Effects of Online Bodyweight High-Intensity Interval Training Intervention and Health Education on the Mental Health and Cognition of Sedentary Young Females
Abstract
1. Introduction
2. Materials and Methods
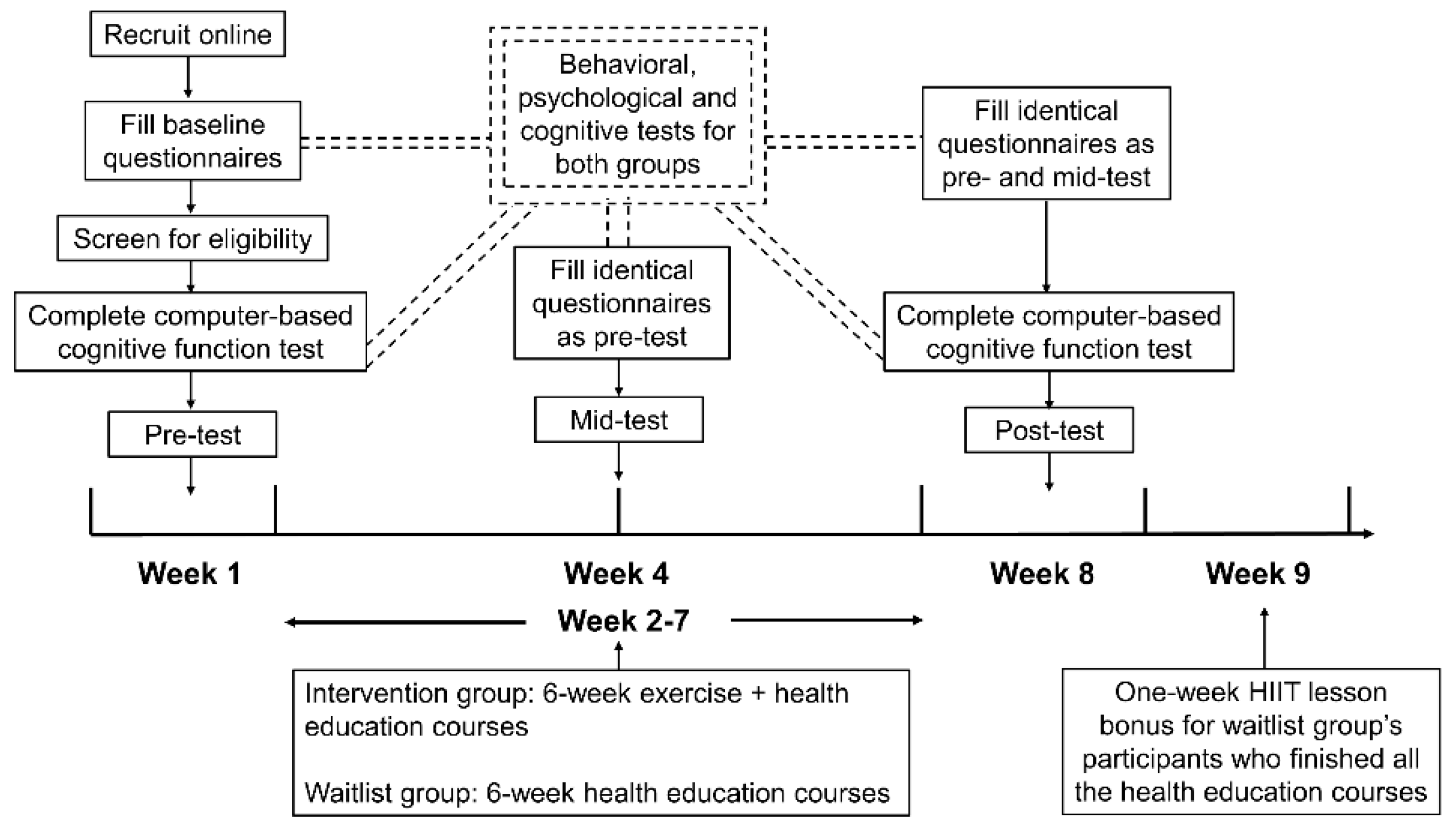
2.1. Designs
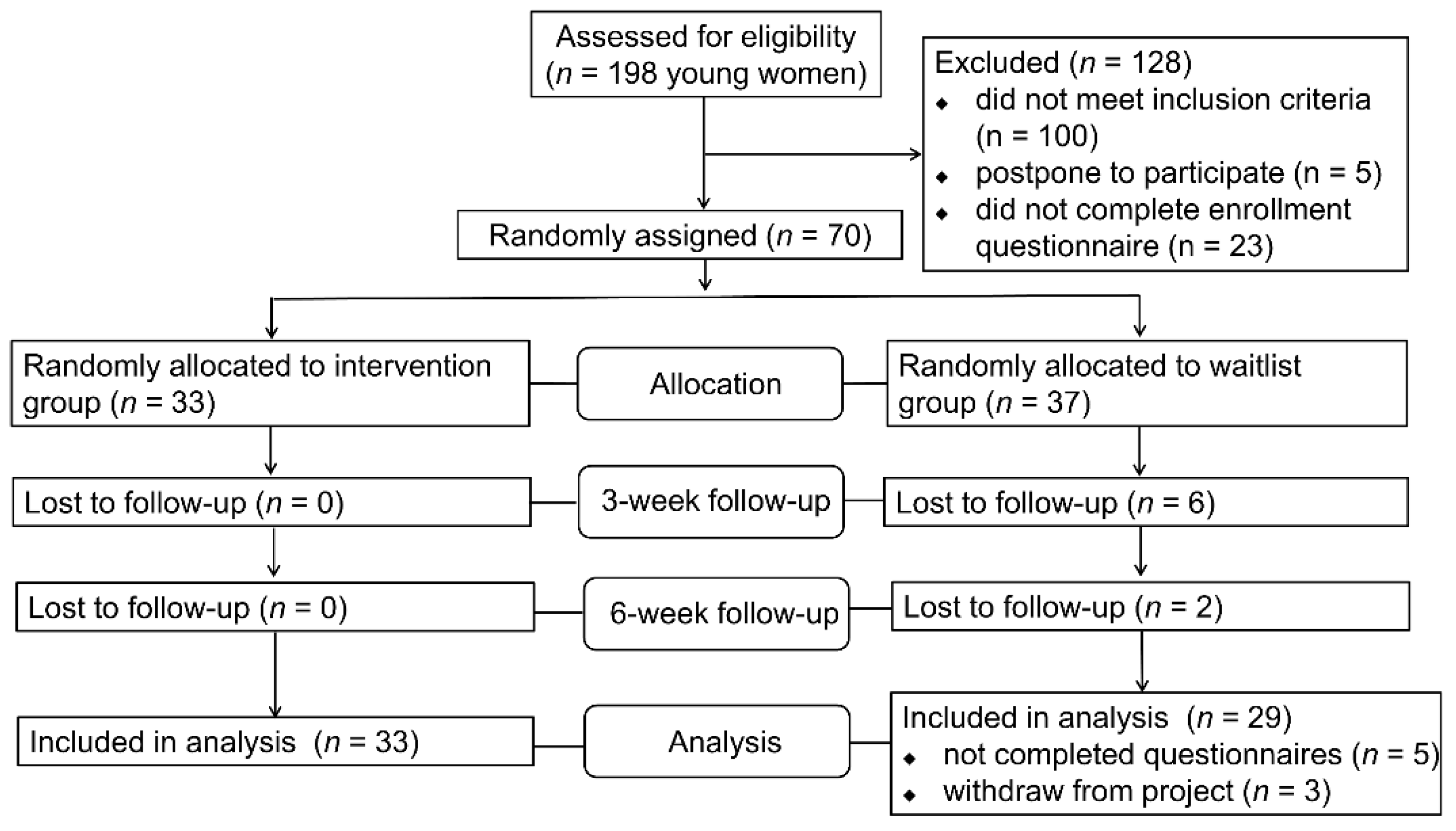
2.2. Participants
2.3. Interventions
2.4. Measurements
2.5. Ethical Consideration
2.6. Statistical Analysis
3. Results
3.1. Characteristics of the Survey Participants
3.2. Effects of the Interventions on Health-Related Behaviors and Mental Health
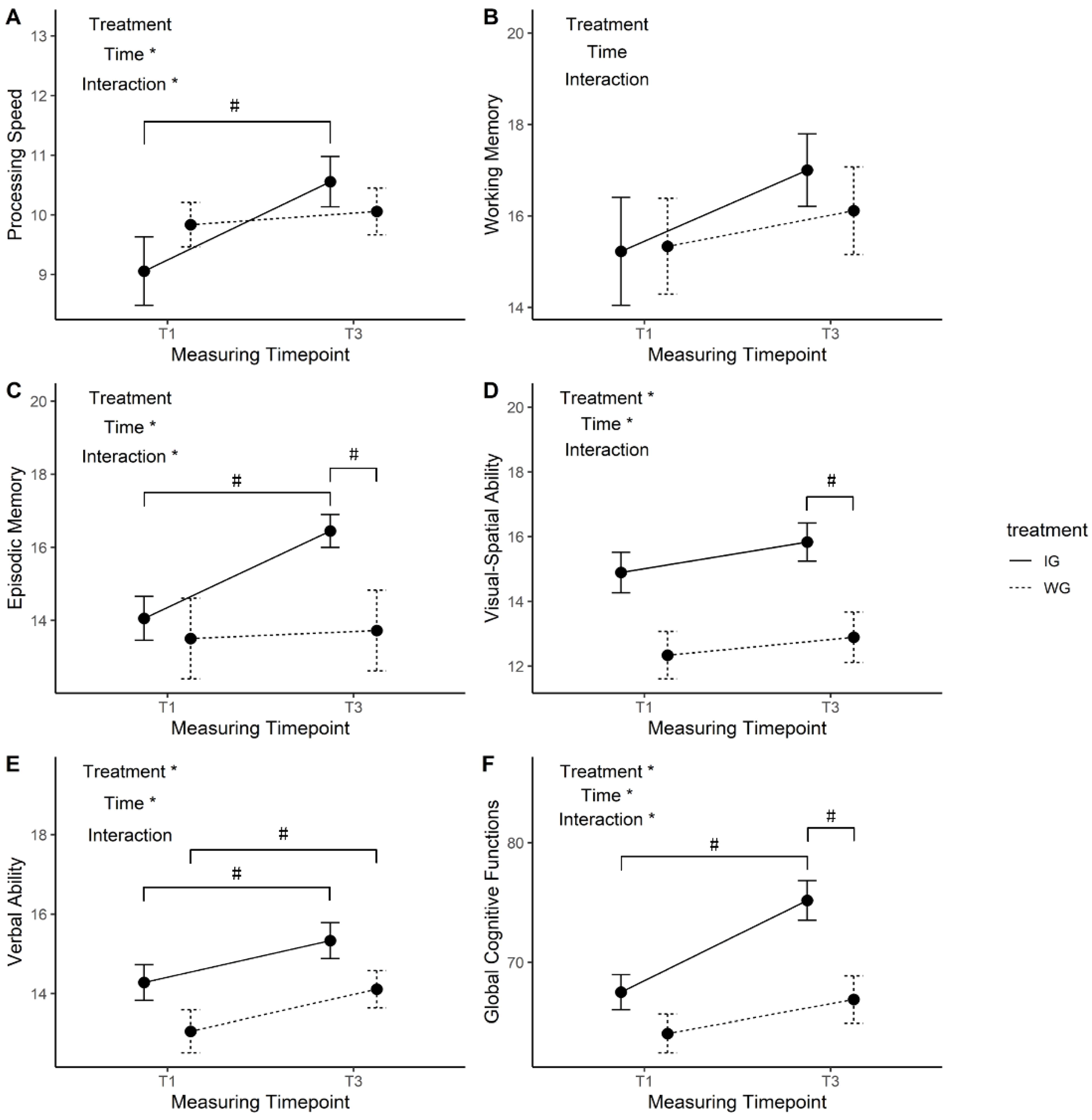
3.3. Changes of Cognitive Function Over the 6-Week Intervention
4. Discussion
4.1. Effects of the Online Intervention on Health-Related Behaviors and Mental Health
4.2. Changes in Domain-Specific and Global Cognition over the Six-Week Online Intervention
4.3. Limitations and Strengths
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thivel, D. Physical Activity, Inactivity, and Sedentary Behaviors: Definitions and Implications in Occupational Health. Front. Public Health 2018, 6, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Caspersen, C.J.; Powell, K.E.; Christenson, G.M. Physical Activity, Exercise, and Physical Fitness: Definitions and Distinctions for Health-Related Research. Public Health Rep. 1985, 100, 126–131. [Google Scholar] [PubMed]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. Exercise and Physical Activity for Older Adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef] [PubMed]
- Warburton, D.E.R. Health benefits of physical activity: The evidence. Can. Med. Assoc. J. 2006, 174, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Pascoe, M.; Bailey, A.P.; Craike, M.; Carter, T.; Patten, R.; Stepto, N.; Parker, A. Physical activity and exercise in youth mental health promotion: A scoping review. BMJ Open Sport Exerc. Med. 2020, 6, e000677. [Google Scholar] [CrossRef] [PubMed]
- Erickson, K.I.; Weinstein, A.M.; Lopez, O.L. Physical Activity, Brain Plasticity, and Alzheimer’s Disease. Arch. Med. Res. 2012, 43, 615–621. [Google Scholar] [CrossRef]
- Bansal, R.; Hellerstein, D.J.; Peterson, B.S. Evidence for neuroplastic compensation in the cerebral cortex of persons with depressive illness. Mol. Psychiatry 2018, 23, 375–383. [Google Scholar] [CrossRef]
- Burdette, J.H.; Laurienti, P.J.; Espeland, M.A.; Morgan, A.; Telesford, Q.; Vechlekar, C.D.; Hayasaka, S.; Jennings, J.M.; Katula, J.A.; Kraft, R.A.; et al. Using network science to evaluate exercise-associated brain changes in older adults. Front. Aging Neurosci. 2010. [Google Scholar] [CrossRef]
- Coelho, F.G.d.M.; Gobbi, S.; Andreatto, C.A.A.; Corazza, D.I.; Pedroso, R.V.; Santos-Galduróz, R.F. Physical exercise modulates peripheral levels of brain-derived neurotrophic factor (BDNF): A systematic review of experimental studies in the elderly. Arch. Gerontol. Geriatr. 2013, 56, 10–15. [Google Scholar] [CrossRef]
- Tremblay, M.S. Sedentary Behavior Research Network (SBRN)—Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef]
- Hamer, M.; Stamatakis, E. Prospective Study of Sedentary Behavior, Risk of Depression, and Cognitive Impairment. Med. Sci. Sports Exerc. 2014, 46, 718–723. [Google Scholar] [CrossRef] [PubMed]
- Falck, R.S.; Davis, J.C.; Liu-Ambrose, T. What is the association between sedentary behaviour and cognitive function? A systematic review. Br. J. Sports Med. 2017, 51, 800–811. [Google Scholar] [CrossRef] [PubMed]
- Bull, F.C.; Bauman, A.E. Physical Inactivity: The “Cinderella” Risk Factor for Noncommunicable Disease Prevention. J. Health Commun. 2011, 16, 13–26. [Google Scholar] [CrossRef] [PubMed]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Edwards, M.K.; Loprinzi, P.D. Experimentally increasing sedentary behavior results in increased anxiety in an active young adult population. J. Affect. Disord. 2016, 204, 166–173. [Google Scholar] [CrossRef]
- Falck, R.S.; Landry, G.J.; Best, J.R.; Davis, J.C.; Chiu, B.K.; Liu-Ambrose, T. Cross-Sectional Relationships of Physical Activity and Sedentary Behavior with Cognitive Function in Older Adults with Probable Mild Cognitive Impairment. Phys. Ther. 2017, 97, 975–984. [Google Scholar] [CrossRef]
- Segar, M.; Jayaratne, T.; Hanlon, J.; Richardson, C.R. Fitting fitness into women’s lives: Effects of a gender-tailored physical activity intervention. Womens Health Issues 2002, 12, 338–347. [Google Scholar] [CrossRef]
- Budde, H.; Schwarz, R.; Velasques, B.; Ribeiro, P.; Holzweg, M.; Machado, S.; Brazaitis, M.; Staack, F.; Wegner, M. The Need for Differentiating between Exercise, Physical Activity, and Training. Autoimmun. Rev. 2016, 15, 110–111. [Google Scholar] [CrossRef]
- Filion, A.J.; Darlington, G.; Chaput, J.-P.; Ybarra, M.; Haines, J. Examining the Influence of a Text Message-Based Sleep and Physical Activity Intervention among Young Adult Smokers in the United States. BMC Public Health 2015, 15, 671. [Google Scholar] [CrossRef]
- Peyman, N.; Rezai-Rad, M.; Tehrani, H.; Gholian-Aval, M.; Vahedian-Shahroodi, M.; Heidarian Miri, H. Digital Media-Based Health Intervention on the Promotion of Women’s Physical Activity: A Quasi-Experimental Study. BMC Public Health 2018, 18, 134. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Jemmott, J.B., III. Mobile App-Based Small-Group Physical Activity Intervention for Young African American Women: A Pilot Randomized Controlled Trial. Prev. Sci. 2019, 20, 863–872. [Google Scholar] [CrossRef] [PubMed]
- The AIBL research group; Brown, B.M.; Peiffer, J.J.; Sohrabi, H.R.; Mondal, A.; Gupta, V.B.; Rainey-Smith, S.R.; Taddei, K.; Burnham, S.; Ellis, K.A.; et al. Intense Physical Activity Is Associated with Cognitive Performance in the Elderly. Transl. Psychiatry 2012, 2, e191. [Google Scholar] [CrossRef]
- Calverley, T.A.; Ogoh, S.; Marley, C.J.; Steggall, M.; Marchi, N.; Brassard, P.; Lucas, S.J.E.; Cotter, J.D.; Roig, M.; Ainslie, P.N.; et al. HIITing the Brain with Exercise: Mechanisms, Consequences and Practical Recommendations. J. Physiol. 2020, 598, 2513–2530. [Google Scholar] [CrossRef] [PubMed]
- Schaun, G.Z.; Pinto, S.S.; Silva, M.R.; Dolinski, D.B.; Alberton, C.L. Whole-Body High-Intensity Interval Training Induce Similar Cardiorespiratory Adaptations Compared with Traditional High-Intensity Interval Training and Moderate-Intensity Continuous Training in Healthy Men. J. Strength Cond. Res. 2018, 32, 2730–2742. [Google Scholar] [CrossRef] [PubMed]
- Gillen, J.B.; Gibala, M.J. Is High-Intensity Interval Training a Time-Efficient Exercise Strategy to Improve Health and Fitness? Appl. Physiol. Nutr. Metab. 2014, 39, 409–412. [Google Scholar] [CrossRef]
- Cao, M.; Quan, M.; Zhuang, J. Effect of High-Intensity Interval Training versus Moderate-Intensity Continuous Training on Cardiorespiratory Fitness in Children and Adolescents: A Meta-Analysis. Int. J. Environ. Res. Public Health 2019, 16, 1533. [Google Scholar] [CrossRef]
- Costigan, S.A.; Eather, N.; Plotnikoff, R.C.; Hillman, C.H.; Lubans, D.R. High-Intensity Interval Training for Cognitive and Mental Health in Adolescents. Med. Sci. Sports Exerc. 2016, 48, 1985–1993. [Google Scholar] [CrossRef]
- Aamot, I.-L.; Forbord, S.H.; Karlsen, T.; Støylen, A. Does Rating of Perceived Exertion Result in Target Exercise Intensity during Interval Training in Cardiac Rehabilitation? A Study of the Borg Scale versus a Heart Rate Monitor. J. Sci. Med. Sport 2014, 17, 541–545. [Google Scholar] [CrossRef]
- Eather, N.; Riley, N.; Miller, A.; Smith, V.; Poole, A.; Vincze, L.; Morgan, P.J.; Lubans, D.R. Efficacy and Feasibility of HIIT Training for University Students: The Uni-HIIT RCT. J. Sci. Med. Sport 2019, 22, 596–601. [Google Scholar] [CrossRef]
- Zamunér, A.R.; Moreno, M.A.; Camargo, T.M.; Graetz, J.P.; Tamburús, N.Y. Assessment of Subjective Perceived Exertion at the Anaerobic Threshold with the Borg CR-10 Scale. J. Sports Sci. Med. 2011, 10, 130–136. [Google Scholar] [PubMed]
- Haddad, M.; Stylianides, G.; Djaoui, L.; Dellal, A.; Chamari, K. Session-RPE Method for Training Load Monitoring: Validity, Ecological Usefulness, and Influencing Factors. Front. Neurosci. 2017, 11, 612. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.; Stewart, S.M. Validity of the International Physical Activity Questionnaire Short Form (IPAQ-SF): A Systematic Review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef]
- Macfarlane, D.J.; Lee, C.C.Y.; Ho, E.Y.K.; Chan, K.L.; Chan, D.T.S. Reliability and Validity of the Chinese Version of IPAQ (Short, Last 7 Days). J. Sci. Med. Sport 2007, 10, 45–51. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Whitt, M.C.; Irwin, M.L.; Swartz, A.M.; Strath, S.J.; O’Brien, W.L.; Bassett, D.R.; Schmitz, K.H.; Emplaincourt, P.O.; et al. Compendium of Physical Activities: An Update of Activity Codes and MET Intensities. Med. Sci. Sports Exerc. 2000, 32, S498–S516. [Google Scholar] [CrossRef]
- Zsido, A.N.; Teleki, S.A.; Csokasi, K.; Rozsa, S.; Bandi, S.A. Development of the Short Version of the Spielberger State—Trait Anxiety Inventory. Psychiatry Res. 2020, 291, 113223. [Google Scholar] [CrossRef]
- Ma, W.-F.; Liu, Y.-C.; Chen, Y.-F.; Lane, H.-Y.; Lai, T.-J.; Huang, L.-C. Evaluation of Psychometric Properties of the Chinese Mandarin Version State-Trait Anxiety Inventory Y Form in Taiwanese Outpatients with Anxiety Disorders: CMSTAI-Y for Patients with Anxiety Disorders. J. Psychiatr. Ment. Health Nurs. 2013, 20, 499–507. [Google Scholar] [CrossRef]
- Wang, Z.; Chen, J.; Boyd, J.E.; Zhang, H.; Jia, X.; Qiu, J.; Xiao, Z. Psychometric Properties of the Chinese Version of the Perceived Stress Scale in Policewomen. PLoS ONE 2011, 6, e28610. [Google Scholar] [CrossRef]
- Lu, W.; Bian, Q.; Wang, W.; Wu, X.; Wang, Z.; Zhao, M. Chinese Version of the Perceived Stress Scale-10: A Psychometric Study in Chinese University Students. PLoS ONE 2017, 12, e0189543. [Google Scholar] [CrossRef]
- Lakens, D. Calculating and Reporting Effect Sizes to Facilitate Cumulative Science: A Practical Primer for t-Tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [PubMed]
- Levine, T.R.; Hullett, C.R. Eta Squared, Partial Eta Squared, and Misreporting of Effect Size in Communication Research. Hum. Commun. Res. 2002, 28, 612–625. [Google Scholar] [CrossRef]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A Novel Coronavirus Outbreak of Global Health Concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef]
- Shah, K.; Kamrai, D.; Mekala, H.; Mann, B.; Desai, K.; Patel, R.S. Focus on Mental Health During the Coronavirus (COVID-19) Pandemic: Applying Learnings from the Past Outbreaks. Cureus 2020, 12. [Google Scholar] [CrossRef]
- Barranco-Ruiz, Y.; Villa-González, E. Health-Related Physical Fitness Benefits in Sedentary Women Employees after an Exercise Intervention with Zumba Fitness®. Int. J. Environ. Res. Public Health 2020, 17, 2632. [Google Scholar] [CrossRef]
- Ornes, L.; Ransdell, L.B. Web-Based Physical Activity Intervention for College-Aged Women. Int. Electron. J. Health Educ. 2007, 10, 126–137. [Google Scholar]
- Prince, S.A.; Saunders, T.J.; Gresty, K.; Reid, R.D. A Comparison of the Effectiveness of Physical Activity and Sedentary Behaviour Interventions in Reducing Sedentary Time in Adults: A Systematic Review and Meta-analysis of Controlled Trials. Obes. Rev. 2014, 15, 905–919. [Google Scholar] [CrossRef]
- O’Dougherty, M.; Hearst, M.O.; Syed, M.; Kurzer, M.S.; Schmitz, K.H. Life Events, Perceived Stress and Depressive Symptoms in a Physical Activity Intervention with Young Adult Women. Ment. Health Phys. Act. 2012, 5, 148–154. [Google Scholar] [CrossRef]
- Gerber, M.; Brand, S.; Herrmann, C.; Colledge, F.; Holsboer-Trachsler, E.; Pühse, U. Increased Objectively Assessed Vigorous-Intensity Exercise Is Associated with Reduced Stress, Increased Mental Health and Good Objective and Subjective Sleep in Young Adults. Physiol. Behav. 2014, 135, 17–24. [Google Scholar] [CrossRef]
- Kramer, A.F.; Erickson, K.I.; Colcombe, S.J. Exercise, Cognition, and the Aging Brain. J. Appl. Physiol. 2006, 101, 1237–1242. [Google Scholar] [CrossRef]
- Hwang, J.; Brothers, R.M.; Castelli, D.M.; Glowacki, E.M.; Chen, Y.T.; Salinas, M.M.; Kim, J.; Jung, Y.; Calvert, H.G. Acute High-Intensity Exercise-Induced Cognitive Enhancement and Brain-Derived Neurotrophic Factor in Young, Healthy Adults. Neurosci. Lett. 2016, 630, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Maddock, R.J.; Casazza, G.A.; Fernandez, D.H.; Maddock, M.I. Acute Modulation of Cortical Glutamate and GABA Content by Physical Activity. J. Neurosci. 2016, 36, 2449–2457. [Google Scholar] [CrossRef] [PubMed]
- Cassilhas, R.C. Physical Exercise, Neuroplasticity, Spatial Learning and Memory. Cell Mol. Life Sci. 2016, 73, 975–985. [Google Scholar] [CrossRef] [PubMed]
- Stillman, C.M.; Cohen, J.; Lehman, M.E.; Erickson, K.I. Mediators of Physical Activity on Neurocognitive Function: A Review at Multiple Levels of Analysis. Front. Hum. Neurosci. 2016, 10, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Pinilla, F.; Hillman, C. The Influence of Exercise on Cognitive Abilities. Front. Psychol. 2013, 3, 403–428. [Google Scholar]
- Leavitt, V.M.; Cirnigliaro, C.; Cohen, A.; Farag, A.; Brooks, M.; Wecht, J.M.; Wylie, G.R.; Chiaravalloti, N.D.; DeLuca, J.; Sumowski, J.F. Aerobic Exercise Increases Hippocampal Volume and Improves Memory in Multiple Sclerosis: Preliminary Findings. Neurocase 2014, 20, 695–697. [Google Scholar] [CrossRef]
- Van Praag, H.; Christie, B.R.; Sejnowski, T.J.; Gage, F.H. Running Enhances Neurogenesis, Learning, and Long-Term Potentiation in Mice. Proc. Natl. Acad. Sci. USA 1999, 96, 13427–13431. [Google Scholar] [CrossRef]
- Voss, M.W.; Prakash, R.S.; Erickson, K.I.; Basak, C.; Chaddock, L.; Kim, J.S.; Alves, H.; Heo, S.; Szabo, A.; White, S.M.; et al. Plasticity of Brain Networks in a Randomized Intervention Trial of Exercise Training in Older Adults. Front. Aging Neurosci. 2010, 2, 32. [Google Scholar] [CrossRef]
- Sink, K.M.; Espeland, M.A.; Castro, C.M.; Church, T.; Cohen, R.; Dodson, J.A.; Guralnik, J.; Hendrie, H.C.; Jennings, J.; Katula, J.; et al. Effect of a 24-Month Physical Activity Intervention vs Health Education on Cognitive Outcomes in Sedentary Older Adults: The LIFE Randomized Trial. JAMA 2015, 314, 781. [Google Scholar] [CrossRef]
- Pahor, M.; Guralnik, J.M.; Ambrosius, W.T.; Blair, S.; Bonds, D.E.; Church, T.S.; Espeland, M.A.; Fielding, R.A.; Gill, T.M.; Groessl, E.J.; et al. Effect of Structured Physical Activity on Prevention of Major Mobility Disability in Older Adults: The LIFE Study Randomized Clinical Trial. JAMA 2014, 311, 2387. [Google Scholar] [CrossRef]
- Herold, F.; Müller, P.; Gronwald, T.; Müller, N.G. Dose–Response Matters!—A Perspective on the Exercise Prescription in Exercise–Cognition Research. Front. Psychol. 2019, 10, 2338. [Google Scholar] [CrossRef] [PubMed]
- Herold, F.; Törpel, A.; Hamacher, D.; Budde, H.; Gronwald, T. A Discussion on Different Approaches for Prescribing Physical Interventions—Four Roads Lead to Rome, but Which One Should We Choose? J. Pers. Med. 2020, 10, 55. [Google Scholar] [CrossRef] [PubMed]
- Lautenschlager, N.T.; Cox, K.L.; Flicker, L.; Foster, J.K.; van Bockxmeer, F.M.; Xiao, J.; Greenop, K.R.; Almeida, O.P. Effect of Physical Activity on Cognitive Function in Older Adults at Risk for Alzheimer Disease: A Randomized Trial. JAMA 2008, 300, 1027. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Zhang, H.; Ma, X.; Di, Q. Mental Health Problems during the COVID-19 Pandemics and the Mitigation Effects of Exercise: A Longitudinal Study of College Students in China. Int. J. Environ. Res. Public Health 2020, 17, 3722. [Google Scholar] [CrossRef] [PubMed]
| Variables | Intervention Group (n = 33) | Waitlist Group (n = 29) | p |
|---|---|---|---|
| Demographics | |||
| Age (years) | 22.61 ± 2.19 | 22.83 ± 2.25 | 0.70 |
| Body weight (kg) | 58.13 ± 19.72 | 60.25 ± 19.55 | 0.67 |
| Height (cm) | 163.03 ± 7.13 | 165.67 ± 5.40 | 0.11 |
| BMI (kg/m2) | 21.79 ± 6.96 | 21.96 ± 7.10 | 0.93 |
| Years of higher education | 4.33 ± 1.67 | 4.34 ± 1.57 | 0.98 |
| Region (city/countryside) | 31/2 | 25/4 | 0.41 |
| Behavior | |||
| PA (METs-minutes/week) | 693.89 ± 593.29 | 1011.53 ± 713.09 | 0.19 |
| MVPA (METs-minutes/week) | 318.79 ± 317.99 | 553.52 ± 853.17 | 0.16 |
| Average ST (minutes/day) | 369.16 ± 131.75 | 334.78 ± 146.13 | 0.30 |
| Psychology | |||
| STAI (score) | 22.21 ± 6.80 | 20.97 ± 6.82 | 0.46 |
| PSS (score) | 19.15 ± 7.77 | 19.24 ± 6.72 | 0.96 |
| Cognition | |||
| Processing Speed (score) | 9.06 ± 2.44 | 9.83 ± 1.58 | 0.21 |
| Working Memory (score) | 15.22 ± 1.12 | 15.33 ± 1.12 | 0.89 |
| Episodic Memory (score) | 14.06 ± 2.55 | 13.50 ± 4.68 | 0.72 |
| Visual-spatial Ability (score) | 14.89 ± 2.65 | 12.33 ± 3.11 | 0.01 * |
| Verbal Ability (score) | 14.28 ± 1.90 | 13.06 ± 2.88 | 0.09 |
| Global Cognitive Function (score) | 67.50 ± 6.23 | 64.06 ± 6.82 | 0.20 |
| Variables | Mean Difference (p) | p () for the Mixed-Effect Model b | |||
|---|---|---|---|---|---|
| Intervention Group (n = 33) | Waitlist Group (n = 29) | Between- Participants | Within- Participants | Interaction- Effect | |
| PA | |||||
| ΔPAT2-T1 | 994.70 (<0.001) * | 690.40 (0.010) * | 0.73 (0.002) | <0.001 * (0.27) | 0.31 (0.019) |
| ΔPAT3-T1 | 1218.00 (<0.001) * | 738.97 (0.003) * | |||
| T2IG-WG | −13.36 (0.96) | ||||
| T3IG-WG | 161.40 (0.51) | ||||
| MVPA | |||||
| ΔMVPAT2-T1 | 718.79 (<0.001) * | 221.66 (0.69) | 0.22 (0.024) | <0.001 * (0.24) | 0.022 * (0.065) |
| ΔMVPAT3-T1 | 940.61 (<0.001) * | 358.90 (0.08) | |||
| T2IG-WG | 282.40 (0.13) | ||||
| T3IG-WG | 346.98 (0.072) | ||||
| AST | |||||
| ΔASTT2-T1 | −66.95 (0.05) * | −73.99 (0.05) * | 0.034 * (0.072) | 0.004 * (0.090) | 0.61 (0.008) |
| ΔASTT3-T1 | −24.92 (0.95) | −63.56 (0.13) | |||
| T2IG-WG | 41.42 (0.16) | ||||
| T3IG-WG | 73.02 (0.038) * | ||||
| STAI (score) | |||||
| ΔSTAIT2-T1 | −4.03 (0.027) * | −1.45 (0.94) | 0.81 (0.001) | <0.001 * (0.11) | 0.38 (0.016) |
| ΔSTAIT3-T1 | −4.73 (0.002) * | −2.69 (0.18) | |||
| T2IG-WG | −1.34 (0.40) | ||||
| T3IG-WG | −0.79 (0.64) | ||||
| PSS (score) | |||||
| ΔPSST2-T1 | −2.39 (0.35) | −1.89 (0.73) | 0.69 (0.003) | <0.001 * (0.15) | 0.89 (0.002) |
| ΔPSST3-T1 | −5.09 (0.001) * | −4.14 (0.02) * | |||
| T2IG-WG | −0.59 (0.77) | ||||
| T3IG-WG | −1.04 (0.54) | ||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, Y.; Zhang, B.; Gan, L.; Ke, L.; Fu, Y.; Di, Q.; Ma, X. Effects of Online Bodyweight High-Intensity Interval Training Intervention and Health Education on the Mental Health and Cognition of Sedentary Young Females. Int. J. Environ. Res. Public Health 2021, 18, 302. https://doi.org/10.3390/ijerph18010302
Zhang Y, Zhang B, Gan L, Ke L, Fu Y, Di Q, Ma X. Effects of Online Bodyweight High-Intensity Interval Training Intervention and Health Education on the Mental Health and Cognition of Sedentary Young Females. International Journal of Environmental Research and Public Health. 2021; 18(1):302. https://doi.org/10.3390/ijerph18010302
Chicago/Turabian StyleZhang, Yao, Beier Zhang, Liaoyan Gan, Limei Ke, Yingyao Fu, Qian Di, and Xindong Ma. 2021. "Effects of Online Bodyweight High-Intensity Interval Training Intervention and Health Education on the Mental Health and Cognition of Sedentary Young Females" International Journal of Environmental Research and Public Health 18, no. 1: 302. https://doi.org/10.3390/ijerph18010302
APA StyleZhang, Y., Zhang, B., Gan, L., Ke, L., Fu, Y., Di, Q., & Ma, X. (2021). Effects of Online Bodyweight High-Intensity Interval Training Intervention and Health Education on the Mental Health and Cognition of Sedentary Young Females. International Journal of Environmental Research and Public Health, 18(1), 302. https://doi.org/10.3390/ijerph18010302





