Some Near- and Far-Environmental Effects on Human Health and Disease with a Focus on the Cardiovascular System
Abstract
1. Introduction
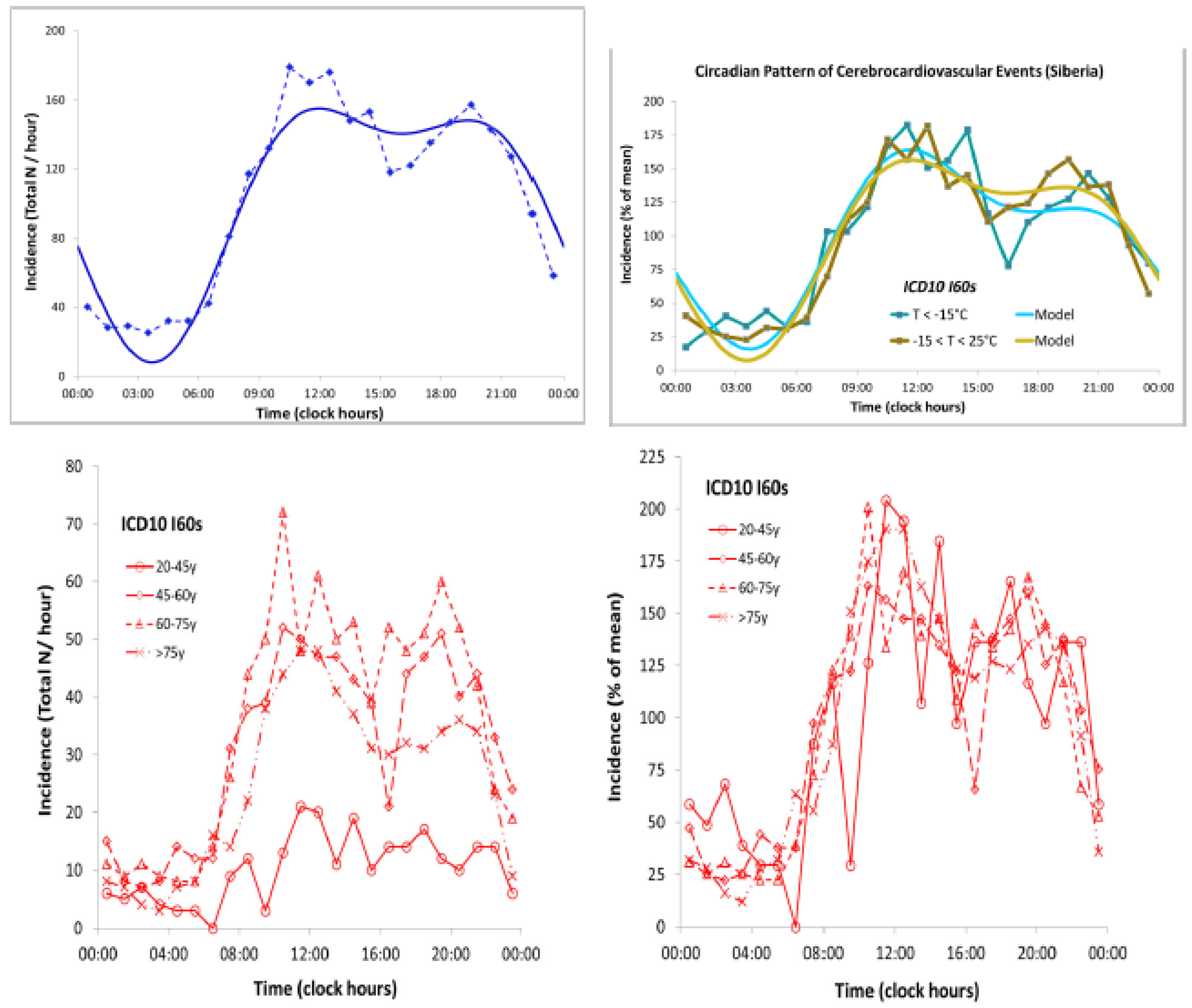
2. Ubiquitous, Partly Endogenous Circadian Rhythms Synchronized by Light
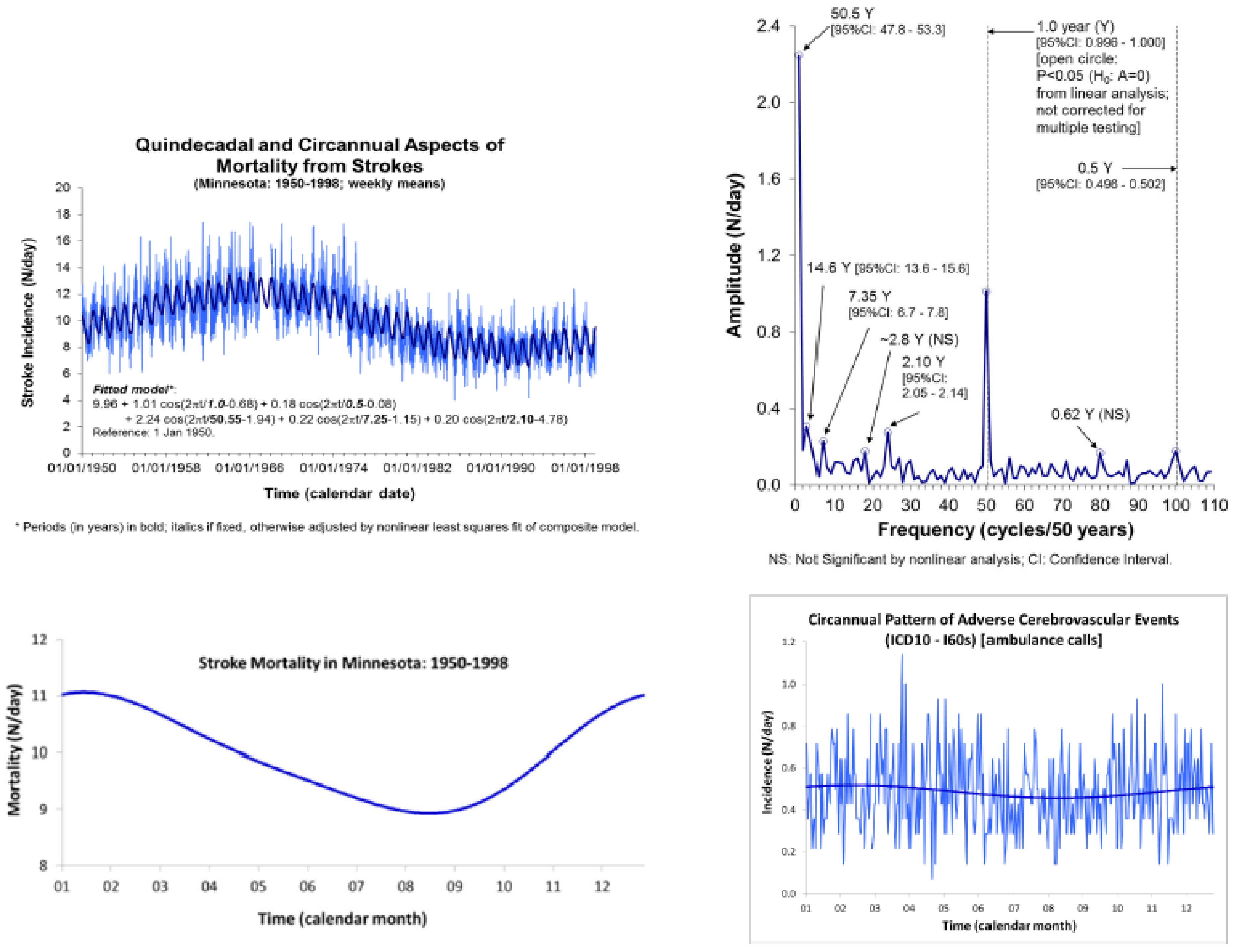
3. Effects of Weather on Human Physiopathology
4. Effects of Atmospheric Temperature and Pressure on Stroke Events
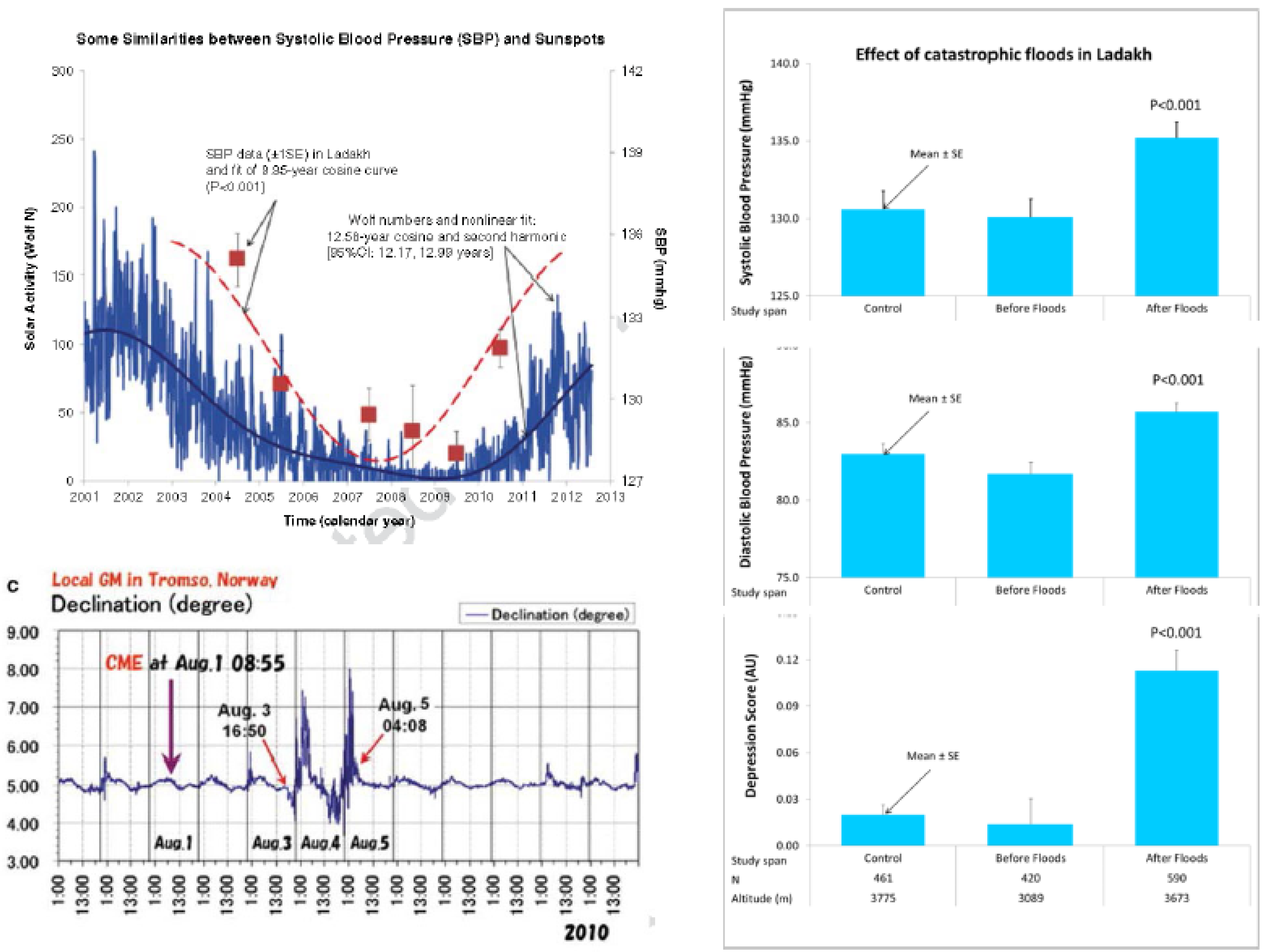
5. Periodicities in Weather Conditions
6. Effects of Space Weather on Human Physiopathology
6.1. Circaseptans
6.2. Circatrigintans
6.3. Cis-Half-Year
6.4. Transyear
6.5. Multidecadals
7. Possible Underlying Mechanisms
8. Conclusions
Author Contributions
Funding
Acknowledgments
Dedication
Conflicts of Interest
References
- Remoundou, K.; Koundouri, P. Environmental effects on public health: An economic perspective. Int. J. Environ. Res. Public Health 2009, 6, 2160–2178. [Google Scholar] [CrossRef] [PubMed]
- Invally, M.; Kaur, G.I.; Kaur, G.A.; Kaur Bhullar, S.; Buttar, H.S. Health care burden of cardiorespiratory diseases caused by particulate matter and chemical air pollutants. World Heart J. 2017, 9, 303–317. [Google Scholar]
- Cai, X.; Li, Z.; Scott, E.M.; Li, X.; Tang, M. Short-term effects of atmospheric particulate matter on myocardial infarction: A cumulative meta-analysis. Environ. Sci. Pollut. Res. Int. 2016, 23, 6139–6148. [Google Scholar] [CrossRef]
- Fedacko, J.; Singh, R.B.; Mojto, V.; Elkilany, G.; Hristova, K.; Pella, D.; Chaves, H. Air pollution and the global heart health: A view point of the International College of Cardiology. World Heart J. 2017, 9, 269–272. [Google Scholar]
- An, Z.; Jin, Y.; Li, J.; Li, W.; Wu, W. Impact of particulate air pollution on cardiovascular health. Curr. Allergy Asthma Rep. 2018, 18, 15. [Google Scholar] [CrossRef]
- Halberg, F.; Cornelissen, G.; Sothern, R.B.; Hillman, D.; Watanabe, Y.; Haus, E.; Schwartzkopff, O.; Best, W.R. Decadal cycles in the human cardiovascular system. World Heart J. 2012, 4, 263–287. [Google Scholar]
- Halberg, F.; Cornelissen, G.; Hillman, D.; Beaty, L.; Hong, S.; Schwartzkopff, O.; Watanabe, Y.; Otsuka, K.; Siegelova, J. Chronobiologically interpreted ambulatory blood pressure monitoring in health and disease. Glob. Adv. Health Med. 2012, 1, 64–88. [Google Scholar] [CrossRef]
- Shearman, L.P.; Sriram, S.; Weaver, D.R.; Maywood, E.S.; Chaves, I.; Zheng, B.; Kume, K.; Lee, C.C.; van der Horst, G.T.; Hastings, M.H.; et al. Interacting molecular loops in the mammalian circadian clock. Science 2000, 288, 1013–1019. [Google Scholar] [CrossRef]
- Abbott, S.M.; Malkani, R.G.; Zee, P.C. Circadian disruption and human health: A bidirectional relationship. Eur. J. Neurosci. 2020, 51, 567–583. [Google Scholar] [CrossRef]
- Wang, D.; Ruan, W.; Chen, Z.; Peng, Y.; Li, W. Shift work and risk of cardiovascular disease morbidity and mortality: A dose response meta-analysis of cohort studies. Eur. J. Prev. Cardiol. 2018, 25, 1293–1302. [Google Scholar] [CrossRef]
- Halberg, F.; Halberg, E.; Barnum, C.P.; Bittner, J.J. Physiologic 24-hour periodicity in human beings and mice, the lighting regimen and daily routine. In Photoperiodism and Related Phenomena in Plants and Animals; Withrow, R.B., Ed.; The American Association for the Advancement of Science: Washington DC, USA, 1959; pp. 803–878. [Google Scholar]
- Challet, E.; Pevet, P. Interactions between photic and nonphotic stimuli to synchronize the master circadian clock in mammals. Front. Biosci. 2003, 8, s246–s257. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Willich, S.N.; Linderer, T.; Wegscheider, K.; Leizorovicz, A.; Alamercery, I.; Schröder, R. Increased morning incidence of myocardial infarction in the ISAM Study: Absence with prior beta-adrenergic blockade. ISAM Study Group Circ. 1989, 80, 853–858. [Google Scholar] [CrossRef] [PubMed]
- Cornelissen, G.; Breus, T.K.; Bingham, C.; Zaslavskaya, R.; Varshitsky, M.; Mirsky, B.; Teibloom, M.; Tarquini, B.; Bakken, E.; Halberg, F. International Womb-to-Tomb Chronome Initiative Group. Beyond circadian chronorisk: Worldwide circaseptan-circasemiseptan patterns of myocardial infarctions, other vascular events, and emergencies. Chronobiologia 1993, 20, 87–115. [Google Scholar] [PubMed]
- Fornasari, P.M.; Gratton, L.; Dolci, D.; Gamba, G.; Ascari, E.; Montalbetti, N.; Halberg, F. Circadian rhythms of clotting, fibrinolytic activators and inhibitors. In Chronobiology; Halberg, F., Scheving, L.E., Powell, E.W., Hayes, D.K., Eds.; Il Ponte: Milan, Italy, 1981; pp. 155–158. [Google Scholar]
- Cornelissen, G.; Tamura, K.; Tarquini, B.; Germanò, G.; Fersini, C.; Rostagno, C.; Zaslavskaya, R.M.; Carandente, O.; Carandente, F.; Halberg, F. Differences in some circadian patterns of cardiac arrhythmia, myocardial infarction and other adverse vascular events. Chronobiologia 1994, 21, 79–88. [Google Scholar] [PubMed]
- Smolensky, M.; Halberg, F.; Sargent, F., II. Chronobiology of the life sequence. In Advances in Climatic Physiology; Itoh, S., Ogata, K., Yoshimura, H., Eds.; Igaku Shoin Ltd.: Tokyo, Japan, 1972; pp. 281–318. [Google Scholar]
- Diaz, A.; Ferrante, D.; Badra, R.; Morales, I.; Becerra, A.; Varini, S.; Nul, D.; Grancelli, H.; Doval, H. Seasonal variation and trends in heart failure morbidity and mortality in a South American community hospital. Congest. Heart Fail. 2007, 13, 263–266. [Google Scholar] [CrossRef] [PubMed]
- Jakovljevic, D.; Salomaa, V.; Sivenius, J.; Tamminen, M.; Sarti, C.; Salmi, K.; Kaarsalo, E.; Narva, V.; Immonen-Raiha, P.; Torppa, J.; et al. Seasonal variation in the occurrence of stroke in a Finnish adult population. The FINMONICA Stroke Register. Finnish Monitoring Trends and Determinants in Cardiovascular Disease. Stroke 1996, 27, 1774–1779. [Google Scholar] [CrossRef]
- Marti-Soler, H.; Gonseth, S.; Gubelmann, C.; Stringhini, S.; Bovet, P.; Chen, P.C.; Wojtyniak, B.; Paccaud, F.; Tsai, D.H.; Zdrojewski, T.; et al. Seasonal variation of overall and cardiovascular mortality: A study in 19 countries from different geographic locations. PLoS ONE 2014, 9, e113500. [Google Scholar] [CrossRef]
- Marti-Soler, H.; Gubelmann, C.; Aeschbacher, S.; Alves, L.; Bobak, M.; Bongard, V.; Clays, E.; de Gaetano, G.; Di Castelnuovo, A.; Elosua, R.; et al. Seasonality of cardiovascular risk factors: An analysis including over 230 000 participants in 15 countries. Heart 2014, 100, 1517–1523. [Google Scholar] [CrossRef]
- Frohlich, M.; Sund, M.; Russ, S.; Hoffmeister, A.; Fischer, H.G.; Hombach, V.; Koenig, W. Seasonal variations of rheological and hemostatic parameters and acute-phase reactants in young, healthy subjects. Arterioscler. Thromb. Vasc. Biol. 1997, 17, 2692–2697. [Google Scholar] [CrossRef]
- Qian, Z.; Lin, H.M.; Stewart, W.F.; Kong, L.; Xu, F.; Zhou, D.; Zhu, Z.; Liang, S.; Chen, W.; Shah, N.; et al. Seasonal pattern of the acute mortality effects of air pollution. J. Air Waste Manag. Assoc. 2010, 60, 481–488. [Google Scholar] [CrossRef]
- Barnett, A.G.; de Looper, M.; Fraser, J.F. The seasonality in heart failure deaths and total cardiovascular deaths. Aust. N. Z. J. Public Health 2008, 32, 408–413. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Zhou, M.; Ou, C.Q.; Yin, P.; Li, M.; Tong, S.; Gasparrini, A.; Liu, X.; Li, J.; Cao, L.; et al. Seasonal variations of temperature-related mortality burden from cardiovascular disease and myocardial infarction in China. Environ. Pollut. 2017, 224, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Danet, S.; Richard, F.; Montaye, M.; Beauchant, S.; Lemaire, B.; Graux, C.; Cottel, D.; Marecaux, N.; Amouyel, P. Unhealthy effects of atmospheric temperature and pressure on the occurrence of myocardial infarction and coronary deaths. A 10-year survey: The Lille-World Health Organization MONICA project (Monitoring trends and determinants in cardiovascular disease). Circulation 1999, 100, E1–E7. [Google Scholar] [CrossRef] [PubMed]
- Minnesota Department of Health. Data, Statistics & Legislation. Available online: http://www.health.state.mn.us/index.html (accessed on 1 April 2017).
- Cornelissen, G.; Halberg, F.; Breus, T.; Syutkina, E.V.; Baevsky, R.; Weydahl, A.; Watanabe, Y.; Otsuka, K.; Siegelova, J.; Fiser, B.; et al. Non-photic solar associations of heart rate variability and myocardial infarction. J. Atmos. Solar Terr. Phys. 2002, 64, 707–720. [Google Scholar] [CrossRef]
- Ohshige, K.; Hori, Y.; Tochikubo, O.; Sugiyama, M. Influence of weather on emergency transport events coded as stroke: Population-based study in Japan. Int. J. Biometeorol. 2006, 50, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Cao, Y.; Hong, D.; Zheng, D.; Richtering, S.; Sandset, E.C.; Leong, T.H.; Arima, H.; Islam, S.; Salam, A.; et al. Ambient temperature and stroke occurrence: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2016, 13, 698. [Google Scholar] [CrossRef]
- Johansson, B.B.; Norrving, B.; Widner, H.; Wu, J.; Halberg, F. Stroke incidence: Circadian and circaseptan (about weekly) variation in onset. Prog. Clin. Biol. Res. 1990, 341, 427–436. [Google Scholar]
- Abbot, C.G. Solar Variation and Weather, a Summary of the Evidence, Completely Illustrated and Documented; Smithsonian Miscellaneous Collections: Washington DC, USA, 1963; p. 4545. [Google Scholar]
- Halberg, F.; Breus, T.K.; Cornelissen, G.; Bingham, C.; Hillman, D.C.; Rigatuso, J.; Delmore, P.; Bakken, E.; International Womb-to-Tomb Chronome Initiative Group. Chronobiology in Space; Medtronic: Minnespolis, MN, USA, 1991. [Google Scholar]
- Vladimirskii, B.M.; Narmanskii, V.Y.; Temuriantz, N.A. Global rhythmics of the solar system in the terrestrial habitat. Biophysics 1995, 40, 731–736. [Google Scholar]
- Cornelissen, G.; Engebretson, M.; Johnson, D.; Otsuka, K.; Burioka, N.; Posch, J.; Halberg, F. The week, inherited in neonatal human twins, found also in geomagnetic pulsations in isolated Antarctica. Biomed. Pharm. 2001, 55, s32–s50. [Google Scholar] [CrossRef]
- Hildebrandt, G.; Bandt-Reges, I. Chronobiologie in Der Naturheilkunde: Grundlagen Der Circaseptanperiodik; Haug: Heidelberg, Germany, 1992; p. 102. [Google Scholar]
- Cornelissen, G.; Halberg, F. The biological week and broader time structures (chronomes): In memory of Gunther Hildebrandt. Percept. Motor Skills 2000, 90, 579–586. [Google Scholar] [CrossRef]
- Reimann, H.A. Periodic Diseases; Blackwell: Oxford, UK, 1963. [Google Scholar]
- Halberg, F.; Cornelissen, G.; Bernhardt, K.-H.; Sampson, M.; Schwartzkopff, O.; Sonntag, D. Egeson’s (George’s) transtridecadal weather cycling and sunspots. Hist. Geo Space Sci. 2010, 1, 49–61. [Google Scholar] [CrossRef] [PubMed]
- Halberg, F.; Cornelissen, G.; Czaplicki, J.; Prabhakaran Nayar, S.R.; Siegelova, J. Brückner-Egeson-Lockyer (BEL) climate cycle in original Brückner’s, Lockyer’s and follow-up data. In Proceedings, Noninvasive Methods in Cardiology; Halberg, F., Kenner, T., Fiser, B., Siegelova, J., Eds.; Masaryk University: Brno, Czech, 2008; pp. 74–89. [Google Scholar]
- Cornelissen, G.; Prabhakaran Nayar, S.R.; Czaplicki, J.; Siegelova, J.; Mendoza, B.; Halberg, F. Brückner-Egeson-Lockyer (BEL) cycle in heliogeomagnetics. In Proceedings, Noninvasive Methods in Cardiology; Halberg, F., Kenner, T., Fiser, B., Siegelova, J., Eds.; Masaryk University: Brno, Czech, 2008; pp. 106–115. [Google Scholar]
- Cornelissen, G.; Otsuka, K.; Halberg, F. Remove and replace for a scrutiny of space weather and human affairs. In Proceedings, International Conference, Space Weather Effects in Humans: In Space and on Earth; Grigoriev, A.I., Zeleny, L.M., Eds.; Space Research Institute: Moscow, Russia, 2013; pp. 508–538. [Google Scholar]
- Vallot, J.; Sardou, G.; Faure, M. De l’influence des taches solaires sur les accidents aigus des maladies chroniques. Académie de Médecine-Gazette des Hôpitaux 1922, 56, 904–905. [Google Scholar]
- Cornelissen, G.; Siegelova, J.; Halberg, F. Blood pressure and heart rate dynamics during pregnancy and early extra-uterine life: Methodology for a chrononeonatology. In Proceedings, Symposium: The Importance of Chronobiology in Diagnosing and Therapy of Internal Diseases; Halberg, F., Kenner, T., Fiser, B., Eds.; Masaryk University: Brno, Czech, 2002; pp. 58–96. [Google Scholar]
- Syutkina, E.V.; Cornelissen, G.; Yatsyk, G.; Studenikin, M.; Baranov, A.; Halberg, F. Over a decade of clinical chrononeonatology and chronopediatrics in Moscow. Neuroendocrinol. Lett. 2003, 24, 132–138. [Google Scholar]
- Cornelissen, G.; Halberg, F.; Wendt, H.W.; Bingham, C.; Sothern, R.B.; Haus, E.; Kleitman, E.; Kleitman, N.; Revilla, M.A.; Revilla, M., Jr.; et al. Resonance of about-weekly human heart rate rhythm with solar activity change. Biologia 1996, 51, 749–756. [Google Scholar] [PubMed]
- Amiranashvili, A.G.; Cornelissen, G.; Amiranashvili, V.; Gheonjian, L.; Chikhladze, V.A.; Gogua, R.A.; Matiashvili, T.G.; Paatashvili, T.; Kopytenko, Y.A.; Siegelova, J.; et al. Circannual and circadecennian stages in mortality from cardiovascular causes in Tbilisi, Republic of Georgia (1980–1992). Scr. Med. 2002, 75, 255–260. [Google Scholar]
- Halberg, F.; Düll-Pfaff, N.; Gumarova, L.; Zenchenko, T.A.; Schwartzkopff, O.; Freytag, E.M.; Freytag, J.; Cornelissen, G. 27-day cycles in human mortality: Traute and Bernhard Düll. Hist. Geo Space Sci. 2013, 4, 47–59. [Google Scholar] [CrossRef][Green Version]
- Rieger, A.; Share, G.H.; Forrest, D.J.; Kanbach, G.; Reppin, C.; Chupp, E.L. A 154-day periodicity in the occurrence of hard solar flares? Nature 1984, 312, 623–625. [Google Scholar] [CrossRef]
- Cornelissen, G.; Halberg, F.; Sothern, R.B.; Hillman, D.C.; Siegelova, J. Blood pressure, heart rate and melatonin cycles synchronization with the season, earth magnetism and solar flares. Scr. Med. 2010, 83, 16–32. [Google Scholar]
- Cornelissen, G.; Tarquini, R.; Perfetto, F.; Otsuka, K.; Gigolashvili, M.; Halberg, F. Investigation of solar about 5-month cycle in human circulating melatonin: Signature of weather in extraterrestrial space? Sun Geosph. 2009, 4, 55–59. [Google Scholar]
- Cornelissen, G.; Burioka, N.; Halberg, F. Other-than-annual variations in morning determinations of uric acid. Clin. Chem. Lab. Med. 2012, 50, 765–770. [Google Scholar] [CrossRef]
- Cornelissen, G.; Halberg, F.; Rostagno, C.; Otsuka, K. A chronomic approach to cardiac arrhythmia and sudden cardiac death. In Proceedings of the 59th Annual Meeting, Japan Society of Neurovegetative Research, Tokyo, Japan, 23–26 May 2018; pp. 56–59. [Google Scholar]
- Richardson, J.D.; Paularena, K.I.; Belcher, J.W.; Lazarus, A.J. Solar wind oscillations with a 1.3-year period. Geophys. Res. Lett. 1994, 21, 1559–1560. [Google Scholar] [CrossRef]
- Cornelissen, G.; Masalov, A.; Halberg, F.; Richardson, J.D.; Katinas, G.S.; Sothern, R.B.; Watanabe, Y.; Syutkina, E.V.; Wendt, H.W.; Bakken, E.E.; et al. Multiple resonances among time structures, chronomes, around and in us. Is an about 1.3-year periodicity in solar wind built into the human cardiovascular chronome? Hum. Physiol. 2004, 30, 202–208. [Google Scholar] [CrossRef]
- Halberg, F.; Cornelissen, G.; Panksepp, J.; Otsuka, K.; Johnson, D. Chronomics of autism and suicide. Biomed. Pharmacother. 2005, 59, S100–S108. [Google Scholar] [CrossRef]
- Halberg, F.; Cornelissen, G.; Otsuka, K.; Watanabe, Y.; Katinas, G.S.; Burioka, N.; Delyukov, A.; Gorgo, Y.; Zhao, Z.Y.; Weydahl, A.; et al. International BIOCOS Study Group. Cross-spectrally coherent ~10.5- and 21-year biological and physical cycles, magnetic storms and myocardial infarctions. Neuroendocrinol. Lett. 2000, 21, 233–258. [Google Scholar] [PubMed]
- Cornelissen, G.; Halberg, F.; Gheonjian, L.; Paatashvili, T.; Faraone, P.; Watanabe, Y.; Otsuka, K.; Sothern, R.B.; Breus, T.; Baevsky, R.; et al. Schwabe’s ~10.5- and Hale’s ~21-year cycles in human pathology and physiology. In Long- and Short-Term Variability in Sun’s History and Global Change; Schröder, W., Ed.; Science Edition: Bremen, Germany, 2000; pp. 79–88. [Google Scholar]
- Halberg, F.; Powell, D.; Otsuka, K.; Watanabe, Y.; Beaty, L.A.; Rosch, P.; Czaplicki, J.; Hillman, D.; Schwartzkopff, O.; Cornelissen, G. Diagnosing vascular variability anomalies, not only MESOR-hypertension. Am. J. Physiol. Heart Circ. Physiol. 2013, 305, H279–H294. [Google Scholar] [CrossRef] [PubMed]
- Kawasaki, T.; Yatagai, A.; Nakaoka, T.; Otsuka, K.; Otsuka, Y.; Watanabe, Y.; Otsuka, K.; Okumiya, K.; Matsubayashi, K.; Norboo, T.; et al. Astro-glocal spatially and temporally (global and local) comprehensive health watch, especially at high altitude. In Proceedings, International Conference, Space Weather Effects in Humans: In Space and on Earth; Grigoriev, A.I., Zeleny, L.M., Eds.; Space Research Institute: Moscow, Russia, 2013; pp. 539–550. [Google Scholar]
- Baevsky, R.M.; Petrov, V.M.; Cornelissen, G.; Halberg, F.; Orth-Gomér, K.; Åkerstedt, T.; Otsuka, K.; Breus, T.; Siegelova, J.; Dusek, J.; et al. Meta-analyzed heart rate variability, exposure to geomagnetic storms, and the risk of ischemic heart disease. Scr. Med. 1997, 70, 199–204. [Google Scholar]
- Otsuka, K.; Cornelissen, G.; Weydahl, A.; Holmeslet, B.; Hansen, T.L.; Shinagawa, M.; Kubo, Y.; Nishimura, Y.; Omori, K.; Yano, S.; et al. Geomagnetic disturbance associated with decrease in heart rate variability in a subarctic area. Biomed. Pharmacother. 2001, 55, 51–56. [Google Scholar] [CrossRef]
- Oinuma, S.; Kubo, Y.; Otsuka, K.; Yamanaka, T.; Murakami, S.; Matsuoka, O.; Ohkawa, S.; Cornelissen, G.; Weydahl, A.; Holmeslet, B.; et al. On behalf of the “ICEHRV” Working Group. Graded response of heart rate variability, associated with an alteration of geomagnetic activity in a subarctic area. Biomed. Pharmacother. 2002, 56, 284–288. [Google Scholar] [CrossRef]
- Cornelissen, G.; Halberg, F.; Schwartzkopff, O.; Delmore, P.; Katinas, G.; Hunter, D.; Tarquini, B.; Tarquini, R.; Perfetto, F.; Watanabe, Y.; et al. Chronomes, time structures, for chronobioengineering for “a full life”. Biomed. Instrum. Technol. 1999, 33, 152–187. [Google Scholar]
- Palmer, S.J.; Rycroft, M.J.; Cermack, M. Solar and geomagnetic activity, extremely low frequency magnetic and electric fields and human health at the Earth’s surface. Surv. Geophys. 2006, 27, 557–595. [Google Scholar] [CrossRef]
- Burch, J.B.; Reif, J.S.; Noonan, C.W.; Yost, M.G. Melatonin metabolite levels in workers exposed to 60-Hz magnetic fields: Work in substations and with 3-phase conductors. J. Occup. Environ. Med. 2000, 42, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Burch, J.B.; Reif, J.S.; Yost, M.G. Geomagnetic activity and human melatonin metabolite excretion. Neurosci. Lett. 2008, 438, 76–79. [Google Scholar] [CrossRef] [PubMed]
- Wilson, B.W. Chronic exposure to ELF fields may induce depression. Bioelectromagnetics 1988, 9, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Shinba, T.; Kariya, N.; Matsuda, S.; Matsuda, H.; Obara, Y. Increase of frontal cerebral blood volume during transcranial magnetic stimulation in depression is related to treatment effectiveness: A pilot study with near-infrared spectroscopy. Psychiatry Clin. Neurosci. 2018, 72, 602–610. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.X.; Hilburn, I.A.; Wu, D.A.; Mizuhara, Y.; Cousté, C.P.; Abrahams, J.N.H.; Bernstein, S.E.; Matani, A.; Shimojo, S.; Kirschvink, J.L. Transduction of the geomagnetic field as evidenced from alpha-band activity in the human brain. eNeuro 2019, 6. [Google Scholar] [CrossRef]
- Ulmer, W.; Cornelissen, G.; Halberg, F. Physical chemistry and the biologic week in the perspective of chrono-oncology. In Vivo 1995, 9, 363–374. [Google Scholar]
- Cherry, N. Schumann resonances, a plausible biophysical mechanism for the human health effects of solar/geomagnetic activity. Nat. Hazards 2002, 26, 279–331. [Google Scholar] [CrossRef]
- McCraty, R.; Atkinson, M.; Stolc, V.; Alabdulgader, A.A.; Vainoras, A.; Ragulskis, M. Synchronization of human autonomic nervous system rhythms with geomagnetic activity in human subjects. Int. J. Environ. Res. Public Health 2017, 14, 770. [Google Scholar] [CrossRef]
- Alabdulgader, A.A. The human heart rate variability; neurobiology of psychophysiological well being and planetary resonance. Gen. Int. Med. Clin. Innov. 2017, 2. [Google Scholar] [CrossRef]
- Mc Craty, R. The energetic heart. Bioelectromagnetic interactions within and between people. In Clinical Applications of Bioelectromagnetic Medicine; Rosch, P.J., Markov, M.S., Eds.; Marcel Dekker: New York, NY, USA, 2004; pp. 541–562. [Google Scholar]
- Cornelissen, G.; Gilge, S.; Halberg, F. Nonphotic extra-annuality, notably transyears, complement dominant photic year and day in the atmosphere. In Proceedings of the 1st International Workshop, Physiology of Adaptation and Quality of Life: Problems of Traditional Medicine and Innovation, People’s Friendship University of Russia, Moscow, Russia, 14–16 May 2008; pp. 391–395. [Google Scholar]
- Turtoi, C.; Cornelissen, G.; Wilson, D.; Halberg, F. About 21-year Hale cyclic signature in agriculture complements those in biomedicine. Biomed. Pharmacother. 2004, 58, S12–S14. [Google Scholar] [CrossRef]
- Schove, D.J. Sunspot Cycles. In Benchmark Papers in Geology/68; Hutchinson Ross: Stroudsburg, PA, USA, 1983; p. 397. [Google Scholar]
- Labitzke, K.; van Loon, H. Some recent studies of probable connection between solar and atmospheric variability. Ann. Geophys. 1993, 11, 1084–1094. [Google Scholar]
- Kondratiev, N.D. The long waves in economic life. Rev. Econ. Stat. 1935, 17, 105–115. [Google Scholar] [CrossRef]
- Milburn, W. Oriental Commerce; Black, Parry & Co.: London, UK, 1813; Volume 1. [Google Scholar]
- Clarke, H. Physical Economy: A preliminary inquiry into the physical laws governing the periods of famines and panics. Railw. Regist. 1847, 5, 155–169. [Google Scholar]
- Cornelissen, G.; Khasigawala, P.; Hillman, D.; Siegelova, J.; Halberg, F. Sunspot cycles drive the cardiovascular system in a unified science. In Noninvasive Methods in Cardiology; Kenner, T., Cornelissen, G., Siegelova, J., Dobsak, P., Eds.; Masaryk University: Brno, Czech, 2013; pp. 79–86. [Google Scholar]
- Barker, D.J.; Thornburg, K.L. The obstetric origins of health for a lifetime. Clin. Obstet. Gynecol. 2013, 56, 511–519. [Google Scholar] [CrossRef]
- Skjaervo, G.R.; Fossoy, F.; Roskaft, E. Solar activity at birth predicted infant survival and women’s fertility in historical Norway. Proceedings of the Royal Society of London—Series B. Biol. Sci. 2015, 282, 20142032. [Google Scholar] [CrossRef]
- Halberg, F.; Cornelissen, G.; Sothern, R.B.; Czaplicki, J.; Schwartzkopff, O. 35-year climate cycle in heliogeophysics, psychophysiology, military politics, and economics. Geophys. Process. Biosph. 2009, 8, 13–42. [Google Scholar]
- Janashia, K.; Tvildiani, L.; Tsibadze, T.; Invia, N.; Kukhianidze, V.; Ramishvili, G. Effects of magneto active compensation of geomagnetic field on heart rate variability of healthy males. Sun Geosph. 2020, in press. [Google Scholar]
- Gurfinkel, Y.; Ljubimov, V. The shielding room in clinic for protection of patients with IHD from influence of geomagnetic disturbances. Med. Phys. 2004, 3, 34–39. Available online: https://www.med2000.ru/art300/artikl309.htm (accessed on 21 July 2017).
- Cornelissen, G.; Beaty, L.A.; Siegelova, J.; Gierke, C.L.; Otsuka, K.; Watanabe, Y.; Syutkina, E.V.; Masalov, A.; Gumarova, L.; Halberg, F. An atlas of chronomes to map broad time structures. In Noninvasive Methods in Cardiology; Kenner, T., Cornelissen, G., Siegelova, J., Dobsak, P., Eds.; Masaryk University: Brno, Czech, 2013; pp. 102–116. [Google Scholar]
- Cornelissen, G.; Beaty, L.A.; Gierke, C.L.; Gumarova, L.; Otsuka, K.; Watanabe, Y.; Wang, Z.; Siegelova, J. Atlas of chronomes: A work in progress. In Noninvasive Methods of Cardiology; Kenner, T., Cornelissen, G., Siegelova, J., Dobsak, P., Eds.; Masaryk University: Brno, Czech, 2014; pp. 87–97. [Google Scholar]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cornelissen Guillaume, G.; Gubin, D.; Beaty, L.A.; Otsuka, K. Some Near- and Far-Environmental Effects on Human Health and Disease with a Focus on the Cardiovascular System. Int. J. Environ. Res. Public Health 2020, 17, 3083. https://doi.org/10.3390/ijerph17093083
Cornelissen Guillaume G, Gubin D, Beaty LA, Otsuka K. Some Near- and Far-Environmental Effects on Human Health and Disease with a Focus on the Cardiovascular System. International Journal of Environmental Research and Public Health. 2020; 17(9):3083. https://doi.org/10.3390/ijerph17093083
Chicago/Turabian StyleCornelissen Guillaume, Germaine, Denis Gubin, Larry A Beaty, and Kuniaki Otsuka. 2020. "Some Near- and Far-Environmental Effects on Human Health and Disease with a Focus on the Cardiovascular System" International Journal of Environmental Research and Public Health 17, no. 9: 3083. https://doi.org/10.3390/ijerph17093083
APA StyleCornelissen Guillaume, G., Gubin, D., Beaty, L. A., & Otsuka, K. (2020). Some Near- and Far-Environmental Effects on Human Health and Disease with a Focus on the Cardiovascular System. International Journal of Environmental Research and Public Health, 17(9), 3083. https://doi.org/10.3390/ijerph17093083






