Adaptability and Resilience of Academic Radiation Oncology Personnel and Procedures during COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Mitigating Procedures
2.2. General Recommendations
- Hospital infection control policies were strictly followed;
- Everyone entering the department was monitored for temperature and screened for symptoms such as fever, cough, or chest pain. If febrile or symptomatic, employees were directed to receive COVID-19 testing;
- Staff treating COVID-19-positive patients were required to wear full PPE, gloves, mask, gowns, goggles, or face shields);
- Everyone was required to wear masks and gloves and to wash their hands with soap/hand sanitizers before and after patient contact;
- Visitors were allowed in the department only when needed;
- All treatment devices and surfaces were cleaned with disinfectant wipes after each treatment;
- Exam room doors remained open for contactless operation and air exchange;
- Consultations and follow-ups were held using telemedicine;
- COVID-19-positive patients were treated at the end of the day on a designated machine;
- A two-week quarantine period was mandated when a member living in the staff/patient’s home tested positive;
- Patients were tested negative for special procedures (brachytherapy, gamma knife, and SBRT);
- Children requiring sedation for irradiation were tested weekly;
- Laptop computers and database access were provided to staff for remote work;
- All teaching conferences, tumor boards, and weekly chart rounds were virtually conducted using teleconferencing.
2.3. Physicians
- Patients were triaged into three groups; (1) patients with radiation emergencies, (2) patients whose treatment could not be postponed, and (3) patients with cancers where treatment could be safely postponed. In general, treatment was only given for groups 1 and 2;
- Only one on-call physician was in the department daily; others were in the clinic only once a week for patient’s on-treatment visits.
2.4. Nursing
- Two nurses were required to be in the clinic;
- Nurses were responsible for maintaining a clean and contamination-free clinic and observing;
- Social distancing among patients was enforced.
2.5. Physicists
- At least two physicists were on site for 2–3 days each week;
- Additional staffing were required on site for special procedures (two physicists each for brachytherapy and gamma knife and one for the SBRT);
- Treatment plans and chart checks were performed by off-site physicists;
- Calibration machine maintenance and QA were performed after hours.
2.6. Dosimetrists
- Two dosimetrists were available on site daily;
- Every dosimetrist was provided a laptop computer to facilitate remote work;
- Communications were maintained as needed via email, phone, and teleconferencing.
2.7. Radiation Therapists
- A two-week rotation with 3 days/week for treatment was adopted;
- When patient volumes decreased to 50%, they were placed in the hospital’s “labor pool” to allow them to work and be paid off;
- Instructed to remain in their assigned rooms to minimize cross exposure;
- After each treatment, they were required to disinfect every treatment device and surface.
2.8. Residents and Students
- Students were instructed to stay at home unless needed;
- One on-call resident was required to be in the clinic each week, while the others were allowed to work from home;
- All clinical and educational activities were performed remotely.
2.9. Laboratory Research
- Laboratory research was halted during the COVID-19 period except data analyses, computational work, maintenance of cell lines, and freezer stocks;
- Research staff were instructed to stay at home;
- Computational research support was available to staff and faculty.
2.10. Impact of Departmental Response
- Questionnaire survey response from all staff based on Institutional Review Board (IRB) exempt status;
- Census of departmental activities (consultations, treatments, and attendance during teaching and clinical conferences);
- COVID-19 infection rates among staff and patients;
- Rates of normalization of activities during the reactivation phase.
3. Results
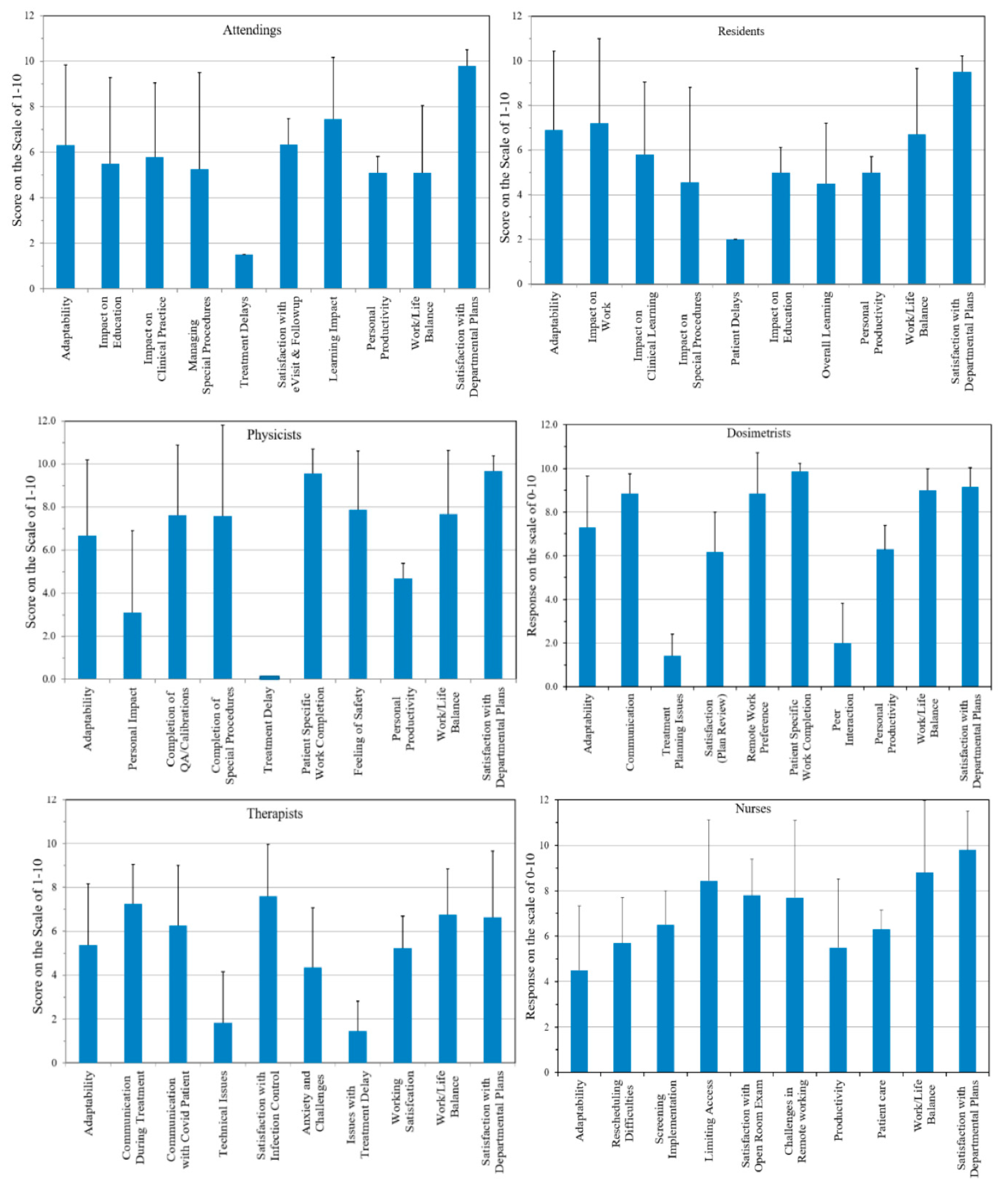
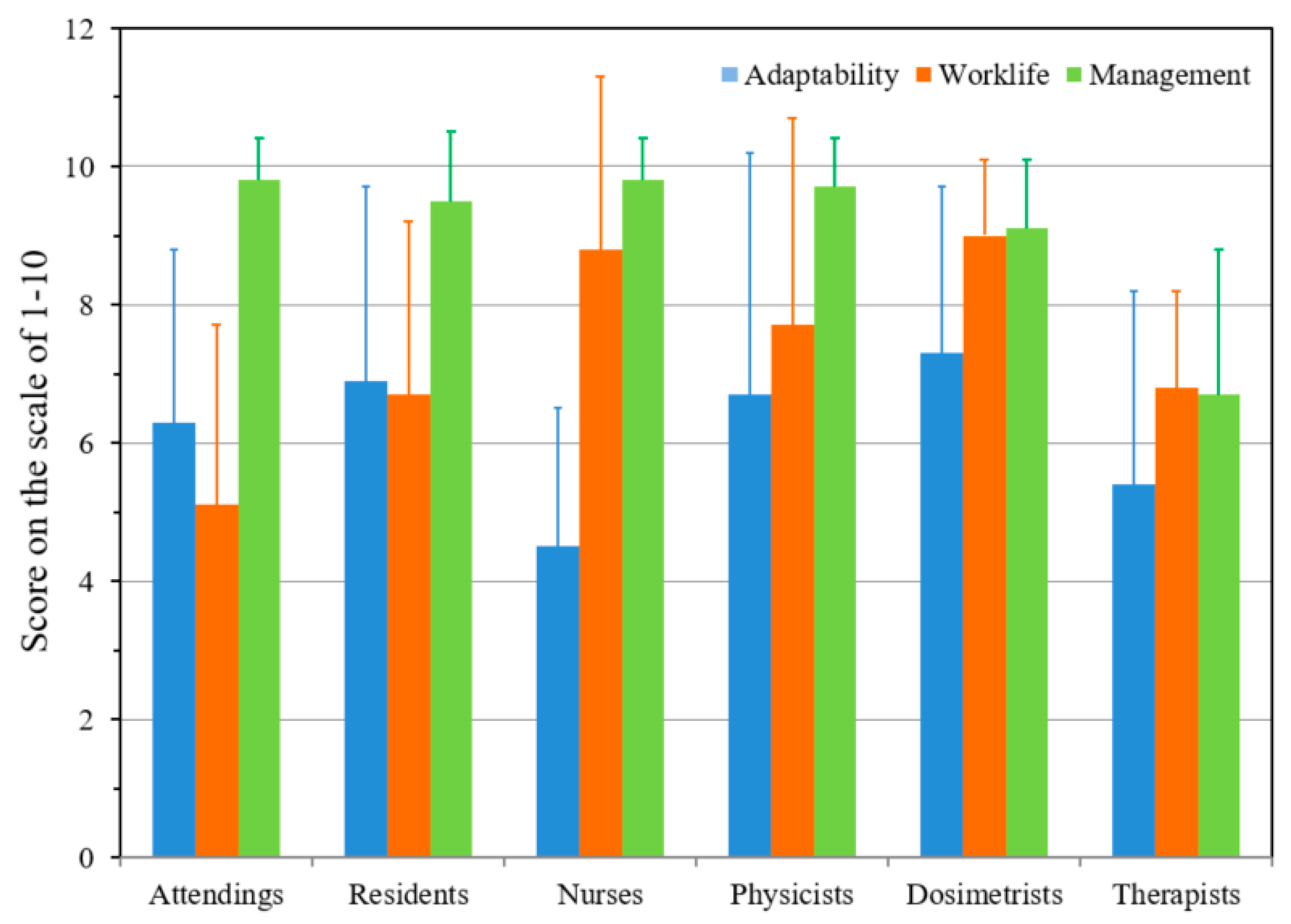
3.1. Questionnaire Response
3.2. Census of Departmental Activities
3.3. COVID-19 Infection Rates
3.4. Census of Activities during the Reactivation Phase
4. Discussions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Belser, J.A.; Tumpey, T.M. The 1918 flu, 100 years later. Science 2018, 359, 255. [Google Scholar] [CrossRef]
- Fauci, A.S.; Lane, H.C.; Redfield, R.R. Covid-19—Navigating the Uncharted. N. Engl. J. Med. 2020, 382, 1268–1269. [Google Scholar] [CrossRef]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef]
- Timmis, K.; Brüssow, H. The COVID-19 pandemic: Some lessons learned about crisis preparedness and management, and the need for international benchmarking to reduce deficits. Environ. Microbiol. 2020, 22, 1986–1996. [Google Scholar] [CrossRef]
- Kooraki, S.; Hosseiny, M.; Myers, L.; Gholamrezanezhad, A. Coronavirus (COVID-19) Outbreak: What the Department of Radiology Should Know. J. Am. Coll. Radiol. 2020, 17, 447–451. [Google Scholar] [CrossRef]
- Hosseiny, M.; Kooraki, S.; Gholamrezanezhad, A.; Reddy, S.; Myers, L. Radiology Perspective of Coronavirus Disease 2019 (COVID-19): Lessons From Severe Acute Respiratory Syndrome and Middle East Respiratory Syndrome. Am. J. Roentgenol. 2020, 214, 1078–1082. [Google Scholar] [CrossRef]
- Hope, M.D.; Raptis, C.A.; Shah, A.; Hammer, M.M.; Henry, T.S. A role for CT in COVID-19? What data really tell us so far. Lancet 2020, 395, 1189–1190. [Google Scholar] [CrossRef]
- Beigel, J.H.; Tomashek, K.M.; Dodd, L.E.; Mehta, A.K.; Zingman, B.S.; Kalil, A.C.; Hohmann, E.; Chu, H.Y.; Luetkemeyer, A.; Kline, S.; et al. Remdesivir for the Treatment of Covid-19—Final Report. N. Engl. J. Med. 2020, 383, 1813–1826. [Google Scholar] [CrossRef] [PubMed]
- Combs, S.E.; Belka, C.; Niyazi, M.; Corradini, S.; Pigorsch, S.; Wilkens, J.; Grosu, A.L.; Guckenberger, M.; Ganswindt, U.; Bernhardt, D. First statement on preparation for the COVID-19 pandemic in large German Speaking University-based radiation oncology departments. Radiat. Oncol. 2020, 15, 74. [Google Scholar] [CrossRef] [PubMed]
- Simcock, R.; Thomas, T.V.; Estes, C.; Filippi, A.R.; Katz, M.A.; Pereira, I.J.; Saeed, H. COVID-19: Global radiation oncology’s targeted response for pandemic preparedness. Clin. Transl. Radiat. Oncol. 2020, 22, 55–68. [Google Scholar] [CrossRef] [PubMed]
- Kalapurakal, J.A.; Zafirovski, A.; Smith, J.; Fisher, P.; Sathiaseelan, V.; Barnard, C.; Rademaker, A.W.; Rave, N.; Mittal, B.B. A comprehensive quality assurance program for personnel and procedures in radiation oncology: Value of voluntary error reporting and checklists. Int. J. Radiat. Oncol. Biol. Phys. 2013, 86, 241–248. [Google Scholar] [CrossRef] [PubMed]
- PRO. Special issue of PRO is dedicated to saftey. Pract. Radiat. Oncol. 2015, 5, 277. [Google Scholar]
- IAEA. Lessons Learned from Accedental Exposures in Radiotherapy; Safety Reports Series No. 17; IAEA: Vienna, Austria, 2000. [Google Scholar]
- Das, I.J.; Andersen, A. Equipment and Software: Commissioning from the Quality and Saftey perspective. In Quality and Saftey in Radiation Oncology, Implementing Tools and Best Practices for Patients, Providers and Payers; Dicker, A.P., Williams, T.R., Ford, E.C., Eds.; Demos Medical: New York, NY, USA, 2017; pp. 73–84. [Google Scholar]
- Zietman, A.L.; Palta, J.R.; Steinberg, M.L. Saftey Is No Accident: A Framework for Quality Radiation Oncology and Care; American Society for Radiation Oncology: Fairfax, VA, USA, 2012. [Google Scholar]
- Hsiang, S.; Allen, D.; Annan-Phan, S.; Bell, K.; Bolliger, I.; Chong, T.; Druckenmiller, H.; Huang, L.Y.; Hultgren, A.; Krasovich, E.; et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature 2020. [Google Scholar] [CrossRef]
- Cobianchi, L.; Dal Mas, F.; Peloso, A.; Pugliese, L.; Massaro, M.; Bagnoli, C.; Angelos, P. Planning the Full Recovery Phase: An Antifragile Perspective on Surgery After COVID-19. Ann. Surg. 2020, 272, e296–e299. [Google Scholar] [CrossRef] [PubMed]
- Angelos, P. Surgeons, Ethics, and COVID-19: Early Lessons Learned. J. Am. Coll. Surg. 2020, 230, 1119–1120. [Google Scholar] [CrossRef]
- Kuderer, N.M.; Choueiri, T.K.; Shah, D.P.; Shyr, Y.; Rubinstein, S.M.; Rivera, D.R.; Shete, S.; Hsu, C.Y.; Desai, A.; de Lima Lopes, G., Jr.; et al. Clinical impact of COVID-19 on patients with cancer (CCC19): A cohort study. Lancet 2020, 395, 1907–1918. [Google Scholar] [CrossRef]
- Ameri, A.; Ameri, P.; Rahnama, N.; Mokhtari, M.; Sedaghat, M.; Hadavand, F.; Bozorgmehr, R.; Haghighi, M.; Taghizadeh-Hesary, F. Low-Dose Whole-Lung Irradiation for COVID-19 Pneumonia: Final Results of a Pilot Study. Int. J. Radiat. Oncol. Biol. Phys. 2021, 109, 859–866. [Google Scholar] [CrossRef]
- Das, I.J.; Kalapurakal, J.A.; Mittal, B.B. Caution warranted for low-dose radaition therapy for Covid-19. Br. J. Radiol. 2021, 93, 20200466. [Google Scholar] [CrossRef]
- Barcellini, A.; Filippi, A.R.; Dal Mas, F.; Cobianchi, L.; Corvò, R.; Price, P.; Orlandi, E. To a new normal in radiation oncology: Looking back and planning forward. Tumori 2020, 106, 440–444. [Google Scholar] [CrossRef]
- Thomson, D.J.; Palma, D.; Guckenberger, M.; Balermpas, P.; Beitler, J.J.; Blanchard, P.; Brizel, D.; Budach, W.; Caudell, J.; Corry, J.; et al. Practice Recommendations for Risk-Adapted Head and Neck Cancer Radiation Therapy During the COVID-19 Pandemic: An ASTRO-ESTRO Consensus Statement. Int. J. Radiat. Oncol. Biol. Phys. 2020, 107, 618–627. [Google Scholar] [CrossRef]
- Reuter-Oppermann, M.; Müller-Polyzou, R.; Wirtz, H.; Georgiadis, A. Influence of the pandemic dissemination of COVID-19 on radiotherapy practice: A flash survey in Germany, Austria and Switzerland. PLoS ONE 2020, 15, e0233330. [Google Scholar] [CrossRef] [PubMed]
- Wei, W.; Zheng, D.; Lei, Y.; Wu, S.; Verma, V.; Liu, Y.; Wei, X.; Bi, J.; Hu, D.; Han, G. Radiotherapy workflow and protection procedures during the Coronavirus Disease 2019 (COVID-19) outbreak: Experience of the Hubei Cancer Hospital in Wuhan, China. Radiother Oncol. 2020, 148, 203–210. [Google Scholar] [CrossRef]
- Hollander, J.E.; Davis, T.M.; Doarn, C.; Goldwater, J.C.; Klasko, S.; Lowery, C.; Papanagnou, D.; Rasmussen, P.; Sites, F.D.; Stone, D.; et al. Recommendations from the First National Academic Consortium of Telehealth. Popul. Health Manag. 2018, 21, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Hollander, J.E.; Carr, B.G. Virtually Perfect? Telemedicine for Covid-19. N. Engl. J. Med. 2020, 382, 1679–1681. [Google Scholar] [CrossRef]
- Schneider, E.C. Failing the Test—The Tragic Data Gap Undermining the U.S. Pandemic Response. N. Engl. J. Med. 2020, 383, 299–302. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Das, I.J.; Kalapurakal, J.A.; Strauss, J.B.; Zawislak, B.R.; Gopalakrishnan, M.; Bajaj, A.; Mittal, B.B. Adaptability and Resilience of Academic Radiation Oncology Personnel and Procedures during COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 5095. https://doi.org/10.3390/ijerph18105095
Das IJ, Kalapurakal JA, Strauss JB, Zawislak BR, Gopalakrishnan M, Bajaj A, Mittal BB. Adaptability and Resilience of Academic Radiation Oncology Personnel and Procedures during COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(10):5095. https://doi.org/10.3390/ijerph18105095
Chicago/Turabian StyleDas, Indra J., John A. Kalapurakal, Jonathan B. Strauss, Brian R. Zawislak, Mahesh Gopalakrishnan, Amishi Bajaj, and Bharat B. Mittal. 2021. "Adaptability and Resilience of Academic Radiation Oncology Personnel and Procedures during COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 10: 5095. https://doi.org/10.3390/ijerph18105095
APA StyleDas, I. J., Kalapurakal, J. A., Strauss, J. B., Zawislak, B. R., Gopalakrishnan, M., Bajaj, A., & Mittal, B. B. (2021). Adaptability and Resilience of Academic Radiation Oncology Personnel and Procedures during COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(10), 5095. https://doi.org/10.3390/ijerph18105095






