Abstract
Although some studies showed that lifestyle was associated with oral health behavior, few studies investigated the association between household type and oral health behavior. The aim of this prospective cohort study was to investigate the association between household type, oral health behavior, and periodontal status among Japanese university students. Data were obtained from 377 students who received oral examinations and self-questionnaires in 2016 and 2019. We assessed periodontal status using the percentage of bleeding on probing (%BOP), probing pocket depth, oral hygiene status, oral health behaviors, and related factors. We used structural equation modeling to determine the association between household type, oral health behaviors, gingivitis, and periodontitis. At follow-up, 252 students did not live with their families. The mean ± standard deviation of %BOP was 35.5 ± 24.7 at baseline and 32.1 ± 25.3 at follow-up. In the final model, students living with their families were significantly more likely to receive regular dental checkup than those living alone. Regular checkup affected the decrease in calculus. The decrease in calculus affected the decrease in %BOP over 3 years. Living with family was directly associated with regular dental checkups and indirectly contributed to gingival status among Japanese university students.
1. Introduction
After university admission, university students obtain more freedom and independence. The beginning of university school life is often the first time that young people assume the responsibility to choose daily habits. Usually, university students in Japan are divided into two categories according to household type: Those who continue to live with their family and those who live far from their usual residence and their family. In Japan, about 60% of national and public university students live alone apart from their family [1]. Some students living apart from their families easily develop negative life habits [2]. The young adult period at the university may influence future lifestyle choices, health, and quality of life. Therefore, proper lifestyle choices for university students are important for good health later in life.
Previous studies [3,4,5,6] reported the association between living alone and lifestyle. Some cross-sectional and cohort studies reported that living alone was a risk factor of harmful lifestyle habits for university students, such as eating choices (food type) [3,4,5] and alcohol consumption [6]. Another cross-sectional study showed that university students who lived with their families had a greater chance of having good oral health-related dietary behaviors than those who lived alone [7]. In the field of dentistry, some cross-sectional and cohort studies mentioned that adults living alone were less likely to receive dental checkups [8,9]. However, few cohort studies investigated the association between living alone, oral health behavior, and oral diseases.
Among oral diseases, periodontal disease, including gingivitis and periodontitis, is one of the major diseases among young adults. It is an inflammatory disease of soft and/or hard tissues surrounding the tooth that is caused by the accumulation of bacterial biofilm (dental plaque) [10]. Periodontal disease is a risk factor for tooth loss [11]. Thus, prevention of periodontal disease, especially in the early stage or young adulthood, is very important.
Avoiding plaque accumulation with good oral hygiene behavior prevents periodontal disease. Some previous studies reported that oral health behaviors such as tooth brushing, dental floss use, and regular dental checkup affect oral hygiene and periodontal status in university students and adults [12,13,14].
Therefore, we hypothesized that university students living alone away from their families would have worse oral health behaviors and subsequently develop periodontal disease, compared with those living with families. The purpose of this cohort study was to analyze the association between household type (continuing to living with family or living alone far from family), oral health behavior, and periodontal status in university students.
2. Materials and Methods
2.1. Ethics Statement
The protocol of this study was approved by the Ethics Committee of Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences (No. 1060). All methods were performed in accordance with the Declaration of Helsinki. Informed consent was verbally obtained from each participant. Study reporting conformed to STROBE guidelines.
2.2. Study Population
We estimated sample size using G*Power and calculated the minimum sample size. We set an alpha of 0.05, power (1−β) of 0.80, and an effect size of 0.31 based on our preliminary research. The sample size was 264.
First-year students volunteered to receive oral examinations and answer self-reported questionnaires at the Health Service Center of Okayama University in April 2016 (baseline). Participants were recruited from all faculties (Faculties of Letters, Education, Law, Economics, Science, Pharmaceutical Sciences, Engineering, Environmental Science and Technology, Agriculture, Medicine, and Dentistry). After a 3-year follow-up, students volunteered to receive the oral examination and answer the questionnaire again (April 2019).
Inclusion criteria were students aged < 20 years and students who provided complete data at baseline. Exclusion criteria were students who had already lived apart from their family before university admission and students who provided incomplete data. Furthermore, we excluded students who had a history of smoking because smoking was expected to affect periodontal status [10]. We treated the data of students who did not receive the oral examination at follow-up as missing data. We widely promoted students to receive oral examinations to prevent selection bias due to loss of follow-up.
2.3. Self-Questionnaires
A self-administered questionnaire was delivered to each student before participating in dental examinations at baseline and follow-up. In addition to sex and age, the questionnaire included the following items. The students were asked about the following oral health behaviors: Daily frequency of tooth brushing (≥two times/≤one time); dental floss use (yes/no); receiving regular dental checkup (yes/no) [12,14,15]; and household type (living with family/living alone).
2.4. Oral Examination
Twelve dentists (D.E., T.Y., K.K., M.Y-T., A.T., A.Y., Y.U-F., D.F., T.K., N.T., K.F., and H.S.) examined oral status at baseline and follow-up. The following 10 teeth were selected for periodontal examination: Two molars in each posterior sextant and the upper right and lower left central incisors. The periodontal status was assessed using the Community Periodontal Index (CPI) [16] using a CPI probe (YDM, Tokyo, Japan) to evaluate 6 sites on each tooth (mesio-buccal, mid-buccal, disto-buccal, disto-lingual, mid-lingual, and mesio-lingual). Bleeding on probing (BOP) was an earlier and more sensitive indicator of inflammation than probing depth [17]. Therefore, in this study, the percentage of teeth exhibiting BOP (%BOP) was assessed among the 10 examined teeth using a CPI probe as an earlier sign of periodontal disease or gingivitis [12,14]. The level of dental plaque and calculus was assessed using the Debris Index-Simplified (DI-S) and Calculus Index-Simplified (CI-S) of Oral Hygiene Index-Simplified (OHI-S) [18]. Periodontal disease was defined using pocket scores of CPI criteria: Presence of probing pocket depth (PPD) ≥ 4 mm (pocket score = 1 or 2) at baseline and follow-up. After training the examiners, the CPI score in the 10 teeth was recorded and repeated within a 2-week interval in 2 volunteers. Intra- and inter-examiner reliabilities, evaluated by κ statistics, of CPI score were >0.8.
2.5. Statistical Analyses
Statistical analyses were conducted using SPSS version 22 (IBM, Tokyo, Japan). The normality of data was investigated by the Shapiro–Wilk test. We did not confirm the normal distribution of each value. The chi-squared test and Mann–Whitney U test were used to determine the significance of differences in sex, age, oral health behavior (tooth brushing frequency, dental floss use, and regular dental checkup), and oral status (DI-S, CI-S, %BOP and PPD). Values of p < 0.05 were considered significantly different.
Pathway analysis was performed to reveal the process from household type, oral health behavior, oral hygiene status, to periodontal status. We estimated an initial model (full model) with all the hypothesized pathways. Figure 1 shows an ideal model based on our hypothesis. Household type and oral health behavior indices were categorical indices. Changes in DI-S, CI-S, and %BOP during the 3-year study period were calculated by subtracting the baseline value from the follow-up value. These values were used as continuous variables. Change in PPD was divided into 3 groups according to the presence or absence of periodontal pockets of ≥ 4 mm at baseline and follow-up: (1) Pocket score = 0 at follow-up; (2) pocket score = 1 or 2 at baseline and follow-up; (3) pocket score = 0 at baseline, and 1 or 2 at follow-up, which was used as a categorical variable.
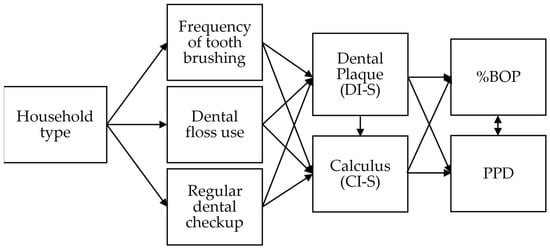
Figure 1.
Pathway based on hypothesis showing the association between household type, oral health behavior, oral hygiene status; Debris Index-Simplified (DI-S) and Calculus Index-Simplified (CI-S), percentage of bleeding on probing (%BOP), and probing pocket depth (PPD).
Mplus version 8.2 software (Muthén and Muthén, Los Angeles, CA, USA) was used for pathway analysis. Continuous and categorical variables were included in our data. Therefore, the pathway analysis was performed using weighted least-squares parameter estimates (WLSMV). WLSMV uses a diagonal weight matrix with robust standard errors and mean and variance adjusted chi-squared test statistics. The goodness of fit of the model was assessed using the comparative fit index (CFI), root mean square error of approximation (RMSEA), and the Tucker–Lewis coefficient (TLI) [12,19]. An RMSEA value < 0.05 suggested adequate fit, whereas CFI and TLI represented incremental fit; values > 0.95 indicated an adequate fit, whereas those > 0.90 were still acceptable [19,20]. Non-significant paths were removed in a step-by-step approach.
3. Results
Figure 2 shows a flowchart of participants included in this 3-year cohort study from baseline to follow-up. At baseline, 2174 students received voluntary oral examinations and answered self-reported questionnaires. We selected 2026 students who met the inclusion criteria. At follow-up, we excluded 1649 students who did not undergo an oral examination and matched exclusion criteria. Finally, we analyzed 377 students (follow-up rate, 18.6%).
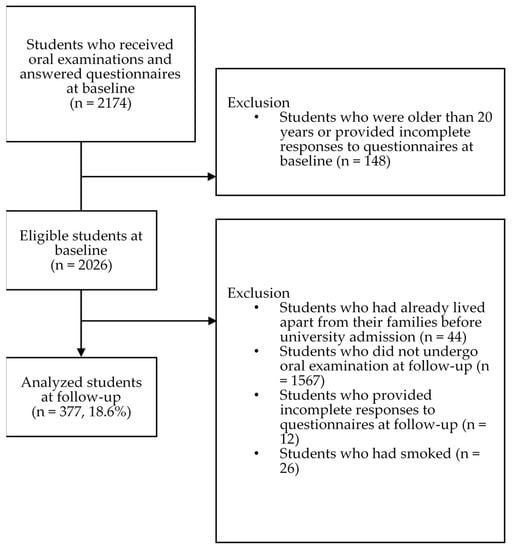
Figure 2.
Flowchart of students included in analyses.
Table 1 shows the characteristics of the participants. This study analyzed data from 377 participants (187 males and 190 females; aged 18–19 years at baseline). At follow-up, 252 students (66.8%) did not live with their families (133 males, 52.8%; 119 females, 47.2%). Mean %BOP value was 35.5 ± 24.7 (mean ± standard deviation) at baseline and 32.1 ± 25.3% at follow-up.

Table 1.
Participant characteristics (n = 377).
Table 2 shows the results of self-questionnaires and the oral examination according to the two household types at follow-up. At baseline and follow-up, household type was not associated with sex, age, daily frequency of tooth brushing, or dental floss use (p > 0.05). At follow-up, participants who were living with their families reported significantly greater regular dental checkups than participants who were not (p = 0.004); no such difference was observed at baseline. At baseline and follow-up, there were no significant differences in DI-S, CI-S, OHI-S, %BOP, and PPD between students living with family and students living alone.

Table 2.
Differences in sex, age, oral health behavior, and oral status by household type at baseline and follow-up.
The final model (Figure 3) was estimated with only statistically significant paths retained. Figure 3 shows parameter estimates for the final structural model. The final model exhibited good fit (χ2 = 2.366; df = 3; p = 0.500; CFI = 1.000; TLI = 1.032; RMSEA = 0.000 [0.000–0.079]). The model indicated that (1) students who lived with their families were significantly more likely to receive regular dental checkups than those who lived alone; (2) regular checkup affected the decrease in calculus, and (3) the decrease in calculus affected the decrease in %BOP over the 3-year study period.
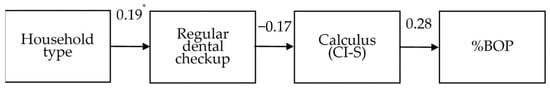
Figure 3.
Pathway based on structural equation modeling showing the association between household type, oral health behavior, oral hygiene status, and the percentage of bleeding on probing (%BOP). * Values above single-headed arrows indicate standardized coefficients.
4. Discussion
To the best of our knowledge, this study is the first prospective cohort study to investigate the association between household type, oral health behavior, and periodontal status in young adults using the pathway analysis. Pathway analysis enables variables to act both as independent and dependent variables and explore the complex causal relationship involved in disease processes [21]. We showed that students who lived with their families were significantly more likely to receive regular dental checkups than those who lived alone. Receiving regular dental checkups directly affected the decrease in calculus. The decrease in calculus, in turn, directly affected the decrease in %BOP (gingival status) over the 3-year study period. After all, the household type was indirectly associated with %BOP through regular dental checkups and calculus (CI-S).
Living with families was directly associated with a regular dental checkup. Oral health behaviors of students living with their families may be influenced by familial oral health behaviors, and students may be encouraged to receive regular dental checkups. A previous study reported that parents’ dental visits within the previous year significantly affected regular dental checkups for secondary school students [22]. Moreover, adults living with a partner or spouse enhanced the chance of receiving dental checkups [8,9].
Living away from family may have a negative effect on receiving regular dental checkups through an indirect factor; the financial difficulties of students living alone. Living alone away from family may increase financial burden because of increased costs related to living alone compared to living with others [23]. Socioeconomic status was associated with regular dental checkups, although the participants in these reports were not university students [13,24,25].
Receiving regular dental checkups affected the decrease in calculus in this study. Our result supports the findings of previous studies indicating a positive effect of a dental checkup on oral hygiene status [12,13,14]. According to previous studies, tooth brushing, dental floss use, and receiving regular dental checkups were significantly associated with good oral hygiene status in Japanese university students [12,14]. Oral health education from dental clinics showed to be effective in improving oral health behavior, knowledge, and oral hygiene status of adolescents [12,14,26]. Dentists play an important role in the prevention of oral disease of general people [27,28]. Continuing oral health education effectively maintained oral health behavior, including regular dental checkups [29,30,31]. Taken together, it is quite reasonable that receiving regular dental checkups affected the decrease in calculus.
In the final model, the decrease in calculus affected the decrease in %BOP. Our result partially supports those of previous studies [12,14], indicating a significant association between oral hygiene status and %BOP in Japanese university students. By contrast, the decrease in dental plaque did not affect the decrease in %BOP, which is inconsistent with the results of previous studies [12,14]. Gingivitis is caused by the continuous accumulation of dental plaque [10], but DI-S is closely related to oral hygiene status immediately before data acquisition. CI-S may be more effective as an indicator of current gingivitis rather than DI-S.
The results of this study might be clinically relevant. When clinicians encounter younger patients living away from their families, increased efforts may be needed to prevent periodontal disease. This work was an observational study. Further studies are, therefore, needed to clarify whether clinical interventions can help prevent periodontal disease in young people for the young living alone.
In this final model, there was no relationship between living alone and tooth brushing or dental floss use. Although no such significant associations have been observed in adults or university students in previous studies, oral self-care such as tooth brushing and dental floss use may not be affected by familial behaviors compared to the effect on visiting the dental office. Furthermore, this result may be influenced by floor and ceiling effects because a very low percentage of students used floss, and a very high percentage of students brushed their teeth twice or more per day.
The change in PPD was excluded in the final model. BOP is an earlier and more sensitive indicator of inflammation than probing depth [17]. Therefore, in this study, the final model may include %BOP but not PPD.
In this study, university students’ oral health behavior tended to be better than in the previous prospective 3-year cohort studies in university students [32,33]. In the present study, 30.2% of students answered received regular dental checkups at follow-up. On the other hand, the previous 3-year cohort studies showed a lower prevalence (10.5–14.0%). The percentage of students who answered that they brushed their teeth more than once (87.5 %) was slightly higher than the previous cohort studies (75.0–84.7%). The percentage of students who answered they used dental floss (16.7%) was also slightly higher than the previous cohort studies (10.7–15.4%) [32,33].
There are some limitations associated with our study. First, we did not investigate whether students’ families had a dental checkup and the recall interval for a dental checkup. Previous studies investigated the association between secondary school students’ regular dental checkups and parents’ most recent dental visits [22]. Second, we did not consider factors that may be associated with periodontal diseases, such as students’ faculties [34], students’ and their families’ education level [35,36], socioeconomic status [37,38], psychosocial factors [39], and social capital [15], in this study. Future studies are needed to reveal these effects. Third, there may have been a selection bias, given the low follow-up rate. In this study, analyzed students (n = 377) comprised 18.6% of all eligible students (n = 2026). The response rate in this study was within the previous prospective 3-year cohort studies in university students (13.4–25.7%) [32,33,40,41]. No significant differences were seen in %BOP and sex ratios between analyzed and non-analyzed students (377 vs. 1649 students; Mann–Whitney U test: p > 0.05, chi-squared test: p > 0.05). Any effects of a selection bias would have, therefore, been negligible. Forth, we examined only 10 teeth in the oral examination, which might have led to under- or overestimation. We may have a bias that a full examination of all teeth about dental plaque, calculus, PPD, and BOP can be avoided. Finally, all participants were recruited from Okayama University students. This may limit the ability to extrapolate these findings to the general young population.
5. Conclusions
Living with family was directly associated with regular dental checkups and indirectly associated with gingival status among Japanese university students. When clinicians encounter younger patients living away from their families, increased efforts may be needed to prevent periodontal disease.
Author Contributions
Conceptualization, M.N., D.E., and M.M.; methodology, M.N., D.E., and M.M.; validation, M.N.; formal analysis, M.N.; investigation, M.N., D.E., K.K., A.Y., Y.U.-F., D.F., T.K., N.T., H.S., and M.M.I.; resources, M.M.; data curation, M.N., D.E., and N.T.; writing—original draft preparation, M.N.; writing—review and editing, all authors; visualization, M.M.; supervision, M.M.; project administration, Y.I. and M.M.; funding acquisition, M.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of Okayama University Graduate School of Medicine, Dentistry, and Pharmaceutical Sciences (No. 1060).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to ethical issues.
Acknowledgments
The authors are grateful to Toshiki Yoneda (Dental Clinic, Okayama, Japan) for data collection and Ayano Taniguchi-Tabata (Dental Clinic, Okayama, Japan) for checking the accuracy of the data, statistical methods employed, and interpretation of the data.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Independent Administrative Institution Japan Student Services Organization, Japan. Life Style Survey (in Japanese). 2016. Available online: https://www.jasso.go.jp/about/statistics/gakusei_chosa/__icsFiles/afieldfile/2018/06/01/data16_all.pdf (accessed on 30 November 2020).
- Fujitsuka, C.; Fujiwara, Y.; Ishida, H.; Yonetani, S.; Kimura, K. Three Month Survey of Life Habits in College Freshmen. Kawasaki Med. Welf. J. 2002, 12, 321–330. [Google Scholar] [CrossRef]
- Lupi, S.; Bagordo, F.; Stefanati, A.; Grassi, T.; Piccinni, L.; Bergamini, M.; De Donno, A. Assessment of lifestyle and eating habits among undergraduate students in northern Italy. Ann. Ist. Super Sanità 2015, 51, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Papadaki, A.; Hondros, G.; Scott, J.A.; Kapsokefalou, M. Eating habits of University students living at, or away from home in Greece. Appetite 2007, 49, 169–176. [Google Scholar] [CrossRef] [PubMed]
- Kremmyda, L.S.; Papadaki, A.; Hondros, G.; Kapsokefalou, M.; Scott, J.A. Differentiating between the effect of rapid dietary acculturation and the effect of living away from home for the first time, on the diets of Greek students studying in Glasgow. Appetite 2008, 50, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Moure-Rodriguez, L.; Carbia, C.; Lopez-Caneda, E.; Corral Varela, M.; Cadaveira, F.; Caamaño-Isorna, F. Trends in alcohol use among young people according to the pattern of consumption on starting university: A 9-year follow-up study. PLoS ONE 2018, 13, e019374. [Google Scholar] [CrossRef] [PubMed]
- Enshaei, Z.; Feizi, A.; Saied-Moallemi, Z. Oral health behaviours and oral health-related dietary behaviours: The interrelationship and determinants by latent class analysis. Community Dent. Health 2018, 35, 173–178. [Google Scholar] [CrossRef]
- Erdsiek, F.; Waury, D.; Brzoska, P. Oral health behaviour in migrant and non-migrant adults in Germany: The utilization of regular dental check-ups. BMC Oral Health 2017, 17, 84. [Google Scholar] [CrossRef]
- Christensen, L.B.; Petersen, P.E.; Steding-Jessen, M. Consumption of dental services among adults in Denmark 1994–2003. Eur. J. Oral Sci. 2007, 115, 174–179. [Google Scholar] [CrossRef]
- Pihlstrom, B.L.; Michalowicz, B.S.; Johnson, N.W. Periodontal diseases. Lancet 2005, 366, 1809–1820. [Google Scholar] [CrossRef]
- Lang, N.P.; Schätzle, M.A.; Löe, H. Gingivitis as a risk factor in periodontal disease. J. Clin. Periodontol. 2009, 36, 3–8. [Google Scholar] [CrossRef]
- Mizutani, S.; Ekuni, D.; Furuta, M.; Tomofuji, T.; Irie, K.; Azuma, T.; Kojima, A.; Nagase, J.; Iwasaki, Y.; Morita, M. Effects of self-efficacy on oral health behaviours and gingival health in university students aged 18- or 19-years-old. J. Clin. Periodontol. 2012, 39, 844–849. [Google Scholar] [CrossRef] [PubMed]
- Lang, W.P.; Farghaly, M.M.; Ronis, D.L. The relation of preventive dental behaviors to periodontal health status. J. Clin. Periodontol. 1994, 21, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Furuta, M.; Ekuni, D.; Irie, K.; Azuma, T.; Tomofuji, T.; Ogura, T.; Morita, M. Sex differences in gingivitis relate to interaction of oral health behaviors in young people. J. Periodontol. 2011, 82, 558–565. [Google Scholar] [CrossRef] [PubMed]
- Furuta, M.; Ekuni, D.; Takao, S.; Suzuki, E.; Morita, M.; Kawachi, I. Social capital and self-rated oral health among young people. Community Dent. Oral Epidemiol. 2012, 40, 97–104. [Google Scholar] [CrossRef]
- Ainamo, J.; Barmes, D.; Beagrie, G.; Cutress, T.; Martin, J.; Sardo-Infirri, J. Development of the World Health Organization (WHO) community periodontal index of treatment needs (CPITN). Int. Dent. J. 1982, 32, 281–291. [Google Scholar] [PubMed]
- Greenstein, G. The role of bleeding upon probing in the diagnosis of periodontal disease: A literature review. J. Periodontol. 1984, 55, 684–688. [Google Scholar] [CrossRef] [PubMed]
- Greene, J.C.; Vermillion, J.R. The simplified oral hygiene index. J. Am. Dent. Assoc. 1964, 68, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Hu, L.T.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Browne, M.W.; Cudeck, R. Alternative Ways of Assessing Model Fit. In Testing Structural Equation Models; Sage Publications: Newbury Park, CA, USA, 1993; pp. 136–162. [Google Scholar]
- Kojima, A.; Ekuni, D.; Mizutani, S.; Furuta, M.; Irie, K.; Azuma, T.; Tomofuji, T.; Iwasaki, Y.; Morita, M. Relationships between self-rated oral health, subjective symptoms, oral health behavior and clinical conditions in Japanese university students: A cross-sectional survey at Okayama University. BMC Oral Health 2013, 13, 62. [Google Scholar] [CrossRef]
- Scott, G.; Brodeur, J.M.; Olivier, M.; Benigeri, M. Parental factors associated with regular use of dental services by second-year secondary school students in Quebec. J. Can. Dent. Assoc. 2002, 68, 604–608. [Google Scholar]
- Raymo, J.M. Living alone in Japan: Relationships with happiness and health. Demogr. Res. 2015, 32, 1267–1298. [Google Scholar] [CrossRef] [PubMed]
- Payne, B.J.; Locker, D. Relationship between dental and general health behaviors in a canadian population. J. Public Health Dent. 1996, 56, 198–204. [Google Scholar] [CrossRef]
- Ronis, D.L.; Lang, W.P.; Farghaly, M.M.; Passow, E. Tooth brushing, flossing, and preventive dental visits by detroit-area residents in relation to demographic and socioeconomic factors. J. Public Health Dent. 1993, 53, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Taniguchi-Tabata, A.; Ekuni, D.; Mizutani, S.; Yamane-Takeuchi, M.; Kataoka, K.; Azuma, T.; Tomofuji, T.; Iwasaki, Y.; Morita, M. Associations between dental knowledge, source of dental knowledge and oral health behavior in Japanese university students: A cross-sectional study. PLoS ONE 2017, 12, e0179298. [Google Scholar] [CrossRef] [PubMed]
- Iwamoto, A.; Ishiikawa, Y.; Yagi, M.; Ohuchi, A.; Sato, T.; Fukai, K.; Ando, Y.; Chinushi, N. Changing patterns of behavior related to oral health in dental health examination program for adults that gives priority to risk-funding and health-guidance. J. Dent. Health 2012, 62, 33–40. [Google Scholar] [CrossRef]
- Hugoson, A.; Koch, G.; Göthberg, C.; Helkimo, A.N.; Lundin, S.Å.; Norderyd, O.; Sjödin, B.; Sondell, K. Oral health of individuals aged 3-80 years in Jönköping, Sweden during 30 years (1973-2003) I. Review of findings on dental care habits and knowledge of oral health. Swed. Dent. J. 2005, 29, 125–138. [Google Scholar]
- Anaise, J.Z.; Zilkah, E. Effectiveness of a dental education program on oral cleanliness of schoolchildren in Israel. Community Dent. Oral Epidemiol. 1976, 4, 186–189. [Google Scholar] [CrossRef]
- Hart, E.J.; Behr, M.T. The effects of educational intervention & parental support on dental health. J. Sch. Health 1980, 50, 572–576. [Google Scholar] [CrossRef]
- Angelopoulou, M.V.; Kavvadia, K.; Taoufik, K.; Oulis, C.J. Comparative clinical study testing the effectiveness of school based oral health education using experiential learning or traditional lecturing in 10year-old children. BMC Oral Health 2015, 15, 51. [Google Scholar] [CrossRef][Green Version]
- Mizutani, S.; Ekuni, D.; Tomofuji, T.; Irie, K.; Azuma, T.; Iwasaki, Y.; Morita, M. Self-efficacy and progression of periodontal disease: A prospective cohort study. J. Clin. Periodontol. 2015, 42, 1083–1089. [Google Scholar] [CrossRef]
- Uchida-Fukuhara, Y.; Ekuni, D.; Islam, M.M.; Kataoka, K.; Taniguchi-Tabata, A.; Fukuhara, D.; Toyama, N.; Kobayashi, T.; Fujimori, K.; Sawada, N.; et al. Caries increment and salivary microbiome during university life: A prospective cohort study. Int. J. Environ. Res. Public Health 2020, 17, 3713. [Google Scholar] [CrossRef]
- Dhaifullah, E.; Al-Maweri, S.A.; Al-Motareb, F.; Halboub, E.; Elkhatat, E.; Baroudi, K.; Tarakji, B. Periodontal health condition and associated factors among university students, Yemen. J. Clin. Diagn. Res. 2015, 9, ZC30–ZC33. [Google Scholar] [CrossRef]
- Paulander, J.; Axelsson, P.; Lindhe, J. Association between level of education and oral health status in 35-, 50-, 65- and 75-year-olds. J. Clin. Periodontol. 2003, 30, 697–704. [Google Scholar] [CrossRef]
- Bendoraitienė, E.; Zūbienė, J.; Vasiliauskienė, I.; Saldūnaitė, K.; Andruškevičienė, V.; Basevičienė, N.; Slabšinskienė, E. Periodontal status in 18-year-old Lithuanian adolescents: An epidemiological study. Medicina 2017, 53, 253–258. [Google Scholar] [CrossRef]
- Cronin, A.J.; Claffey, N.; Stassen, L.F. Who is at risk? Periodontal disease risk analysis made accessible for the general dental practitioner. Br. Dent. J. 2008, 205, 131–137. [Google Scholar] [CrossRef]
- Morita, I.; Nakagaki, H.; Yoshii, S.; Tsuboi, S.; Hayashizaki, J.; Igo, J.; Mizuno, K.; Sheiham, A. Gradients in periodontal status in Japanese employed males. J. Clin. Periodontol. 2007, 34, 952–956. [Google Scholar] [CrossRef]
- Genco, R.J.; Ho, A.W.; Grossi, S.G.; Dunford, R.G.; Tedesco, L.A. Relationship of stress, distress, and inadequate coping behaviors to periodontal disease. J. Periodontol. 1999, 70, 711–723. [Google Scholar] [CrossRef]
- Kunitomo, M.; Ekuni, D.; Mizutani, S.; Tomofuji, T.; Irie, K.; Azuma, T.; Yamane, M.; Kataoka, K.; Taniguchi-Tabata, A.; Mizuno, H.; et al. Association between Knowledge about Comprehensive Food Education and Increase in Dental Caries in Japanese University Students: A Prospective Cohort Study. Nutrients 2016, 8, 114. [Google Scholar] [CrossRef]
- Toyama, N.; Ekuni, D.; Taniguchi-Tabata, A.; Kataoka, K.; Yamane-Takeuchi, M.; Fujimori, K.; Kobayashi, T.; Fukuhara, D.; Irie, K.; Azuma, T.; et al. Awareness of clenching and underweight are risk factors for onset of crowding in young adults: A prospective 3-year cohort study. Int. J. Environ. Res. Public Health 2019, 16, 690. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).