Multi-System Physical Exercise Intervention for Fall Prevention and Quality of Life in Pre-Frail Older Adults: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
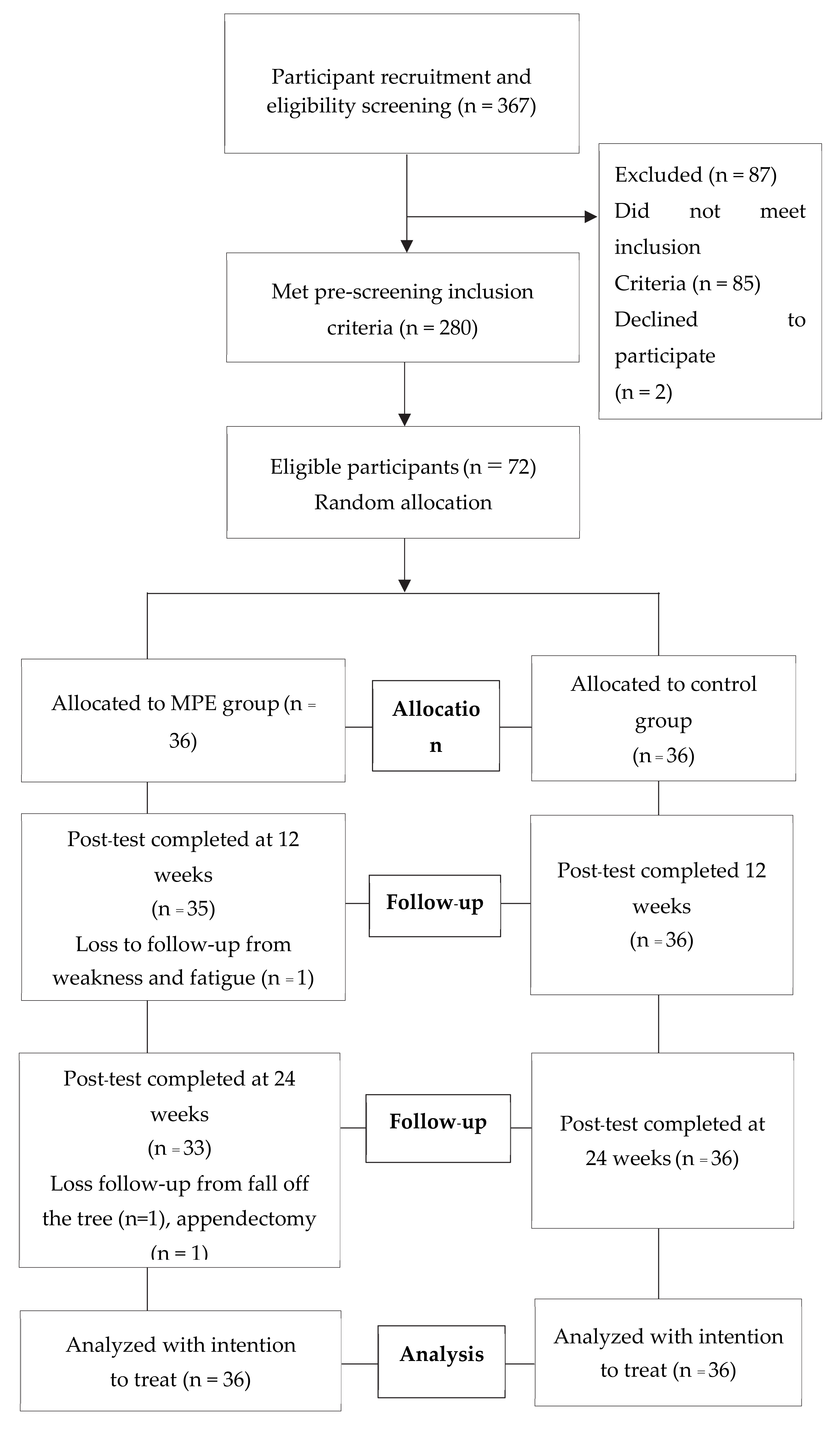
2.1. Study Design
2.2. Participants
2.3. Intervention
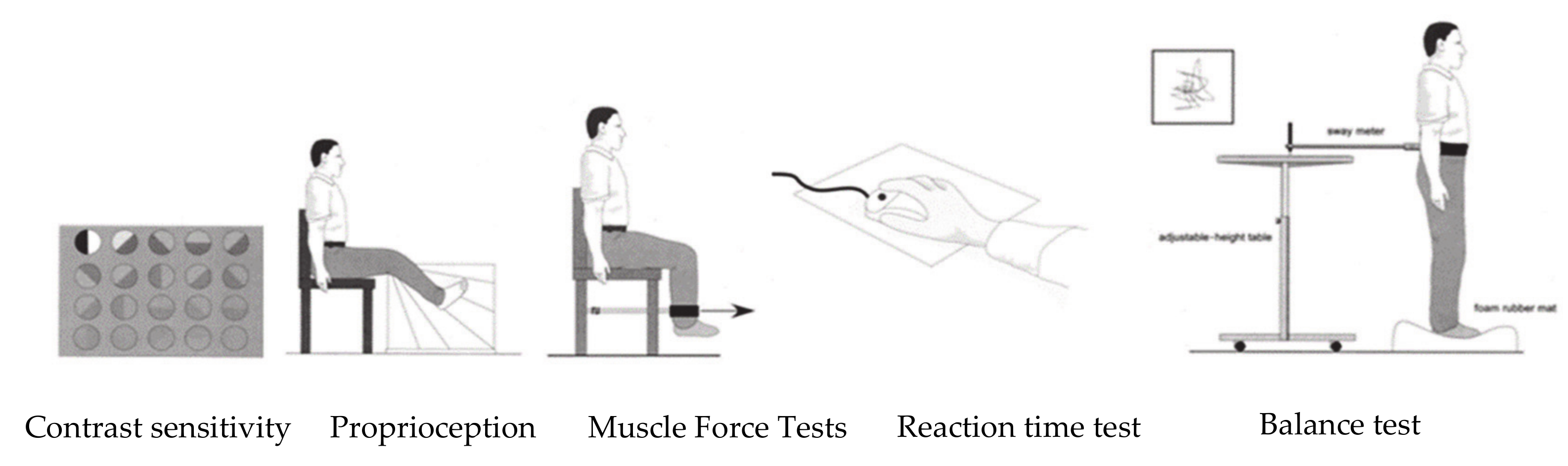
2.4. Outcome Measures
2.4.1. Primary Outcome
2.4.2. Secondary Outcomes
2.5. Data Analysis
2.6. Ethical Consideration
3. Results
3.1. Baseline Characteristics
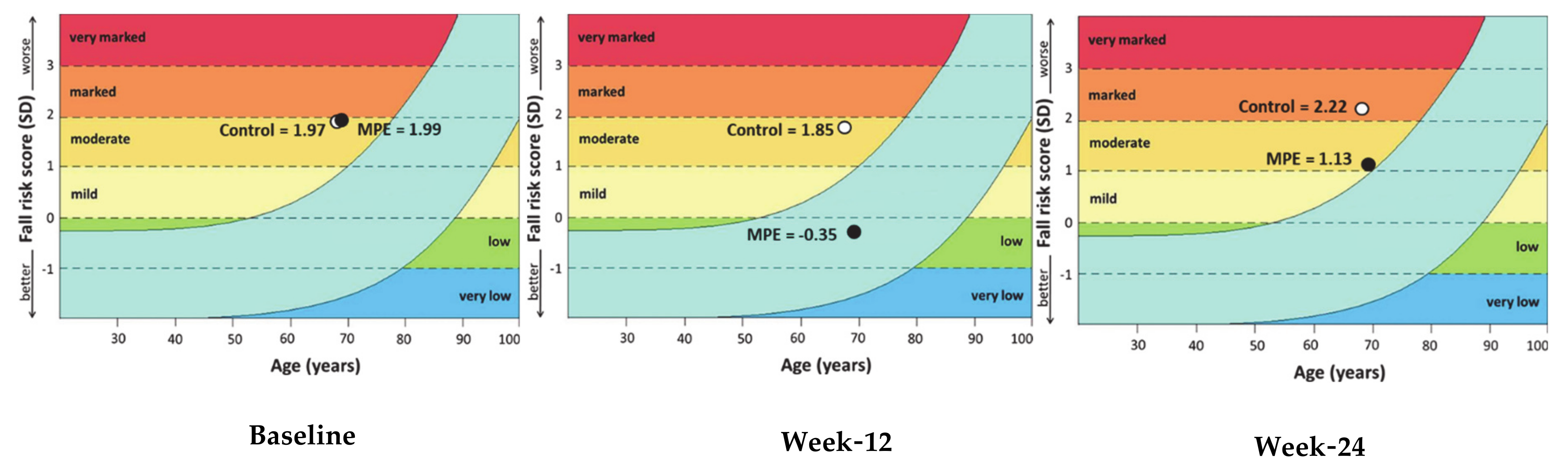
3.2. Fall Risk Score
3.2.1. Fear of Falling Scores
3.2.2. Depression Scores
3.2.3. Health-Related Quality of Life (HRQOL)
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- United Nations. “Ageing”, United Nations. Available online: https://www.un.org/en/sections/issues-depth/ageing/ (accessed on 19 December 2019).
- Ferrucci, L.; Giallauria, F.; Guralnik, J.M. Epidemiology of aging. Radiol. Clin. N. Am. 2008, 46, 643. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Mao, G.; Leng, S.X. Frailty syndrome: An overview. Clin. Interv. Aging 2014, 9, 433–441. [Google Scholar] [PubMed]
- Xue, Q.L. The Frailty Syndrome: Definition and Natural History. Clin. Geriatr. Med. 2011, 27, 1–15. [Google Scholar] [CrossRef]
- Sharif, S.I.; Al-Harbi, A.B.; Al-Shihabi, A.M.; Al-Daour, D.S.; Sharif, R.S. Falls in the elderly: Assessment of prevalence and risk factors. Pharm. Pract. (Granada) 2018, 16, 1206. [Google Scholar] [CrossRef] [PubMed]
- Umegaki, H.; Makino, T.; Uemura, K.; Shimada, H.; Cheng, X.W.; Dodge, H.; Kuzuya, M. Falls in community-dwelling prefrail older adults. Health Soc. Care Community 2019, 28, 110–115. [Google Scholar] [CrossRef]
- Cheng, M.H.; Chang, S.F. Frailty as a Risk Factor for Falls Among Community Dwelling People: Evidence from a Meta-Analysis. J. Nurs. Scholarsh. 2017, 49, 529–536. [Google Scholar] [CrossRef]
- Berry, S.D.; Miller, R.R. Falls: Epidemiology, pathophysiology, and relationship to fracture. Curr. Osteoporos. Rep. 2008, 6, 149–154. [Google Scholar] [CrossRef]
- Gilardi, F.; Scarcella, P.; Proietti, M.G.; Capobianco, G.; Rocco, G.; Capanna, A.; Mancinelli, S.; Marazzi, M.C.; Palombi, L.; Liotta, G. Frailty as a predictor of mortality and hospital services use in older adults: A cluster analysis in a cohort study. Eur. J. Public Health 2018, 28, 842–846. [Google Scholar] [CrossRef]
- Chang, S.F.; Lin, H.C.; Cheng, C.L. The Relationship of Frailty and Hospitalization Among Older People: Evidence from a Meta-Analysis. J. Nurs. Scholarsh. 2018, 50, 383–391. [Google Scholar] [CrossRef]
- Buckinx, F.; Rolland, Y.; Reginster, J.Y.; Ricour, C.; Petermans, J.; Bruyere, O. Burden of frailty in the elderly population: Perspectives for a public health challenge. Arch. Public Health 2015, 73, 19. [Google Scholar] [CrossRef]
- Galet, C.; Zhou, Y.; Eyck, P.T.; Romanowski, K.S. Fall injuries, associated deaths, and 30-day readmission for subsequent falls are increasing in the elderly US population: A query of the WHO mortality database and National Readmission Database from 2010 to 2014. Clin. Epidemiol. 2018, 10, 1627–1637. [Google Scholar] [CrossRef]
- Pasquetti, P.; Apicella, L.; Mangone, G. Pathogenesis and treatment of falls in elderly. Clin. Cases Miner. Bone Metab. 2014, 11, 222–225. [Google Scholar] [CrossRef]
- Fernandes, V.L.S.; Ribeiro, D.M.; Fernandes, L.C.; de Menezes, R.L. Postural changes versus balance control and falls in community-living older adults: A systematic review. Fisioter. Mov. 2018, 31, 1–15. [Google Scholar] [CrossRef]
- Ribeiro, F.; Oliveira, J. Aging effects on joint proprioception: The role of physical activity in proprioception preservation. Eur. Rev. Aging Phys. Act. 2007, 4, 71–76. [Google Scholar] [CrossRef]
- Amarya, S.; Singh, K.; Sabharwal, M. Ageing Process and Physiological Changes; IntechOpen: London, UK, 2018; pp. 1–24. [Google Scholar]
- Liu, C.K.; Fielding, R.A. Exercise as an Intervention for Frailty. Clin. Geriatr. Med. 2011, 27, 101–110. [Google Scholar] [CrossRef] [PubMed]
- De Labra, C.; Guimaraes-Pinheiro, C.; Maseda, A.; Lorenzo, T.; Millan-Calenti, J.C. Effects of physical exercise interventions in frail older adults: A systematic review of randomized controlled trials. BMC Geriatr. 2015, 15, 154. [Google Scholar] [CrossRef] [PubMed]
- Pillatt, A.P.; Nielsson, J.; Schneider, R.H. Effects of physical exercise in frail older adults: A systematic review. Fisioter. Pesqui 2019, 26, 225–232. [Google Scholar]
- Toosizadeh, N.; Ehsani, H.; Miramonte, M.; Mohler, J. Proprioceptive impairments in high fall risk older adults: The effect of mechanical calf vibration on postural balance. Biomed. Eng. Online 2018, 17, 51. [Google Scholar] [CrossRef]
- Patar, M.G.; Scheicher, M. Effects of strength and balance training on the mobility, fear of falling and grip strength of elderly female fallers. J. Bodyw. Mov. Ther. 2014, 19, 646–650. [Google Scholar]
- Lopez, P.; Pinto, R.S.; Radaelli, R.; Rech, A.; Grazioli, R.; Izquierdo, M.; Cadore, E.L. Benefits of resistance training in physically frail elderly: A systematic review. Aging Clin. Exp. Res. 2018, 30, 889–899. [Google Scholar] [CrossRef]
- Hosseini, L.; Kargozar, E.; Sharifi, F.; Negarandeh, R.; Memari, A.H.; Navab, E. Tai Chi Chuan can improve balance and reduce fear of falling in community dwelling older adults: A randomized control trial. J. Exerc. Rehabil. 2018, 14, 1024–1031. [Google Scholar] [CrossRef] [PubMed]
- Fisseha, B.; Janakiraman, B.; Yitayeh, A.; Ravichandran, H. Effect of square stepping exercise for older adults to prevent fall and injury related to fall: Systematic review and meta-analysis of current evidences. J. Exerc. Rehabil. 2017, 13, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, V.A.; Abbott, R.A.; Whear, R.; Bethel, A.; Ukoumunne, O.C.; Thompson-Coon, J.; Stein, K. Multiple component interventions for preventing falls and fall-related injuries among older people: Systematic review and meta-analysis. BMC Geriatr. 2014, 14, 15. [Google Scholar] [CrossRef] [PubMed]
- Fairhall, N.; Sherrington, C.; Lord, S.R.; Kurrle, S.E.; Langron, C.; Lockwood, K.; Monaghan, N.; Aggar, C.; Cameron, I.D. Effect of a multifactorial, interdisciplinary intervention on risk factors for falls and fall rate in frail older people: A randomised controlled trial. Age Ageing 2014, 43, 616–622. [Google Scholar] [CrossRef]
- Ng, T.; Nyunt, M.S.Z.; Feng, L.; Feng, L.; Niti, M.; Tan, B.Y.; Chan, G.; Khoo, S.A. Multi-domains lifestyle interventions reduces depressive symptoms among frail and pre-frail older persons: Randomized controlled trial. J. Nutr. Health Aging 2017, 21, 918–926. [Google Scholar] [CrossRef] [PubMed]
- Chou, C.H.; Hwang, C.L.; Wu, Y.T. Effect of exercise on physical function, daily living activities, and quality of life in the frail older adults: A meta-analysis. Arch. Phys. Med. Rehabil. 2012, 93, 237–244. [Google Scholar] [CrossRef] [PubMed]
- Lord, S.R.; Menz, H.; Tiedemann, A. A Physiological Profile Approach to Falls Risk Assessment and Prevention. Phys. Ther. 2003, 83, 237–252. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, M146–M156. [Google Scholar] [CrossRef]
- Binder, E.F.; Schechtman, K.B.; Ehsani, A.A.; Steger-May, K.; Brown, M.; Sinacore, D.R.; Yarasheski, K.E.; Holloszy, J.O. Effects of exercise training on frailty in community-dwelling older adults: Results of a randomized controlled trial. J. Am. Geriatr. Soc. 2002, 50, 1921–1928. [Google Scholar] [CrossRef]
- Thiamwong, L. Psychometric Testing of the Falls Efficacy Scale-International (FES-I) in Thai Older Adults. J. Health Sci. Med. Res. 2011, 29, 277–287. [Google Scholar]
- Wongpakaran, N.; Wongpankaran, T. Prevalence of major depressive disorder in long-term care facilities: A report northern Thailand. Psychogeriatrics 2012, 12, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Shiekh, J.; Yesavage, J. Geriatric Depression Scale; recent findings and development of a short version. In Clinical Gerontology: A Guide to Assessment and Intervention; Brink, T., Ed.; Haworth Press: New York, NY, USA, 1986; pp. 165–173. [Google Scholar]
- Leurmarnkul, W.; Meetam, P. Properties Testing of the Retranslated SF-36 (Thai Version). Thail. J. Pharm. Sci. 2005, 29, 69–88. [Google Scholar]
- Lasonguannek, N.; Wiroteurairuang, T.; Siritho, S.; Prayoonwiwat, N. Reliability of the Thai Version of SF-36 Questionnaire for an Evaluation of Quality of Life in Multiple Sclerosis Patients in Multiple Sclerosis at Clinic at Siriraj Hospital. J. Med. Assoc. Thail. 2011, 94, s84–s88. [Google Scholar]
- Liabsuetrakul, T.; Southern Soil-Transmitted Helminths and Maternal Health Working Group. Is international or Asian criteria-based body mass index associated with maternal anaemia, low birthweight, and preterm births among Thai population? An observational study. J. Health Popul. Nutr. 2011, 29, 218–228. [Google Scholar] [CrossRef]
- Ferreira, B.C.; Teixeira, P.S.; Geiane, A.S.; Maya, A.T.D.; Brasil, P.A.; Souza, V.C.; Cordova, C.; Ferreira, A.P.; Lima, R.M.; Nobrega, O.T. Effects of a 12-Week Exercise Training Program on Physical Function in Institutionalized Frail Elderly. J. Aging Res. 2018, 2018, 1–8. [Google Scholar] [CrossRef]
- Liao, Y.Y.; Chen, I.H.; Wang, R.Y. Effects of Kinect-based exergaming on frailty status and physical performance in prefrail and frail elderly: A randomized controlled trial. Sci. Rep. 2019, 9, 9353. [Google Scholar] [CrossRef]
- Faber, M.J.; Bosscher, R.J.; Chin, A.; Paw, M.J.; van Wieringen, P.C. Effects of exercise programs on falls and mobility in frail and pre-frail older adults: A multicenter randomized controlled trial. Arch. Phys. Med. Rehabil. 2006, 87, 885–896. [Google Scholar] [CrossRef]
- Cadore, E.L.; Rodriguez-Manas, L.; Sinclair, A.; Izquierdo, M. Effects of different exercise interventions on risk of falls, gait ability, and balance in physically frail older adults: A systematic review. Rejuvenation Res. 2013, 16, 105–114. [Google Scholar] [CrossRef]
- Riva, D.; Fani, M.; Benedetti, M.G.; Scarsini, A.; Rocca, F.; Mamo, C. Effects of High-Frequency Proprioceptive Training on Single Stance Stability in Older Adults: Implications for Fall Prevention. BioMed Res. Int. 2019, 2019, 1–11. [Google Scholar] [CrossRef]
- Martinez-Amat, A.; Hita-Contreras, F.; Lomas-Vega, R.; Caballero-Martinez, I.; Alvarez, P.J.; Martinez-Lopez, E. Effects of 12-week proprioception training program on postural stability, gait, and balance in older adults: A controlled clinical trial. J. Strength Cond. Res. 2013, 27, 2180–2188. [Google Scholar] [CrossRef]
- Aman, J.E.; Elangovan, N.; Yeh, I.; Konczak, J. The effectiveness of proprioceptive training for improving motor function: A systematic review. Front. Hum. Neurosci. 2014, 8, 1075. [Google Scholar] [CrossRef] [PubMed]
- Ferlinc, A.; Fabiani, E.; Velnar, T.; Gradisnik, L. The Importance and Role of Proprioception in the Elderly: A Short Review. Mater. Sociomed. 2019, 31, 219–221. [Google Scholar] [CrossRef] [PubMed]
- Srinivas-Shankar, U.; Wu, F. Frailty and Muscle Function: Role for Testosterone? Front. Horm. Res. 2009, 37, 133–149. [Google Scholar] [PubMed]
- Dodds, R.; Sayer, A.A. Sarcopenia and frailty: New challenges for clinical practice. Clin. Med. (Lond.) 2016, 16, 455–458. [Google Scholar] [CrossRef] [PubMed]
- Marzetti, E.; Leeuwenburgh, C. Skeletal muscle apoptosis, sarcopenia and frailty at old age. Exp. Gerontol. 2006, 41, 1234–1238. [Google Scholar] [CrossRef] [PubMed]
- Clegg, A.; Young, J. The frailty syndrome. Clin. Med. (Lond.) 2011, 11, 72–75. [Google Scholar] [CrossRef]
- Yarasheski, K.E.; Pak-Loduca, J.; Hasten, D.L.; Obert, K.A.; Brown, M.B.; Sinacore, D.R. Resistance exercise training increases mixed muscle protein synthesis rate in frail women and men ≥76 yr old. Am. J. Physiol. 1999, 277, E118–E125. [Google Scholar] [CrossRef] [PubMed]
- Haider, S.; Grabovac, I.; Dorner, T.E. Effects of physical activity interventions in frail and prefrail community-dwelling people on frailty status, muscle strength, physical performance and muscle mass—A narrative review. Wien. Klin. Wochenschr. 2019, 131, 244–254. [Google Scholar] [CrossRef]
- Bray, N.W.; Smart, R.R.; Jakobi, J.M.; Jones, G.R. Exercise prescription to reverse frailty. Appl. Physiol. Nutr. Metab. 2016, 41, 1112–1116. [Google Scholar] [CrossRef]
- Chen, R.; Wu, O.; Wang, D.; Li, Z.; Liu, H.; Liu, G.; Cui, Y.; Song, L. Effects of elastic band exercise on the frailty states in pre-frail elderly people. Physiother. Theory Pract. 2019, 11, 1–9. [Google Scholar] [CrossRef]
- Okubo, Y.; Schoene, D.; Lord, S.R. Step training improves reaction time, gait and balance and reduces falls in older people: A systematic review and meta-analysis. Br. J. Sports Med. 2017, 51, 586–593. [Google Scholar] [CrossRef] [PubMed]
- Stephen, R.L.; Delbaere, K.; Sturnieks, D.L. Chapter 10—Aging. Handb. Clin. Neurol. 2018, 159, 157–171. [Google Scholar]
- Porciattia, V.; Fiorentinia, A.; Morronea, M.C.; Burrab, D.C. The effects of ageing on reaction times to motion onset. Vis. Res. 1999, 39, 2157–2164. [Google Scholar] [CrossRef]
- Hernandez, A.; Silder, A.; Heiderscheit, B.C.; Thelen, D.G. Effect of age on center of mass motion during human walking. Gait Posture 2009, 30, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Osoba, M.Y.; Rao, A.K.; Agrawal, S.K.; Lalwani, A.K. Balance and gait in the elderly: A contemporary review. Laryngoscope Investig. Otolaryngol. 2019, 4, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Alfieri, F.M.; Riberto, M.; Abril-Carreres, A.; Boldo-Alcaine, M.; Rusca-Castellet, E.; Garreta-Figuera, R.; Battistella, L.R. Effectiveness of an exercise program on postural control in frail older adults. Clin. Interv. Aging 2012, 7, 593–598. [Google Scholar] [CrossRef] [PubMed]
- Pena, S.B.; Guimaraes, H.C.Q.C.P.; Lopes, J.L.; Guandalini, L.S.; Taminato, M.; Barbosa, D.A.; de Leite, B.A.L.B. Fear of falling and risk of falling: A systematic review and meta-analysis. Acta Paul. Enferm. 2019, 32, 4. [Google Scholar]
- Hadjistavropoulos, T.; Delbaere, K.; Fitzgerald, T.D. Reconceptualizing the Role of Fear of Falling and Balance Confidence in Fall Risk. J. Aging Health 2011, 23, 3–23. [Google Scholar] [CrossRef]
- Kendrick, D.; Kumar, A.; Carpenter, H.; Zijlstra, G.A.; Skelton, D.A.; Cook, J.R.; Stevens, Z.; Belcher, C.M.; Haworth, D.; Gawler, S.J.; et al. Exercise for reducing fear of falling in older people living in the community. Cochrane Database Syst. Rev. 2014, 28. [Google Scholar] [CrossRef]
- Jeoung, B.J. Relationships of exercise with frailty, depression, and cognitive function in older women. J. Exerc. Rehabil. 2014, 10, 291–294. [Google Scholar] [CrossRef]
- Gill, D.L.; Hammond, C.C.; Reifsteck, E.J.; Jehu, C.M.; Williams, R.A.; Adams, M.M.; Lange, E.H.; Becofsky, K.; Rodriguez, E.; Shang, Y. Physical Activity and Quality of Life. J. Prev. Med. Public Health 2013, 46, S28–S34. [Google Scholar] [CrossRef] [PubMed]
- Lina, Y.C.; Changa, J.C.; Chenb, Y.M.; Lic, C.M.; Huang, L.H. Health Related Quality of Life Among Frail and Pre-Frail Older Adults in Taiwan. Int. J. Gerontol. 2017, 11, 249–252. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Y.; Du, S.; Wang, Q.; Xia, H.; Sun, R. Exercise interventions for improving physical function, daily living activities and quality of life in community-dwelling frail older adults: A systematic review and meta-analysis of randomized controlled trials. Geriatr. Nurs. 2019, in press. [Google Scholar] [CrossRef]
- Oh, A.R.; Yi, E.S. A study on the effects of exercise motivation of the elderly people on euphoria. J. Exerc. Rehabil. 2017, 13, 387–392. [Google Scholar] [CrossRef] [PubMed]
| Beginner (Weeks 1 to 4) | Intermediate (Weeks 5 to 8) | Advanced (Weeks 9 to 12) |
|---|---|---|
| Proprioception Seated ankle ball Single leg stance (hip flexion) with support and with flexion and extension of knees Single leg stance (hip extension) with support and with flexion and extension of knees | Proprioception Standing ankle ball with support Single leg stance (hip flexion) with eyes closed and with support and with flexion and extension of knees Single leg stance (hip extension) with eyes closed and with support and with flexion and extension of knees | Proprioception Standing ankle ball without support Single leg stance (hip flexion) without support and with flexion and extension of the knee Single leg stance (hip extension) without support and with flexion and extension of knees |
| Muscle strengthening Seated alternate double knee lifts with weights Modified chair stands (Challenger) Seated alternate kicks with weighHip extension standing with support with weights | Muscle strengthening Sit-to-stand with support Knee raise standing with support and with weight Squats to a chair with supportStep back lunges with support | Muscle strengthening Sit-to-stand without support Knee raise standing without support and with weight Squats to a chair without support Step back lunges without support |
| Reaction time Seated alternate touches to front Seated alternate touches to back Seated alternate touches to side Seated alternate touches to 3 steps (forward, side, backward) | Reaction time Step-up with support Step forward standing with support Step backward standing with support Step to sides standing with support 3 steps standing (forward, side, and backward) with support | Reaction time Step up without support Step forward standing without support Step backward standing without support Step to sides standing without support 3 steps standing (forward, side, and backward) without support |
| Balance Seated alternate weight shifts Seated calf and toe raise Heel raise with support Crossover with support | Balance Heel-to-toe standing with support Side leg raise with support Heel raises without support Calf and toe raise without support Crossover without support | Balance Heel-to-toe without support Leaning star Heel walking Toe walking 8 shaped walking flex mat |
| Characteristics | MPE Group (n = 36) | Control Group (n = 36) | p-Value |
|---|---|---|---|
| Age (years), mean ± SD | 69.14 ± 3.55 | 68.89 ± 3.86 | 0.776 |
| 65–69, n (%) | 24 (66.7) | 23 (63.9) | |
| 70–74, n (%) | 8 (22.2) | 9 (25) | |
| ≥75, n (%) | 4 (11.1) | 4 (11.1) | |
| Number of comorbidities, mean ± SD | 0.86 ± 0.76 | 0.83 ± 0.60 | 0.865 |
| Number of drugs, mean ± SD | 0.86 ± 0.76 | 0.77 ± 0.54 | 0.594 |
| Body mass index ≠ (kg/m2), mean ± SD | 24.46 ± 4.06 | 24.32 ± 4.36 | 0.883 |
| Underweight <18.5, n (%) | 2 (5.6) | 4 (11.1) | |
| Normal weight 18.5–22.9, n (%) | 12 (33.3) | 9 (25) | |
| Overweight 23.0–27.5, n (%) | 15 (41.7) | 15 (41.7) | |
| Obese >27.5, n (%) | 7 (19.4) | 8 (22.2) | |
| Fall risk (Z-score), mean ± SD | 1.99 ± 0.58 | 1.97 ± 0.61 | 0.862 |
| Outcomes | Baseline a | Week 12 b | Week 24 c | p-Value Within Group |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Fall risk index score | ||||
| MPE Group | 1.99 ± 0.58 | −0.35 ± 0.72 | 1.13 ± 0.84 | <0.001 ab,ac,bc |
| Control Group | 1.97 ± 0.61 | 1.85 ± 0.59 | 2.22 ± 0.55 | <0.05 ac,bc |
| p-Value between Groups | 0.862 | <0.001 | <0.001 | |
| Edge-contrast sensitivity (dB) | ||||
| MPE Group | 21.13 ± 1.01 | 21.36 ± 1.15 | 21.27 ± 1.03 | 0.063 |
| Control Group | 21.05 ± 0.89 | 21.02 ± 0.81 | 20.97 ± 0.84 | 0.907 |
| p-Value between Groups | 0.713 | 0.160 | 0.173 | |
| Proprioception (degree error) | ||||
| MPE Group | 2.77 ± 1.60 | 0.48 ± 1.13 | 1.56± 1.48 | <0.001 ab,ac,bc |
| Control Group | 2.71 ± 1.44 | 3.13 ± 1.45 | 3.01 ± 1.73 | 0.383 |
| p-Value between Groups | 0.878 | <0.001 | <0.001 | |
| Knee extension strength (kg force) | ||||
| MPE Group | 13.87 ± 5.17 | 18.75 ± 6.03 | 13.06 ± 5.58 | <0.001 ab,bc |
| Control Group | 16.56 ± 7.31 | 13.20 ± 5.01 | 7.47 ± 4.85 | <0.001 ab,ac,bc |
| p-Value between Groups | 0.077 | <0.001 | <0.001 | |
| Hand reaction time (ms) | ||||
| MPE Group | 336.80 ± 67.91 | 251.98 ± 37.74 | 318.81 ± 60.57 | <0.001 ab,bc |
| Control Group | 345.76 ± 79.26 | 355.08 ± 45.73 | 386.40 ± 66.42 | 0.002 ac,bc |
| p-Value between Groups | 0.608 | <0.001 | <0.001 | |
| Sway path (mm2) | ||||
| MPE Group | 1642 ± 1038.05 | 452.41 ± 377.80 | 902.47 ± 473.75 | <0.001 ab,ac,bc |
| Control Group | 1433.08 ± 754.49 | 1018.86 ± 351.66 | 1209.52 ± 401.39 | 0.001 ab,bc |
| p-Value between Groups | 0.332 | <0.001 | 0.004 | |
| Outcomes | Baseline a | Week 12 b | Week 24 c | p-Value within Group |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | ||
| Fear of Fall Score | ||||
| MPE Group | 40.13 ± 6.60 | 18.05 ± 4.85 | 24.27 ± 12.23 | <0.001 ab,ac,bc |
| Control Group | 37.55 ± 13.00 | 25.69 ± 9.97 | 38.52 ± 12.47 | <0.001 ab,bc |
| p-Value between Groups | 0.292 | <0.001 | <0.001 | |
| Depression Score | ||||
| MPE Group | 2.77 ± 1.74 | 0.50 ± 0.87 | 2.58 ± 2.03 | <0.001 ab,bc |
| Control Group | 2.58 ± 2.28 | 1.16 ±0.77 | 2.30 ± 1.60 | <0.001 ab,bc |
| p-Value between Groups | 0.686 | 0.001 | 0.522 | |
| Overall Health-Related Quality of Life (HRQOL) | ||||
| MPE Group | 67.35 ± 10.82 | 93.91 ± 9.00 | 85.62 ± 12.34 | <0.001 ab,bc,ac |
| Control Group | 76.96 ± 8.66 | 90.42 ± 1.68 | 81.96 ± 7.86 | <0.001 ab,bc,ac |
| p-Value between Groups | <0.001 | 0.025 | 0.138 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chittrakul, J.; Siviroj, P.; Sungkarat, S.; Sapbamrer, R. Multi-System Physical Exercise Intervention for Fall Prevention and Quality of Life in Pre-Frail Older Adults: A Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 3102. https://doi.org/10.3390/ijerph17093102
Chittrakul J, Siviroj P, Sungkarat S, Sapbamrer R. Multi-System Physical Exercise Intervention for Fall Prevention and Quality of Life in Pre-Frail Older Adults: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2020; 17(9):3102. https://doi.org/10.3390/ijerph17093102
Chicago/Turabian StyleChittrakul, Jiraporn, Penprapa Siviroj, Somporn Sungkarat, and Ratana Sapbamrer. 2020. "Multi-System Physical Exercise Intervention for Fall Prevention and Quality of Life in Pre-Frail Older Adults: A Randomized Controlled Trial" International Journal of Environmental Research and Public Health 17, no. 9: 3102. https://doi.org/10.3390/ijerph17093102
APA StyleChittrakul, J., Siviroj, P., Sungkarat, S., & Sapbamrer, R. (2020). Multi-System Physical Exercise Intervention for Fall Prevention and Quality of Life in Pre-Frail Older Adults: A Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 17(9), 3102. https://doi.org/10.3390/ijerph17093102






