Analyzing the Job Demands-Control-Support Model in Work-Life Balance: A Study among Nurses in the European Context
Abstract
1. Introduction
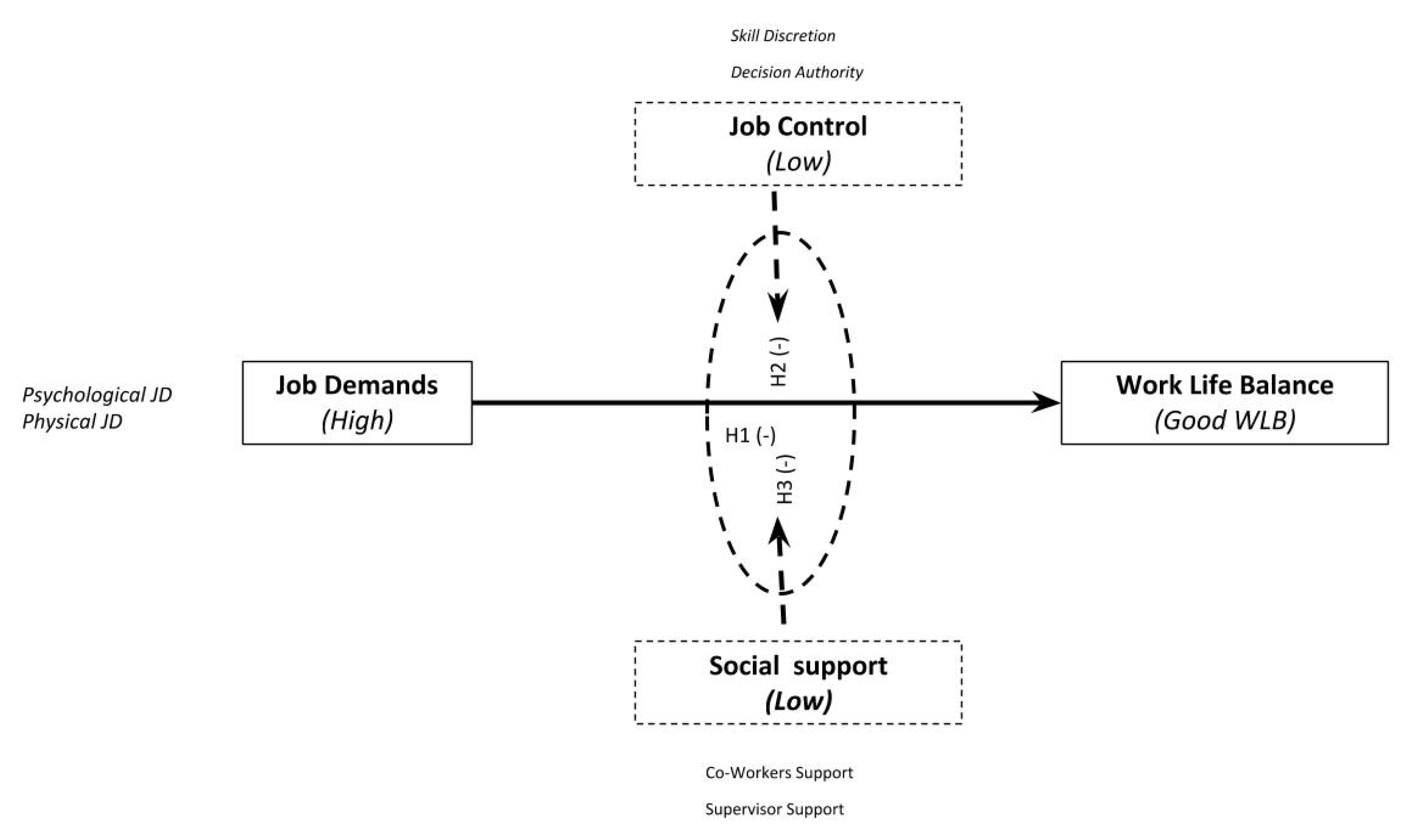
2. Managing Demands, Control and Support in an Organizational Context in Nursing
3. Research Hypotheses
4. Methodology
4.1. Data Collection and Sampling
4.2. Measures and Methodology: The Binary Logistic Regression Model
5. Results
5.1. Job Demand−Control−Support Factors and Work-Life Balance
5.2. Strain Model
5.3. Iso-Strain Model
6. Discussion
7. Conclusions and Limitations
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Babatunde, A.; Mordi, C.; Simpson, R.; Adisa, T.; Oruh, E. Time Biases: Exploring the Work-Life Balance of Single Nigeria Managers and Professionals. J. Manag. Psychol. 2019, 35, 35–70. [Google Scholar] [CrossRef]
- Lee, D.J.; Sirgy, M.J. Work-Life Balance in the Digital Workplace: The Impact of Schedule Flexibility and Telecommuting on Work-Life Balance and Overall Life Satisfaction. Thriving Digit. Work. 2019, 355–384. [Google Scholar] [CrossRef]
- Kowitlawkul, Y.; Yap, S.F.; Makabe, S.; Chan, S.; Takagai, J.; Tam, W.W.S.; Nurumal, M.S. Investigating nurses’ quality of life and work-life balance statuses in Singapore. Int. Nurs. Rev. 2019, 66, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Casper, W.J.; Vaziri, H.; Wayne, J.H.; DeHauw, S.; Greenhaus, J. The jingle-jangle of work–nonwork balance: A comprehensive and meta-analytic review of its meaning and measurement. J. Appl. Psychol. 2018, 103, 182. [Google Scholar] [CrossRef] [PubMed]
- Duxbury, L.E.; Higgins, C.A. Gender differences in work-family conflict. J. Appl. Psychol. 1991, 76, 60. [Google Scholar] [CrossRef]
- Williams, L.J.; Bozdogan, H.; Aiman-Smith, L. Inference problems with equivalent models. In Advanced Structural Equation Modeling: Issues and Techniques; Erlbaum: Mahwah, NJ, USA, 1996; pp. 279–314. [Google Scholar]
- Ozer, E.M. The impact of childcare responsibility and self-efficacy on the psychological health of professional working mothers. Psychol. Women Q. 1995, 19, 315–355. [Google Scholar] [CrossRef]
- Crompton, R.; Lyonette, C. Work-life ‘balance’ in Europe. Acta Sociol. 2006, 49, 379–393. [Google Scholar] [CrossRef]
- Parent-Thirion, A.; Fernandez Macias, E.; Hurley, J.; Vermeylen, G. Fourth European Working Conditions Survey; European Foundation for the Improvement of Living and Working Conditions: Dublin, Ireland, 2007.
- Lee, J.M.; Choi, H.G. Influence of organizational culture supporting work-life balance on well-being and depression mediated by work-life balance. Korean J. Ind. Organ. Psychol. 2019, 32, 1–27. [Google Scholar] [CrossRef][Green Version]
- Niessen, C.; Müller, T.; Hommelhoff, S.; Westman, M. The impact of preventive coping on business travelers’ work and private life. J. Organ. Behav. 2018, 39, 113–127. [Google Scholar] [CrossRef]
- Rodríguez González, S. Desigualdad por causa de género en la Seguridad Social: Carreras de cotización y prestaciones. Lan Harremanak. Rev. Relac. Laborales 2017, 38, 93–125. [Google Scholar]
- Cramer, E.; Hunter, B. Relationships between working conditions and emotional wellbeing in midwives. Women Birth. 2019, 32, 521–532. [Google Scholar] [CrossRef] [PubMed]
- Hayes, B.; Prihodova, L.; Walsh, G.; Doyle, F.; Doherty, S. Doctors don’t Do-little: A national cross-sectional study of workplace well-being of hospital doctors in Ireland. BMJ Open 2019, 9, e025433. [Google Scholar] [CrossRef] [PubMed]
- Nielsen, M.B.; Einarsen, S.V. What we know, what we do not know, and what we should and could have known about workplace bullying: An overview of the literature and agenda for future research. Aggress. Violent Behav. 2018, 42, 71–83. [Google Scholar] [CrossRef]
- Karasek, R. Job demands, job decision latitude, and mental strain: Implications for job redesign. Adm. Sci. Q. 1979, 24, 285–308. [Google Scholar] [CrossRef]
- Karasek, R. Healthy Work: Stress, Productivity, and the Reconstruction of Working Life; Basic Books: New York, NY, USA, 1990. [Google Scholar]
- Johnson, V.J.; Hall, E.M. Job strain, work place social support, and cardiovascular disease: A cross-sectional study of a random sample of the Swedish working population. Am. J. Public Heal. 1988, 78, 1336–1342. [Google Scholar] [CrossRef]
- Salin, D. Risk factors of workplace bullying for men and women: The role of the psychosocial and physical work environment. Scand. J. Psychol. 2015, 56, 69–77. [Google Scholar] [CrossRef]
- Ariza-Montes, A.; Arjona-Fuentes, J.M.; Han, H.; Law, R. Work environment and well-being of different occupational groups in hospitality: Job Demand–Control–Support model. Int. J. Hosp. Manag. 2018, 73, 1–11. [Google Scholar] [CrossRef]
- Asif, F.; Javed, U.; Janjua, S.Y. The job demand-control-support model and employee wellbeing: A meta-analysis of previous research. Pak. J. Psychol. Res. 2018, 33, 1. [Google Scholar]
- Mivšek, P.; Äimälä, A.M.; Žvanut, B.; Tuomi, J. Midwifery students’ well-being among undegraduates in Slovenia: A pilot study. Midwifery 2018, 61, 63–65. [Google Scholar] [CrossRef]
- Rong, Y.; Guo, K.R.; Yin, H.F.; Wu, Y.F.; Li, S.; Sun, D.Y. Evaluating the level of occupational stress and its influence factors among traffic police in a district in Shanghai. Chin. J. Ind. Hyg. Occup. Dis. 2019, 37, 352–356. [Google Scholar] [CrossRef]
- Schernhammer, E.S.; Feskanich, D.; Liang, G.; Scott, A.J.; Singh, R.B.; Anjum, B.; Takahashi, M. Stress and Burnout in Doctors. Camb. Handb. Psychol. Health Med. 2019, 27, 361. [Google Scholar]
- Schilling, R.; Colledge, F.; Ludyga, S.; Pühse, U.; Brand, S.; Gerber, M. Does cardiorespiratory fitness moderate the association between occupational stress, cardiovascular risk, and mental health in police officers? Int. J. Environ. Res. Public Health 2019, 16, 2349. [Google Scholar] [CrossRef] [PubMed]
- Chambel, M.J.; Carvalho, V.S.; Cesário, F.; Lopes, S. The Work-to-Life Conflict Mediation between Job Characteristics and Well-Being at Work, Career Development International; Emerald Publishing Limited: Bingley, UK, 2017. [Google Scholar]
- Ibrahim, R.Z.A.R.; Saputra, J.; Bakar, A.A.; Dagang, M.M.; Nazilah, S.; Ali, M.; Yasin, M.A.S.M. Role of Supply Chain Management on the Job Control and Social Support for Relationship between Work-Family Conflict and Job Satisfaction. Int. J. Sup. Chain 2019, 8, 907. [Google Scholar]
- Goller, M.; Harteis, C.; Gijbels, D.; Donche, V. Engineering students’ learning during internships: Exploring the explanatory power of the job demands-control-support model. J. Eng. Educ. 2020, 1–18. [Google Scholar] [CrossRef]
- Ogunyemi, A.O.; Babalola, S.O.; Akanbi, S.O. Job Demands and Mental Strain Relationship: The Moderating Effect of Perceived Organizational Support on the Mediating Role of Job Decision Latitude among Nigerian Immigration Officers. KIU J. Soc. Sci. 2019, 5, 141–150. [Google Scholar]
- Rana, F.A.; Javed, U. Psychosocial job characteristics, employee well-being, and quit intentions in Pakistan’s insurance sector. Glob. Bus. Organ. Excel. 2019, 38, 38–45. [Google Scholar] [CrossRef]
- Vassos, M.; Nankervis, K.; Skerry, T.; Lante, K. Can the job demand-control-(support) model predict disability support worker burnout and work engagement? J. Intellect. Dev. Disabil. 2019, 44, 139–149. [Google Scholar] [CrossRef]
- Park, H.; Oh, H.; Boo, S. The Role of Occupational Stress in the Association between Emotional Labor and Mental Health: A Moderated Mediation Model. Sustainability 2019, 11, 1886. [Google Scholar] [CrossRef]
- Schmitt, H. Job Demands, Job Control, and Social Support on Burnout: Why Type Matters. Ph.D. Thesis, Alliant International University, Alhambra, CA, USA, 2019. [Google Scholar]
- Ding, G.; Liu, H.; Huang, Q.J. Enterprise social networking usage as a moderator of the relationship between work stressors and employee creativity: A multilevel study. Inf. Manag. 2019, 56, 103165. [Google Scholar] [CrossRef]
- Grzywacz, J.G.; Frone, M.J.; Brewer, C.S.; Kovner, C.T. Quantifying work–family conflict among registered nurses. Res. Nurs. Heal. 2006, 29, 414–426. [Google Scholar] [CrossRef]
- Cortese, C.G.; Ghislieri, C.; Colombo, L. Determinants of nurses’ job satisfaction: The role of work–family conflict, job demand, emotional charge and social support. J. Nurs. Manag. 2010, 18, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Russo, M.; Buonocore, F. The relationship between work–family enrichment and nurse turnover. J. Manag. Psychol. 2012, 27, 216–236. [Google Scholar] [CrossRef]
- Tummers, L.G.; Den Dulk, L. The effects of work alienation on organisational commitment, work effort and work-to-family enrichment. J. Nurs. Manag. 2013, 21, 850–859. [Google Scholar] [CrossRef]
- Lecca, L.I.; Finstad, G.L.; Traversini, V.; Lulli, L.G.; Gualco, B.; Taddei, G. The Role of Job Support as a Target for the Management of Work-Related Stress: The State of Art. Qual. Access Success 2020, 21, 174. [Google Scholar]
- Liu, Y.; Zhang, J.; Hennessy, D.A.; Zhao, S.; Ji, H. Psychological strains, depressive symptoms, and suicidal ideation among medical and non-medical staff in urban china. J. Affect. Disord. 2019, 245, 22–27. [Google Scholar] [CrossRef] [PubMed]
- Henson, J.S. The Effectiveness of a Robotic Seal on Compassion Satisfaction in Acute Care Nurses: A Mixed Methods Approach. Ph.D. Thesis, The University of Texas at Tyler, Tyler, TX, USA, 2019. [Google Scholar]
- Papastavrou, E.; Andreou, P.; Tsangari, H.; Schubert, M.; De Geest, S. Rationing of nursing care within professional environmental constraints: A correlational study. Clin. Nurs. Res. 2014, 23, 314–335. [Google Scholar] [CrossRef] [PubMed]
- Schwarzer, R.; Knoll, N. Functional roles of social support within the stress and coping process: A theoretical and empirical overview. Clin. Nurs. Res. 2007, 42, 243–252. [Google Scholar] [CrossRef]
- McGinnity, F.; Russell, H.; Watson, D.; Kingston, G.; Kelly, E. Winners and Losers? The Equality Impact of the Great Recession in Ireland; Economic and Social Research Institute (ESRI): Redlands, CA, USA, 2014; ISBN 978-1-908275-67-7. [Google Scholar]
- Lahana, E.; Tsaras, K.; Kalaitzidou, A.; Galanis, P.; Kaitelidou, D.; Sarafis, P. Conflicts management in public sector nursing. Int. J. Health Manag. 2019, 12, 33–39. [Google Scholar] [CrossRef]
- Russo, M.; Shteigman, A.; Carmeli, A. Workplace and family support and work–life balance: Implications for individual psychological availability and energy at work. J. Posit. Psychol. 2016, 11, 173–188. [Google Scholar] [CrossRef]
- Haar, J.M.A.; Sune, A.; Russo, M.; Ollier-Malaterre, A. A cross-national study on the antecedents of work–life balance from the fit and balance perspective. Soc. Indic. Res. 2019, 142, 261–282. [Google Scholar] [CrossRef]
- Cheng, S.Y.; Lin, P.C.; Chang, Y.K.; Lin, Y.K.; Lee, P.H.; Chen, S.R. Sleep quality mediates the relationship between work–family conflicts and the self-perceived health status among hospital nurses. J. Nurs. Manag. 2019, 27, 381–387. [Google Scholar] [CrossRef] [PubMed]
- Neeson, J. Nurses are human beings too. Nurs. Stand. 2017, 31, 32. [Google Scholar] [CrossRef] [PubMed]
- Lu, H.; Zhao, Y.; While, A. Job satisfaction among hospital nurses: A literature review. Int. J. Nurs. Stud. 2019, 94, 21–31. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Statistics: Monitoring Health for the SDGs Sustainable Development Goals; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Lemieux-Cumberlege, A.; Taylor, E.P. An exploratory study on the factors affecting the mental health and well-being of frontline workers in homeless services. Health Soc. Care Community 2019, 27, e367–e378. [Google Scholar] [CrossRef]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef]
- Barnett, M.D.; Martin, K.J.; Garza, C.J. Satisfaction with work–family balance mediates the relationship between workplace social support and depression among hospice nurses. J. Nurs. Sch. 2019, 51, 187–194. [Google Scholar] [CrossRef]
- Griffith, R. The elements of negligence liability in nursing. Br. J. Nurs. 2020, 29, 176–177. [Google Scholar] [CrossRef]
- Harrod, M.; Petersen, L.; Weston, L.E.; Gregory, L.; Mayer, J.; Samore, M.H.; Drews, A.; Krein, S.L. Understanding workflow and personal protective equipment challenges across different healthcare personnel roles. Clin. Infect. Dis. 2019, 69, 185–191. [Google Scholar] [CrossRef]
- Bureau of Labor Statistics Nonfatal Occupational Injuries and Illnesses Requiring Days Away From Work. Industry Injury and Illness Data–2015; Bureau of Labor Statistics, US Department of Labor: Washington, DC, USA, 2015; pp. 1–28.
- Khan, S.A.; Waqas, M.; Siddiqui, M.; Ujjan, B.U.; Khan, M.; Bari, M.E.; Azeem, M.A. Work-life balance amongst residents in surgical and non-surgical specialties in a tertiary care hospital in Karachi. JPMA. J. Pak. Med. Assoc. 2020, 70, 252. [Google Scholar] [CrossRef]
- Daxini, S.; Mehta, N. A Study on Impact of Work Stress on Work-Life balance Among Full Time Women Faculties in Self Financing Courses in Mumbai Suburban. Adv. Innov. Res. 2019, 29, 130–139. [Google Scholar]
- Lin, Y.L.; Tomasi, J.; Guerguerian, A.M.; Trbovich, P. Technology-mediated macrocognition: Investigating how physicians, nurses, and respiratory therapists make critical decisions. J. Crit. Care 2019, 53, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Fukumori, T.; Miyazaki, A.; Takaba, C.; Taniguchi, S.; Asai, M. Traumatic Events Among Cancer Patients That Lead to Compassion Fatigue in Nurses: A Qualitative Study. J. Pain Symptom Manag. 2020, 59, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Hysong, S.J.; Amspoker, A.B.; Hughes, A.M.; Woodard, L.; Oswald, F.L.; Petersen, L.A.; Lester, H.F. Impact of team configuration and team stability on primary care quality. Implement. Sci. 2019, 14, 22. [Google Scholar] [CrossRef] [PubMed]
- Hussain, I.R.; Mujtaba, B.G. The relationship between work-life conflict and employee performance: A study of national database and registration authority workers in Pakistan. J. Knowl. Manag. Econ. Inf. Technol. 2012, 2, 1–11. [Google Scholar]
- Dobber, J.; Latour, C.; Snaterse, M.; van Meijel, B.; terRiet, G.; Scholte op Reimer, W.; Peters, R. Developing nurses’ skills in motivational interviewing to promote a healthy lifestyle in patients with coronary artery disease. Eur. J. Cardiovasc. Nurs. 2019, 18, 28–37. [Google Scholar] [CrossRef]
- Ulrich, B.; Barden, C.; Cassidy, L.; Varn-Davis, N. Frontline nurse manager and chief nurse executive skills: Perceptions of direct care nurses. Nurse Leader 2019, 17, 109–112. [Google Scholar] [CrossRef]
- Dello Russo, S.; Mascia, D.; &Morandi, F. Individual perceptions of HR practices, HRM strength and appropriateness of care: A meso, multilevel approach. Int. J. Hum. Resour. Manag. 2018, 29, 286–310. [Google Scholar] [CrossRef]
- Ronquillo, C.; Boschma, G.; Wong, S.T.; Quiney, L. Beyond greener pastures: Exploring contexts surrounding Filipino nurse migration in Canada through oral history. Nurs. Inq. 2011, 18, 262–275. [Google Scholar] [CrossRef]
- Labrague, L.J.; McEnroe-Petitte, D.M.; Tsaras, K. Predictors and outcomes of nurse professional autonomy: A cross-sectional study. Int. J. Nurs. Pr. 2019, 25, e12711. [Google Scholar] [CrossRef]
- Olmedo, G.R. Medicalización, psiquiatrización… żdespsiquiatrización? Con-Cienc. Soc. Anu. Didáctica Geogr. Hist. Cienc. Soc. 2009, 13, 17–40. [Google Scholar]
- Azizi, S.; Jafari, S.; Ebrahimian, A. Shortage of Men Nurses in the Hospitals in Iran and the World: A Narrative Review. Sci. J. Nurs. Midwifery Paramed. Fac. 2019, 5, 6–23. [Google Scholar]
- White, E.M.; Aiken, L.H.; Sloane, D.M.; McHugh, M.D. Nursing home work environment, care quality, registered nurse burnout and job dissatisfaction. Geriatr. Nurs. 2019, 52. [Google Scholar] [CrossRef] [PubMed]
- McGilton, K.S.; Tourangeau, A.; Kavcic, C.; Wodchis, W.P. Determinants of regulated nurses’ intention to stay in long-term care homes. J. Nurs. Manag. 2013, 21, 771–781. [Google Scholar] [CrossRef] [PubMed]
- Ropponen, A.; Koskinen, A.; Puttonen, S.; Härmä, M. Exposure to working-hour characteristics and short sickness absence in hospital workers: A case-crossover study using objective data. Int. J. Nurs. Stud. 2019, 91, 14–21. [Google Scholar] [CrossRef]
- Van Der Heijden, B.I.; Peeters, M.C.; Le Blanc, P.M.; Van Breukelen, J.W.M. Job characteristics and experience as predictors of occupational turnover intention and occupational turnover in the European nursing sector. J. Vocat. Behav. 2018, 108, 108–120. [Google Scholar] [CrossRef]
- De Jonge, J.; Mulder, M.J.; Nijhuis, F.J. The incorporation of different demand concepts in the job demand-control model: Effects on health care professionals. Soc. Sci. Med. 1999, 48, 1149–1160. [Google Scholar] [CrossRef]
- Scanlan, J.N.; Still, M. Relationships between burnout, turnover intention, job satisfaction, job demands and job resources for mental health personnel in an Australian mental health service. BMC Health Serv. Res. 2019, 19, 62. [Google Scholar] [CrossRef]
- Yamaguchi, Y.; Inoue, T.; Harada, H.; Oike, M. Job control, work-family balance and nurses’ intention to leave their profession and organization: A comparative cross-sectional survey. Int. J. Nurs. Stud. 2016, 64, 52–62. [Google Scholar] [CrossRef]
- Mark, G.; Smith, A.P. Occupational stress, job characteristics, coping, and the mental health of nurses. Br. J. Health Psychol. 2012, 17, 505–521. [Google Scholar] [CrossRef]
- Smith, J.H.; Sweet, L. Becoming a nurse preceptor, the challenges and rewards of novice registered nurses in high acuity hospital environments. Nurse Educ. Pr. 2019, 36, 101–107. [Google Scholar] [CrossRef]
- Sigurdardottir, A.O.; Svavarsdottir, E.K.; Juliusdottir, S. Family nursing hospital training and the outcome on job demands, control and support. Nurse Educ. Today 2015, 35, 854–858. [Google Scholar] [CrossRef] [PubMed]
- Chiu, Y.L.; Tsai, C.C.; Chiang, C.Y.F. The relationships among nurses’ job characteristics and attitudes toward web-based continuing learning. Nurse Educ. Today 2013, 33, 327–333. [Google Scholar] [CrossRef] [PubMed]
- Nabirye, R.C.; Brown, K.C.; Pryor, E.R.; Maples, E.H. Occupational stress, job satisfaction and job performance among hospital nurses in Kampala, Uganda. J. Nurs. Manag. 2011, 19, 760–768. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, P.; Carragher, L.; Carragher, N.; Treacy, J. Development and validation of an instrument to measure stress among older adult nursing students: The Student Nurse Stressor-15 (SNS-15) Scale. J. Clin. Nurs. 2019, 28, 1336–1345. [Google Scholar] [CrossRef]
- Kelly, L.A.; Lefton, C.; Fischer, S.A. Nurse Leader Burnout, Satisfaction, and Work-Life Balance. JONA: J. Nurs. Adm. 2019, 49, 404–410. [Google Scholar] [CrossRef]
- Xanthopoulou, D.; Bakker, A.B.; Demerouti, E.; Schaufeli, W.B. Work engagement and financial returns: A diary study on the role of job and personal resources. J. Occup. Organ. Psychol. 2009, 82, 183–200. [Google Scholar] [CrossRef]
- McVicar, A. Scoping the common antecedents of job stress and job satisfaction for nurses (2000–2013) using the job demands–resources model of stress. J. Nurs. Manag. 2016, 24, E112–E136. [Google Scholar] [CrossRef]
- Hochwälder, J. The psychosocial work environment and burnout among Swedish registered and assistant nurses: The main, mediating, and moderating role of empowerment. Nurs. Health Sci. 2007, 9, 205–211. [Google Scholar] [CrossRef]
- Sundin, L.; Hochwälder, J.; Bildt, C.; Lisspers, J. The relationship between different work-related sources of social support and burnout among registered and assistant nurses in Sweden: A questionnaire survey. Int. J. Nurs. Stud. 2007, 44, 758–769. [Google Scholar] [CrossRef]
- Rugulies, R.; Aust, B.; &Pejtersen, J.H. Do psychosocial work environment factors measured with scales from the Copenhagen Psychosocial Questionnaire predict register-based sickness absence of 3 weeks or more in Denmark? Scand. J. Public Health 2010, 38, 42–50. [Google Scholar] [CrossRef]
- Widerszal-Bazyl, M. Copenhagen psychosocial questionnaire (copsoq). Medycynapracy 2017, 68, 329–349. [Google Scholar]
- Van Smeden, M.; Moons, K.G.; de Groot, J.A.; Collins, G.S.; Altman, D.G.; Eijkemans, M.J.; Reitsma, J.B. Sample size for binary logistic prediction models: Beyond events per variable criteria. Stat. Methods Med Res. 2019, 28, 2455–2474. [Google Scholar] [CrossRef] [PubMed]
- Debray, T.P.; Damen, J.A.; Riley, R.D.; Snell, K.; Reitsma, J.B.; Hooft, L.; Collins, G.; Moons, K.G. A framework for meta-analysis of prediction model studies with binary and time-to-event outcomes. Stat. Methods Med Res. 2019, 28, 2768–2786. [Google Scholar] [CrossRef] [PubMed]
- Birolim, M.M.; Mesas, A.E.; González, A.D.; Santos, H.G.D.; Haddad, M.D.C.F.L.; Andrade, S.M.D. Job strain among teachers: Associations with occupational factors according to social support. Cienc. Saudecoletiva 2019, 24, 1255–1264. [Google Scholar] [CrossRef]
- Tam, J.Z.; Mohamed, Z.; Puteh, S.E.W.; Ismail, N.H. A systematic review on identifying associated factors in deciding work-relatedness of chronic back pain among employee. Malays. J. Public Health Med. 2019, 19, 1–14. [Google Scholar]
- Nguyen Ngoc, A.; Le ThiThanh, X.; Le Thi, H.; Vu Tuan, A.; Nguyen Van, T. Occupational Stress Among Health Worker in a National Dermatology Hospital in Vietnam, 2018. Frontiers in Psychiatry. 2020, 10, 950. [Google Scholar] [CrossRef]
- Wesołowska, K.; Elovainio, M.; Gluschkoff, K.; Hietapakka, L.; Kaihlanen, A.M.; Lehtoaro, S.; Heponiemi, T. Psychosocial work environment and cross-cultural competence among native and foreign-born registered nurses. Res. Nurs. Health 2019, 42, 349–357. [Google Scholar] [CrossRef]
- BagheriHosseinabadi, M.; Ebrahimi, M.H.; Khanjani, N.; Biganeh, J.; Mohammadi, S.; Abdolahfard, M. The effects of amplitude and stability of circadian rhythm and occupational stress on burnout syndrome and job dissatisfaction among irregular shift working nurses. J. Clin. Nurs. 2019, 28, 1868–1878. [Google Scholar] [CrossRef]
- Arnetz, J.; Sudan, S.; Goetz, C.; Counts, S.; Arnetz, B. Nurse work environment and stress biomarkers: Possible implications for patient outcomes. J. Occup. Environ. Med. 2019, 61, 676–681. [Google Scholar] [CrossRef]
- Karatepe, O.M.; Uludag, O. Conflict, exhaustion, and motivation: A study of frontline employees in Northern Cyprus hotels. Int. J. Hosp. Manag. 2007, 26, 645–665. [Google Scholar] [CrossRef]
- Ghislieri, C.; Gatti, P.; Molino, M.; Cortese, C.G. Work–family conflict and enrichment in nurses: Between job demands, perceived organisational support and work–family backlash. J. Nurs. Manag. 2017, 25, 65–75. [Google Scholar] [CrossRef] [PubMed]
- Voydanoff, P. The effects of work demands and resources on work-to-family conflict and facilitation. J. Nurs. Manag. 2004, 66, 398–412. [Google Scholar] [CrossRef]
- Hussain, A.; Rivers, P.A.; Glover, S.H.; Fottler, M.D. Strategies for dealing with future shortages in the nursing workforce: A review. Health Serv. Manag. Res. 2012, 25, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Mc Carthy, V.J.; Wills, T.; Crowley, S. Nurses, age, job demands and physical activity at work and at leisure: A cross-sectional study. Appl. Nurs. Res. 2018, 40, 116–121. [Google Scholar] [CrossRef]
- Nam, S.; Lee, S.J. Occupational factors associated with obesity and leisure-time physical activity among nurses: A cross sectional study. Int. J. Nurs. Stud. 2016, 57, 60–69. [Google Scholar] [CrossRef]
- Qureshi, M.A.; Ab Hamid, K.B.; Jeihoony, P.; Ali, R.; Brohi, N.A.; Magsi, R.; Shah, S.M.M. Is Supervisor Support Matter in Job Satisfaction? A Moderating Role of Fairness Perception among Nurses in Pakistan. Acad. Strateg. Manag. J. 2018, 17, 1–10. [Google Scholar]
- Greenglass, E.R.; Burke, R.J.; Fiksenbaum, L. Workload and burnout in nurses. J. Community Appl. Soc. Psychol. 2001, 11, 211–215. [Google Scholar] [CrossRef]
- Garrett, D.K.; McDaniel, A.M. A new look at nurse burnout: The effects of environmental uncertainty and social climate. JONA J. Nurs. Adm. 2001, 31, 91–96. [Google Scholar] [CrossRef]
- Haluza, D.; Schmidt, V.M.; Blasche, G. Time course of recovery after two successive night shifts: A diary study among Austrian nurses. J. Nurs. Manag. 2019, 27, 190–196. [Google Scholar] [CrossRef]
- Vedaa, Ø.; Harris, A.; Erevik, E.K.; Waage, S.; Bjorvatn, B.; Sivertsen, B.; Moen, B.E.; Pallesen, S. Short rest between shifts (quick returns) and night work is associated with work-related accidents. Int. Arch. Occup. Environ. Health 2019, 92, 829–835. [Google Scholar] [CrossRef]
- Mahendran, A.V.; Panatik, S.A.; Rajab, A.; Nordin, N. The Influence of Work-life Balance on Burnout among Nurses. Indian, J. Public Health Res. Dev. 2019, 10, 3338. [Google Scholar] [CrossRef]
- Bae, J.; Jennings-McGarity, P.; Hardeman, C.P.; Kim, E.; Lee, M.; Littleton, T.; Saasa, S. Compassion Satisfaction Among Social Work Practitioners: The Role of Work–Life Balance. J. Soc. Serv. Res. 2019, 1–11. [Google Scholar] [CrossRef]
- Pisarski, A.; Brook, C.; Bohle, P.; Gallois, C.; Watson, B.; Winch, S. Extending a model of shift-work tolerance. Chronobiol. Int. 2006, 23, 1363–1377. [Google Scholar] [CrossRef] [PubMed]
- Chunta, K.S. New Nurse Leaders: Creating a Work-Life Balance and Finding Joy in Work. J. Radiol. Nurs. 2020. [Google Scholar] [CrossRef]
- Dousin, O.; Collins, N.; Kaur Kler, B. Work-Life Balance, Employee Job Performance and Satisfaction Among Doctors and Nurses in Malaysia. Int. J. Hum. Resour. Stud. 2019, 9, 306–319. [Google Scholar] [CrossRef]
- Fuentes, R. Implementing a Self-Scheduling Model to Decrease Nurse Turnover in Medical-Surgical Nursing. Ph.D. Thesis, Walden University, Minneapolis, MI, USA, 2019. [Google Scholar]
- Ahmed, J.; Saleem, N.; Fatima, K. Factors Influencing Work Life Balance of Women Entrepreneurs: A Case of Quetta (Pakistan). Dialogue 2019, 14, 93. [Google Scholar]
- Zaghini, F.; Fiorini, J.; Piredda, M.; Fida, R.; Sili, A. The relationship between nurse managers’ leadership style and patients’ perception of the quality of the care provided by nurses: Cross sectional survey. Int. J. Nurs. Stud. 2020, 101, 103446. [Google Scholar] [CrossRef]
- De Souza, B.; Ramsay, R. Medical Women’s Federation celebrates its long history. BMJ 2019, 336, 90. [Google Scholar] [CrossRef]
- Hirschman, A.O. Exit, Voice, and Loyalty: Responses to decline in Firms, Organizations, and States; Harvard University Press: Cambridge, MA, USA, 1970; Volume 25. [Google Scholar]
- Mushfiqur, R.; Mordi, C.; Oruh, E.S.; Nwagbara, U.; Mordi, T.; Turner, I.M. The impacts of work-life-balance (WLB) challenges on social sustainability: The experience of Nigerian female medical doctors. Empl. Relat. 2018, 40, 868–888. [Google Scholar] [CrossRef]
- Adisa, T.A.; Gbadamosi, G.; Osabutey, E.L. What happened to the border? The role of mobile information technology devices on employees’ work-life balance. Pers. Rev. 2017, 46, 1651–1671. [Google Scholar] [CrossRef]
- Abdul-Rashid, S.H.; Sakundarini, N.; Raja Ghazilla, R.A.; Thurasamy, R. The impact of sustainable manufacturing practices on sustainability performance: Empirical evidence from Malaysia. Int. J. Oper. Prod. Manag. 2017, 37, 182–204. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, M.Y. Factors affecting organizational commitment of general hospital nurses in small and medium sized cities. J. Korean Acad. Nurs. Adm. 2019, 25, 14–24. [Google Scholar] [CrossRef]
- Tabriz, A.A.; Birken, S.A.; Shea, C.M.; Fried, B.J.; Viccellio, P. What is full capacity protocol, and how is it implemented successfully? Implement. Sci. 2019, 14, 73. [Google Scholar] [CrossRef]
- Wallace, A.S.; Pierce, N.L.; Davisson, E.; Manges, K.; Tripp-Reimer, T. Social resource assessment: Application of a novel communication tool during hospital discharge. Patient Educ. Couns. 2019, 102, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Baris, V.K.; Seren Intepeler, S. Cross-cultural adaptation and psychometric evaluation of the Turkish version of the Self-Efficacy for Preventing Falls-Nurse. J. Nurs. Manag. 2019, 27, 1791–1800. [Google Scholar] [CrossRef] [PubMed]
- Tucker, M.K.; Jimmieson, N.L.; Bordia, P. Supervisor support as a double-edged sword: Supervisor emotion management accounts for the buffering and reverse-buffering effects of supervisor support. Int. J. Stress Manag. 2018, 25, 14. [Google Scholar] [CrossRef]
- Somers, M.J.; Birnbaum, D.; Casal, J. Supervisor support, control over work methods and employee well-being: New insights into nonlinearity from artificial neural networks. Int. J. Hum. Resour. Manag. 2018, 1–23. [Google Scholar] [CrossRef]
- Jennings, K.N. In the balance: Work/life balance of senior development professionals within higher education. Ph.D. Thesis, Iowa State University, Ames, IA, USA, 2007. [Google Scholar]
- Pelfrene, E.; Vlerick, P.; Kittel, F.; Mak, R.P.; Kornitzer, M.; Backer, G.D. Psychosocial work environment and psychological well-being: Assessment of the buffering effects in the job demand–control (–support) model in BELSTRESS. Stress Health 2002, 18, 43–56. [Google Scholar] [CrossRef]
| Variables in the Model | Odds Ratios | ||||||
|---|---|---|---|---|---|---|---|
| 95% C.I. for OR | |||||||
| Variables | B | Standard | Wald | p | OR | Lower | Upper |
| Job Demands | |||||||
| Psychological JD (high) | −0.520 | 0.151 | 11.863 | 0.001 | 0.594 | 0.442 | 0.799 |
| Physical JD (high) | −0.613 | 0.15 | 16.711 | 0.000 | 0.542 | 0.404 | 0.727 |
| Job Control | |||||||
| Skill discretion (low) | −0.087 | 0.148 | 0.348 | 0.555 | 0.917 | 0.686 | 1.224 |
| Decision authority (low) | −0.188 | 0.163 | 1.324 | 0.250 | 0.829 | 0.602 | 1.141 |
| Social Support | |||||||
| Co-worker support (low) | −0.257 | 0.228 | 1.271 | 0.260 | 0.773 | 0.494 | 1.209 |
| Supervisor support (low) | 0.412 | 0.306 | 1.811 | 0.178 | 0.662 | 0.364 | 1.207 |
| Variables in the Model | Odds Ratios | ||||||
|---|---|---|---|---|---|---|---|
| 95% C.I. for OR | |||||||
| Variables | B | Standard | Wald | p | OR | Lower | Upper |
| Job Demands | |||||||
| Psychological JD (high) | 0.025 | 0.321 | 0.006 | 0.937 | 1.026 | 0.546 | 1.926 |
| Physical JD (high) | −0.397 | 0.193 | 4.223 | 0.040 | 0.672 | 0.460 | 0.982 |
| Job Control | |||||||
| Skill discretion (low) | 0.320 | 0.248 | 1.673 | 0.196 | 1.377 | 0.848 | 2.237 |
| Decision authority (low) | −0.095 | 0.216 | 0.192 | 0.661 | 0.917 | 0.596 | 1.389 |
| Moderator effect of JC | |||||||
| PhyJD x JC (Skill) | −0.257 | 0.329 | 0.541 | 0.462 | 0.785 | 0.412 | 1.495 |
| PhyJD x JC (Dauth) | 0.007 | 0.320 | 0.000 | 0.983 | 1.007 | 0.538 | 1.886 |
| PsyJD x JC (Skill) | −0.533 | 0.195 | 7.467 | 0.006 | 0.587 | 0.400 | 0.860 |
| PsyJD x JC (Skill) | −0.302 | 0.313 | 0.929 | 0.335 | 0.739 | 0.400 | 1.366 |
| Variables in the Model | Odds Ratios | ||||||
|---|---|---|---|---|---|---|---|
| 95% C.I. for OR | |||||||
| Variables | B | Standard | Wald | p | OR | Lower | Upper |
| Job Demands | |||||||
| Psychological JD (high) | −0.122 | 0.466 | 0.069 | 0.793 | 0.885 | 0.355 | 2.206 |
| Physical JD (high) | −0.397 | 0.193 | 4.223 | 0.040 | 0.672 | 0.460 | 0.982 |
| Job Control | |||||||
| Skill discretion (low) | −0.041 | 0.351 | 0.014 | 0.906 | 0.960 | 0.483 | 1.908 |
| Decision authority (low) | −0.175 | 0.301 | 0.337 | 0.562 | 0.840 | 0.466 | 1.515 |
| Moderator effect of JC | |||||||
| PhyJD x JC (Skill) | 0.259 | 0.485 | 0.285 | 0.594 | 1.295 | 0.500 | 3.354 |
| PhyJD x JC (Dauth) | −0.341 | 0.461 | 0.548 | 0.459 | 0.711 | 0.288 | 1.754 |
| PsyJD x JC (Skill) | −0.348 | 0.487 | 0.511 | 0.475 | 0.706 | 0.272 | 1.834 |
| PsyJD x JC (Skill) | −0.621 | 0.264 | 5.543 | 0.019 | 0.538 | 0.321 | 0.901 |
| Social Support | |||||||
| Co-worker support (low) | 0.029 | 0.466 | 0.004 | 0.950 | 1.03 | 0.413 | 2.566 |
| Supervisor support (low) | −0.215 | 0.485 | 0.196 | 0.658 | 0.807 | 0.312 | 2.087 |
| Moderator effect of Social Support | |||||||
| PhyJD x JC (Skill) | 0.769 | 0.521 | 2.178 | 0.140 | 2.157 | 0.777 | 5.989 |
| PhyJD x JC (Dauth) | −0.749 | 0.267 | 7.848 | 0.005 | 0.473 | 0.280 | 0.799 |
| PsyJD x JC (Skill) | −0.814 | 0.519 | 2.457 | 1.117 | 0.443 | 0.160 | 1.226 |
| PsyJD x JC (Skill) | 0.522 | 0.492 | 1.126 | 0.289 | 1.686 | 0.642 | 4.423 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Navajas-Romero, V.; Ariza-Montes, A.; Hernández-Perlines, F. Analyzing the Job Demands-Control-Support Model in Work-Life Balance: A Study among Nurses in the European Context. Int. J. Environ. Res. Public Health 2020, 17, 2847. https://doi.org/10.3390/ijerph17082847
Navajas-Romero V, Ariza-Montes A, Hernández-Perlines F. Analyzing the Job Demands-Control-Support Model in Work-Life Balance: A Study among Nurses in the European Context. International Journal of Environmental Research and Public Health. 2020; 17(8):2847. https://doi.org/10.3390/ijerph17082847
Chicago/Turabian StyleNavajas-Romero, Virginia, Antonio Ariza-Montes, and Felipe Hernández-Perlines. 2020. "Analyzing the Job Demands-Control-Support Model in Work-Life Balance: A Study among Nurses in the European Context" International Journal of Environmental Research and Public Health 17, no. 8: 2847. https://doi.org/10.3390/ijerph17082847
APA StyleNavajas-Romero, V., Ariza-Montes, A., & Hernández-Perlines, F. (2020). Analyzing the Job Demands-Control-Support Model in Work-Life Balance: A Study among Nurses in the European Context. International Journal of Environmental Research and Public Health, 17(8), 2847. https://doi.org/10.3390/ijerph17082847







