Loneliness, Malnutrition and Change in Subjective Age among Older Adults during COVID-19 Pandemic
Abstract
1. Introduction
1.1. Subjective Age of Older Adults
1.2. Loneliness in Older Adults
1.3. Mediating Factors
1.3.1. Depressive Symptoms
1.3.2. Malnutrition
2. The Current Study
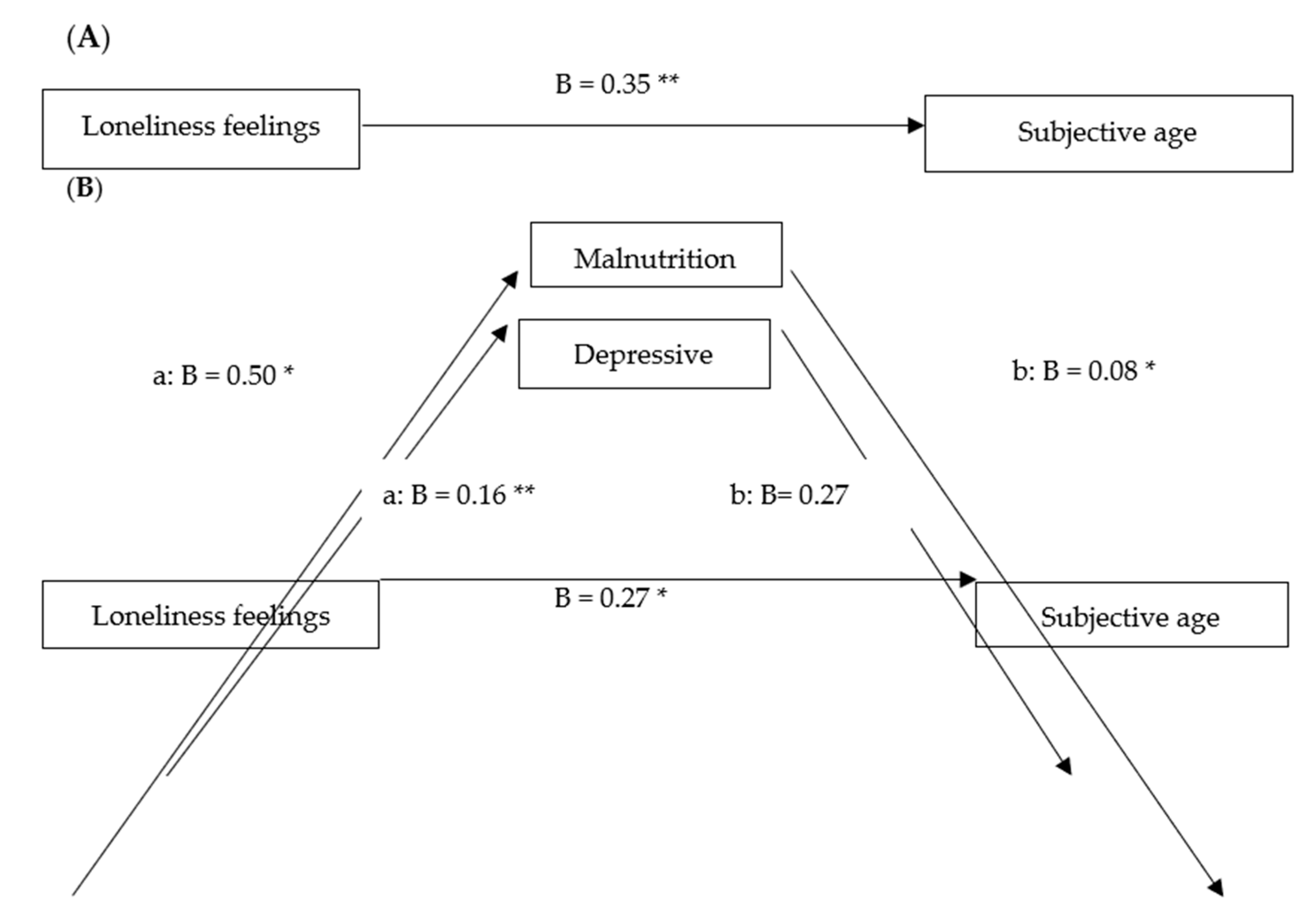
- In comparison with the period before the pandemic, older adults feel older in age during the pandemic.
- Feelings of loneliness are associated with subjective age during times of crisis.
- Feelings of loneliness are indirectly associated with subjective age during crises through depressive symptoms and malnutrition; lonely older adults feel older during crises, and this is associated with higher levels of depressive symptoms and malnutrition.
3. Method
3.1. Study Design and Participants
3.2. Procedures
3.3. Measures
3.3.1. Independent Variable: Loneliness
3.3.2. Dependent Variable: Subjective Age during a Crisis (the COVID-19 Pandemic).
3.4. Mediators
3.4.1. Depressive Symptoms
3.4.2. Malnutrition
3.5. Covariates
3.6. Data Analyses
4. Results
The Mediation Analyses
5. Discussion
6. Conclusions and Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Kotter-Grühn, D.; Neupert, S.D.; Stephan, Y. Feeling old today? Daily health, stressors, and affect explain day-to-day variability in subjective age. Psychol. Health 2015, 30, 1470–1485. [Google Scholar] [CrossRef]
- Stephan, Y.; Sutin, A.R.; Terracciano, A. How old do you feel? The role of age discrimination and biological aging in subjective age. PLoS ONE 2015, 10, 1–12. [Google Scholar] [CrossRef]
- Kornadt, A.E.; Hess, T.M.; Voss, P.; Rothermund, K. Subjective age across the life span: A differentiated, longitudinal approach. J. Gerontol. B Psychol. Sci. Soc. Sci. 2018, 73, 767–777. [Google Scholar] [CrossRef]
- Westerhof, G.J.; Miche, M.; Brothers, A.F.; Barrett, A.E.; Diehl, M.; Montepare, J.M.; Wurm, S. The influence of subjective aging on health and longevity: A meta-analysis of longitudinal data. Psychol. Aging 2014, 29, 793–802. [Google Scholar] [CrossRef]
- Westerhof, G.J.; Barrett, A.E. Age identity and subjective well-being: A comparison of the United States and Germany. J. Gerontol. B Psychol. Sci. Soc. Sci. 2005, 60, S129–S136. [Google Scholar] [CrossRef]
- Stephan, Y.; Caudroit, J.; Jaconelli, A.; Terracciano, A. Subjective age and cognitive functioning: A 10-year prospective study. Am. J. Geriatr. Psychiatry 2014, 22, 1180–1187. [Google Scholar] [CrossRef] [PubMed]
- Spuling, S.M.; Miche, M.; Wurm, S.; Wahl, H.W. Exploring the causal interplay of subjective age and health dimensions in the second half of life: A cross-lagged panel analysis. Zeitschrift Fur Gesundheitspsychologie 2013, 21, 5–15. [Google Scholar] [CrossRef]
- Ambrosi-Randić, N.; Nekić, M.; Junaković, I. Felt age, desired, and expected lifetime in the context of health, well-being, and successful aging. Int. J. Aging Hum. Dev. 2018, 87, 33–51. [Google Scholar] [CrossRef] [PubMed]
- Brothers, A.; Miche, M.; Wahl, H.W.; Diehl, M. Examination of associations among three distinct subjective aging constructs and their relevance for predicting developmental correlates. J. Gerontol. B Psychol. Sci. Soc. Sci. 2017, 72, 547–560. [Google Scholar] [CrossRef] [PubMed]
- Mock, S.E.; Eibach, R.P. Aging attitudes moderate the effect of subjective age on psychological well-being: Evidence from a 10-year longitudinal study. Psychol. Aging 2011, 26, 979–986. [Google Scholar] [CrossRef] [PubMed]
- Keyes, C.L.M.; Westerhof, G.J. Chronological and subjective age differences in flourishing mental health and major depressive episode. Aging Ment. Health 2012, 16, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Shrira, A.; Bodner, E.; Palgi, Y. The interactive effect of subjective age and subjective distance-to-death on psychological distress of older adults. Aging Ment. Health 2014, 18, 1066–1070. [Google Scholar] [CrossRef] [PubMed]
- Pinquart, M.; Sörensen, S. Gender differences in self-concept and psychological wellbeing in old age: A meta-analysis. J. Gerontol. B Psychol. Sci. Soc. Sci. 2001, 56, 195–213. [Google Scholar] [CrossRef] [PubMed]
- Choi, E.Y.; Kim, Y.S.; Lee, H.Y.; Shin, H.R.; Park, S.; Cho, S.E. The moderating effect of subjective age on the association between depressive symptoms and cognitive functioning in Korean older adults. Aging Ment. Health 2019, 23, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Hülür, G.; Hertzog, C.; Pearman, A.M.; Gerstorf, D. Correlates and moderators of change in subjective memory and memory performance: Findings from the health and retirement study. Gerontology 2015, 61, 232–240. [Google Scholar] [CrossRef] [PubMed]
- Pearman, A.; Hertzog, C.; Gerstorf, D. Little evidence for links between memory complaints and memory performance in very old age: Longitudinal analyses from the Berlin aging study. Psychol. Aging 2014, 29, 828–842. [Google Scholar] [CrossRef] [PubMed]
- Rippon, I.; Steptoe, A. Is the relationship between subjective age, depressive symptoms and activities of daily living bidirectional? Soc. Sci. Med. 2018, 214, 41–48. [Google Scholar] [CrossRef]
- Segel-Karpas, D.; Palgi, Y. “It is nothing more than a senior moment”: The moderating role of subjective age in the effect of change in memory on self-rated memory. Aging Ment. Health 2017. [Google Scholar] [CrossRef]
- Ayalon, L.; Palgi, Y.; Avidor, S.; Bodner, E. Accelerated increase and decrease in subjective age as a function of changes in loneliness and objective social indicators over a four-year period: Results from the health and retirement study. Aging Ment. Health 2016, 20, 743–751. [Google Scholar] [CrossRef]
- Andersson, L. Loneliness research and interventions: A review of the literature. Aging Ment. Health 1998, 2, 264274. [Google Scholar] [CrossRef]
- Gierveld, J.D.J. A review of loneliness: Concept and definitions, determinants and consequences. Rev. Clin. Gerontol. 1998, 8, 7380. [Google Scholar] [CrossRef]
- Hawkley, L.C.; Cacioppo, J.T. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 2010, 40, 218–227. [Google Scholar] [CrossRef] [PubMed]
- Fees, B.S.; Martin, P.; Poon, L.W. A model of loneliness in older adults. J. Gerontol. B Psychol. Sci. Soc. Sci. 1999, 54, 231–239. [Google Scholar] [CrossRef] [PubMed]
- Shiovitz-Ezra, S.; Ayalon, L. Situational versus chronic loneliness as risk factors for all-cause mortality. Int. Psychogeriatr. 2010, 22, 455462. [Google Scholar] [CrossRef] [PubMed]
- Hawkley, L.C.; Masi, C.M.; Berry, J.D.; Cacioppo, J.T. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol. Aging 2006, 21, 152–164. [Google Scholar] [CrossRef]
- Perissinotto, C.M.; Stijacic Cenzer, I.; Covinsky, K.E. Loneliness in older persons: A predictor of functional decline and death. Arch. Intern. Med. 2012, 172, 1078–1083. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Hawkley, L.C.; Berntson, G.G.; Ernst, J.M.; Gibbs, A.C.; Stickgold, R.; Hobson, J.A. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychol. Sci. 2002, 13, 384–387. [Google Scholar] [CrossRef]
- Wilson, R.S.; Krueger, K.R.; Arnold, S.E.; Schneider, J.A.; Kelly, J.F.; Barnes, L.L.; Tang, Y.; Bennet, D.A. Loneliness and risk of Alzheimer disease. Arch. Gen. Psychiatry 2007, 64, 234–240. [Google Scholar] [CrossRef]
- Degges-White, S.; Kepic, M. Friendships, subjective age, and life satisfaction of women in midlife. Adultspan J. 2019, 19, 39–53. [Google Scholar] [CrossRef]
- Luo, Y.; Hawkley, L.C.; Waite, L.J.; Cacioppo, J.T. Loneliness, health, and mortality in old age: A national longitudinal study. Soc. Sci. Med. 2012, 74, 907–914. [Google Scholar] [CrossRef]
- Golden, J.; Conroy, R.M.; Bruce, I.; Denihan, A.; Greene, E.; Kirby, M.; Lawlor, B.A. Loneliness, social support networks, mood and wellbeing in community dwelling elderly. Int. J. Geriatr. Psychiatry 2009, 24, 694–700. [Google Scholar] [CrossRef] [PubMed]
- Seeman, T.E. Social ties and health: The benefits of social integration. Ann. Epidemiol. 1996, 6, 442–451. [Google Scholar] [CrossRef]
- Dykstra, P.A.; van Tilburg, T.G.; Gierveld, J.D.J. Changes in older adult loneliness: Results from a seven-year longitudinal study. Res. Aging 2005, 27, 725–747. [Google Scholar] [CrossRef]
- Korporaal, M.; Broese van Groenou, M.I.; van Tilburg, T.G. Effects of own and spousal disability on loneliness among older adults. J. Aging Health 2008, 20, 306–325. [Google Scholar] [CrossRef]
- Wrzus, C.; Hänel, M.; Wagner, J.; Neyer, F.J. Social network changes and life events across the life span: A meta-analysis. Psychol. Bull. 2013, 139, 53–80. [Google Scholar] [CrossRef]
- Ustun, T.B.; Ayuso-Mateos, J.L.; Chatterji, S.; Mathers, C.; Murray, C.J.L. Global burden of depressive disorders in the year 2000. Br. J. Psychiatry 2004, 184, 386–392. [Google Scholar] [CrossRef]
- Compton, W.M.; Conway, K.P.; Stinson, F.S.; Grant, F.F. Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991–1992 and 2001–2002. Am. J. Psychiatry 2006, 163, 2141–2147. [Google Scholar] [CrossRef]
- Fiske, A.; Wetherell, J.L.; Gatz, M. Depression in older adults. Annu. Rev. Clin. Psychol. 2009, 5, 363–389. [Google Scholar] [CrossRef]
- Pratt, L.A.; Brody, D.J. Depression in the U.S. Household Population, 2009–2012 (NCHS Data Brief No. 172); National Center for Health Statistics: Hyattsville, MD, USA, 2014. Available online: http://www.cdc.gov/nchs/products/databriefs/db172.htm (accessed on 29 December 2019).
- Gerst-Emerson, K.; Jayawardhana, J. Loneliness as a public health issue: The impact of loneliness on health care utilization among older adults. Am. J. Public Health 2015, 105, 1013–1019. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Thisted, R.A. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychol. Aging 2006, 21, 140–151. [Google Scholar] [CrossRef]
- James, B.D.; Wilson, R.S.; Barnes, L.L.; Bennett, D.A. Late-life social activity and cognitive decline in old age. J. Int. Neuropsychol. Soc. 2011, 17, 998–1005. [Google Scholar] [CrossRef] [PubMed]
- Lund, R.; Nilsson, C.J.; Avlund, K. Can the higher risk of disability onset among older people who live alone be alleviated by strong social relations? A longitudinal study of non-disabled men and women. Age Ageing 2010, 39, 319–326. [Google Scholar] [CrossRef] [PubMed]
- Bekhet, A.K.; Zauszniewski, J.A. Mental health of elders in retirement communities: Is loneliness a key factor? Arch. Psychiatr. Nurs. 2012, 26, 214–224. [Google Scholar] [CrossRef] [PubMed]
- Infurna, F.J.; Gerstorf, D.; Robertson, S.; Berg, S.; Zarit, S.H. The nature and cross-domain correlates of subjective age in the oldest old: Evidence from the OCTO study. Psychol. Aging 2010, 25, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Liang, K. The cross-domain correlated of subjective age in Chinese oldest-old. Aging Ment. Health 2014, 18, 217–224. [Google Scholar] [CrossRef]
- Bergland, A.; Nicolaisen, M.; Thorsen, K. Predictors of subjective age in people aged 40–79 years: A five-year follow-up study. The impact of mastery, mental and physical health. Aging Ment. Health 2014, 18, 653–661. [Google Scholar] [CrossRef]
- Stratton, R.J.; Green, C.J.; Elia, M. Scientific criteria for defining malnutrition. In Disease-Related Malnutrition: An Evidence-Based Approach to Treatment; CABI Publishing: Egham, UK, 2003; pp. 1–34. [Google Scholar]
- Brownie, S. Why are elderly individuals at risk of nutritional deficiency? Int. J. Nurs. Pract. 2006, 12, 110–118. [Google Scholar] [CrossRef]
- Cereda, E.; Pedrolli, C.; Klersy, C.; Bonardi, C.; Quarleri, L.; Cappello, S.; Turri, A.; Rondanelli, M.; Caccialanza, R. Nutritional status in older persons according to healthcare setting: A systematic review and meta-analysis of prevalence data using MNA®. Clin. Nutr. 2016, 35, 1282–1290. [Google Scholar] [CrossRef]
- De Morais, C.; Oliveira, B.; Afonso, C.; Lumbers, M.; Raats, M.; De Almeida, M.D.V. Nutritional risk of European elderly. Eur. J. Clin. Nutr. 2013, 67, 1215–1219. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Ageing and Health; WHO: Geneva, Switzerland, 2015. [Google Scholar] [CrossRef]
- Guyonnet, S.; Rolland, Y. Screening for malnutrition in older people. Clin. Geriatr. Med. 2015, 31, 429–437. [Google Scholar] [CrossRef]
- Kalan, U.; Arik, F.; Soysal, P. Malnutrition in older people. Encycl. Biomed. Gerontol. 2019. [Google Scholar] [CrossRef]
- Soenen, S.; Chapman, I.M. Body weight, anorexia, and undernutrition in older people. J. Am. Med. Dir. Assoc. 2013, 14, 642–648. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.C.H.; Schilling, L.S.; Lyder, C.H. A concept analysis of malnutrition in the elderly. J. Adv. Nurs. 2001, 36, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Fávaro-Moreira, N.C.; Krausch-Hofmann, S.; Matthys, C.; Vereecken, C.; Vanhauwaert, E.; Declercq, A.; Bekkering, G.E.; Duyck, J. Risk factors for malnutrition in older adults: A systematic review of the literature based on longitudinal data. Adv. Nutr. 2016, 7, 507–522. [Google Scholar] [CrossRef] [PubMed]
- Mangels, A.R. Malnutrition in older adults: An evidence-based review of risk factors, assessment, and intervention. Am. J. Nurs. 2018. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Vahia, I.V.; Blazer, D.G.; Smith, G.S.; Karp, J.F.; Steffens, D.C.; Forester, B.P.; Tampi, R.; Agronin, M.; Jeste, D.V.; Reynolds, F.C. COVID-19, mental health and aging: A need for new knowledge to bridge science and service. Am. J. Geriatr. Psychiatry 2020, 28, 695–697. [Google Scholar] [CrossRef]
- Yesavage, J.A.; Brink, T.L. Development and validation of a geriatric depression screening scale: A preliminary report. J. Psychiatr. Res. 1983, 17, 37–49. [Google Scholar] [CrossRef]
- Hayes, A.F. PROCESS [Macro]. Available online: http://afhayes.com/introduction-to-mediation-moderation-and-conditional-process-analysis.html (accessed on 3 November 2012).
- Preacher, K.J.; Hayes, A.F. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 2008, 40, 879–891. [Google Scholar] [CrossRef]
- Morle, J.E.; Vellas, B. COVID-19 and older adult. J. Nutr. Health. Aging. 2020, 24, 364–365. [Google Scholar] [CrossRef]
- Graham, J.E.; Christian, L.M.; Kiecolt-Glaser, J.K. Stress, age, and immune function: Toward a lifespan approach. J. Behav. Med. 2006, 29, 389–400. [Google Scholar] [CrossRef] [PubMed]
- Foster, H.; Hagan, J.; Brooks-Gunn, J. Growing up fast: Stress exposure and subjective “weathering” in emerging adulthood. J. Health Soc. Behav. 2008, 49, 162–177. [Google Scholar] [CrossRef] [PubMed]
- Schafer, M.H.; Shippee, T. Age identity in context: Stress and the subjective side of aging. Soc. Psychol. Q. 2010, 73, 245–264. [Google Scholar] [CrossRef]
- Lazarus, R.S. Stress and Emotion: A New Synthesis; Springer: New York, NY, USA, 1999. [Google Scholar]
- Zautra, A.J. Emotions, Stress, and Health; Oxford University Press: New York, NY, USA, 2003. [Google Scholar]
- Whitbourne, S.K. (Ed.) The Encyclopedia of Adulthood and Aging, 3 Volume Set; John Wiley & Sons: Hoboken, NJ, USA, 2016; Volume 1. [Google Scholar]
- Eskelinen, K.; Hartikainen, S.; Nykanen, I. Is loneliness associated with malnutrition in older people? Int. J. Gerontol. 2016, 10, 43–45. [Google Scholar] [CrossRef]
- Chatindiara, I.; Sheridan, N.; Kruger, M.; Wham, C. Eating less the logical thing to do? Vulnerability to malnutrition with advancing age: A qualitative study. Appetite 2020, 146, 104502. [Google Scholar] [CrossRef]
- Hammons, A.J.; Fiese, B.H. Is frequency of shared family meals related to the nutritional health of children and adolescents? Pediatrics 2011, 127, e1565–e1574. [Google Scholar] [CrossRef]
- Locher, J.L.; Robinson, C.O.; Roth, D.L.; Ritchie, C.S.; Burgio, K.L. The effect of the presence of others on caloric intake in homebound older adults. J. Gerontol. A Biol. Sci. Med. Sci. 2005, 60, 1475–1478. [Google Scholar] [CrossRef]
- Bofill, S. Aging and loneliness in Catalonia: The social dimension of food behavior. Ageing Int. 2004, 29, 385–398. [Google Scholar] [CrossRef]
- Kreausukon, P.; Gellert, P.; Lippke, S.; Schwarzer, R. Planning and self-efficacy can increase fruit and vegetable consumption: A randomized controlled trial. J. Behav. Med. 2012, 35, 443–451. [Google Scholar] [CrossRef]
- Holwerda, T.J.; Deeg, D.J.; Beekman, A.T.; van Tilburg, T.G.; Stek, M.L.; Jonker, C.; Schoevers, R.A. Feelings of loneliness, but not social isolation, predict dementia onset: Results from the Amsterdam Study of the Elderly (AMSTEL). J. Neurol. Neurosurg. Psychiatry 2014, 85, 135–142. [Google Scholar] [CrossRef]
| Background Characteristics | N | Valid % | Mean | SD | Range |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 96 | 47.8 | |||
| Female | 105 | 52.2 | |||
| Health status | 3.61 | 1.15 | 1–5 | ||
| Age | 74.3 | 6.3 | |||
| Education | 10.0 | 4.0 | |||
| Marital status | |||||
| No partner | 54 | 26.9 | |||
| Has a partner | 143 | 71.1 | |||
| Missing value | 4 | 2.0 | |||
| Independent variable | |||||
| Loneliness feelings | 2.2 | 1.1 | 1–4 | ||
| Mediators | |||||
| Depressive symptoms | 4.77 | 3.2 | 0–15 | ||
| Malnutrition | 6.82 | 4.3 | 0–20 | ||
| Dependent variable | |||||
| Subjective age during COVID-19 1 pandemic | 2.94 | 1.73 | 0–5 |
| Variable | Mean | SD | t | p Value |
|---|---|---|---|---|
| Subjective age before COVID-19 pandemic | 2.76 | (1.7) | 2.3 | 0.03 |
| Subjective age during COVID-19 pandemic | 2.94 | (1.7) |
| Variables | Subjective Age during the COVID-19 Pandemic | ||||
|---|---|---|---|---|---|
| Mean | SD | Test a | p Value | ||
| Demographic characteristics | |||||
| Gender | Male | 2.75 | 1.8 | t = −1.50 | 0.14 |
| Female | 3.11 | 1.7 | |||
| Age | r = −0.05 | 0.52 | |||
| Education | r = −0.08 | 0.29 | |||
| Marital status | With partner | 2.77 | 1.7 | t = −2.41 | 0.02 |
| Without partner | 3.43 | 1.68 | |||
| Independent variable | |||||
| Loneliness feelings | r = 0.75 | 0.000 | |||
| Mediators | |||||
| Depressive symptoms | r = 0.22 | 0.002 | |||
| Malnutrition | r = 0.27 | 0.000 | |||
| Covariates | Independent Variable | Mediating Variable | Dependent Variable | Covariates→DV | IV→M | MV→DV | Direct Effect IV→DV | Indirect Effect | Total Effect | Adj R2 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (IV) | (MeV) | (DV) | (path a) | (path b) | (path C’) | (a × b) | 95%CI | (C) | R2 | ||
| Age group | Loneliness feelings | Depressive symptoms | Subjective age during COVID-19 pandemic | ns | 0.16 ** | 0.27 | 0.27 * | 0.04 | −0.003–0.14 | 0.35 ** | 0.15 *** |
| Gender | ns | ||||||||||
| Marital status | ns | ||||||||||
| Education | Malnutrition | ns | 0.50 * | 0.08* | 0.04 | 0.002–0.13 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vitman Schorr, A.; Yehuda, I.; Tamir, S. Loneliness, Malnutrition and Change in Subjective Age among Older Adults during COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 106. https://doi.org/10.3390/ijerph18010106
Vitman Schorr A, Yehuda I, Tamir S. Loneliness, Malnutrition and Change in Subjective Age among Older Adults during COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2021; 18(1):106. https://doi.org/10.3390/ijerph18010106
Chicago/Turabian StyleVitman Schorr, Adi, Itamar Yehuda, and Snait Tamir. 2021. "Loneliness, Malnutrition and Change in Subjective Age among Older Adults during COVID-19 Pandemic" International Journal of Environmental Research and Public Health 18, no. 1: 106. https://doi.org/10.3390/ijerph18010106
APA StyleVitman Schorr, A., Yehuda, I., & Tamir, S. (2021). Loneliness, Malnutrition and Change in Subjective Age among Older Adults during COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 18(1), 106. https://doi.org/10.3390/ijerph18010106






