Abstract
Virtual runs (real running or walking activities using online recording platforms) have been popular in the digital age and could have the potential to promote physical activity (PA) in workplaces. We investigated the effects of a virtual-run intervention (VRI) on PA and body compositions among university employees. A three-phase intervention was conducted over 6 months: 0 (pre-intervention), 1 (during intervention), and 2 (post-intervention). Exercise stages of change were assessed in phases 0 and 2. Body compositions (body weight, body mass index, fat mass, percentage of fat mass, fat-free mass, and percentage of fat-free mass) were assessed in phases 0, 1, and 2. Running and walking times were recorded through a mobile application. Forty-seven participants completed the VRI. The number of participants at the maintenance stage increased from 34.04% in phase 0 (n = 16) to 63.83% in phase 2 (n = 30). None of the changes in body compositions were significant (p > 0.05). The median running and walking time among participants at the maintenance stage was 151.85 (interquartile range, 109.15) min/week. Future research should focus on approaches to improve the efficacy of VRIs and their effects on health outcomes.
1. Introduction
Physical inactivity or insufficient physical activity (PA) is a global public health challenge [1,2]. Worldwide, more than one-fifth of adults are insufficiently physically active [1]. One possible reason for physical inactivity is a busy lifestyle and heavy workload [3,4]. White collar and professional workers spend a large proportion of their working time on light-intensity PA and sedentary behaviors [5,6]. Specifically, university employees are likely to be sedentary, physically inactive, and have a high prevalence of high body mass index (BMI) and blood pressure [7]. Fountaine et al. investigated occupational sitting and PA among four categories of university employees (administration, faculty, staff, facilities management) [8]. They showed that most university employees participated in low levels of leisure-time PA and spent ~75% of a workday on sitting activities (except facilities-management workers) [8].
Promoting PA in workplaces is a potential approach to increase PA and improve health outcomes among employees [9,10,11]. Moreover, a systematic review by Grimani and colleagues showed that health-promotion interventions in the workplace, including PA and nutrition, can improve productivity, work performance, and workability [12]. Intervention patterns to promote PA in workplaces are diverse [13]. In a context of a university worksite, Butler and colleagues presented the positive effects of an intervention on daily step counts and cardiovascular health outcomes [14]. Promoting PA among employees in university worksites requires the understanding of specific barriers to participation in health-promotion programs [15].
Virtual runs or virtual races have become popular in recent years [16]. Each virtual run consists of different components and characteristics [17,18]. A virtual run has not been defined clearly. In general, a virtual run is defined as a running or walking activity using an online platform to record activities. Specifically, a virtual run needs a real running or walking activity (a real activity) and an online recording platform (a virtual platform). Participants use a time-based goal (e.g., run or walk for 30 days) or a distance-based goal (e.g., run or walk for 100 km).
The possible advantages of virtual runs are flexibility (participants can run or walk at any time and place) and the recording systems. This setup can help participants adjust their PA strategies and achieve PA goals. However, there is a knowledge gap of the effects of virtual runs on PA and health outcomes. We investigated the effects of a workplace-based virtual-run intervention (VRI) on PA and body compositions among university employees.
2. Materials and Methods
2.1. Study Design
A pre- and post-intervention study was conducted between March and October 2019. The study consisted of three phases: (i) phase 0 (pre-intervention); (ii) phase 1 (during intervention); (iii) phase 2 (post-intervention).
2.2. Setting and Participants
The workplace-based study was conducted on a campus at Walailak University (Nakhon Si Thammarat, Thailand). The total number of university employees recruited was 1213. These university employees were invited to participate in the ‘virtual run program’. Exclusion criteria were employees who had contraindications to exercise (e.g., coronary artery disease, uncontrolled hypertension, uncontrolled diabetes mellitus) or core members of the Walailak University Running for Health Club (WURfHC; the authors of this article). The program invitation with a registration link was posted on the intranet webpage of Walailak University and Facebook™ page of the WURfHC.
2.3. VRI and Data Collection
In phase 0 (pre-intervention), participants were requested to complete the demographic and exercise stages of change (ESC) questions via a Google™ Form (Alphabet, Mountain View, CA, USA). Subsequently, participants were assigned to download Endomondo™ (Under Armour, Baltimore, MD, USA) on personal mobile devices. Endomondo is a free mobile application that uses the Global Positioning System to track PA [19]. By the end of March 2019, the core members of the WURfHC (the authors) were assigned, as the group motivators and observers, into five running groups. Each running group consisted of a combination of participants with mixed ESC (pre-contemplation, contemplation, preparation, action, maintenance). Each participant could see his/her running and walking time, as well as that of peers, within the group. Within each group, the group motivators also recorded their running and walking times and could encourage participants by text messages and their records in the application. Body compositions (body weight, fat mass, percentage of fat mass, fat-free mass, percentage of fat-free mass) were measured by bioelectrical impedance analysis using a Tanita model SC330P machine (Tanita, Tokyo, Japan).
In phase 1 (during intervention), participants had undertaken a virtual run (running and walking activities at any location and any time) over a 6-month period during the summer to early rainy season, which was a suitable period for outdoor activities (April to September 2019). Participants were requested to record only running and walking activities for travelling and recreational reasons. The participants could record their running and walking activities through three methods: (i) carrying a mobile device and turning on the application during activities; (ii) recording the activities using wearable devices (e.g., smart watches) and transferring the records to the application; (iii) recording the activity time on the application manually after activities. Participants were asked to omit recording occupational PA. In July 2019 (at 3 months of intervention), the body compositions of participants were measured.
In phase 2 (post-intervention), participants answered a questionnaire regarding ESC. Body compositions were measured. Accumulation of running and walking time was collected from the application by the group observers. Running jerseys were rewarded for participants who participated in more than 600 min of running and walking activities within 6 months. Table 1 shows the summary of the interventions.

Table 1.
Summary of virtual-run intervention and data-collection processes.
2.4. Outcome Measurement and Data Analyses
2.4.1. Demographic Data and ESC
Age of participants was described as the mean ± standard deviation (SD). Sex was presented as frequencies and percentages. The ESC questionnaire consisted of four dichotomous questions (Yes or No): (i) ‘I am currently physically active (at least 30 min per week)’; (ii) ‘I intend to become more physically active in the next 6 months’; (iii) ‘I currently engage in regular physical activity’; (iv) ‘I have been regularly physically active for the past 6 months’ [20]. The interpretation was a stage of change (Table 2) [20,21].

Table 2.
Interpretation and description of exercise stages of change.
The ESC of each participant was described and compared between phase 0 and phase 2. Changes in the ESC were translated to ‘improved’ (higher stage), ‘remained’ (similar stage), or ‘declined’ (lower stage).
2.4.2. Statistical Analysis
Body weight, fat mass, and fat-free mass were measured in kilograms. Percentage of fat mass and fat-free mass were recorded. BMI was calculated automatically by the measuring machine. Body compositions were presented as the mean ± SD or median and interquartile range (IQR), as appropriate, in phase 0, phase 1, and phase 2. Each variable of body composition was tested for a normal distribution using the Shapiro–Wilk test. Trends (three-point analysis) of body compositions were evaluated using one-way analysis of variance (one-way ANOVA) or the Kruskal–Wallis test. The total running and walking time was presented in minutes. The weekly time was calculated by dividing the total time with the number of weeks of participation in the intervention (total time in minutes/26 weeks). The median time spent on running and walking and IQR were calculated and classified into each ESC. A value of p < 0.05 was considered significant, and data were analyzed using GraphPad Prism v8.3.1 (GraphPad, San Diego, CA, USA).
2.5. Ethical Approval of the Study Protocol
The study protocol was approved by the Human Research Ethics Committee of Walailak University (WUEC-19-034-01). Participation in the study was entirely voluntary. Details of the study were provided on the first page of the online questionnaire in phase 0. Participants were asked to provide their consent by ticking a checkbox before taking part in the study.
3. Results
3.1. Participants
A total of 103 employees (64 females and 39 males; mean age, 37.82 ± 9.15 years) completed the questionnaire in phase 0. Fourteen employees did not participate in the VRI. Therefore, 89 participants (53 females and 36 males; mean age 37.37 ± 9.22 years) started the VRI. Forty-seven participants (30 females and 17 males; mean age 39.94 ± 9.12 years) completed the VRI (retention = 52.81%).
3.2. Motivation Towards PA
The motivations of 103 employees based on the ESC were assessed in phase 0. Forty-two of them (40.78%) were at the maintenance stage. In phase 2, the ESC in 47 participants were evaluated; 30 participants (63.83%) were at the maintenance stage. Of 47 participants who completed the VRI, the improved stage was dominant (n = 24, 51.06%). Sixteen were at the remained stage (34.04%) and seven were in the declined stage (14.90%) (Table 3).

Table 3.
Exercise stages of change in phase 0 (pre-intervention) and phase 2 (post-intervention).
3.3. Body Compositions
In phase 0, 47 participants, who engaged in the VRI, completed the assessment for body compositions. In phase 1, 26 participants were assessed. In phase 2, 47 participants attended the assessment for body compositions.
3.3.1. Body Weight and BMI
The median (IQR) of body weight (in kg) was 63.00 (27.00), 65.00 (25.00), and 64.00 (16.00) in phase 0, 1, and 2, respectively. The median (IQR) of BMI was stable from phase 0 to phase 2: 24.00 (4.00) kg/m2. The change in body weight (Figure 1a) and BMI (Figure 1b) was not significant (Kruskal–Wallis test).
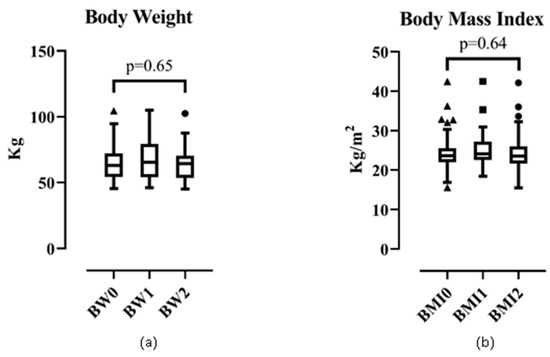
Figure 1.
Trend of (a) body weight and (b) body mass index.
3.3.2. Fat Mass and Percentage of Fat Mass
Fat mass and percentage of fat mass were not significant over the intervention period (Figure 2). The median (IQR) of fat mass (in kg) was 17.00 (8.00), 17.00 (10.00), and 17.00 (10.00) in phase 0, 1, and 2, respectively (p = 0.78 by the Kruskal–Wallis test). The mean ± SD of percentage of fat mass was 27.00% ± 10.00%, 28.00% ± 11.00%, and 27.00% ± 10.00% for phase 0, 1, and 2, respectively (p = 0.92 by one-way ANOVA).
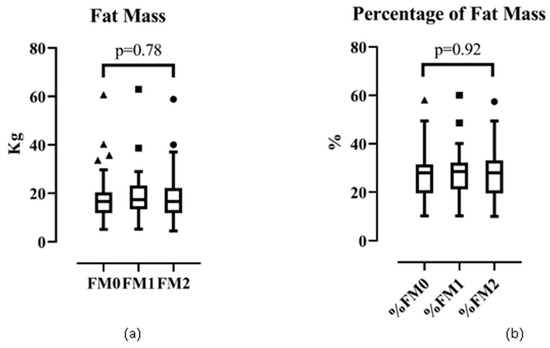
Figure 2.
Trend of (a) fat mass and (b) percentage of fat mass.
3.3.3. Fat-free Mass and Percentage of Fat-free Mass
The change in fat-free mass and percentage of fat-free mass was not significant in phase 0, 1, and 2 (Figure 3). The median (IQR) of fat-free mass (in kg) was 41.00 (15.00), 41.00 (18.00), and 41.00 (13.00) in phase 0, 1, and 2 (p = 0.83 by the Kruskal–Wallis test). The mean ± SD of the percentage of fat-free mass was 69.00% ± 9.90%, 68.00% ± 10.00%, and 69.00% ± 9.90% in phase 0, 1, and 2, respectively (p = 0.91 by one-way ANOVA).
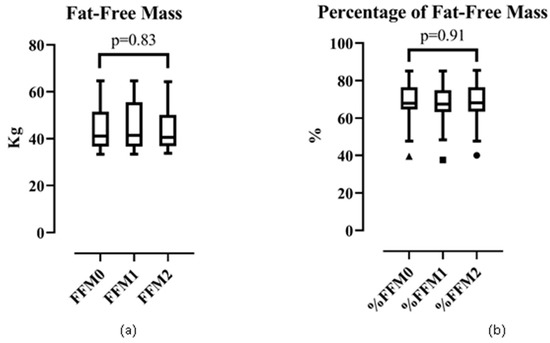
Figure 3.
Trend analysis of: (a) fat-free mass and (b) percentage of fat-free mass.
3.4. Running and Walking Time
Table 4 presents the total running and walking time collected in phase 2 and weekly running and walking time (calculated by dividing the total time with 26 weeks). Of 47 participants, the median (IQR) running and walking time was 1545.00 (2290.50) min over 26 weeks of the VRI, which was 59.42 (88.10) min/week. Participants in the maintenance stage (n = 30) achieved 151.85 (109.15) min/week.

Table 4.
Running and walking time by exercise stages of change.
4. Discussion
The VRI obtained low retention (52.81%) among voluntary participants in a university worksite. Initially, most participants were at the maintenance stage, whereas more than half dropped out of the VRI. In addition, 51.06% of participants who engaged in the entire intervention period reported improvement in the ESC. Body compositions were not changed significantly during the 6-month VRI.
In phase 0, only 8.55% (103/1204; excluding the authors) of university employees were interested in the VRI. Of 103 registered participants, 14 were considered non-usage attrition (never used the intervention) [22]. Of 89 participants who commenced the intervention, 42 dropped out (dropout attrition, 47.19%). Overall, the attrition prevalence was 54.37% (56/103). The attrition prevalence of our study is comparable with that of other digital health interventions in workplaces (range, 0% to 60%; median, 21%) [23]. This intervention offered some components for which barriers had to be overcome by employees (e.g., using an online platform, offering objective PA measurement), and another approach, such as offering incentives, might improve the retention of study participants [24]. Nevertheless, in terms of promoting PA at workplaces, participatory, multicomponent, and holistic approaches are required [25].
Initially, of 47 participants in the VRI, 16 (34.04%) were at the maintenance stage. At the end of the VRI, 30 (63.83%) were at the maintenance stage. One mechanism that might explain the overall improvement in motivation towards PA was a mixture of participants at different stages in each running group. This approach enabled the Köhler effect among participants: a reaction in a group when a weaker member is motivated by stronger members [26]. Although the overall changes were improved, some participants were stable at similar stages, whereas others regressed to lower stages. Three out of 16 participants relapsed from the maintenance stage to lower stages: this reflected dynamic changes of PA behaviors. A challenge of this VRI was to prevent a relapse of physical inactivity or insufficient PA in active participants.
Although the VRI had the potential to improve motivations towards PA, it could not improve body compositions over the 6-month period. The VRI assigned participants to collect activities time without a specific goal. An ideal virtual run can offer a SMART goal, which can be an effective scheme to enhance physical fitness [27]. The SMART mnemonic refers to: Specific (a specific activity, such as running or walking), Measurable (an objective recording system), Achievable (a program for different individuals), Results-focused (a realistic result), and Timely (a realistic timeframe) [28]. Virtual-run administrators should manage a clear and specific goal for each VRI.
Overall, participants spent 59.42 min/week on running and walking activities through the intervention period. Participants at the maintenance stage (151.85 min/week) achieved the weekly recommended time, but PA intensity could not be measured. Current PA recommendations suggest that adults should undertake ≥150 min/week of moderate-intensity aerobic PA or ≥75 min/week of vigorous-intensity aerobic PA or an equivalent combination of moderate-to-vigorous-intensity PA [29,30,31]. In addition, a virtual run should set the moderate-to-vigorous-intensity PA as a threshold. This may be a key factor to improve VRI efficacy.
Our study had three main strengths. First, the VRI offered an easy and convenient program in a workplace-based setting in which participants could engage at any time and place. Second, the PA recording system was an objective measurement that provided several simple methods to record running and walking activities. This approach could support participants with various mobile devices. Although one method was a manual recording method, running and walking time was easily recorded and validated. Third, a long intervention period allowed observation of changes in PA motivations over the 6-month period.
The study had three major limitations. First, the study cohort was small. This reflected a lack of interest in the VRI among university employees. Second, the prevalence of attrition was high. A possible reason was that the motivational incentives might not be enough to retain the number of participants. Third, PA records did not indicate PA intensity. For example, a participant recorded a certain time for a walking session, but this information did not specify the intensity of the activity.
5. Conclusions
The VRI could improve motivations towards PA among university employees. However, some challenges (high prevalence of attrition, a non-improvement of body composition, non-achievement of PA recommendations) were addressed. Future research should focus on approaches to improve the efficacy of VRIs and their effects on health outcomes.
Author Contributions
Conceptualization, A.W., W.A. and W.P.; methodology, A.W.; validation, A.W; formal analysis, A.W. and W.P.; investigation, A.W.; resources, A.W., W.A., W.P., P.S., U.C., S.K., W.C., K.E. and N.C.; data curation, A.W., W.A., W.P., P.S., U.C., S.K., W.C., K.E. and N.C.; writing—original draft preparation, A.W.; writing—review and editing, A.W.; visualization, A.W.; project administration, W.C., K.E. and N.C.; funding acquisition, A.W. All authors have read and agreed to the published version of the manuscript.
Funding
Study expenses were funded by Walailak University under the Walailak University Running for Health Club and the new strategic research (P2P) project.
Acknowledgments
The authors wish to thank the project assistant, Aekthawat Watthanachon.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Kohl, H.W., 3rd; Craig, C.L.; Lambert, E.V.; Inoue, S.; Alkandari, J.R.; Leetongin, G.; Kahlmeier, S. The pandemic of physical inactivity: Global action for public health. Lancet 2012, 380, 294–305. [Google Scholar] [CrossRef]
- Angel, S. Movement perceived as chores or a source of joy: A phenomenological-hermeneutic study of physical activity and health. Int. J. Qual. Stud. Health Well-Being 2018, 13, 1516088. [Google Scholar] [CrossRef] [PubMed]
- Wattanapisit, A.; Fungthongcharoen, K.; Saengow, U.; Vijitpongjinda, S. Physical activity among medical students in Southern Thailand: A mixed methods study. BMJ Open 2016, 6, e013479. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.; Brown, W. Steps and sitting in a working population. Int. J. Behav. Med. 2004, 11, 219–224. [Google Scholar] [CrossRef] [PubMed]
- Thorp, A.A.; Healy, G.N.; Winkler, E.; Clark, B.K.; Gardiner, P.A.; Owen, N.; Dunstan, D.W. Prolonged sedentary time and physical activity in workplace and non-work contexts: A cross-sectional study of office, customer service and call centre employees. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 128. [Google Scholar] [CrossRef]
- Alkhatib, A. High prevalence of sedentary risk factors amongst university employees and potential health benefits of campus workplace exercise intervention. Work 2015, 52, 589–595. [Google Scholar] [CrossRef]
- Fountaine, C.J.; Piacentini, M.; Liguori, G.A. Occupational sitting and physical activity among university employees. Int. J. Exerc. Sci. 2014, 7, 295–301. [Google Scholar]
- Mulchandani, R.; Chandrasekaran, A.M.; Shivashankar, R.; Kondal, D.; Agrawal, A.; Panniyammakal, J.; Tandon, N.; Prabhakaran, D.; Sharma, M.; Goenka, S. Effect of workplace physical activity interventions on the cardio-metabolic health of working adults: Systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 134. [Google Scholar] [CrossRef]
- Dadaczynski, K.; Schiemann, S.; Backhaus, O. Promoting physical activity in worksite settings: Results of a German pilot study of the online intervention Healingo fit. BMC Public Health 2017, 17, 696. [Google Scholar] [CrossRef] [PubMed]
- Grande, A.J.; Cieslak, F.; Silva, V. Workplace exercise for changing health behavior related to physical activity. Work 2015, 53, 479–484. [Google Scholar] [CrossRef] [PubMed]
- Grimani, A.; Aboagye, E.; Kwak, L. The effectiveness of workplace nutrition and physical activity interventions in improving productivity, work performance and workability: A systematic review. BMC Public Health 2019, 19, 1676. [Google Scholar] [CrossRef] [PubMed]
- Jirathananuwat, A.; Pongpirul, K. Promoting physical activity in the workplace: A systematic meta-review. J. Occup. Health 2017, 59, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Butler, C.E.; Clark, B.R.; Burlis, T.L.; Castillo, J.C.; Racette, S.B. Physical activity for campus employees: A university worksite wellness program. J. Phys. Act. Health 2015, 12, 470–476. [Google Scholar] [CrossRef]
- Leininger Lisa, J.; Adams Kent, J.; DeBeliso, M. Differences in health promotion program participation, barriers and physical activity among faculty, staff and administration at a university worksite. Int. J. Workplace Health Manag. 2015, 8, 246–255. [Google Scholar] [CrossRef]
- Dening, L. The Rise of Virtual Races. Available online: https://www.theguardian.com/lifeandstyle/the-running-blog/2016/jul/14/the-rise-of-virtual-races (accessed on 10 March 2020).
- Virtual Runner UK. How Virtual Running Works. Available online: https://www.virtualrunneruk.com/how-it-works/ (accessed on 10 March 2020).
- Brately, R. How to Organize a Virtual Race. Available online: https://www.racedirectorshq.com/how-to-organize-a-virtual-race/ (accessed on 10 March 2020).
- Under Armour. Endomondo. Available online: https://www.endomondo.com/ (accessed on 25 February 2020).
- American College of Sports Medicine. Exercise is Medicine: Healthcare Providers’ Action Guide. Available online: https://exerciseismedicine.org/assets/page_documents/HCP_Action_Guide(3).pdf (accessed on 25 February 2020).
- Prochaska, J.O.; Velicer, W.F. The transtheoretical model of health behavior change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef]
- Jahangiry, L.; Shojaeizadeh, D.; Montazeri, A.; Najafi, M.; Mohammad, K.; Yaseri, M. Adherence and attrition in a web-based lifestyle intervention for people with metabolic syndrome. Iran J. Public Health 2014, 43, 1248–1258. [Google Scholar]
- Howarth, A.; Quesada, J.; Silva, J.; Judycki, S.; Mills, P.R. The impact of digital health interventions on health-related outcomes in the workplace: A systematic review. Digit. Health 2018, 4, 2055207618770861. [Google Scholar] [CrossRef]
- Meng, L.; Wolff, M.B.; Mattick, K.A.; DeJoy, D.M.; Wilson, M.G.; Smith, M.L. Strategies for worksite health interventions to employees with elevated risk of chronic diseases. Saf. Health Work 2017, 8, 117–129. [Google Scholar] [CrossRef]
- Chau, J.Y.; Engelen, L.; Kolbe-Alexander, T.; Young, S.; Olsen, H.; Gilson, N.; Burton, N.W.; Bauman, A.E.; Brown, W.J. In Initiative Overload: Australian perspectives on promoting physical activity in the workplace from diverse industries. Int. J. Environ. Res. Public Health 2019, 16, 516. [Google Scholar] [CrossRef]
- Irwin, B.C.; Scorniaenchi, J.; Kerr, N.L.; Eisenmann, J.C.; Feltz, D.L. Aerobic exercise is promoted when individual performance affects the group: A test of the Kohler motivation gain effect. Ann. Behav. Med. 2012, 44, 151–159. [Google Scholar] [CrossRef] [PubMed]
- Samantha, M.M.; Stewart, G.T. The Effects of a goal setting intervention on aerobic fitness in middle school students. J. Teach. Phys. Educ. 2015, 34, 576–587. [Google Scholar]
- Frates, E.P.; Bonnet, J. Collaboration and negotiation: The key to therapeutic lifestyle change. Am. J. Lifestyle Med. 2016, 10, 302–312. [Google Scholar] [CrossRef] [PubMed]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The physical activity guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef] [PubMed]
- Wattanapisit, A. A review of the current international physical activity guidelines for various age groups to prevent and control noncommunicable diseases. Songklanagarind Med. J. 2016, 34, 39–49. [Google Scholar]
- World Health Organization. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).