Validation of an Online Version of the Alcohol Use Disorders Identification Test (AUDIT) for Alcohol Screening in Spanish University Students
Abstract
1. Introduction
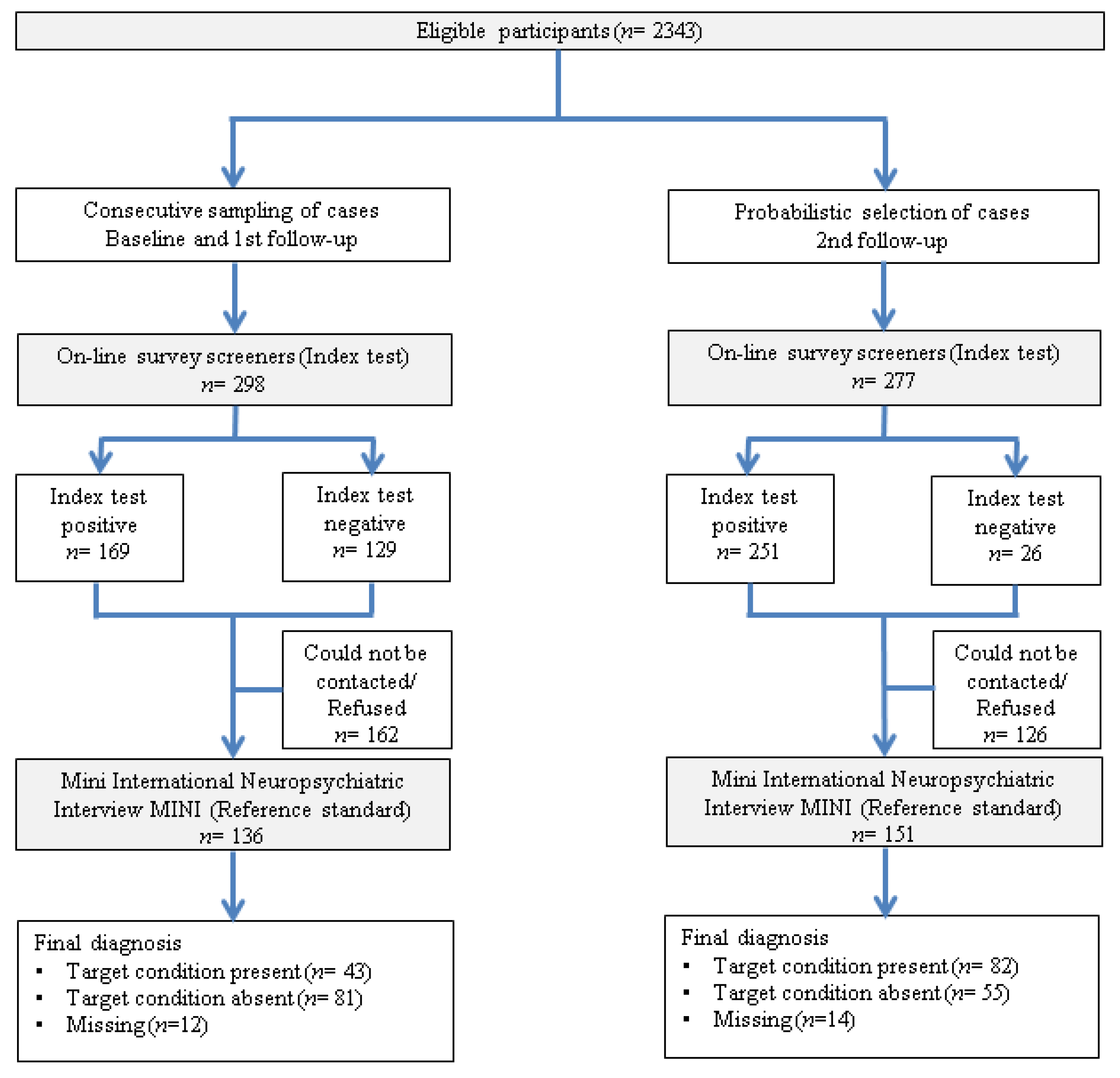
2. Materials and Methods
2.1. Participants
2.2. Online Survey
2.3. Reappraisal Instruments
2.4. Analysis
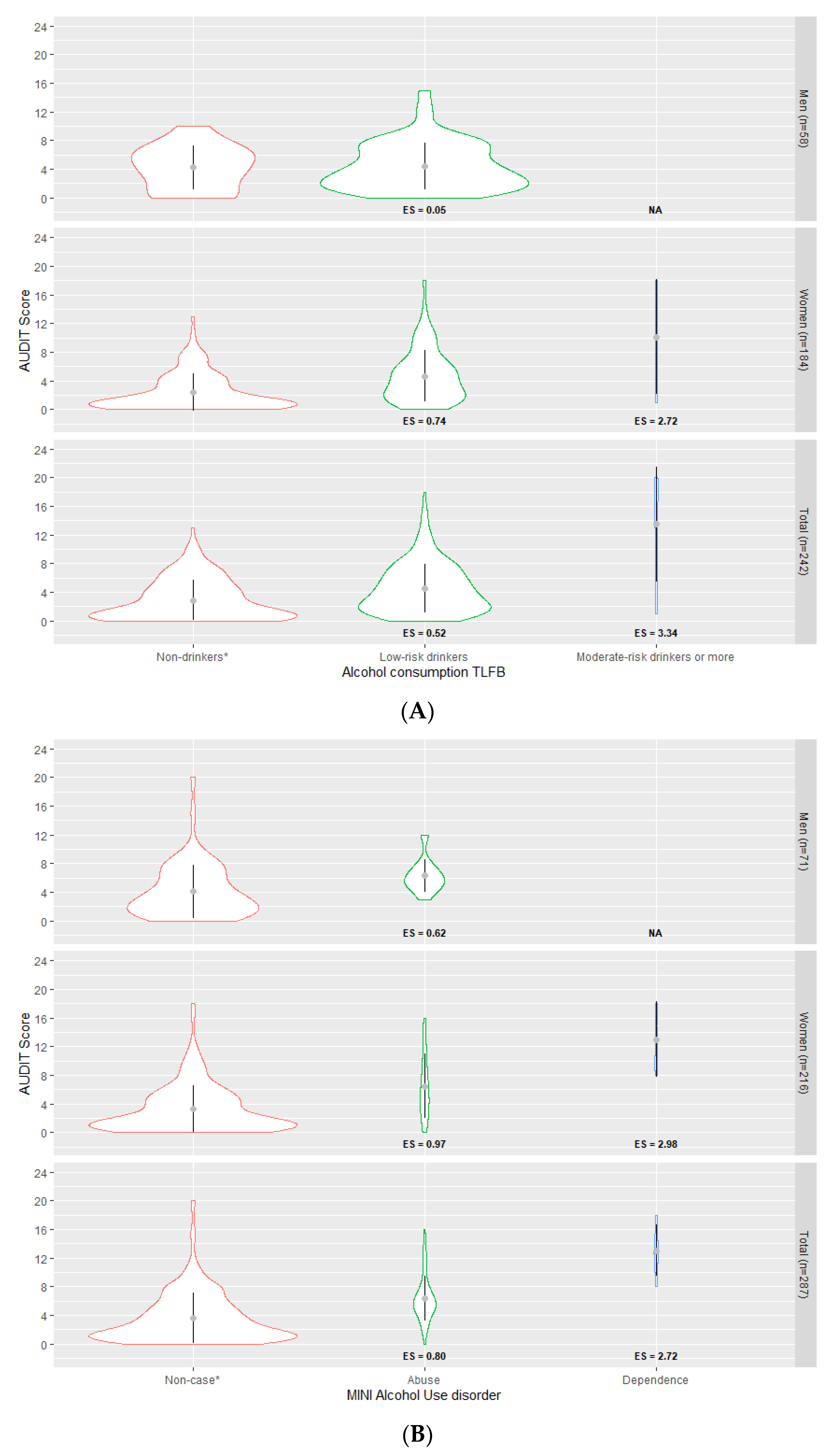
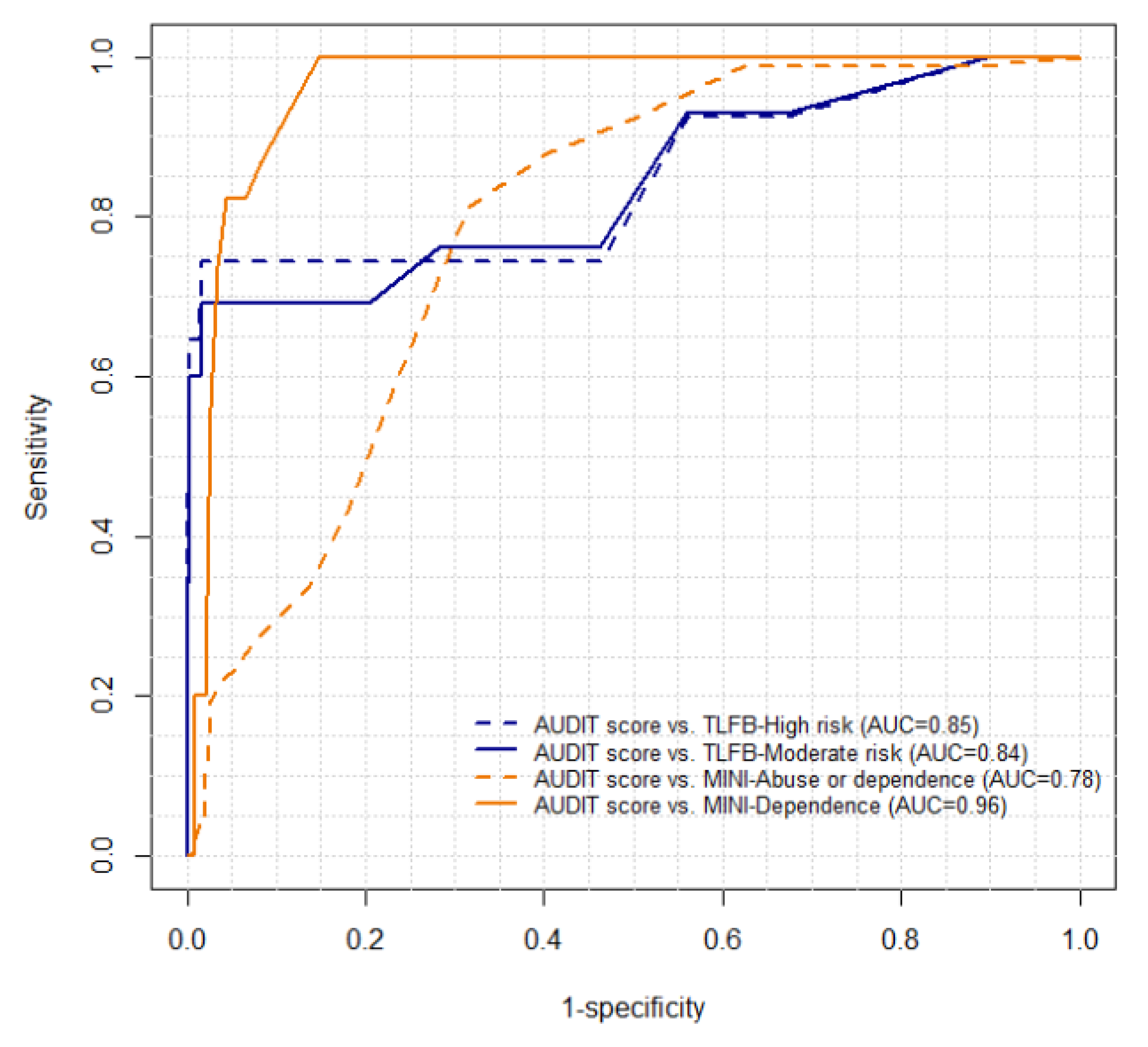
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Status Report on Alcohol and Health 2018; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Griswold, M.G.; Fullman, N.; Hawley, C.; Arian, N.; Zimsen, S.R.; Tymeson, H.D.; Venkateswaran, V.; Tapp, A.D.; Forouzanfar, M.H.; Salama, J.S.; et al. Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the global burden of disease study 2016. Lancet 2018, 392, 1015–1035. [Google Scholar] [CrossRef]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA); Task Force of the National Advisory Council on Alcohol Abuse and Alcoholism. A Call to Action: Changing the Culture of Drinking at US Colleges; National Institutes of Health: Bethesda, MD, USA, 2002. Available online: https://www.collegedrinkingprevention.gov/niaaacollegematerials/publications/calltoaction.aspx (accessed on 10 February 2021).
- ESPAD group. ESPAD Report 2019: Results from the European School Survey Project on Alcohol and Other Drugs; Publications Office of the European Union: Luxembourg, 2020; Available online: https://www.emcdda.europa.eu/publications/joint-publications/espad-report-2019_en (accessed on 10 February 2021).
- Plan Nacional sobre Drogas. Informe EDADES 2019 [EDADES Report 2019]; Ministerio de Sanidad, Consumo y Bienestar Social: Madrid, Spain, 2019.
- Slutske, W.S. Alcohol use disorders among US college students and their non–college-attending peers. Arch. Gen. Psychiatry 2005, 62, 321. [Google Scholar] [CrossRef] [PubMed]
- Kypri, K.; Cronin, M.; Wright, C.S. Do university students drink more hazardously than their non-student peers? Addiction 2005, 100, 713–714. [Google Scholar] [CrossRef]
- Bartoli, F.; Carretta, D.; Crocamo, C.; Schivalocchi, A.; Brambilla, G.; Clerici, M.; Carrà, G. Prevalence and correlates of binge drinking among young adults using alcohol: A cross-sectional survey. Biomed. Res. Int. 2014, 2014, 930795. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.W.; Naimi, T.S.; Brewer, R.D.; Jones, S.E. Binge drinking and associated health risk behaviors among high school students. Pediatrics 2007, 119, 77–85. [Google Scholar] [CrossRef]
- O’Malley, P.M.; Johnston, L.D. Epidemiology of alcohol and other drug use among American college students. J. Stud. Alcohol Suppl. 2002, 14, 23–39. [Google Scholar] [CrossRef]
- Davoren, M.P.; Demant, J.; Shiely, F.; Perry, I.J. Alcohol consumption among university students in Ireland and the United Kingdom from 2002 to 2014: A systematic review. BMC Public Health 2016, 16, 173. [Google Scholar] [CrossRef]
- Wicki, M.; Kuntsche, E.; Gmel, G. Drinking at European universities? A review of students’ alcohol use. Addict. Behav. 2010, 35, 913–924. [Google Scholar] [CrossRef] [PubMed]
- Caamaño-Isorna, F.; Corral, M.; Parada, M.; Cadaveira, F. Factors associated with risky consumption and heavy episodic drinking among Spanish university students. J. Stud. Alcohol Drugs. 2008, 69, 308–312. [Google Scholar] [CrossRef]
- Saitz, R.; Helmuth, E.D.; Aromaa, S.E.; Guard, A.; Belanger, M.; Rosenbloom, D.L. Web-based screening and brief intervention for the spectrum of alcohol problems. Prev. Med. 2004, 39, 969–975. [Google Scholar] [CrossRef]
- Sinadinovic, K.; Berman, A.H.; Hasson, D.; Wennberg, P. Internet-based assessment and self-monitoring of problematic alcohol and drug use. Addict. Behav. 2010, 35, 464–470. [Google Scholar] [CrossRef]
- Dawson, D.A.; Saha, T.D.; Grant, B.F. A multidimensional assessment of the validity and utility of alcohol use disorder severity as determined by item response theory models. Drug Alcohol Depend. 2010, 107, 31–38. [Google Scholar] [CrossRef]
- Saunders, J.B.; Aasland, O.G.; Babor, T.F.; De la Fuente, J.R.; Grant, M. Development of the Alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction 1993, 88, 91–804. [Google Scholar] [CrossRef] [PubMed]
- Rubio, G.; Bermejo, J.; Caballero, M.C.; Santo-Domingo, J.C. Validación de la prueba para la identificación de trastornos por uso de alcohol (AUDIT) en atención Primaria. Rev. Clín. Española 1998, 198, 11–14. [Google Scholar]
- Contel, M.; Gual, A.; Colom, J. Test para la identificación de trastornos por uso de alcohol (AUDIT): Traducción y validación del AUDIT al catalán y castellano. Adicciones 1999, 11, 337–347. [Google Scholar] [CrossRef]
- Gómez Arnáiz, A.; Aguiar Bautista, J.; Santana Montesdeoca, J.M.; Jorrín Morenoy, A.M.S.M.; Conde Morenoy, A.; Betancor León, P. Utilidad diagnóstica del cuestionario alcohol use disorders identification test (AUDIT) para detectar el consumo de alcohol de riesgo en atención primaria. Med. Clin. 2001, 116, 121–124. [Google Scholar] [CrossRef]
- de Torres, L.P.; Fernández-García, J.A.; Arias-Vega, R.; Muriel-Palomino, M.; Márquez-Rebollo, E.; Ruiz-Moral, R. Validación del cuestionario AUDIT para la identificación del consumo de riesgo y de los trastornos por el uso de alcohol en mujeres. Atención Primaria 2005, 36, 499–506. [Google Scholar] [CrossRef][Green Version]
- Boubeta, A.R.; Ferreiro, S.G.; Gallego, M.A.; Tobio, T.B.; Mallou, J.V. Validación del TEST de identificación de trastornos por consumo de alcohol (audit) en población adolescente española. Behav. Psychol. Psicol. Conduct. 2017, 25, 371–386. [Google Scholar]
- Cortés, M.T.; Giménez, J.A.; Motos, P.; Sancerni, M.D. Different versions of the Alcohol Use Disorders Identification Test (AUDIT) as screening instruments for underage binge drinking. Drug Alcohol Depend. 2016, 158, 52–59. [Google Scholar] [CrossRef]
- García-Carretero, M.Á.; Novalbos Ruiz, J.P.; Martínez Delgado, J.M.; O’Ferrall González, C. Validación del test para la identificación de trastornos por uso de alcohol en población universitaria: AUDIT y AUDIT-C. Adicciones 2016, 28, 194. [Google Scholar] [CrossRef]
- Cortés, M.T.; Giménez, J.A.; Motos, P.; Sancerni, M.D.; Cadaveira, F. The utility of the alcohol use disorders identification test (AUDIT) for the analysis of binge drinking in university students. Psicothema 2017, 29, 229–235. [Google Scholar]
- Blasco Cubedo, M.J.; Castellvi Obiols, P.; Almenara, J.; Lagares, C.; Roca, M.; Sesé Hernández, A.; Piqueras, J.A.; Soto-Sanz, V.; Rodríguez-Marín, J.; Echeburúa, E.; et al. Predictive models for suicidal thoughts and behaviors among Spanish University students: Rationale and methods of the UNIVERSAL (University & mental health) project. BMC Psychiatry 2016, 16, 122. [Google Scholar]
- Bowling, A. Mode of questionnaire administration can have serious effects on data quality. J. Public Health 2005, 27, 281–291. [Google Scholar] [CrossRef] [PubMed]
- Cook, C. Mode of administration bias. J. Man. Manip. Ther. 2010, 18, 61–63. [Google Scholar] [CrossRef] [PubMed]
- Babor, T.F.; Higgins-Biddle, J.C.; Saunders, J.B.; Monteiro, M.G. The Alcohol Use Disorders Identification Test; World Health Organization: Geneva, Switzerland, 2001. [Google Scholar]
- Sobell, L.C.; Sobell, M.B. Timeline Follow-Back. In Measuring Alcohol Consumption; Litten, R.Z., Allen, J.P., Eds.; Humana Press: Totowa, NJ, USA, 1992. [Google Scholar] [CrossRef]
- Sheehan, D.V.; Lecrubier, Y.; Sheehan, K.H.; Amorim, P.; Janavs, J.; Weiller, E.; Hergueta, T.; Baker, R.; Dunbar, G.C. The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J. Clin. Psychiatry 1998, 59 (Suppl. 2), 22–33. [Google Scholar]
- Ballester, L.; Alayo, I.; Vilagut, G.; Almenara, J.; Cebrià, A.I.; Echeburúa, E.; Gabilondo, A.; Gili, M.; Lagares, C.; Piqueras, J.A.; et al. Accuracy of online survey assessment of mental disorders and suicidal thoughts and behaviors in Spanish university students. Results of the WHO World Mental Health-International College Student initiative. PLoS ONE 2019, 14, e0221529. [Google Scholar] [CrossRef]
- Cohen, J.F.; Korevaar, D.A.; Altman, D.G.; Bruns, D.E.; Gatsonis, C.A.; Hooft, L.; Irwig, L.; Levine, D.; Reitsma, J.B.; de Vet, H.C.W.; et al. STARD 2015 guidelines for reporting diagnostic accuracy studies: Explanation and elaboration. BMJ Open 2016, 6, 1–17. [Google Scholar] [CrossRef]
- Kokotailo, P.K.; Egan, J.; Gangnon, R.; Brown, D.; Mundt, M.; Fleming, M. Validity of the alcohol use disorders identification test in college students. Alcohol Clin. Exp. Res. 2004, 28, 914–920. [Google Scholar] [CrossRef]
- Aalto, M.; Alho, H.; Halme, J.T.; Seppä, K. AUDIT and its abbreviated versions in detecting heavy and binge drinking in a general population survey. Drug Alcohol Depend. 2009, 103, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Tuunanen, M.; Aalto, M.; Seppä, K. Binge drinking and its detection among middle-aged men using AUDIT, AUDIT-C and AUDIT-3. Drug Alcohol Rev. 2007, 26, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Ministerio de Sanidad. Límites de Consumo de Bajo Riesgo de Alcohol. Actualización del Riesgo Relacionado con los Niveles de Consumo de Alcohol, el Patrón de Consumo y el Tipo de Bebida; Ministerio de Sanidad: Madrid, Spain, 2020. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/Prevencion/alcohol/docs/Limites_Consumo_Bajo_Riesgo_Alcohol_Revision_evidencia_cientifica.pdf (accessed on 10 February 2021).
- Ministerio de Sanidad y Consumo. Prevención de los problemas derivados del alcohol. In 1a Conferencia de prevención y promoción de la salud en la práctica clínica en España; Ministerio de Sanidad y Consumo: Madrid, Spain, 2007. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/docs/prevencionProblemasAlcohol.pdf (accessed on 10 February 2021).
- Parada, M.; Corral, M.; Caamaño-Isorna, F.; Mota, N.; Crego, A.; Rodríguez Holguín, S.; Cadaveira, F. Definición del concepto de consumo intensivo de alcohol adolescente (binge drinking). Adicciones 2011, 23, 53. [Google Scholar] [CrossRef] [PubMed]
- Rosón, B. Consumo de riesgo y perjudicial de alcohol. Prevalencia y métodos de detección en la práctica clínica. Galicia Clin. 2008, 69, 29–44. [Google Scholar] [CrossRef]
- Bobes, J. A Spanish validation study of the Mini-international neuropsychiatric interview. Eur. Psychiatry 1998, 13, 198s–199s. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM–IV; American Psychiatric Association: Washington, DC, USA, 1994. [Google Scholar]
- Kyriazos, T.A. Applied psychometrics: Sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology 2018, 9, 2207–2230. [Google Scholar] [CrossRef]
- Gatignon, H. Confirmatory factor analysis. In Statistical Analysis of Management Data; Springer: New York, NY, USA, 2010; pp. 59–122. [Google Scholar]
- Schreiber, J.B.; Nora, A.; Stage, F.K.; Barlow, E.A.; King, J. Reporting structural equation modeling and confirmatory factor analysis results: A review. J. Educ Res. 2006, 99, 23–38. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Hedges, L.V.; Olkin, I. Estimation of a single effect size: Parametric and non-parametric methods. In Statistical Methods for Meta-Analysis; Academic Press: Orlando, FL, USA, 1985; pp. 75–106. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Lawrence Elrbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Avenevoli, S.; Green, J.; Gruber, M.J.; Guyer, M.; He, Y.; Jin, R.; Kaufman, J.; Sampson, N.A.; Alan M Zaslavsky, A.M.; et al. National comorbidity survey replication adolescent supplement (NCS-A): III. Concordance of DSM-IV/CIDI diagnoses with clinical reassessments. J. Am. Acad. Child. Adolesc. Psychiatry 2009, 48, 386–399. [Google Scholar] [CrossRef]
- SAS Institute Inc. SAS Software 9.4; SAS Campus Drive: Cary, NC, USA, 2014. [Google Scholar]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide; Muthén & Muthén: Los Angeles, CA, USA, 2017. [Google Scholar]
- de Meneses-Gaya, C.; Zuardi, A.W.; Loureiro, S.R.; Crippa, J.A.S. Alcohol use disorders identification test (AUDIT): An updated systematic review of psychometric properties. Psychol. Neurosci. 2009, 2, 83–97. [Google Scholar] [CrossRef]
- Nunnally, J.C.; Bernstein, I.H. The assessment of reliability. Psychom. Theory 1994, 3, 248–292. [Google Scholar]
- Skipsey, K.; Burleson, J.A.; Kranzler, H.R. Utility of the AUDIT for identification of hazardous or harmful drinking in drug-dependent patients. Drug Alcohol Depend. 1997, 45, 157–163. [Google Scholar] [CrossRef]
- Carey, K.B.; Carey, M.P.; Chandra, P.S. Psychometric evaluation of the alcohol use disorders identification test and short drug abuse screening test with psychiatric patients in India. J. Clin. Psychiatry 2003, 64, 767–774. [Google Scholar] [CrossRef]
- Adewuya, A.O. Validation of the alcohol use disorders identification test (AUDIT) as a screening tool for alcohol-related problems among nigerian university students. Alcohol Alcohol. 2005, 40, 575–577. [Google Scholar] [CrossRef] [PubMed]
- Vetter, T.R.; Schober, P.; Mascha, E.J. Diagnostic testing and decision-making: Beauty is not just in the eye of the beholder. Anesth. Analg. 2018, 127, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- First, M.B.; Spitzer, R.L.; Gibbon, M.; Williams, J.B. Structured Clinical Interview for Axis I DSM-IV Disorders; New York State Psychiatric Institute: New York, NY, USA, 1994. [Google Scholar]
- Kessler, R.C.; Üstün, T.B. The world mental health (WMH) survey initiative version of the World Health Organization (WHO) composite international diagnostic interview (CIDI). Int. J. Methods Psychiatr. Res. 2004, 13, 93–121. [Google Scholar] [CrossRef] [PubMed]
- Hagman, B.T. Toward efficient screening for DSM-5 alcohol use disorders in college students: Performance of the audit-c. Addict. Disord. Treat. 2015, 14, 1–15. [Google Scholar] [CrossRef]
- Hagman, B.T. Performance of the AUDIT in detecting DSM-5 alcohol use disorders in college students. Subst. Use Misuse. 2016, 51, 1521–1528. [Google Scholar] [CrossRef]
- Dawson, D.A.; Smith, S.M.; Saha, T.D.; Rubinsky, A.D.; Grant, B.F. Comparative performance of the AUDIT-C in screening for DSM-IV and DSM-5 alcohol use disorders. Drug Alcohol Depend. 2012, 126, 384–388. [Google Scholar] [CrossRef]
- Moehring, A.; Rumpf, H.-J.; Hapke, U.; Bischof, G.; John, U.; Meyer, C. Diagnostic performance of the alcohol use disorders identification test (AUDIT) in detecting DSM-5 alcohol use disorders in the general population. Drug Alcohol Depend. 2019, 204, 107530. [Google Scholar] [CrossRef]
- Ekholm, O.; Strandberg-Larsen, K.; Grønbæk, M. Influence of the recall period on a beverage-specific weekly drinking measure for alcohol intake. Eur J. Clin. Nutr. 2011, 65, 520–525. [Google Scholar] [CrossRef]
- Poulton, A.; Pan, J.; Bruns, L.R.; Sinnott, R.O.; Hester, R. Assessment of alcohol intake: Retrospective measures versus a smartphone application. Addict. Behav. 2018, 83, 35–41. [Google Scholar] [CrossRef]
- Ekholm, O. Influence of the recall period on self-reported alcohol intake. Eur. J. Clin. Nutr. 2004, 58, 60–63. [Google Scholar] [CrossRef]
- Cunningham, J.A.; Ansara, D.; Wild, T.C.; Toneatto, T.; Koski Jännes, A. What is the price of perfection? The hidden costs of using detailed assessment instruments to measure alcohol consumption. J. Stud. Alcohol. 1996, 60, 756–758. [Google Scholar] [CrossRef] [PubMed]
- Vakili, S.; Sobell, L.C.; Sobell, M.B.; Simco, E.R.; Agrawal, S. Using the timeline followback to determine time windows representative of annual alcohol consumption with problem drinkers. Addict. Behav. 2008, 33, 1123–1130. [Google Scholar] [CrossRef] [PubMed]
- Kypri, K.; Hallett, J.; Howat, P.; McManus, A.; Maycock, B.; Bowe, S.; Horton, N.J. Randomized controlled trial of proactive web-based alcohol screening and brief intervention for university students. Arch. Intern. Med. 2009, 169, 1508–1514. [Google Scholar] [CrossRef] [PubMed]
| Total n = 287 | Men n = 71 | Women n = 216 | p-Value | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Age | ||||
| 18 | 177 (69.6) | 45 (76.0) | 132 (64.4) | 0.09 |
| 19 | 54 (14.5) | 13 (11.6) | 41 (16.9) | |
| 20+ | 56 (15.9) | 13 (12.4) | 43 (18.8) | |
| Nationality | ||||
| Non-Spanish | 29 (2.9) | 4 (2.3) | 25 (3.2) | 0.74 |
| Field of studies | ||||
| Arts and Humanities | 37 (9.8) | 2 (7.0) | 35 (11.9) | <0.01 * |
| Engineering and Architecture | 32 (18.6) | 21 (32.0) | 11 (8.2) | |
| Health Sciences | 85 (15.7) | 14 (10.2) | 71 (20.1) | |
| Science | 25 (8.4) | 11 (8.6) | 14 (8.2) | |
| Social and Legal Sciences | 108 (47.6) | 23 (42.2) | 85 (51.6) | |
| AUDIT categories | ||||
| Binge drinking a | 45 (18.9) | 14 (25.4) | 31 (13.6) | 0.02 * |
| Risk drinking b | 65 (21.9) | 12 (20.2) | 53 (23.3) | 0.53 |
| Probable dependence c | 11 (3.3) | 3 (3.5) | 8 (3.2) | 0.76 |
| TLFB Alcohol consumption | ||||
| Binge drinking d | 32 (9.8) | 8 (9.6) | 24 (10.0) | 0.93 |
| Low-risk drinkers e | 112 (51.4) | 34 (65.9) | 78 (39.6) | <0.01 * |
| Moderate-risk drinkers or more f | 7 (2.0) | 1 (1.8) | 6 (2.1) | 1.0 |
| High-risk drinkers g | 6 (2.0) | 1 (1.8) | 5 (2.1) | 1.0 |
| MINI alcohol use disorder | ||||
| Abuse h | 29 (10.0) | 11 (14.2) | 18 (6.4) | 0.03 * |
| Dependence i | 7 (1.5) | 2 (1.6) | 5 (1.3) | 1.0 |
| Abuse/Dependence j | 35 (11.2) | 13 (15.6) | 22 (7.6) | 0.03 * |
| AUDIT Items | Mean (SD) | Corrected Item-Total Correlation | Cronbach’s Alpha If Item Deleted |
|---|---|---|---|
| 1 | 1.69 (0.67) | 0.539 | 0.798 |
| 2 | 0.61 (0.76) | 0.509 | 0.800 |
| 3 | 0.78 (0.88) | 0.663 | 0.781 |
| 4 | 0.29 (0.77) | 0.520 | 0.798 |
| 5 | 0.27 (0.53) | 0.558 | 0.796 |
| 6 | 0.18 (0.53) | 0.332 | 0.816 |
| 7 | 0.46 (0.69) | 0.502 | 0.800 |
| 8 | 0.41 (0.66) | 0.623 | 0.786 |
| 9 | 0.27 (0.79) | 0.446 | 0.808 |
| 10 | 0.06 (0.35) | 0.339 | 0.816 |
| AUDIT Items | Standardized Factor Loadings | |
|---|---|---|
| Estimate | SE | |
| 1 | 0.696 | 0.021 |
| 2 | 0.622 | 0.020 |
| 3 | 0.777 | 0.015 |
| 4 | 0.759 | 0.019 |
| 5 | 0.753 | 0.016 |
| 6 | 0.545 | 0.026 |
| 7 | 0.688 | 0.019 |
| 8 | 0.797 | 0.014 |
| 9 | 0.659 | 0.023 |
| 10 | 0.569 | 0.032 |
| RMSEA (95% CI) | 0.049 (0.043–0.056) | |
| CFI | 0.973 | |
| TLI | 0.966 | |
| χ2 (DF), p-value | 219.073 (35), p < 0.001 | |
| AUDIT | TLFB | Positive Operating Characteristics | Negative Operating Characteristics | McNemar | AUC | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cut-Off Point | % (SE) | % (SE) | SN (SE) | PPV (SE) | LR+ | SP (SE) | NPV (SE) | LR− | χ2 (p-Value) | ||
| Total (n = 242) | |||||||||||
| Binge drinking a | 18.9 (2.5) | 9.8 (1.9) | 41.4 (9.9) | 21.6 (5.9) | 2.5 | 83.6 (2.4) | 92.9 (1.8) | 0.7 | 10.1 (0.002 *) | 0.63 | |
| Moderate-risk drinkers or more b | 6/8 | 22.2 (2.7) | 2 (0.9) | 76.2 (19.0) | 6.9 (3.4) | 3.6 | 78.9 (2.6) | 99.4 (0.6) | 0.3 | 48.91 (<0.001 *) | 0.78 |
| High-risk drinkers c | 13 | 3 (1.1) | 1.9 (0.9) | 74.4 (19.5) | 46.2 (17.6) | 43.8 | 98.3 (0.8) | 99.5 (0.4) | 0.3 | 1.58 (0.209) | 0.86 |
| Men (n = 58) ^ | |||||||||||
| Binge drinking a | 25.4 (5.7) | 9.5 (3.9) | 50.7 (15.8) | 19.0 (7.4) | 2.2 | 77.3 (4.1) | 93.7 (2.6) | 0.6 | 11.3 (0.001 *) | 0.64 | |
| Women (n = 184) | |||||||||||
| Binge drinking a | 13.6 (2.5) | 10.1 (2.2) | 34.4 (12.7) | 25.5 (10.0) | 3 | 88.7 (2.8) | 92.4 (2.4) | 0.7 | 1.05 (0.30 *) | 0.62 | |
| Moderate-risk drinkers or more d | 6 | 23.2 (3.1) | 2.4 (1.1) | 63.9 (27.7) | 6.6 (4.3) | 2.9 | 77.8 (3.5) | 98.9 (1.0) | 0.5 | 27.06 (<0.001 *) | 0.71 |
| High-risk drinkers e | 13 | 3 (1.3) | 2.1 (1.1) | 59.6 (28.3) | 43.0 (24.8) | 35.1 | 98.3 (1.1) | 99.1 (0.8) | 0.4 | 0.37 (0.542) | 0.79 |
| AUDIT | MINI | Positive Operating Characteristics | Negative Operating Characteristics | McNemar | AUC | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Cut-Off Point | % (SE) | % (SE) | SN (SE) | PPV (SE) | LR+ | SP (SE) | NPV (SE) | LR− | χ2 (p-Value) | ||
| Total (n = 287) | |||||||||||
| Alcohol abuse/dependence a | 8 | 15.9 (2.2) | 11.2 (1.9) | 33.9 (8.4) | 23.9 (6.3) | 2.5 | 86.3 (2.2) | 91.2 (1.8) | 0.8 | 3.23 (0.072) | 0.60 |
| Alcohol dependence b | 13 | 3.3 (1.1) | 1.5 (0.7) | 56 (24.8) | 24.9 (14.4) | 22.4 | 97.5 (0.9) | 99.3 (0.5) | 0.5 | 3.12 (0.077) | 0.77 |
| Men (n = 71) ^ | |||||||||||
| Alcohol abuse/dependence a | 8 | 20.1 (4.8) | 15.6 (4.3) | 26.6 (9.9) | 20.7 (8.1) | 1.4 | 81.1 (3.8) | 85.7 (3.5) | 0.9 | 0.93 (0.334) | 0.54 |
| Women (n = 216) | |||||||||||
| Alcohol abuse/dependence a | 8 | 12.6 (2.3) | 7.7 (1.8) | 46 (13.8) | 28.1 (10.0) | 4.7 | 90.2 (2.5) | 95.3 (1.8) | 0.6 | 2.86 (0.091) | 0.68 |
| Alcohol dependence b | 13 | 3.2 (1.2) | 1.5 (0.8) | 54.3 (35.2) | 26.4 (19.7) | 22.6 | 97.6 (1.2) | 99.3 (0.7) | 0.5 | 1.39 (0.239) | 0.76 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ballester, L.; Alayo, I.; Vilagut, G.; Almenara, J.; Cebrià, A.I.; Echeburúa, E.; Gabilondo, A.; Gili, M.; Lagares, C.; Piqueras, J.A.; et al. Validation of an Online Version of the Alcohol Use Disorders Identification Test (AUDIT) for Alcohol Screening in Spanish University Students. Int. J. Environ. Res. Public Health 2021, 18, 5213. https://doi.org/10.3390/ijerph18105213
Ballester L, Alayo I, Vilagut G, Almenara J, Cebrià AI, Echeburúa E, Gabilondo A, Gili M, Lagares C, Piqueras JA, et al. Validation of an Online Version of the Alcohol Use Disorders Identification Test (AUDIT) for Alcohol Screening in Spanish University Students. International Journal of Environmental Research and Public Health. 2021; 18(10):5213. https://doi.org/10.3390/ijerph18105213
Chicago/Turabian StyleBallester, Laura, Itxaso Alayo, Gemma Vilagut, José Almenara, Ana Isabel Cebrià, Enrique Echeburúa, Andrea Gabilondo, Margalida Gili, Carolina Lagares, José A. Piqueras, and et al. 2021. "Validation of an Online Version of the Alcohol Use Disorders Identification Test (AUDIT) for Alcohol Screening in Spanish University Students" International Journal of Environmental Research and Public Health 18, no. 10: 5213. https://doi.org/10.3390/ijerph18105213
APA StyleBallester, L., Alayo, I., Vilagut, G., Almenara, J., Cebrià, A. I., Echeburúa, E., Gabilondo, A., Gili, M., Lagares, C., Piqueras, J. A., Roca, M., Soto-Sanz, V., Blasco, M. J., Castellví, P., G. Forero, C., Mortier, P., Alonso, J., & on behalf of the UNIVERSAL Study Group. (2021). Validation of an Online Version of the Alcohol Use Disorders Identification Test (AUDIT) for Alcohol Screening in Spanish University Students. International Journal of Environmental Research and Public Health, 18(10), 5213. https://doi.org/10.3390/ijerph18105213








