A Mental Health Drop-In Centre Offering Brief Transdiagnostic Psychological Assessment and Treatment in a Paediatric Hospital Setting: A One-Year Descriptive Study
Abstract
1. Introduction
2. Methods
2.1. Design
2.2. Participants
2.3. Ethics
2.4. Procedure
2.5. The Booth
2.6. Recruitment
2.7. Intervention
2.7.1. Early Identification
2.7.2. Initial Assessment
2.7.3. Triage
2.7.4. Brief Intervention
2.7.5. Training and Supervision of Volunteers and Staff
2.8. Measures
2.8.1. Assessment of Interest
2.8.2. Participant Demographics, Symptom Profiles and Interventions Allocated to
2.8.3. Child Mental Health Measures
2.8.4. Parent Mental Health Measures (Self-Report)
2.9. Analyses
3. Results
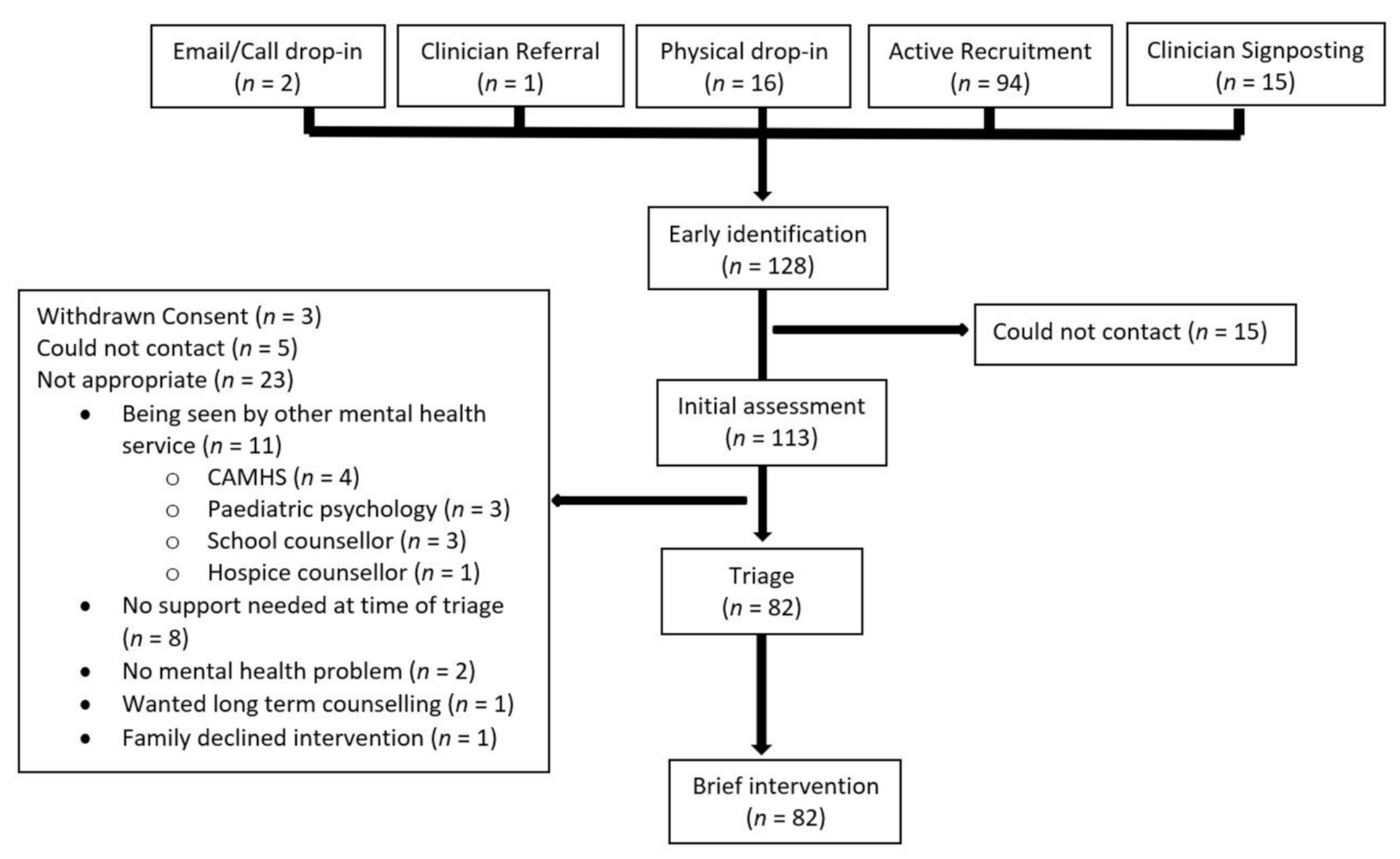
3.1. Early Identification
3.2. Initial Assessment
3.3. Triage
3.4. Brief Intervention
4. Discussion
4.1. Early Identification and Initial Assessment
4.2. Triage and Brief Intervention
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dalgleish, T.; Black, M.; Johnston, D.; Bevan, A. Transdiagnostic approaches to mental health problems: Current status and future directions. J. Consult. Clin. Psychol. 2020, 88, 179–195. [Google Scholar] [CrossRef] [PubMed]
- McEvoy, P.M.; Nathan, P.; Norton, P.J. Efficacy of Transdiagnostic Treatments: A Review of Published Outcome Studies and Future Research Directions. J. Cogn. Psychother. 2009, 23, 20–33. [Google Scholar] [CrossRef]
- Costello, E.J.; Mustillo, S.; Erkanli, A.; Keeler, G.; Angold, A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch. Gen. Psychiatry 2003, 60, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, M.J.; Nissen, J.B.; Mors, O.; Thomsen, P.H. Age and gender differences in depressive symptomatology and comorbidity: An incident sample of psychiatrically admitted children. J. Affect. Disord. 2005, 84, 85–91. [Google Scholar] [CrossRef] [PubMed]
- Lynch, F.L.; Dickerson, J.F.; Rozenman, M.S.; Gonzalez, A.; Schwartz, K.T.G.; Porta, G.; O’Keeffe-Rosetti, M.; Brent, D.; Weersing, V.R. Cost-effectiveness of Brief Behavioral Therapy for Pediatric Anxiety and Depression in Primary Care. JAMA Netw. Open 2021, 4, e211778. [Google Scholar] [CrossRef]
- Blackman, J.A.; Gurka, M.J.; Gurka, K.K.; Oliver, M.N. Emotional, developmental and behavioural co-morbidities of children with chronic health conditions. J. Paediatr. Child Health 2011, 47, 742–747. [Google Scholar] [CrossRef] [PubMed]
- Cousino, M.K.; Hazen, R.A. Parenting stress among caregivers of children with chronic illness: A systematic review. J. Pediatr. Psychol. 2013, 38, 809–828. [Google Scholar] [CrossRef] [PubMed]
- Vermaes, I.P.; van Susante, A.M.; van Bakel, H.J. Psychological functioning of siblings in families of children with chronic health conditions: A meta-analysis. J. Pediatr. Psychol. 2012, 37, 166–184. [Google Scholar] [CrossRef]
- Stewart, S.M.; Rao, U.; Emslie, G.J.; Klein, D.; White, P.C. Depressive symptoms predict hospitalization for adolescents with type 1 diabetes mellitus. Pediatrics 2005, 115, 1315–1319. [Google Scholar] [CrossRef] [PubMed]
- Naylor, C. Mental Health and Long-Term Conditions: The Cost of Co-Morbidity; The King’s Fund: London, UK, 2012. [Google Scholar]
- Zima, B.T.; Rodean, J.; Hall, M.; Bardach, N.S.; Coker, T.R.; Berry, J.G. Psychiatric Disorders and Trends in Resource Use in Pediatric Hospitals. Pediatrics 2016, 138, e20160909. [Google Scholar] [CrossRef]
- Children’sCommissioner. Lightning Review: Access to Child and Adolescent Mental Health Services; Children’s Commissioner: London, UK, 2016. [Google Scholar]
- Hendriksen, J.G.; Peijnenborgh, J.C.; Aldenkamp, A.P.; Vles, J.S. Diagnostic overshadowing in a population of children with neurological disabilities: A cross sectional descriptive study on acquired ADHD. Eur. J. Paediatr. Neurol. 2015, 19, 521–524. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.A.; Nunns, M.; Shaw, L.; Rogers, M.; Walker, E.; Ford, T.; Garside, R.; Ukoumunne, O.; Titman, P.; Shafran, R.; et al. Interventions to improve the mental health of children and young people with long-term physical conditions: Linked evidence syntheses. Health Technol. Assess. 2019, 23, 1–164. [Google Scholar] [CrossRef]
- Smith, M.M.; Pereira, S.P.; Chan, L.; Rose, C.; Shafran, R. Impact of Well-being Interventions for Siblings of Children and Young People with a Chronic Physical or Mental Health Condition: A Systematic Review and Meta-Analysis. Clin. Child Fam. Psychol. Rev. 2018, 21, 246–265. [Google Scholar] [CrossRef] [PubMed]
- Law, E.; Fisher, E.; Eccleston, C.; Palermo, T.M. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst. Rev. 2019, 3, CD009660. [Google Scholar] [CrossRef] [PubMed]
- Bennett, S.; Shafran, R.; Coughtrey, A.; Walker, S.; Heyman, I. Psychological interventions for mental health disorders in children with chronic physical illness: A systematic review. Arch. Dis. Child. 2015, 100, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Catanzano, M.; Bennett, S.D.; Sanderson, C.; Patel, M.; Manzotti, G.; Kerry, E.; Coughtrey, A.E.; Liang, H.; Heyman, I.; Shafran, R. Brief psychological interventions for psychiatric disorders in young people with long term physical health conditions: A systematic review and meta-analysis. J. Psychosom. Res. 2020, 136, 110187. [Google Scholar] [CrossRef] [PubMed]
- Shafran, R.; Myles-Hooton, P.; Bennett, S.; Ost, L.G. The concept and definition of low intensity cognitive behaviour therapy. Behav. Res. Ther. 2021, 138, 103803. [Google Scholar] [CrossRef] [PubMed]
- Hawton, K.; Salkovskis, P.M.; Kirk, J.; Clark, D.M. Cognitive Behaviour Therapy for Psychiatric Problems: A Practical Guide; Oxford University Press: Oxford, UK, 1989. [Google Scholar]
- Stallard, P. Low-intensity interventions for anxiety disorders. Lancet Psychiatry 2017, 4, 508–509. [Google Scholar] [CrossRef]
- Crenna-Jennings, W.; Hutchinson, J. Access to Children and Young People’s Mental Health Services; Education Policy Institute: London, UK, 2018. [Google Scholar]
- Clark, D.M.; Layard, R.; Smithies, R.; Richards, D.A.; Suckling, R.; Wright, B. Improving access to psychological therapy: Initial evaluation of two UK demonstration sites. Behav. Res. Ther. 2009, 47, 910–920. [Google Scholar] [CrossRef] [PubMed]
- Hilferty, F.; Cassells, R.; Muir, K.; Duncan, A.; Christensen, D.; Mitrou, F.; Gao, G.; Mavisakalyan, A.; Hafekost, K.; Tarverdi, Y.; et al. Is Headspace Making a Difference to Young People’s Lives? Final Report of the Independent Evaluation of the Headspace Program; University of New South Wales: Sydney, Australia, 2015. [Google Scholar]
- Iyer, S.N.; Boksa, P.; Lal, S.; Shah, J.; Marandola, G.; Jordan, G.; Doyle, M.; Joober, R.; Malla, A.K. Transforming youth mental health: A Canadian perspective. Ir. J. Psychol. Med. 2015, 32, 51–60. [Google Scholar] [CrossRef] [PubMed]
- O’Keeffe, L.; O’Reilly, A.; O’Brien, G.; Buckley, R.; Illback, R. Description and outcome evaluation of Jigsaw: An emergent Irish mental health early intervention programme for young people. Ir. J. Psychol. Med. 2015, 32, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Barwick, M.; Urajnik, D.; Sumner, L.; Cohen, S.; Reid, G.; Engel, K.; Moore, J.E. Profiles and service utilization for children accessing a mental health walk-in clinic versus usual care. J. Evid. Based Soc. Work 2013, 10, 338–352. [Google Scholar] [CrossRef]
- Love, R.L. A Walk-In Clinic in a University Mental Health Service: Some Preliminary Findings. J. Am. Coll. Health 2010, 31, 224–225. [Google Scholar] [CrossRef]
- Nath, R.; Shannon, H.; Georgiades, K.; Sword, W.; Raina, P. The impact of drop-in centers on the health of street children in New Delhi, India: A cross-sectional study. Child Abuse Negl. 2016, 62, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Cheung, A.; Jegathesan, T.; Mantini, A.; Chan, J.; Vijendra Das, R.; Aiyadurai, R.; Freeman, S. The Role of Ontario’s First School-Based Health Clinic in Accessing Developmental and Mental Health Care for Children from Inner City Elementary Schools: A retrospective Chart Review. Paediatr. Child Health 2017, 22, e6–e7. [Google Scholar] [CrossRef]
- Catanzano, M.; Bennett, S.D.; Kerry, E.; Liang, H.; Heyman, I.; Coughtrey, A.E.; Fifield, K.; Taylor, C.; Dalgleish, T.; Xu, L.; et al. Evaluation of a mental health drop-in centre offering brief transdiagnostic psychological assessment and treatment for children and adolescents with long-term physical conditions and their families: A single-arm, open, non-randomised trial. Evid. Based Ment. Health 2021, 24, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Glazebrook, C.; Hollis, C.; Heussler, H.; Goodman, R.; Coates, L. Detecting emotional and behavioural problems in paediatric clinics. Child Care Health Dev. 2003, 29, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Joosten, M.M.H.; Maurice-Stam, H.; Scholten, L.; Grootenhuis, M.A. Hearing siblings’ voices: Exploring the (online) support needs of siblings of children with a chronic condition. J. Patient Rep. Outcomes 2019, 3, 11. [Google Scholar] [CrossRef]
- Goodman, R.; Ford, T.; Richards, H.; Gatward, R.; Meltzer, H. The Development and Well-Being Assessment: Description and initial validation of an integrated assessment of child and adolescent psychopathology. J. Child Psychol. Psychiatry 2000, 41, 645–655. [Google Scholar] [CrossRef]
- Noble, M.; Wright, G.; Smith, G.; Dibben, C. Measuring Multiple Deprivation at the Small-Area Level. Environ. Plan. A Econ. Space 2016, 38, 169–185. [Google Scholar] [CrossRef]
- Goodman, A.; Goodman, R. Population mean scores predict child mental disorder rates: Validating SDQ prevalence estimators in Britain. J. Child Psychol. Psychiatry 2011, 52, 100–108. [Google Scholar] [CrossRef]
- Goodman, R. Psychometric properties of the strengths and difficulties questionnaire. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 1337–1345. [Google Scholar] [CrossRef] [PubMed]
- Yao, S.; Zhang, C.; Zhu, X.; Jing, X.; McWhinnie, C.M.; Abela, J.R. Measuring adolescent psychopathology: Psychometric properties of the self-report strengths and difficulties questionnaire in a sample of Chinese adolescents. J. Adolesc. Health 2009, 45, 55–62. [Google Scholar] [CrossRef] [PubMed]
- Muris, P.; Meesters, C.; van den Berg, F. The Strengths and Difficulties Questionnaire (SDQ)—Further evidence for its reliability and validity in a community sample of Dutch children and adolescents. Eur. Child Adolesc. Psychiatry 2003, 12, 1–8. [Google Scholar] [CrossRef]
- Lundh, L.G.; Wangby-Lundh, M.; Bjarehed, J. Self-reported emotional and behavioral problems in Swedish 14 to 15-year-old adolescents: A study with the self-report version of the Strengths and Difficulties Questionnaire. Scand. J. Psychol. 2008, 49, 523–532. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, D.; Gould, M.S.; Brasic, J.; Ambrosini, P.; Fisher, P.; Bird, H.; Aluwahlia, S. A children’s global assessment scale (CGAS). Arch. Gen. Psychiatry 1983, 40, 1228–1231. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Lowe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Lowe, B.; Decker, O.; Muller, S.; Brahler, E.; Schellberg, D.; Herzog, W.; Herzberg, P.Y. Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med. Care 2008, 46, 266–274. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Lowe, B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: A systematic review. Gen. Hosp. Psychiatry 2010, 32, 345–359. [Google Scholar] [CrossRef] [PubMed]
- Edbrooke-Childs, J.; Macdougall, A.; Hayes, D.; Jacob, J.; Wolpert, M.; Deighton, J. Service-level variation, patient-level factors, and treatment outcome in those seen by child mental health services. Eur. Child Adolesc. Psychiatry 2017, 26, 715–722. [Google Scholar] [CrossRef]
- Wolpert, M.; Jenna, J.; Napoleone, E.; Whale, A.; Calderon, A.; Edbrooke-Childs, J. Child and Parent Reported Outcomes and Experience from Child and Young People’s Mental Health Services 2011–2015; CORC: London, UK, 2016. [Google Scholar]
- Department of Health. Towards a Shared Vision for Mental Health; Department of Health: London, UK, 2009. [Google Scholar]
- Hussain, F.; Cochrane, R. Depression in South Asian women living in the UK: A review of the literature with implications for service provision. Transcult. Psychiatry 2004, 41, 253–270. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.S.; Casey, S.J.; Bishop, A.J.; Prytys, M.; Whittinger, N.; Weinman, J. How black African and white British women perceive depression and help-seeking: A pilot vignette study. Int. J. Soc. Psychiatry 2011, 57, 362–374. [Google Scholar] [CrossRef] [PubMed]
- Maginn, S.; Boardman, A.P.; Craig, T.K.; Haddad, M.; Heath, G.; Stott, J. The detection of psychological problems by General Practitioners--influence of ethnicity and other demographic variables. Soc. Psychiatry Psychiatr. Epidemiol. 2004, 39, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Mieloo, C.L.; Bevaart, F.; Donker, M.C.; van Oort, F.V.; Raat, H.; Jansen, W. Validation of the SDQ in a multi-ethnic population of young children. Eur. J. Public Health 2014, 24, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Memon, A.; Taylor, K.; Mohebati, L.M.; Sundin, J.; Cooper, M.; Scanlon, T.; de Visser, R. Perceived barriers to accessing mental health services among black and minority ethnic (BME) communities: A qualitative study in Southeast England. BMJ Open 2016, 6, e012337. [Google Scholar] [CrossRef] [PubMed]
- Mathers, N.; Mitchell, C. Are the gates to be thrown open? Br. J. Gen. Pract. 2010, 60, 317–318. [Google Scholar] [CrossRef] [PubMed]
- Hodgkinson, S.; Godoy, L.; Beers, L.S.; Lewin, A. Improving Mental Health Access for Low-Income Children and Families in the Primary Care Setting. Pediatrics 2017, 139. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.S.; Boardman, J.; Whittinger, N.; Ashworth, M. Can a self-referral system help improve access to psychological treatments? Br. J. Gen. Pract. 2010, 60, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Russ, S.A.; Larson, K.; Halfon, N. A national profile of childhood epilepsy and seizure disorder. Pediatrics 2012, 129, 256–264. [Google Scholar] [CrossRef]
- Betancur, C. Etiological heterogeneity in autism spectrum disorders: More than 100 genetic and genomic disorders and still counting. Brain Res. 2011, 1380, 42–77. [Google Scholar] [CrossRef] [PubMed]
- McEwen, F.S.; Stewart, C.S.; Colvert, E.; Woodhouse, E.; Curran, S.; Gillan, N.; Hallett, V.; Lietz, S.; Garnett, T.; Ronald, A.; et al. Diagnosing autism spectrum disorder in community settings using the Development and Well-Being Assessment: Validation in a UK population-based twin sample. J. Child Psychol. Psychiatry 2016, 57, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Herbert, L.; Hardy, S. Implementation of a Mental Health Screening Program in a Pediatric Tertiary Care Setting. Clin. Pediatr. 2019, 58, 1078–1084. [Google Scholar] [CrossRef] [PubMed]

| Drop-in Centre | Hospital-Wide Data | t/U/χ2/z; p | Nation-Wide Data | t/U/χ2/z; p | ||
|---|---|---|---|---|---|---|
| Age of <18s at the hospital in years, mean ± SD (range) | 9.14 ± 4.28 (0–17) | 6.8 ± 5.20 (0–17) *** | 4.1; p < 0.001 | 11.64 ± 3.39 (0–17) *** | −6.8; p < 0.001 | |
| Age of parents, mean ± SD (range) | 39.19 ± 8.57 (22–54) | |||||
| IMD decile, median (IQR) | 5 (3–8) | 5 (3–8) | 1,615,771; p = 0.18 | |||
| Gender, % (n/n total) | Female | 55 (45/82) | 51 | 0.35; p = 0.55 | 47 (7565) | 1.60; p = 0.21 |
| Male | 45 (37/82) | 49 | 53 (8440) | |||
| Primary recipient of the intervention, % (n/n total) | Patient | 80 (65/82) | ||||
| Parent/carer | 13 (11/82) | |||||
| Sibling | 7 (6/82) | - | ||||
| Ethnicity, % (n/n total) | White | 61 (43/81) | 62 | 3.71; p = 0.45 | 82 *** | 27.3; p < 0.001 |
| Asian | 14 (11/81) | 16 | 5 *** | 11.9; p < 0.001 | ||
| Black | 13 (10/81) | 9 | 5 * | 8.74; p = 0.016 | ||
| Any Mixed background | 6 (5/81) | 4 | 5 | 0.19; p = 1 | ||
| Any other ethnicity | 6 (5/81) | 9 | 3 | 3.86; p = 0.25 | ||
| Parent relationship to child, % (n/n total) | Mother | 87 (71/82) | ||||
| Father | 13 (11/82) | |||||
| Presenting problems, % (n/n total) | Anxiety | 49 (40/82) | 49 | 1.92; p = 0.66 | ||
| Challenging behaviour | 35 (29/82) | 34 | 1.78; p = 0.73 | |||
| Low mood | 22 (18/82) | 50 ** | 10.3; p = 0.005 | |||
| Other | 15 (12/82) | 14 | 0.50; p = 1 | |||
| Co-morbidity defined as being above threshold on 2 or more SDQ-p subscales | Yes | 57 (37/65) | ||||
| Known pre-existing neurodevelopmental diagnosis, % (n/n total) | ASD | 9 (7/74) | 8 | 0.06; p = 0.8 | ||
| Intellectual Disability | 11 (8/74) | 6 | 2.24; p = 0.14 | |||
| None | 81 (60/74) | |||||
| Need for translator, % (n/n total) | Yes | 7 (6/82) | 4 | 1.6; p = 0.21 | ||
| No | 93 (76/82) | 96 | ||||
| County of origin, % (n/n total) | <50 miles of London | 92 (68/74) | ||||
| >50 miles of London | 8 (6/74) | |||||
| History of mental health input, % (n/n total) | Yes | 48 (38/80) | ||||
| No | 52 (42/80) | |||||
| History of risk present, % (n/n total) | Yes | 15 (12/81) | - | - | - | - |
| Primary intervention allocated to, % (n/n total) | Low-intensity CBT | 33 (27/82) | ||||
| Referral | 50 (41/82) | |||||
| Neurodevelopmental assessment | 6 (5/82) | |||||
| Signposting to resources only | 11 (9/82) | |||||
| N/N Total | Median (IQR) | Missing n (%) | Clinical Threshold | % above Clinical Threshold | |||
|---|---|---|---|---|---|---|---|
| SDQ-Parent 4–17 | Total | 57/67 | 19 (13–26) | 10 (15) | High | ≥17 | 67 |
| Impact | 55/67 | 4 (2–6) | 12 (18) | Very high | ≥2 | 80 | |
| Length of difficulties | 55/67 | 4 (4–4) | 16 (22) | ||||
| Burden | 57/67 | 3 (2–3) | 10 (15) | ||||
| Emotional | 57/67 | 6 (3–9) | 10 (15) | High | ≥5 | 63 | |
| Conduct | 57/67 | 3 (1–5) | 10 (15) | High | ≥4 | 49 | |
| Hyperactivity | 57/67 | 6 (3–8) | 10 (15) | Slightly raised | ≥8 | 35 | |
| Peer | 57/67 | 4 (2–6) | 10 (15) | High | ≥4 | 49 | |
| Prosocial | 57/67 | 7 (5–9) | 10 (15) | High | ≤6 | 49 | |
| SDQ-Parent 2–3 | Total | 8/8 | 16 (8–22) | 0 (0) | High | ≥16 | 50 |
| Impact | 8/8 | 4 (1–6) | 0 (0) | Very high | ≥2 | 63 | |
| Length of difficulties | 8/8 | 4 (3–4) | 0 (0) | ||||
| Burden | 8/8 | 3 (2–4) | 0 (0) | ||||
| Emotional | 8/8 | 2 (1–6) | 0 (0) | Close to average | ≥4 | 38 | |
| Conduct | 8/8 | 4 (1–5) | 0 (0) | Slightly raised | ≥5 | 25 | |
| Hyperactivity | 8/8 | 7 (3–9) | 0 (0) | High | ≥7 | 50 | |
| Peer | 8/8 | 3 (1–4) | 0 (0) | Slightly raised | ≥4 | 50 | |
| Prosocial | 8/8 | 8 (5–10) | 0 (0) | Close to average | ≤5 | 25 | |
| PHQ-9 | 54/75 | 8 (3–15) | 21 (28) | Moderate | ≥10 | 44 | |
| GAD-7 | 54/75 | 10 (4–16) | 21 (28) | Moderate | ≥10 | 56 | |
| CGAS | 66/75 | 60 (47–65) | 9 (12) | Some noticeable problems |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Catanzano, M.; Bennett, S.D.; Tibber, M.S.; Coughtrey, A.E.; Liang, H.; Heyman, I.; The Lucy Project Team; Shafran, R. A Mental Health Drop-In Centre Offering Brief Transdiagnostic Psychological Assessment and Treatment in a Paediatric Hospital Setting: A One-Year Descriptive Study. Int. J. Environ. Res. Public Health 2021, 18, 5369. https://doi.org/10.3390/ijerph18105369
Catanzano M, Bennett SD, Tibber MS, Coughtrey AE, Liang H, Heyman I, The Lucy Project Team, Shafran R. A Mental Health Drop-In Centre Offering Brief Transdiagnostic Psychological Assessment and Treatment in a Paediatric Hospital Setting: A One-Year Descriptive Study. International Journal of Environmental Research and Public Health. 2021; 18(10):5369. https://doi.org/10.3390/ijerph18105369
Chicago/Turabian StyleCatanzano, Matteo, Sophie D Bennett, Marc S Tibber, Anna E Coughtrey, Holan Liang, Isobel Heyman, The Lucy Project Team, and Roz Shafran. 2021. "A Mental Health Drop-In Centre Offering Brief Transdiagnostic Psychological Assessment and Treatment in a Paediatric Hospital Setting: A One-Year Descriptive Study" International Journal of Environmental Research and Public Health 18, no. 10: 5369. https://doi.org/10.3390/ijerph18105369
APA StyleCatanzano, M., Bennett, S. D., Tibber, M. S., Coughtrey, A. E., Liang, H., Heyman, I., The Lucy Project Team, & Shafran, R. (2021). A Mental Health Drop-In Centre Offering Brief Transdiagnostic Psychological Assessment and Treatment in a Paediatric Hospital Setting: A One-Year Descriptive Study. International Journal of Environmental Research and Public Health, 18(10), 5369. https://doi.org/10.3390/ijerph18105369






