Determining the Optimal Outcome Measures for Studying the Social Determinants of Health
Abstract
1. Highlights
1.1. What Do We Already Know about This Topic?
1.2. How Does Your Research Contribute to the Field?
1.3. What Are Your Research’s Implications towards Theory, Practice, or Policy?
2. Background
2.1. Measure Selection in Social Policy RCTs
2.2. The Quantitative Shotgun Approach
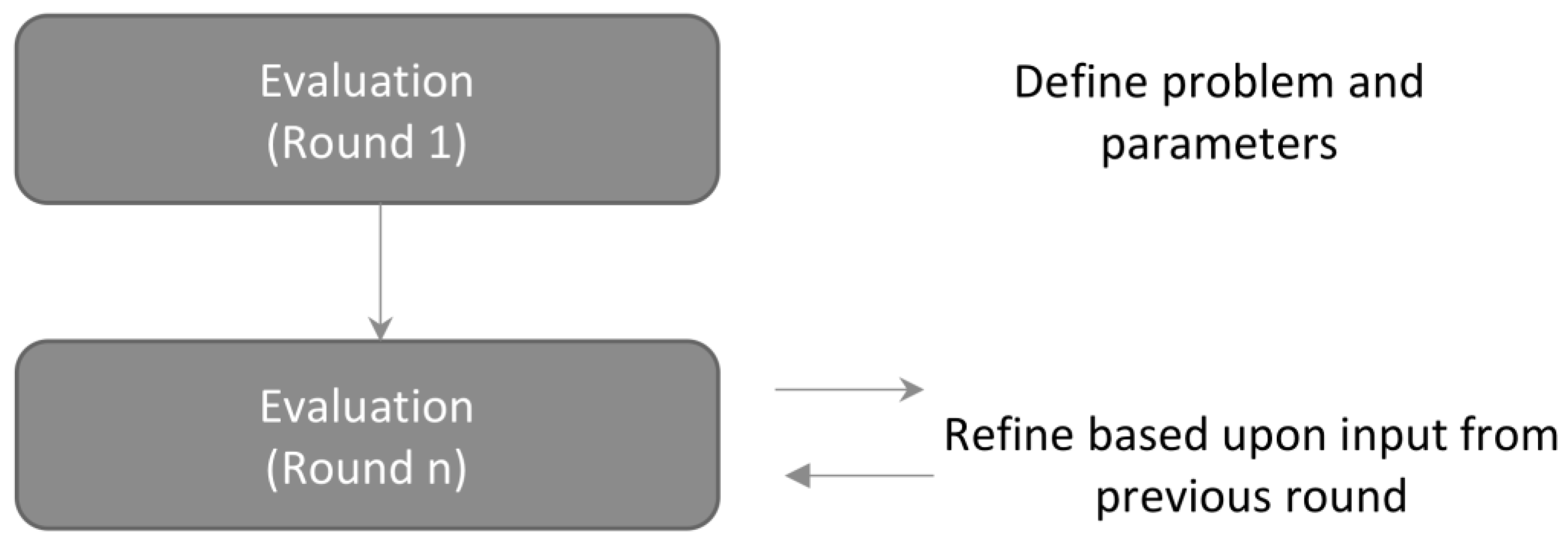
2.3. The Delphi Method
3. The Case Study
3.1. Methods
3.2. Expert Selection
3.3. The Delphi Process
3.3.1. Stage One
3.3.2. Stage Two
3.3.3. Stage Three to Five
4. Results
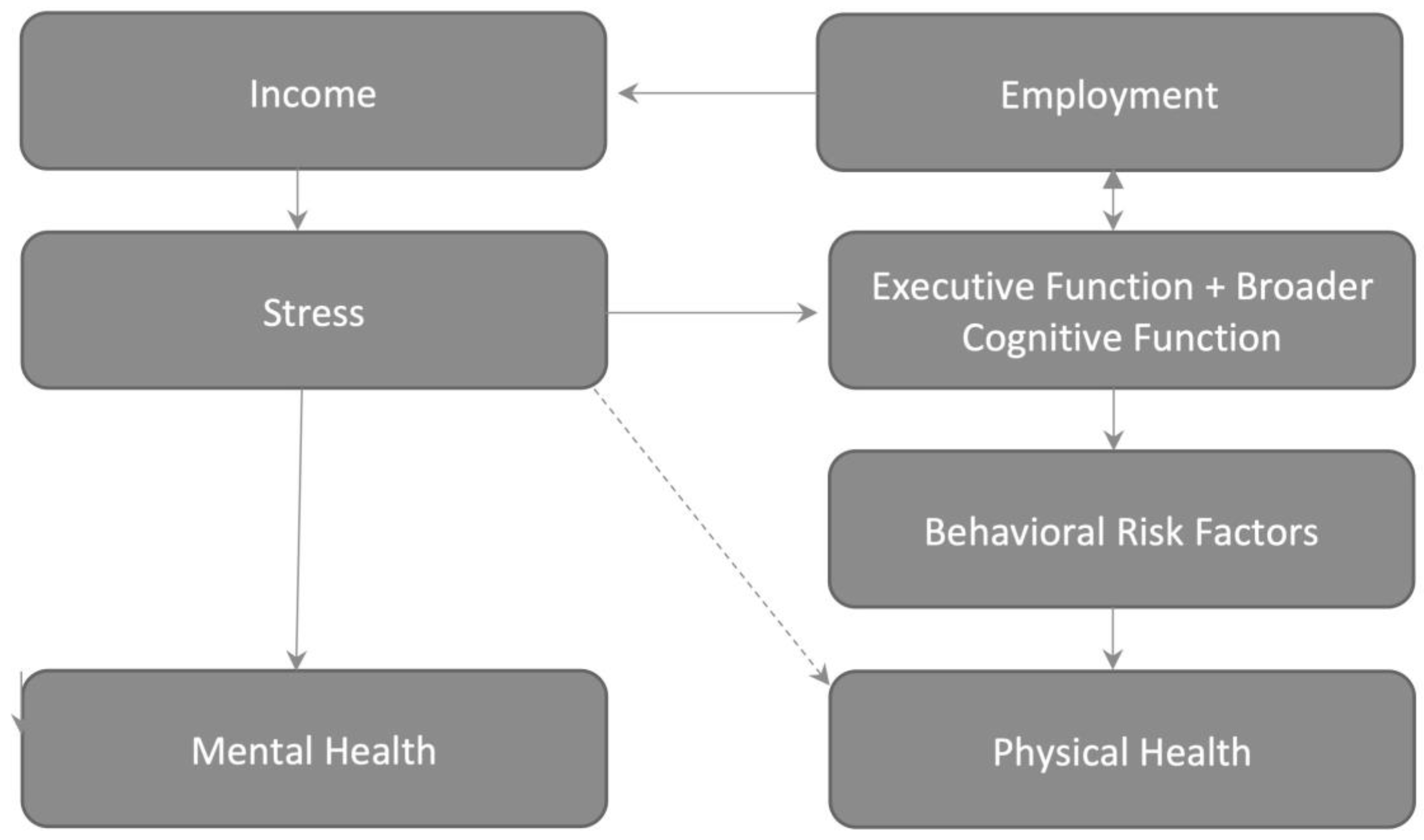
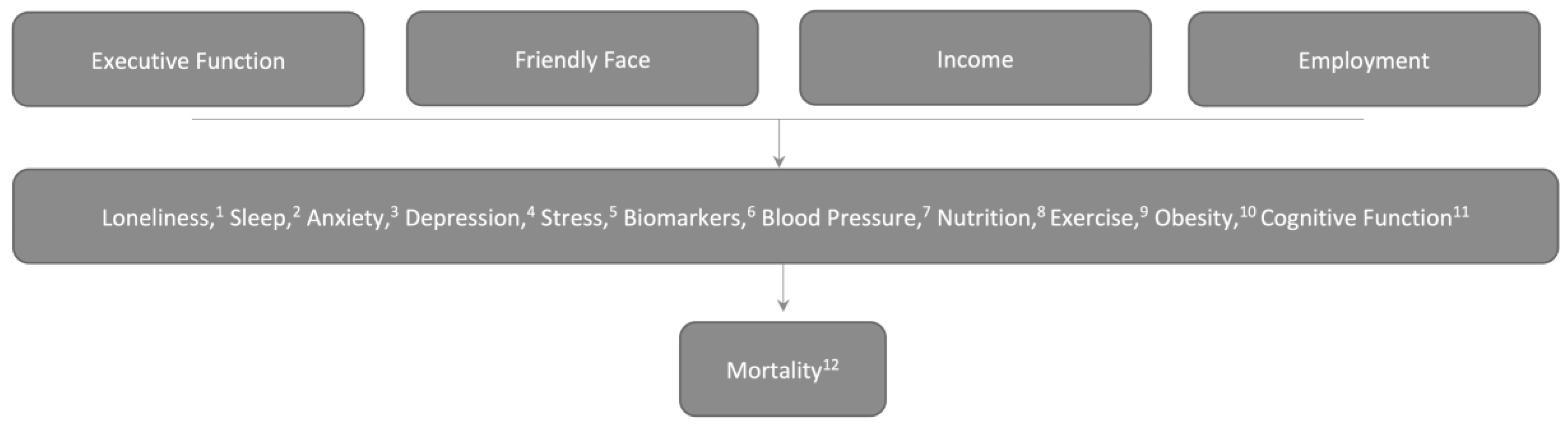
4.1. Round One: Presentation of the Model and Initial Thoughts
4.2. Round Two: Face-to-Face Meeting and Iterative Critique
4.3. Rounds Three to Five
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Tountas, Y. The historical origins of the basic concepts of health promotion and education: The role of ancient Greek philosophy and medicine. Health Promot. Int. 2009, 24, 185–192. [Google Scholar] [CrossRef] [PubMed]
- Virchow, R. Notes on the typhoid epidemic prevailing in Upper Silesia. Arch Pathol. Anat. Physiol. Klin. Med. 1849, 2, 143–322. [Google Scholar] [CrossRef]
- WHO Commission on Social Determinants of Health; World Health Organization. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health: Commission on Social Determinants of Health Final Report; World Health Organization: Geneva, Switzerland, 2008; Available online: https://apps.who.int/iris/bitstream/handle/10665/43943/9789241563703_eng.pdf;jsess (accessed on 16 April 2020).
- Gray, A.M. Inequalities in health. The Black Report: A summary and comment. Int. J. Health Serv. 1982, 12, 349–380. [Google Scholar] [CrossRef] [PubMed]
- Waitzkin, H.; Modell, H. Medicine, socialism, and totalitarianism: Lessons from Chile. N. Engl. J. Med. 1974, 291, 171–177. [Google Scholar] [CrossRef] [PubMed]
- New York State Department of Health. The Delivery System Reform Incentive Payment (DSRIP) Program. Available online: https://www.health.ny.gov/health_care/medicaid/redesign/dsrip/ (accessed on 18 May 2018).
- Kassler, W.J.; Tomoyasu, N.; Conway, P.H. Beyond a traditional payer—CMS’s role in improving population health. N. Engl. J. Med. 2015, 372, 109–111. [Google Scholar] [CrossRef] [PubMed]
- Woolf, S.H.; Aron, L. US Health in International Perspective: Shorter Lives, Poorer Health; National Academies Press: Washington, DC, USA, 2013. [Google Scholar]
- Muennig, P.; Franks, P.; Jia, H.; Lubetkin, E.; Gold, M.R. The income-associated burden of disease in the United States. Soc. Sci. Med. 2005, 61, 2018–2026. [Google Scholar] [CrossRef] [PubMed]
- Haskins, R.; Margolis, G. Show Me the Evidence: Obama’s Fight for Rigor and Results in Social Policy; Brookings Institution Press: Washington, DC, USA, 2014. [Google Scholar]
- Kawachi, I.; Adler, N.E.; Dow, W.H. Money, schooling, and health: Mechanisms and causal evidence. Ann. N. Y. Acad. Sci. 2010, 1186, 56–68. [Google Scholar] [CrossRef] [PubMed]
- Wachter, K.; National Research Council; Commission on Behavioral and Social Sciences and Education. Biosocial opportunities for surveys. In Cells and Surveys: Should Biological Measures Be Included in Social Science Research? Committee on Population, Finch, C.E., Vaupel, J., Kinsella, K., Eds.; National Academy Press: Washington, DC, USA, 2001; pp. 329–336. [Google Scholar]
- Courtin, E.; Kim, S.; Song, S.; Yu, W.; Muennig, P. Can social policies improve health? A systematic review and meta-analysis of 38 randomized trials. Milbank Q. 2020. [Google Scholar] [CrossRef]
- Ludwig, J.; Duncan, G.J.; Gennetian, L.A.; Katz, L.F.; Kessler, R.C.; Kling, J.R.; Sanbonmatsu, L. Neighborhood effects on the long-term well-being of low-income adults. Science 2012, 337, 1505–1510. [Google Scholar] [CrossRef]
- Campbell, F.; Conti, G.; Heckman, J.J.; Moon, S.H.; Pinto, R.; Pungello, E.; Pan, Y. Early childhood investments substantially boost adult health. Science 2014, 343, 1478–1485. [Google Scholar] [CrossRef]
- Baicker, K.; Taubman, S.L.; Allen, H.L.; Bernstein, M.; Gruber, J.H.; Newhouse, J.P.; Schneider, E.C.; Wright, B.J.; Zaslavsky, A.M.; Finkelstein, A.N. The Oregon Experiment—Effects of Medicaid on Clinical Outcomes. N. Engl. J. Med. 2013, 368, 1713–1722. [Google Scholar] [CrossRef] [PubMed]
- Weir, D. Elastic powers: The integration of biomarkers into the Health and Retirement Study. In Biosocial Surveys; National Academies Press (US): Washington, DC, USA, 2008. [Google Scholar]
- Adler, N.E.; Stewart, J. Health disparities across the lifespan: Meaning, methods, and mechanisms. Ann. N. Y. Acad. Sci. 2010, 1186, 5–23. [Google Scholar] [CrossRef] [PubMed]
- Muennig, P. Health selection vs. causation in the income gradient: What can we learn from graphical trends? J. Health Care Poor Underserved 2008, 19, 574–579. [Google Scholar] [CrossRef] [PubMed]
- Muennig, P.; Johnson, G.; Wilde, E.T. The effect of small class sizes on mortality through age 29 years: Evidence from a multicenter randomized controlled trial. Am. J. Epidemiol. 2011, 173, 1468–1474. [Google Scholar] [CrossRef] [PubMed]
- Justice, J.N.; Ferrucci, L.; Newman, A.B.; Aroda, V.R.; Bahnson, J.L.; Divers, J.; Espeland, M.A.; Marcovina, S.; Pollak, M.N.; Kritchevsky, S.B. A framework for selection of blood-based biomarkers for geroscience-guided clinical trials: Report from the TAME Biomarkers Workgroup. Geroscience 2018, 40, 419–436. [Google Scholar] [CrossRef] [PubMed]
- Seeman, T.E.; McEwen, B.S.; Rowe, J.W.; Singer, B.H. Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc. Natl. Acad. Sci. USA 2001, 98, 4770–4775. [Google Scholar] [CrossRef]
- Adler, N.E.; Marmot, M.G.; McEwen, B.; Stewart, J. Socioeconomic status and health in industrial nations: Social, psychological and biological pathways. Ann. N. Y. Acad. Sci. 1999, 896. Available online: https://psycnet.apa.org/record/2000-07137-000 (accessed on 26 April 2020).
- Guyer, H.; Ofstedal, M.; Lessof, C.; Cox, K. The Benefits and Challenges of Collecting Physical Measures and Biomarkers in Cross-National Studies. Available online: https://hrs.isr.umich.edu/sites/default/files/biblio/Collecting%20PM-Bio%20Data_DocumentationReport.pdf (accessed on 8 November 2019).
- Measures of Stress in the Health and Retirement Survey (HRS) and the HRS Family of Studies. Available online: https://stresscenter.ucsf.edu/sites/stresscenter.ucsf.edu/files/Stress%20Measurement%20in%20the%20HRS%20Family%20of%20Studies%20Guide.11-17-17_website%20post.pdf (accessed on 8 November 2019).
- McEwen, B.S. Protective and damaging effects of stress mediators. N. Engl. J. Med. 1998, 338, 171–179. [Google Scholar] [CrossRef]
- Linstone, H.A.; Turoff, M. Delphi Method: Techniques and Applications. 1975. Available online: http://is.njit.edu/pubs/delphibook/ (accessed on 11 March 2009).
- Baker, J.; Lovell, K.; Harris, N. How expert are the experts? An exploration of the concept of ‘expert’ within Delphi panel techniques. Nurse Res. 2006, 14, 59–70. [Google Scholar] [CrossRef]
- MDRC. MyGoals for Employment Success. Available online: https://www.mdrc.org/project/mygoals-employment-success (accessed on 18 May 2018).
- Guare, R.; Dawson, P.; Guare, C. A Manual for Executive Skills Coaching with Adults Affected by Conditions of Poverty and Stress; TauPath, LCC: Fort Collins, CO, USA, 2017. [Google Scholar]
- Hackman, D.A.; Gallop, R.; Evans, G.W.; Farah, M.J. Socioeconomic status and executive function: Developmental trajectories and mediation. Dev. Sci. 2015, 18, 686–702. [Google Scholar] [CrossRef]
- Wolf, T.J. Participation in work: The necessity of addressing executive function deficits. Work 2010, 36, 459–463. [Google Scholar] [CrossRef] [PubMed]
- Hall, P.A.; Fong, G.T.; Epp, L.J.; Elias, L.J. Executive function moderates the intention-behavior link for physical activity and dietary behavior. Psychol. Health 2008, 23, 309–326. [Google Scholar] [CrossRef] [PubMed]
- Anonymized personal communication, 19 September 2019.
- Cohen, S.; Doyle, W.J.; Baum, A. Socioeconomic status is associated with stress hormones. Psychosom. Med. 2006, 68, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Orpana, H.M.; Lemyre, L.; Gravel, R. Income and psychological distress: The role of the social environment. Health Rep. 2009, 20, 21. [Google Scholar] [PubMed]
- Gruenewald, T.L.; Karlamangla, A.S.; Hu, P.; Stein-Merkin, S.; Crandall, C.; Koretz, B.; Seeman, T.E. History of socioeconomic disadvantage and allostatic load in later life. Soc. Sci. Med. 2012, 74, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Seeman, T.; Epel, E.; Gruenewald, T.; Karlamangla, A.; McEwen, B.S. Socio-economic differentials in peripheral biology: Cumulative allostatic load. Ann. N. Y. Acad. Sci. 2010, 1186, 223–239. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muennig, P.; McEwen, B.; Belsky, D.W.; Noble, K.G.; Riccio, J.; Manly, J. Determining the Optimal Outcome Measures for Studying the Social Determinants of Health. Int. J. Environ. Res. Public Health 2020, 17, 3028. https://doi.org/10.3390/ijerph17093028
Muennig P, McEwen B, Belsky DW, Noble KG, Riccio J, Manly J. Determining the Optimal Outcome Measures for Studying the Social Determinants of Health. International Journal of Environmental Research and Public Health. 2020; 17(9):3028. https://doi.org/10.3390/ijerph17093028
Chicago/Turabian StyleMuennig, Peter, Bruce McEwen, Daniel W. Belsky, Kimberly G. Noble, James Riccio, and Jennifer Manly. 2020. "Determining the Optimal Outcome Measures for Studying the Social Determinants of Health" International Journal of Environmental Research and Public Health 17, no. 9: 3028. https://doi.org/10.3390/ijerph17093028
APA StyleMuennig, P., McEwen, B., Belsky, D. W., Noble, K. G., Riccio, J., & Manly, J. (2020). Determining the Optimal Outcome Measures for Studying the Social Determinants of Health. International Journal of Environmental Research and Public Health, 17(9), 3028. https://doi.org/10.3390/ijerph17093028




