Effects of a Tai Chi-Based Stroke Rehabilitation Program on Symptom Clusters, Physical and Cognitive Functions, and Quality of Life: A Randomized Feasibility Study
Abstract
1. Introduction
2. Materials and Methods
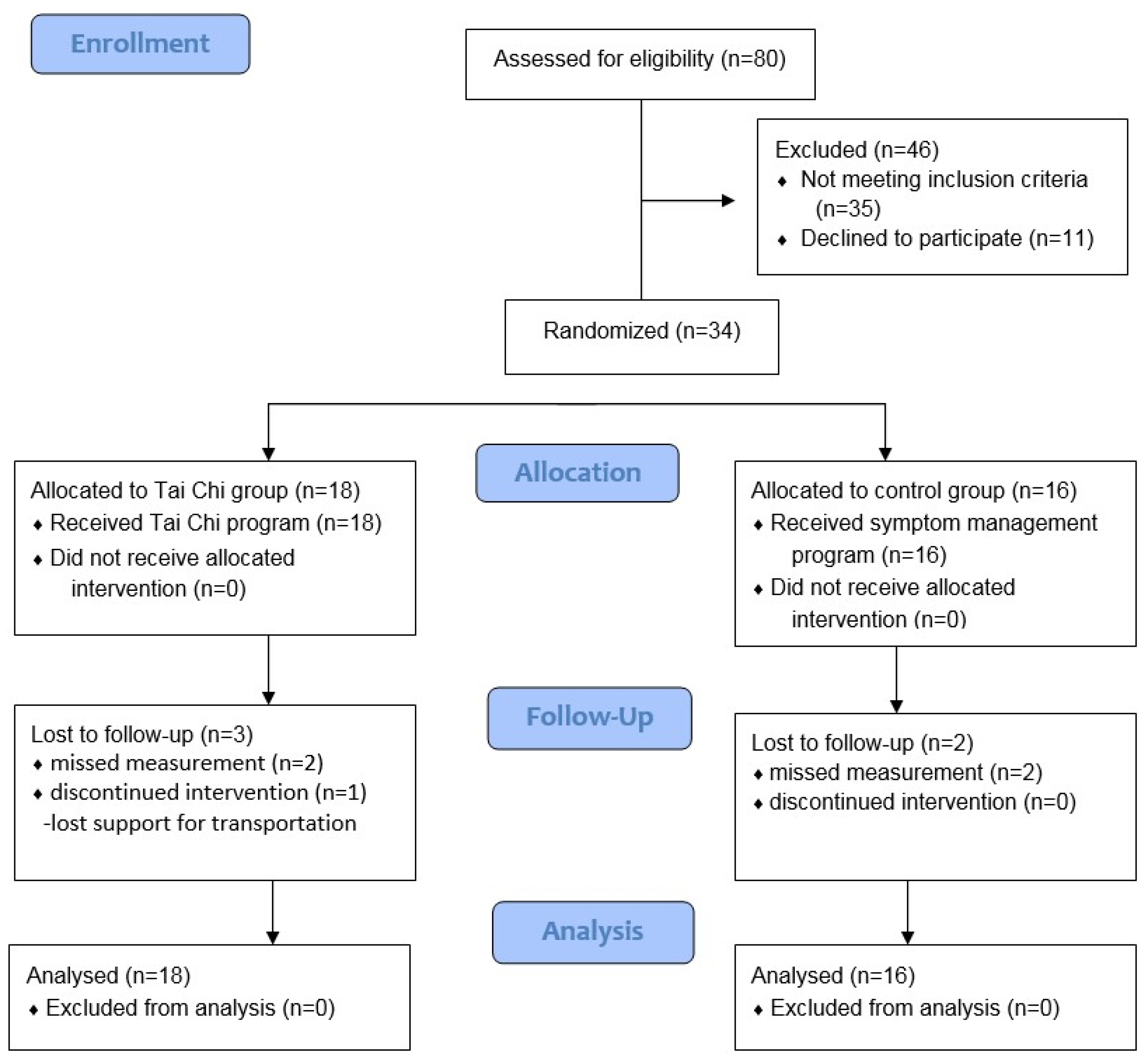
2.1. Study Design
2.2. Participants
2.3. Sample Size
2.4. Randomization and Masking
2.5. Treatments
2.6. Feasibility Monitoring
2.7. Measures
2.7.1. Cognitive Function
2.7.2. Muscle Strength
2.7.3. Balance
2.7.4. Ambulation and Motor Function
2.7.5. Stroke-Specific Quality of Life
2.7.6. Stroke-Symptom Clusters
2.8. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Homogeneity Tests at Baseline
3.3. Treatment Effects on Stroke-Symptom Clusters
3.4. Treatment Effects on Muscle Strength and Physical and Cognitive Functions
3.5. Treatment Effects on SS-QOL
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Stroke, Cerebrovascular Accident. Available online: https://www.who.int/cardiovascular_diseases/resources/atlas/en/ (accessed on 20 March 2020).
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; De Ferranti, S.; Després, J.-P.; Fullerton, H.J.; et al. Executive Summary: Heart Disease and Stroke Statistics—2016 Update. Circulation 2016, 133, 447–454. [Google Scholar] [CrossRef] [PubMed]
- Langhorne, P.; Bernhardt, J.; Kwakkel, G. Stroke rehabilitation. Lancet 2011, 377, 1693–1702. [Google Scholar] [CrossRef]
- Lan, C.; Lai, J.-S.; Chen, S.-Y. Tai Chi Chuan. Sports Med. 2002, 32, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Layne, C.; Lowder, T.; Liu, J. A Review Focused on the Psychological Effectiveness of Tai Chi on Different Populations. Evid.-Based Complement. Altern. Med. 2011, 2012, 1–9. [Google Scholar] [CrossRef]
- Ni, X.; Liu, S.; Lu, F.; Shi, X.; Guo, X. Efficacy and Safety of Tai Chi for Parkinson’s Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS ONE 2014, 9, e99377. [Google Scholar] [CrossRef]
- Taylor-Piliae, R.E.; Hoke, T.M.; Hepworth, J.T.; Latt, L.D.; Najafi, B.; Coull, B.M. Effect of Tai Chi on Physical Function, Fall Rates and Quality of Life Among Older Stroke Survivors. Arch. Phys. Med. Rehabil. 2014, 95, 816–824. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ning, Y.; Liu, H.; Zhou, L.; Zou, Y.; Li, Z. Current trends in tai chi for stroke rehabilitation. J. Tradit. Chin. Med. Sci. 2015, 2, 135–139. [Google Scholar] [CrossRef][Green Version]
- Yang, Y.; Li, X.-Y.; Gong, L.; Zhu, Y.-L.; Hao, Y.-L. Tai Chi for Improvement of Motor Function, Balance and Gait in Parkinson’s Disease: A Systematic Review and Meta-Analysis. PLoS ONE 2014, 9, e102942. [Google Scholar] [CrossRef]
- Logghe, I.H.; Verhagen, A.P.; Rademaker, A.C.; Bierma-Zeinstra, S.M.; van Rossum, E.; Faber, M.J.; Koes, B.W. The effects of Tai Chi on fall prevention, fear of falling and balance in older people: A meta-analysis. Prev. Med. 2010, 51, 222–227. [Google Scholar] [CrossRef]
- Wang, F.; Lee, E.-K.O.; Wu, T.; Benson, H.; Fricchione, G.; Wang, W.; Yeung, A.S. The Effects of Tai Chi on Depression, Anxiety, and Psychological Well-Being: A Systematic Review and Meta-Analysis. Int. J. Behav. Med. 2013, 21, 605–617. [Google Scholar] [CrossRef]
- Wang, C.; Bannuru, R.; Ramel, J.; Kupelnick, B.; Scott, T.; Schmid, C.H. Tai Chi on psychological well-being: Systematic review and meta-analysis. BMC Complement. Altern. Med. 2010, 10, 23. [Google Scholar] [CrossRef]
- Hwang, I.; Song, R.; Ahn, S.; Lee, M.-A.; Wayne, P.M.; Sohn, M.K. Exploring the Adaptability of Tai Chi to Stroke Rehabilitation. Rehabil. Nurs. 2019, 44, 221–229. [Google Scholar] [CrossRef]
- Hsu, C.-Y.; Moyle, W.; Cooke, M.; Jones, C.; Hsu, C.-Y. Seated Tai Chi versus usual activities in older people using wheelchairs: A randomized controlled trial. Complement. Ther. Med. 2016, 24, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Shem, K.; Karasik, D.; Carufel, P.; Kao, M.-C.; Zheng, P. Seated Tai Chi to alleviate pain and improve quality of life in individuals with spinal cord disorder. J. Spinal Cord Med. 2016, 39, 353–358. [Google Scholar] [CrossRef] [PubMed]
- Taylor-Piliae, R.E.; Coull, B.M. Community-based Yang-style Tai Chi is safe and feasible in chronic stroke: A pilot study. Clin. Rehabil. 2011, 26, 121–131. [Google Scholar] [CrossRef] [PubMed]
- Wayne, P.M.; Bs, J.N.W.; Taylor-Piliae, R.E.; Wells, R.E.; Papp, K.V.; Donovan, N.J.; Yeh, G.Y. Effect of Tai Chi on Cognitive Performance in Older Adults: Systematic Review and Meta-Analysis. J. Am. Geriatr. Soc. 2014, 62, 25–39. [Google Scholar] [CrossRef]
- Taylor-Piliae, R.E.; Haskell, W.L. Tai Chi Exercise and Stroke Rehabilitation. Top. Stroke Rehabil. 2007, 14, 9–22. [Google Scholar] [CrossRef]
- Chan, W.N.; Tsang, W.W.-N. The effect of Tai Chi training on the dual-tasking performance of stroke survivors: A randomized controlled trial. Clin. Rehabil. 2018, 32, 1076–1085. [Google Scholar] [CrossRef]
- Xie, G.; Rao, T.; Lin, L.; Lin, Z.; Xiao, T.; Yang, M.; Xu, Y.; Fan, J.; Lin, S.; Wu, J.; et al. Effects of Tai Chi Yunshou exercise on community-based stroke patients: A cluster randomized controlled trial. Eur. Rev. Aging Phys. Act. 2018, 15, 1–12. [Google Scholar] [CrossRef]
- Lee, J.-Y.; Lee, D.W.; Cho, S.-J.; Na, D.L.; Jeon, H.J.; Kim, S.-K.; Lee, Y.R.; Youn, J.-H.; Kwon, M.; Lee, J.-H.; et al. Brief Screening for Mild Cognitive Impairment in Elderly Outpatient Clinic: Validation of the Korean Version of the Montreal Cognitive Assessment. J. Geriatr. Psychiatry Neurol. 2008, 21, 104–110. [Google Scholar] [CrossRef]
- Kang, Y.; Na, D.L.; Hahn, S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J. Korean Neurol. Assoc. 1997, 15, 300–308. [Google Scholar]
- Berg, K.O.; Wood-Dauphinee, S.L.; Williams, J.I.; Maki, B. Measuring balance in the elderly: Validation of an instrument. Can. J. Public Heal. 1992, 83, 7–11. [Google Scholar]
- Lee, J.J.; Lee, H.J.; Park, J.H.; Han, E.Y.; Kim, M.J.; Jung, H.Y. The Korean Version of Berg Balance Scale as an index of activi-ty related to ambulation in subjects with stroke. J. Korean Acad. Rehabil. Med. 2007, 31, 400–403. [Google Scholar]
- Verheyden, G.; Nieuwboer, A.; Mertin, J.; Preger, R.; Kiekens, C.; De Weerdt, W. The Trunk Impairment Scale: A new tool to measure motor impairment of the trunk after stroke. Clin. Rehabil. 2004, 18, 326–334. [Google Scholar] [CrossRef] [PubMed]
- Viosca, E.; Martínez, J.L.; Almagro, P.L.; Gracia, A.; González, C. Proposal and Validation of a New Functional Ambulation Classification Scale for Clinical Use. Arch. Phys. Med. Rehabil. 2005, 86, 1234–1238. [Google Scholar] [CrossRef]
- Banks, J.L.; Marotta, C.A. Outcomes Validity and Reliability of the Modified Rankin Scale: Implications for Stroke Clinical Trials. Stroke 2007, 38, 1091–1096. [Google Scholar] [CrossRef]
- Jung, H.Y.; Park, B.K.; Shin, H.S.; Kang, Y.K.; Pyun, S.B.; Paik, N.J.; Kim, S.H.; Kim, T.H.; Han, T.R. Development of the Korean Version of Modified Barthel Index (K-MBI): Multi-center Study for Subjects with Stroke. J. Korean Acad. Rehabil. Med. 2007, 31, 283–297. [Google Scholar]
- Williams, L.S.; Weinberger, M.; Harris, L.E.; Clark, D.O.; Biller, J. Development of a Stroke-Specific Quality of Life Scale. Stroke 1999, 30, 1362–1369. [Google Scholar] [CrossRef]
- Song, R.; Ahn, S.; Jang, T.; Oh, J.; Sohn, M.K. Development and validation of the stroke symptom cluster scale for Korean adults recovering after a stroke. In Proceedings of the MNRS 41st Annual Research Conference, Midwest Nursing Research Conference Proceedings, Minneapolis, MN, USA, 6–9 April 2017. [Google Scholar]
- González-Fernández, M.; Ottenstein, L.; Atanelov, L.; Christian, A.B. Dysphagia after stroke: An overview. Curr. Phys. Med. Rehabil. Rep. 2013, 1, 187–196. [Google Scholar] [CrossRef]
- Shaker, R.; Easterling, C.; Kern, M.; Nitschke, T.; Massey, B.; Daniels, S.; Grande, B.; Kazandjian, M.; Dikeman, K. Rehabilitation of swallowing by exercise in tube-fed patients with pharyngeal dysphagia secondary to abnormal UES opening. Gastroenterology 2002, 122, 1314–1321. [Google Scholar] [CrossRef]
- Ding, M. Tai Chi for Stroke Rehabilitation. Am. J. Phys. Med. Rehabil. 2012, 91, 1091–1096. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Cruz, C.; Martínez-Núñez, J.M.; Perez, M.E.; Kravzov-Jinich, J.; Ríos-Castañeda, C.; Altagracia-Martinez, M. Evaluation of the Stroke-Specific Quality-of-Life (SSQOL) Scale in Mexico: A Preliminary Approach. Value Health Reg. Issues 2013, 2, 392–397. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Penn, I.-W.; Sung, W.-H.; Lin, C.-H.; Chuang, E.; Chuang, T.-Y.; Lin, P.-H. Effects of individualized Tai-Chi on balance and lower-limb strength in older adults. BMC Geriatr. 2019, 19, 235. [Google Scholar] [CrossRef] [PubMed]
- Tseng, S.-C.; Liu, W.; Finley, M.; McQuade, K. Muscle activation profiles about the knee during Tai-Chi stepping movement compared to the normal gait step. J. Electromyogr. Kinesiol. 2007, 17, 372–380. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.-L.; Guo, J.-B.; Liu, M.-S.; Binglin, C.; Zou, J.; Chen, X.; Zhang, L.-L.; Yue, Y.-S.; Wang, X.-Q. Effect of Traditional Chinese Exercise on Gait and Balance for Stroke: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0135932. [Google Scholar] [CrossRef]
- Gatts, S.K.; Woollacott, M.H. How Tai Chi improves balance: Biomechanics of recovery to a walking slip in impaired seniors. Gait Posture 2007, 25, 205–214. [Google Scholar] [CrossRef]
- Lim, K.-B.; Kim, J.; Lee, H.-J.; Yoo, J.; You, E.-C.; Kang, J. Correlation Between Montreal Cognitive Assessment and Functional Outcome in Subacute Stroke Patients with Cognitive Dysfunction. Ann. Rehabil. Med. 2018, 42, 26–34. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Wang, Y.; Burgess, E.; Wu, J. The effects of Tai Chi exercise on cognitive function in older adults: A meta-analysis. J. Sport Health Sci. 2013. [Google Scholar] [CrossRef]
| Characteristics | Control (n = 16) n(%) or Mean ± SD | Tai Chi (n = 18) n(%) or Mean ± SD | t/χ2 | p | |
|---|---|---|---|---|---|
| Age, years | 57.18 ± 10.65 | 58.72 ± 17.13 | –0.91 | 0.367 | |
| Duration of stroke, months | 10.94 ± 8.50 | 7.58 ± 5.98 | 1.32 | 0.200 | |
| Sex | Male | 11 (68.8) | 10 (55.6) | 0.62 | 0.429 |
| Female | 5 (31.3) | 8 (44.4) | |||
| Education | ≤Primary school (grade 6th) | 3 (18.8) | 4 (22.2) | 1.32 | 0.725 |
| Middle school (grade 7th~9th) | 2 (12.5) | 2 (11.1) | |||
| High school (grade 10th~12th) | 8 (50.0) | 6 (33.3) | |||
| ≥College | 3 (18.8) | 6 (33.3) | |||
| Marital status | Married | 11 (68.8) | 15 (83.3) | 3.71 | 0.447 |
| Other | 5 (31.2) | 3 (16.7) | |||
| Employment | Yes | 4 (25.0) | 3 (16.7) | 0.36 | 0.549 |
| No | 12 (75.0) | 15 (83.3) | |||
| Income, month | <US $2000 | 11 (68.8) | 8 (47.1) | 6.22 | 0.101 |
| US $2000–4000 | 4 (25.0) | 3 (17.6) | |||
| >US $4000 | 1 ( 6.3) | 6 (35.3) | |||
| Diagnosis | Infarction | 8 (50.0) | 12 (66.7) | 0.97 | 0.324 |
| Hemorrhage | 8 (50.0) | 6 (33.3) | |||
| Activities of daily living | Independent | 12 (75.0) | 12 (66.7) | 3.90 | 0.143 |
| Assisted/dependent | 4 (25.0) | 6 (33.3) | |||
| Comorbidity * | Hypertension | 6 (37.5) | 11 (61.1) | 1.89 | 0.169 |
| Cardiovascular disease | 3 (18.8) | 2 (11.1) | 0.39 | 0.648 | |
| Diabetes | 6 (37.5) | 5 (27.8) | 0.37 | 0.545 | |
| Neurological disease | 8 (50.0) | 10 (55.6) | 0.11 | 0.746 | |
| Other | 4 (25.0) | 6 (33.3) | 1.72 | 0.340 | |
| Control (n = 16) N (%) or Mean ± SD | Tai Chi (n = 18) N (%) or Mean ± SD | t | p | ||
|---|---|---|---|---|---|
| Symptom cluster | Mobility | 31.38 ± 9.49 | 28.33 ± 8.29 | 1.00 | 0.326 |
| Sensory | 13.06 ± 3.51 | 11.78 ± 2.82 | 1.18 | 0.246 | |
| Cognition | 17.37 ± 5.89 | 14.61 ± 3.39 | 1.69 | 0.099 | |
| Communication | 20.94 ± 7.94 | 19.61 ± 5.21 | 0.58 | 0.565 | |
| Mood | 27.25 ± 8.70 | 22.33 ± 5.59 | 1.93 | 0.065 | |
| Swallowing | 5.81 ± 1.87 | 5.72 ± 1.71 | 0.15 | 0.884 | |
| Muscle strength | Flexor-I | 125.43 ± 37.71 | 118.93 ± 37.39 | 0.50 | 0.618 |
| Extensor-I | 54.30 ± 20.24 | 56.11 ± 20.07 | –0.26 | 0.795 | |
| Physical function | BBS | 48.75 ± 6.03 | 48.89 ± 6.64 | –0.61 | 0.548 |
| TIS | 16.31 ± 3.32 | 17.67 ± 3.61 | –1.46 | 0.154 | |
| FAC | 3.88 ± 0.62 | 3.72 ± 0.67 | –0.32 | 0.750 | |
| MRS | 1.69 ± 0.79 | 1.78 ± 0.65 | –0.37 | 0.717 | |
| K-MBI | 87.88 ± 10.89 | 87.67 ± 9.93 | 0.06 | 0.954 | |
| Cognitive function | K-MOCA | 24.00 ± 4.56 | 24.06 ± 3.54 | –0.04 | 0.968 |
| K-MMSE | 26.25 ± 4.09 | 26.61 ± 3.90 | –0.26 | 0.794 | |
| SS-QOL | Fatigue | 9.06 ± 3.21 | 10.28 ± 3.01 | –1.14 | 0.263 |
| Family support | 9.18 ± 2.95 | 10.72 ± 2.59 | 1.62 | 0.116 | |
| Language ability | 17.69 ± 5.31 | 18.17 ± 6.15 | –0.24 | 0.811 | |
| Movement ability | 18.25 ± 5.67 | 19.06 ± 4.21 | –0.47 | 0.639 | |
| Emotion | 15.75 ± 5.34 | 17.56 ± 4.37 | –0.28 | 0.781 | |
| Social role | 13.94 ± 5.20 | 13.56 ± 4.13 | 0.24 | 0.813 | |
| Personality | 9.31 ± 4.24 | 9.67 ± 3.65 | –0.26 | 0.795 | |
| Thought processes | 8.69 ± 3.50 | 9.22 ± 2.58 | –0.51 | 0.613 | |
| Self-care | 13.88 ± 3.61 | 12.11 ± 2.81 | 1.60 | 0.119 | |
| Outcome | Baseline | 3 Months | 6 Months | F | p | ||
|---|---|---|---|---|---|---|---|
| Mobility | Tai Chi | 28.33 ± 8.29 | 26.39 ± 8.08 | 26.22 ± 7.87 | T | 5.72 | 0.011 |
| Control | 31.38 ± 9.49 | 28.75 ± 8.19 | 30.13 ± 7.75 | G | 1.29 | 0.264 | |
| T × G | 0.61 | 0.504 | |||||
| Sensory | Tai Chi | 11.78 ± 2.82 | 11.28 ± 2.52 | 10.56 ± 2.25 | T | 2.98 | 0.058 |
| Control | 13.06 ± 3.51 | 12.88 ± 3.03 | 12.31 ± 2.98 | G | 3.19 | 0.083 | |
| T × G | 0.17 | 0.783 | |||||
| Cognition | Tai Chi | 14.61 ± 3.39 | 14.05 ± 3.81 | 12.22 ± 2.83 | T | 8.35 | 0.001 |
| Control | 17.37 ± 5.89 | 15.87 ± 5.50 | 15.31 ± 4.22 | G | 3.54 | 0.069 | |
| T × G | 0.73 | 0.482 | |||||
| Communication | Tai Chi | 19.61 ± 5.21 | 17.83 ± 4.37 | 16.50 ± 4.23 | T | 4.57 | 0.014 |
| Control | 20.94 ± 7.94 | 21.31 ± 7.91 | 20.19 ± 6.49 | G | 2.07 | 0.016 | |
| T × G | 2.04 | 0.138 | |||||
| Mood | Tai Chi | 22.33 ± 5.59 | 21.94 ± 7.23 | 20.11 ± 5.49 | T | 2.60 | 0.097 |
| Control | 27.25 ± 8.70 | 25.69 ± 8.87 | 25.38 ± 8.42 | G | 3.95 | 0.056 | |
| T × G | 0.39 | 0.624 | |||||
| Swallowing | Tai Chi | 5.72 ± 1.71 | 5.06 ± 1.39 | 5.39 ± 1.42 | T | 1.61 | 0.206 |
| Control | 5.81 ± 1.87 | 7.31 ± 2.82 | 6.19 ± 1.64 | G | 3.50 | 0.070 | |
| T × G | 8.96 | 0.001 |
| Outcome | Baseline | 3 Months | 6 Months | F | p | ||
|---|---|---|---|---|---|---|---|
| Flexor-I | Tai Chi | 118.93 ± 37.39 | 129.33 ± 36.17 | 137.70 ± 33.32 | T | 0.94 | 0.377 |
| Control | 125.43 ± 37.71 | 119.51 ± 38.07 | 116.00 ± 31.56 | G | 0.51 | 0.479 | |
| T × G | 8.61 | 0.002 | |||||
| Extensor-I | Tai Chi | 56.12 ± 20.08 | 59.84 ± 18.57 | 59.80 ± 20.73 | T | 1.37 | 0.260 |
| Control | 54.31 ± 20.24 | 58.97 ± 23.02 | 55.92 ± 19.77 | G | 0.12 | 0.733 | |
| T × G | 0.18 | 0.782 | |||||
| BBS | Tai Chi | 48.89 ± 6.64 | 51.33 ± 5.77 | 53.59 ± 7.64 | T | 35.31 | <0.001 |
| Control | 48.75 ± 6.03 | 50.06 ± 5.93 | 52.25 ± 3.61 | G | 0.18 | 0.677 | |
| T × G | 0.85 | 0.434 | |||||
| TIS | Tai Chi | 17.67 ± 3.61 | 19.33 ± 3.18 | 20.72 ± 2.89 | T | 44.18 | <0.001 |
| Control | 16.31 ± 3.32 | 18.50 ± 3.10 | 19.25 ± 3.34 | G | 1.35 | 0.255 | |
| T × G | 0.55 | 0.556 | |||||
| FAC | Tai Chi | 3.72 ± 0.67 | 3.94 ± 0.73 | 4.22 ± 0.55 | T | 7.03 | 0.002 |
| Control | 3.88 ± 0.62 | 3.81 ± 0.54 | 3.88 ± 0.62 | G | 0.30 | 0.590 | |
| T × G | 6.78 | 0.002 | |||||
| MRS | Tai Chi | 1.78 ± 0.65 | 1.67 ± 0.59 | 1.56 ± 0.78 | T | 0.25 | 0.782 |
| Control | 1.69 ± 0.79 | 1.81 ± 0.75 | 1.81 ± 0.83 | G | 0.20 | 0.657 | |
| T × G | 2.12 | 0.129 | |||||
| K-MBI | Tai Chi | 87.67 ± 9.93 | 89.50 ± 8.35 | 92.78 ± 7.95 | T | 14.21 | <0.001 |
| Control | 87.88 ± 10.89 | 86.13 ± 13.09 | 89.88 ± 10.61 | G | 0.36 | 0.555 | |
| T × G | 3.23 | 0.046 | |||||
| K-MOCA | Tai Chi | 24.06 ± 3.54 | 25.33 ± 4.09 | 26.67 ± 3.25 | T | 3.62 | 0.044 |
| Control | 24.00 ± 4.56 | 23.69 ± 6.31 | 23.56 ± 5.33 | G | 1.14 | 0.294 | |
| T × G | 7.09 | 0.004 | |||||
| K-MMSE | Tai Chi | 26.61 ± 3.90 | 27.11 ± 3.38 | 28.06 ± 2.98 | T | 0.98 | 0.381 |
| Control | 26.25 ± 4.09 | 25.69 ± 4.60 | 25.63 ± 3.76 | G | 1.29 | 0.265 | |
| T × G | 4.33 | 0.017 | |||||
| Outcome | Baseline | 3 Months | 6 Months | F | p | ||
|---|---|---|---|---|---|---|---|
| Energy | Tai Chi | 10.28 ± 3.01 | 9.56 ± 2.85 | 9.00 ± 2.28 | T | 2.11 | 0.130 |
| Control | 9.06 ± 3.21 | 10.00 ± 3.08 | 9.00 ± 2.92 | G | 0.09 | 0.771 | |
| T × G | 2.19 | 0.120 | |||||
| Family roles | Tai Chi | 10.72 ± 2.59 | 10.44 ± 3.24 | 10.22 ± 3.42 | T | 0.03 | 0.972 |
| Control | 9.19 ± 2.95 | 9.56 ± 3.10 | 9.88 ± 3.05 | G | 0.93 | 0.341 | |
| T × G | 1.16 | 0.321 | |||||
| Language | Tai Chi | 18.17 ± 6.15 | 19.72 ± 3.64 | 18.67 ± 4.46 | T | 0.54 | 0.585 |
| Control | 17.69 ± 5.31 | 17.25 ± 5.78 | 16.69 ± 4.67 | G | 1.24 | 0.274 | |
| T × G | 0.85 | 0.418 | |||||
| Mobility | Tai Chi | 19.06 ± 4.21 | 21.89 ± 4.56 | 20.72 ± 4.97 | T | 2.80 | 0.079 |
| Control | 18.25 ± 5.67 | 18.81 ± 6.31 | 17.38 ± 6.41 | G | 2.19 | 0.149 | |
| T × G | 1.73 | 0.191 | |||||
| Mood | Tai Chi | 16.22 ± 4.51 | 17.56 ± 4.37 | 17.78 ± 4.70 | T | 0.54 | 0.583 |
| Control | 15.75 ± 5.34 | 15.69 ± 3.63 | 14.69 ± 3.94 | G | 1.78 | 0.191 | |
| T × G | 2.27 | 0.123 | |||||
| Social roles | Tai Chi | 13.56 ± 4.13 | 14.28 ± 4.04 | 16.11 ± 5.09 | T | 3.01 | 0.056 |
| Control | 13.94 ± 5.20 | 14.63 ± 5.51 | 15.19 ± 4.13 | G | 0.002 | 0.962 | |
| T × G | 0.45 | 0.617 | |||||
| Personality | Tai Chi | 9.67 ± 3.65 | 9.89 ± 3.01 | 11.17 ± 3.24 | T | 5.97 | 0.004 |
| Control | 9.31 ± 4.24 | 9.69 ± 3.96 | 10.38 ± 3.38 | G | 0.15 | 0.698 | |
| T × G | 0.31 | 0.733 | |||||
| Thinking | Tai Chi | 9.22 ± 2.58 | 10.44 ± 2.87 | 11.33 ± 2.74 | T | 7.93 | 0.001 |
| Control | 8.69 ± 3.50 | 9.38 ± 2.47 | 9.06 ± 2.64 | G | 2.10 | 0.157 | |
| T × G | 3.70 | 0.030 | |||||
| Self-care | Tai Chi | 12.11 ± 2.81 | 12.56 ± 3.15 | 18.78 ± 5.06 | T | 52.00 | <0.001 |
| Control | 13.88 ± 3.61 | 12.06 ± 3.62 | 16.00 ± 3.93 | G | 0.20 | 0.661 | |
| T × G | 8.82 | 0.001 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, R.; Park, M.; Jang, T.; Oh, J.; Sohn, M.K. Effects of a Tai Chi-Based Stroke Rehabilitation Program on Symptom Clusters, Physical and Cognitive Functions, and Quality of Life: A Randomized Feasibility Study. Int. J. Environ. Res. Public Health 2021, 18, 5453. https://doi.org/10.3390/ijerph18105453
Song R, Park M, Jang T, Oh J, Sohn MK. Effects of a Tai Chi-Based Stroke Rehabilitation Program on Symptom Clusters, Physical and Cognitive Functions, and Quality of Life: A Randomized Feasibility Study. International Journal of Environmental Research and Public Health. 2021; 18(10):5453. https://doi.org/10.3390/ijerph18105453
Chicago/Turabian StyleSong, Rhayun, Moonkyoung Park, Taejeong Jang, Jiwon Oh, and Min Kyun Sohn. 2021. "Effects of a Tai Chi-Based Stroke Rehabilitation Program on Symptom Clusters, Physical and Cognitive Functions, and Quality of Life: A Randomized Feasibility Study" International Journal of Environmental Research and Public Health 18, no. 10: 5453. https://doi.org/10.3390/ijerph18105453
APA StyleSong, R., Park, M., Jang, T., Oh, J., & Sohn, M. K. (2021). Effects of a Tai Chi-Based Stroke Rehabilitation Program on Symptom Clusters, Physical and Cognitive Functions, and Quality of Life: A Randomized Feasibility Study. International Journal of Environmental Research and Public Health, 18(10), 5453. https://doi.org/10.3390/ijerph18105453






