanek, K.D.; Arias, E.; Tejada-Vera, B. National Vital Statistics Reports. Natl. Vital Stat. Rep. 2021, 69. Available online: https://www.cdc.gov/nchs/data/nvsr/nvsr69/nvsr69-13-tables-508.pdf (accessed on 1 March 2021).
- World Health Organization. Available online: https://www.who.int/en/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 15 August 2020).
- World Health Organization. Available online: https://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html (accessed on 15 August 2020).
- Kang, M.-Y.; Cho, S.-H.; Yoo, M.-S.; Kim, T.; Hong, Y.-C. Long working hours may increase risk of coronary heart disease. Am. J. Ind. Med. 2014, 57, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, M.; Heikkilä, K.; Jokela, M.; Ferrie, J.E.; Batty, G.D.; Vahtera, J.; Kivimäki, M. Long working hours and coronary heart disease: A systematic review and meta-analysis. Am. J. Epidemiol. 2012, 176, 586–596. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Pega, F.; Ujita, Y.; Brisson, C.; Clays, E.; Descatha, A.; Ferrario, M.M.; Godderis, L.; Iavicoli, S.; Landsbergis, P.A.; et al. The effect of exposure to long working hours on ischaemic heart disease: A systematic review and meta-analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury. Envriron. Int. 2020, 142, 105739. [Google Scholar] [CrossRef] [PubMed]
- Kivimaki, M.; Jokela, M.; Nyberg, S.T.; Singh-Manoux, A.; Fransson, E.I.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Casini, A.; et al. Long working hours and risk of coronary heart disease and stroke: A systematic review and meta-analysis of published and unpublished data for 603 838 individuals. Lancet 2015, 386, 1739–1746. [Google Scholar] [CrossRef]
- Kivimäki, M.; Nyberg, S.T.; Batty, G.D.; Fransson, E.I.; Heikkilä, K.; Alfredsson, L.; Bjorner, J.B.; Borritz, M.; Burr, H.; Casini, A.; et al. Job strain as a risk factor for coronary heart disease: A collaborative meta-analysis of individual participant data. Lancet 2012, 380, 1491–1497. [Google Scholar] [CrossRef]
- Wirtz, P.H.; von Känel, R. Psychological Stress, Inflammation, and Coronary Heart Disease. Curr. Cardiol. Rep. 2017, 19, 111. [Google Scholar] [CrossRef]
- Sara, J.D.; Prasad, M.; Eleid, M.F.; Zhang, M.; Widmer, R.J.; Lerman, A. Association Between Work-Related Stress and Coronary Heart Disease: A Review of Prospective Studies Through the Job Strain, Effort-Reward Balance, and Organizational Justice Models. J. Am. Hear. Assoc. 2018, 7, e008073. [Google Scholar] [CrossRef]
- Vetter, C.; Devore, E.E.; Wegrzyn, L.R.; Massa, J.; Speizer, F.E.; Kawachi, I.; Rosner, B.; Stampfer, M.J.; Schernhammer, E.S. Association Between Rotating Night Shift Work and Risk of Coronary Heart Disease Among Women. JAMA 2016, 315, 1726–1734. [Google Scholar] [CrossRef]
- Hermansson, J.; Bøggild, H.; Hallqvist, J.; Karlsson, B.; Knutsson, A.; Nilsson, T.; Reuterwall, C.; Gådin, K.G. Interaction between Shift Work and Established Coronary Risk Factors. Int. J. Occup. Environ. Med. 2019, 10, 57–65. [Google Scholar] [CrossRef]
- Torquati, L.; Mielke, G.I.; Brown, W.J.; Kolbe-Alexander, T. Shift work and the risk of cardiovascular disease. A systematic review and meta-analysis including dose-response relationship. Scand. J. Work. Environ. Health 2018, 44, 229–238. [Google Scholar] [CrossRef]
- Stone, G.W.; Maehara, A.; Lansky, A.J.; De Bruyne, B.; Cristea, E.; Mintz, G.S.; Mehran, R.; McPherson, J.; Farhat, N.; Marso, S.P.; et al. A Prospective Natural-History Study of Coronary Atherosclerosis. N. Engl. J. Med. 2011, 364, 226–235. [Google Scholar] [CrossRef]
- Ali, Z.A.; Karimi Galougahi, K.; Maehara, A.; Shlofmitz, R.A.; Ben-Yehuda, O.; Mintz, G.S.; Stone, G.W. Intracoronary Optical Coherence Tomography 2018: Current Status and Future Directions. JACC Cardiovasc. Interv. 2017, 10, 2473–2487. [Google Scholar] [CrossRef]
- Nakanishi, R.; Motoyama, S.; Leipsic, J.; Budoff, M.J. How accurate is atherosclerosis imaging by coronary computed tomography angiography? J. Cardiovasc. Comput. Tomogr. 2019, 13, 254–260. [Google Scholar] [CrossRef]
- Williams, M.C.; Newby, D.E.; Nicol, E.D. Coronary atherosclerosis imaging by CT to improve clinical outcomes. J. Cardiovasc. Comput. Tomogr. 2019, 13, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Cury, R.C.; Abbara, S.; Achenbach, S.; Agatston, A.; Berman, D.S.; Budoff, M.J.; Dill, K.E.; Jacobs, J.E.; Maroules, C.D.; Rubin, G.D.; et al. CAD-RADS™: Coronary Artery Disease—Reporting and Data System. J. Am. Coll. Radiol. 2016, 13, 1458–1466.e9. [Google Scholar] [CrossRef] [PubMed]
- Foldyna, B.; Szilveszter, B.; Scholtz, J.-E.; Banerji, D.; Maurovich-Horvat, P.; Hoffmann, U. CAD-RADS—A new clinical decision support tool for coronary computed tomography angiography. Eur. Radiol. 2017, 28, 1365–1372. [Google Scholar] [CrossRef]
- Guaricci, A.I.; De Santis, D.; Carbone, M.; Muscogiuri, G.; Guglielmo, M.; Baggiano, A.; Serviddio, G.; Pontone, G. Coronary atherosclerosis assessment by coronary ct angiography in asymptomatic diabetic population: A critical systematic review of the literature and future perspectives. Biomed Res. Int. 2018, 2018, 1–13. [Google Scholar] [CrossRef]
- Lee, K.Y.; Hwang, B.-H.; Kim, T.-H.; Kim, C.J.; Kim, J.-J.; Choo, E.-H.; Choi, I.J.; Choi, Y.; Park, H.-W.; Koh, Y.-S.; et al. Computed Tomography Angiography Images of Coronary Artery Stenosis Provide a Better Prediction of Risk Than Traditional Risk Factors in Asymptomatic Individuals With Type 2 Diabetes: A Long-term Study of Clinical Outcomes. Diabetes Care 2017, 40, 1241–1248. [Google Scholar] [CrossRef] [PubMed]
- Dedic, A.; Kate, G.-J.R.T.; Roos, C.J.; Neefjes, L.A.; De Graaf, M.A.; Spronk, A.; Delgado, V.; Van Lennep, J.E.R.; Moelker, A.; Ouhlous, M.; et al. Prognostic Value of Coronary Computed Tomography Imaging in Patients at High Risk Without Symptoms of Coronary Artery Disease. Am. J. Cardiol. 2016, 117, 768–774. [Google Scholar] [CrossRef]
- Kang, W.; Park, W.-J.; Jang, K.-H.; Kim, S.-H.; Gwon, D.-H.; Lim, H.-M.; Ahn, J.-S.; Moon, J.-D. Coronary artery atherosclerosis associated with shift work in chemical plant workers by using coronary CT angiography. Occup. Environ. Med. 2016, 73, 501–505. [Google Scholar] [CrossRef]
- Slim, J.; Castillo-Rojas, L.; Hann, M.; Symons, J.; Martinho, S.; Sim, J.; Jimenez, S.; Haney, B.; Villines, T.C.; Shry, E.A.; et al. Computed Tomography Coronary Angiography Versus Stress Myocardial Perfusion Imaging for Risk Stratification in Patients With High Occupational Risk. J. Thorac. Imaging 2012, 27, 40–43. [Google Scholar] [CrossRef]
- D’Agostino, S.R.B.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General Cardiovascular Risk Profile for Use in Primary Care. Circulation 2008, 117, 743–753. [Google Scholar] [CrossRef]
- Wilson, P.W.F.; D’Agostino, R.B.; Levy, D.; Belanger, A.M.; Silbershatz, H.; Kannel, W.B. Prediction of Coronary Heart Disease Using Risk Factor Categories. Circulation 1998, 97, 1837–1847. [Google Scholar] [CrossRef]
- D’Agostino, R.B.; Grundy, S.; Sullivan, L.M.; Wilson, P. For the CHD Risk Prediction Group Validation of the Framingham Coronary Heart Disease Prediction Scores. JAMA 2001, 286, 180–187. [Google Scholar] [CrossRef]
- Rabanal, K.S.; Meyer, H.E.; Pylypchuk, R.; Mehta, S.; Selmer, R.M.; Jackson, R.T. Performance of a Framingham cardiovascular risk model among Indians and Europeans in New Zealand and the role of body mass index and social deprivation. Open Heart 2018, 5, e000821. [Google Scholar] [CrossRef]
- La Torre, G.; Palmeri, V.; Pagano, L.; Nati, G.; Sernia, S.; Mannocci, A. Evaluation of cardiovascular risk profile: A comparative analysis between CUORE algorithm and the Framingham risk scores. Eur. Rev. Med. Pharm. Sci. 2018, 22, 2398–2404. [Google Scholar]
- Diagnosis ADA. Available online: https://www.diabetes.org/a1c/diagnosis (accessed on 17 April 2021).
- Williams, B.; Mancia, G.; Spiering, W.; Rosei, E.A.; Azizi, M.; Burnier, M.; Clement, D.L.; Coca, A.; DeSimone, G.; Dominiczak, A.; et al. 2018 ESC/ESH Guidelines for themanagement of arterial hypertension. Eur. Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; De Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, 1082. [Google Scholar] [CrossRef]
- Labor Standards Law in Taiwan—Laws & Regulations Database of The Republic of China. Available online: https://law.moj.gov.tw/LawClass/LawSingle.aspx?pcode=N0030001&flno=54 (accessed on 18 April 2021).
- Body Mass Index for Adult in Taiwan—Welfare, M.H. Available online: https://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=542&pid=9737 (accessed on 18 April 2021).
- Choi, T.-Y.; Li, D.; Nasir, K.; Zeb, I.; Sourayanezhad, S.; Gupta, M.; Hacioglu, Y.; Mao, S.S.; Budoff, M.J. Differences in Coronary Atherosclerotic Plaque Burden and Composition According to Increasing Age on Computed Tomography Angiography. Acad. Radiol. 2013, 20, 202–208. [Google Scholar] [CrossRef] [PubMed]
- Gurudevan, S.; Garg, P.; Malik, S.; Khattar, R.; Saremi, F.; Hecht, H.; DeMaria, A.; Narula, J. Impaired fasting glucose is associated with increased severity of subclinical coronary artery disease compared to patients with diabetes and normal fasting glucose: Evaluation by coronary computed tomographic angiography. BMJ Open 2016, 6, e005148. [Google Scholar] [CrossRef]
- Im, T.S.; Chun, E.J.; Lee, M.S.; Adla, T.; Kim, J.A.; Choi, S.I. Grade-response relationship between blood pressure and severity of coronary atherosclerosis in asymptomatic adults: Assessment with coronary CT angiography. Int. J. Cardiovasc. Imaging 2014, 30, 105–112. [Google Scholar] [CrossRef]
- Yi, M.; Chun, E.J.; Lee, M.S.; Lee, J.; Choi, S.I. Coronary CT angiography findings based on smoking status: Do ex-smokers and never-smokers share a low probability of developing coronary atherosclerosis? Int. J. Cardiovasc. Imaging 2015, 31, 169–176. [Google Scholar] [CrossRef]
- Kim, J.A.; Chun, E.J.; Lee, M.S.; Kim, K.J.; Choi, S.I. Relationship between amount of cigarette smoking and coronary atherosclerosis on coronary CTA in asymptomatic individuals. Int. J. Cardiovasc. Imaging 2013, 29, 21–28. [Google Scholar] [CrossRef]
- Tay, S.Y.; Chang, P.-Y.; Lao, W.T.; Lin, Y.C.; Chung, Y.-H.; Chan, W.P. The proper use of coronary calcium score and coronary computed tomography angiography for screening asymptomatic patients with cardiovascular risk factors. Sci. Rep. 2017, 7, 1–8. [Google Scholar] [CrossRef]
- Gan, L.; Yang, L.; Yan, G. Predict value of adiponectin for coronary atherosclerosis plaques according to computed tomography angiography in an asymptomatic population. Clin. Imaging 2018, 51, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Miname, M.H.; Ii, M.S.R.; Filho, J.P.; Avila, L.F.; Bortolotto, L.A.; Martinez, L.R.C.; Rochitte, C.E.; Santos, R.D. Evaluation of subclinical atherosclerosis by computed tomography coronary angiography and its association with risk factors in familial hypercholesterolemia. Atherosclerosis 2010, 213, 486–491. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, K.; Matsumoto, T.; Aono, H.; Furukawa, H.; Samukawa, M. Prevalence of subclinical atherosclerosis in asymptomatic patients with low-to-intermediate risk by 64-slice computed tomography. Coron. Artery Dis. 2011, 22, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.J.; Woolf, N.; Rowles, P.M.; Pepper, J. Morphology of the endothelium over atherosclerotic plaques in human coronary arteries. Heart 1988, 60, 459–464. [Google Scholar] [CrossRef]
- Stary, H.C.; Chandler, A.B.; Dinsmore, R.E.; Fuster, V.; Glagov, S.; Insull, W.; Rosenfeld, M.E.; Schwartz, C.J.; Wagner, W.D.; Wissler, R.W. A Definition of Advanced Types of Atherosclerotic Lesions and a Histological Classification of Atherosclerosis. Circulation 1995, 92, 1355–1374. [Google Scholar] [CrossRef]
- Kannel, W.B.; Castelli, W.P.; Gordon, T.; McNamara, P.M. Serum Cholesterol, Lipoproteins, and the Risk of Coronary Heart Disease. Ann. Intern. Med. 1971, 74, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Kjelsberg, M.O. Multiple risk factor intervention trial. JAMA 1982, 248, 1465–1477. [Google Scholar] [CrossRef]
- Lewington, S.; Whitlock, G.; Clarke, R.; Sherliker, P.; Emberson, J.; Halsey, J.; Qizilbash, N.; Peto, R.; Collins, R. Blood cholesterol and vascular mortality by age, sex, and blood pressure: A meta-analysis of individual data from 61 prospective studies with 55 000 vascular deaths. Lancet 2007, 370, 1829–1839. [Google Scholar] [CrossRef] [PubMed]
- Chobanian, A.V. Exacerbation of Atherosclerosis by Hypertension. Arch. Intern. Med. 1996, 156, 1952–1956. [Google Scholar] [CrossRef]
- Rapsomaniki, E.; Timmis, A.; George, J.; Rodriguez, M.P.; Shah, A.D.; Denaxas, S.; White, I.R.; Caulfield, M.J.; Deanfield, J.; Smeeth, L.; et al. Blood pressure and incidence of twelve cardiovascular diseases: Lifetime risks, healthy life-years lost, and age-specific associations in 1·25 million people. Lancet 2014, 383, 1899–1911. [Google Scholar] [CrossRef]
- Murphy, A.O.; Johnson, C.A.; Roth, G.; Forouzanfar, M.H.; Naghavi, M.; Ng, M.; Pogosova, N.; Vos, T.; Murray, C.J.L.; Moran, A.E. Ischaemic heart disease in the former Soviet Union 1990–2015 according to the Global Burden of Disease 2015 Study. Heart 2017, 104, 58–66. [Google Scholar] [CrossRef]
- Wu, Y.-J.; Mar, G.-Y.; Wu, M.-T.; Wu, F.-Z. A LASSO-Derived Risk Model for Subclinical CAC Progression in Asian Population with an Initial Score of Zero. Front. Cardiovasc. Med. 2021, 7, 619798. [Google Scholar] [CrossRef]
- Shen, Y.-W.; Wu, Y.-J.; Hung, Y.-C.; Hsiao, C.-C.; Chan, S.-H.; Mar, G.-Y.; Wu, M.-T.; Wu, F.-Z. Natural course of coronary artery calcium progression in Asian population with an initial score of zero. BMC Cardiovasc. Disord. 2020, 20, 1–10. [Google Scholar] [CrossRef]
- Budoff, M.J.; Hokanson, J.E.; Nasir, K.; Shaw, L.J.; Kinney, G.L.; Chow, D.; DeMoss, D.; Nuguri, V.; Nabavi, V.; Ratakonda, R.; et al. Progression of Coronary Artery Calcium Predicts All-Cause Mortality. JACC Cardiovasc. Imaging 2010, 3, 1229–1236. [Google Scholar] [CrossRef]
- ESC Guidelines on Diabetes 2019, Pre-diabetes and Cardiovascular Diseases Developed in Collaboration with the EASD—American College of Cardiology. Available online: https://www.acc.org/latest-in-cardiology/articles/2020/03/09/13/11/2019-esc-guidelines-on-diabetes-pre-diabetes-and-cvd (accessed on 10 May 2021).
- Plank, F.; Friedrich, G.; Dichtl, W.; Klauser, A.; Jaschke, W.; Franz, W.-M.; Feuchtner, G. The diagnostic and prognostic value of coronary CT angiography in asymptomatic high-risk patients: A cohort study. Open Heart 2014, 1, e000096. [Google Scholar] [CrossRef]
- Jin, K.N.; Chun, E.J.; Lee, C.-H.; Kim, J.A.; Lee, M.S.; Choi, S.I. Subclinical coronary atherosclerosis in young adults: Prevalence, characteristics, predictors with coronary computed tomography angiography. Int. J. Cardiovasc. Imaging 2012, 28, 93–100. [Google Scholar] [CrossRef]
- Marsh, R.W. Predicting cardiovascular events using three stage Discriminant Function is much more accurate than Framingham or QRISK. Eur. J. Epidemiol. 2011, 26, 915–918. [Google Scholar] [CrossRef] [PubMed]
| Factors | n = 309 (%) |
|---|---|
| Male/female | 184 (59.5)/125 (40.5) |
| Age (y/o) (mean ± S.D.) | 52.5 ± 5.6 |
| BMI (kg/m2) (mean ± S.D.) | 26.7 ± 3.9 |
| eGFR (mL/min/1.73 m2) (mean ± S.D.) | 78.73 ± 13.99 |
| Diabetes mellitus (+/−) | 45 (14.6)/264 (85.4) |
| Hypertension (+/−) | 119 (38.5)/190 (61.5) |
| Hyperlipidemia (+/−) | 101 (32.7)/208 (67.3) |
| Smoking (current/ex/never -smoker) | 21 (6.8)/11 (3.6)/277 (89.6) |
| Alcohol (+/−) | 68 (22.0)/241 (78.0) |
| HBV or HCV (+/−) | 31 (10.0)/278 (90.0) |
| Heart disease (+/−) | 16 (5.2)/293 (94.8) |
| CVA (+/−) | 5 (1.6)/304 (98.4) |
| 10-year risk of myocardial infarction or death rate | |
| Intermediate-risk level (10–20%) | 252 (81.6) |
| High-risk level (>20%) | 57 (18.4) |
| CAD-RADS | |
| 0 | 117 (37.9) |
| 1–2 | 161 (52.1) |
| 3–5 | 31 (10.0) |
| Risk Factor | Total No. of Patients (%) | No. of Patients with Significant Coronary Stenosis | p | OR (95% CI) |
|---|---|---|---|---|
| Sex | 0.329 | 1.482 (0.672–3.264) | ||
| male | 184 (59.5) | 21 | ||
| female | 125 (40.5) | 10 | ||
| Age | 0.005 ** | 2.954 (1.377–6.340) | ||
| ≥55 | 116 (37.5) | 19 | ||
| <55 | 193 (62.5) | 12 | ||
| BMI | 0.987 | 0.994 (0.468–2.108) | ||
| ≥27 | 130 (42.1) | 13 | ||
| <27 | 179 (57.9) | 18 | ||
| Hypertension | 0.008 ** | 2.818 (1.314–6.045) | ||
| Yes | 119 (38.5) | 19 | ||
| No | 190 (61.5) | 12 | ||
| Hyperlipidemia | 0.007 ** | 2.804 (1.322–5.950) | ||
| Yes | 101 (32.7) | 17 | ||
| No | 208 (67.3) | 14 | ||
| Diabetes | 0.428 | 1.471 (0.567–3.815) | ||
| Yes | 45 (14.6) | 6 | ||
| No | 264 (85.4) | 25 | ||
| Smoke | 0.508 0.943 | 1.543 (0.427–5.579) 0.926 (0.114–7.513) | ||
| Current smoker | 21 (6.8) | 3 | ||
| Ex-smoker | 11 (3.6) | 1 | ||
| Never smoker | 277 (89.6) | 27 | ||
| Alcohol | 0.408 | 0.656 (0.242–1.779) | ||
| Yes | 68 (22.0) | 5 | ||
| No | 241 (78.0) | 26 | ||
| Framingham Risk Score | 0.041 * | 2.340 (1.035–5.291) | ||
| Intermediate-risk level (10–20%) | 252 (81.6) | 21 | ||
| High-risk level (>20%) | 57 (18.4) | 10 |
| Risk Factor | Coefficient | SE | OR (95% CI) | p |
|---|---|---|---|---|
| Age ≥ 55 (y/o) | 0.999 | 0.400 | 2.716 (1.239–5.954) | 0.013 * |
| Hypertension | 0.827 | 0.401 | 2.287 (1.042–5.019) | 0.039 * |
| Hyperlipidemia | 0.969 | 0.395 | 2.635 (1.215–5.713) | 0.014 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, P.-Y.; Chen, R.-Y.; Wu, F.-Z.; Mar, G.-Y.; Wu, M.-T.; Wang, F.-W. Use of Coronary Computed Tomography Angiography to Screen Hospital Employees with Cardiovascular Risk Factors. Int. J. Environ. Res. Public Health 2021, 18, 5462. https://doi.org/10.3390/ijerph18105462
Li P-Y, Chen R-Y, Wu F-Z, Mar G-Y, Wu M-T, Wang F-W. Use of Coronary Computed Tomography Angiography to Screen Hospital Employees with Cardiovascular Risk Factors. International Journal of Environmental Research and Public Health. 2021; 18(10):5462. https://doi.org/10.3390/ijerph18105462
Chicago/Turabian StyleLi, Po-Yi, Ru-Yih Chen, Fu-Zong Wu, Guang-Yuan Mar, Ming-Ting Wu, and Fu-Wei Wang. 2021. "Use of Coronary Computed Tomography Angiography to Screen Hospital Employees with Cardiovascular Risk Factors" International Journal of Environmental Research and Public Health 18, no. 10: 5462. https://doi.org/10.3390/ijerph18105462
APA StyleLi, P.-Y., Chen, R.-Y., Wu, F.-Z., Mar, G.-Y., Wu, M.-T., & Wang, F.-W. (2021). Use of Coronary Computed Tomography Angiography to Screen Hospital Employees with Cardiovascular Risk Factors. International Journal of Environmental Research and Public Health, 18(10), 5462. https://doi.org/10.3390/ijerph18105462







