Respiratory and Allergic Effects in Children Exposed to Pesticides—A Systematic Review
Abstract
1. Introduction
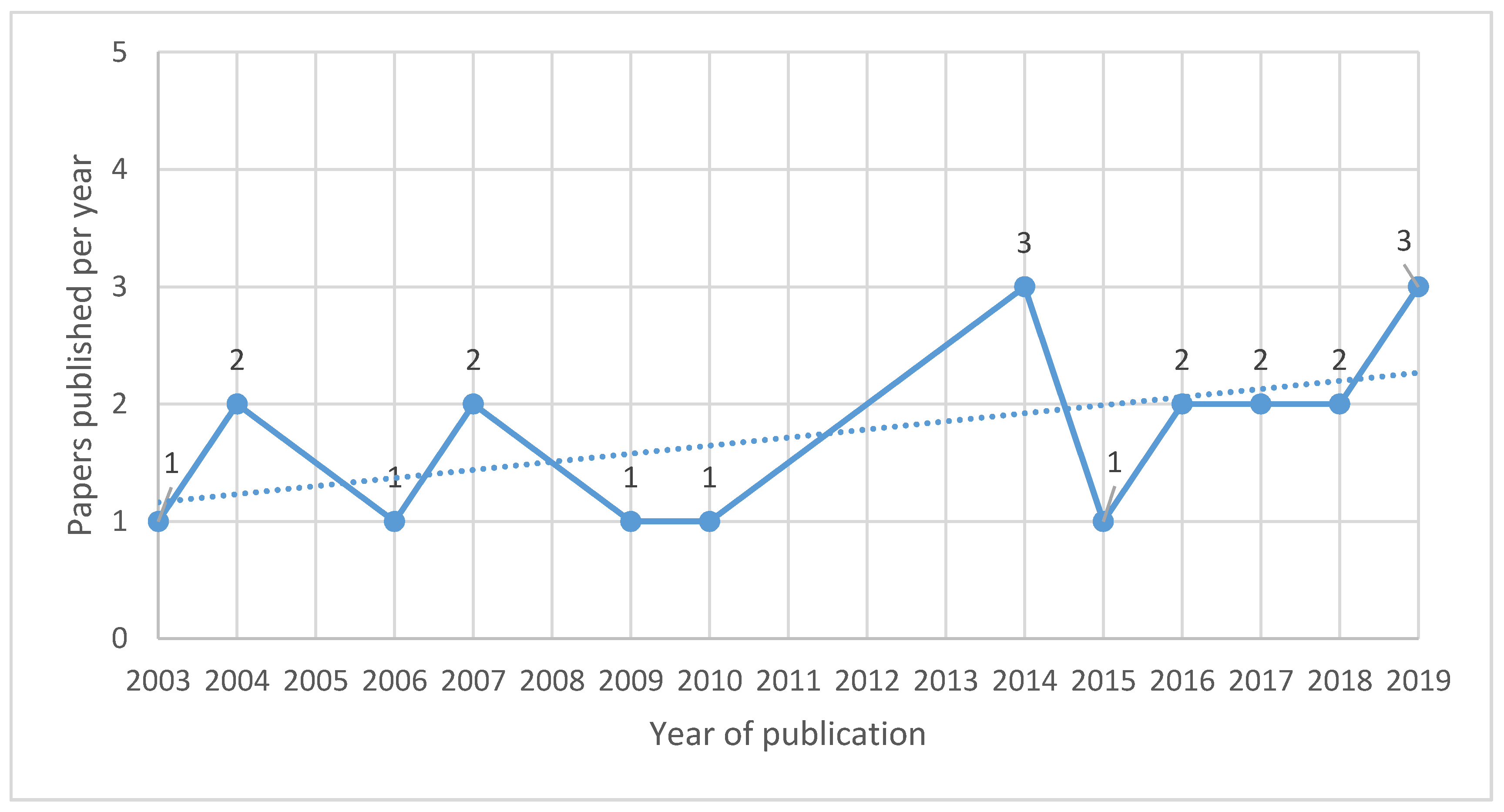
2. Materials and Methods
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Fareed, M.; Pathak, M.K.; Bihari, V.; Kamal, R.; Srivastava, A.K.; Kesavachandran, C.N. Adverse respiratory health and hematological alterations among agricultural workers occupationally exposed to organophosphate pesticides: A cross-sectional study in North India. PLoS ONE 2013, 8, e69755. [Google Scholar] [CrossRef]
- Chakraborty, S.; Mukherjee, S.; Roychoudhury, S.; Siddique, S.; Lahiri, T.; Ray, M.R. Chronic Exposures to Cholinesterase-inhibiting Pesticides Adversely Affect Respiratory Health of Agricultural Workers in India. J. Occup. Heal. 2009, 51, 488–497. [Google Scholar] [CrossRef] [PubMed]
- Baldi, I.; Robert, C.; Piantoni, F.; Tual, S.; Bouvier, G.; Lebailly, P.; Raherison, C. Agricultural exposure and asthma risk in the AGRICAN French cohort. Int. J. Hyg. Environ. Health 2014, 217, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Hoppin, J.A.; Umbach, D.M.; London, S.J.; Henneberger, P.K.; Kullman, G.J.; Coble, J.; Alavanja, M.C.R.; Beane Freeman, L.E.; Sandler, D.P. Pesticide use and adult-onset asthma among male farmers in the Agricultural Health Study. Eur. Respir. J. 2009, 34, 1296–1303. [Google Scholar] [CrossRef]
- Shama, F.A.; Skogstad, M.; Nijem, K.; Bjertness, E.; Kristensen, P. Cross-shift changes in lung function among palestinian farmers during high- and low-exposure periods to pesticides: A longitudinal study. Arch. Environ. Occup. Heal. 2015, 70, 218–224. [Google Scholar] [CrossRef]
- De Jong, K.; Boezen, H.M.; Kromhout, H.; Vermeulen, R.; Postma, D.S.; Vonk, J.M. Association of occupational pesticide exposure with accelerated longitudinal decline in lung function. Am. J. Epidemiol. 2014, 179, 1323–1330. [Google Scholar] [CrossRef]
- Buralli, R.J.; Ribeiro, H.; Mauad, T.; Amato-Lourenço, L.F.; Salge, J.M.; Diaz-Quijano, F.A.; Leão, R.S.; Marques, R.C.; Silva, D.S.; Guimarães, J.R.D. Respiratory condition of family farmers exposed to pesticides in the state of Rio de Janeiro, Brazil. Int. J. Environ. Res. Public Health 2018, 15, 1203. [Google Scholar] [CrossRef]
- Ye, M.; Beach, J.; Martin, J.W.; Senthilselvan, A. Occupational pesticide exposures and respiratory health. Int. J. Environ. Res. Public Health 2013, 10, 6442–6471. [Google Scholar] [CrossRef]
- Mamane, A.; Raherison, C.; Tessier, J.F.; Baldi, I.; Bouvier, G. Environmental exposure to pesticides and respiratory health. Eur. Respir. Rev. 2015, 24, 462–473. [Google Scholar] [CrossRef]
- Hyland, C.; Laribi, O. Review of take-home pesticide exposure pathway in children living in agricultural areas. Environ. Res. 2017, 156, 559–570. [Google Scholar] [CrossRef]
- Bradman, A.; Castorina, R.; Barr, D.B.; Chevrier, J.; Harnly, M.E.; Eisen, E.A.; McKone, T.E.; Harley, K.; Holland, N.; Eskenazi, B. Determinants of organophosphorus pesticide urinary metabolite levels in young children living in an agricultural community. Int. J. Environ. Res. Public Health 2011, 8, 1061–1083. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Toepel, K.; Irish, R.; Fenske, R.A.; Barr, D.B.; Bravo, R. Organic diets significantly lower children’s dietary exposure to organophosphorus pesticides. Environ. Health Perspect. 2006, 114, 260–263. [Google Scholar] [CrossRef] [PubMed]
- Marks, A.R.; Harley, K.; Bradman, A.; Kogut, K.; Barr, D.B.; Johnson, C.; Calderon, N.; Eskenazi, B. Organophosphate pesticide exposure and attention in young Mexican-American children: The CHAMACOS study. Environ. Health Perspect. 2010, 118, 1768–1774. [Google Scholar] [CrossRef] [PubMed]
- Roberts, J.R.; Karr, C.J. Pesticide exposure in children. Pediatrics 2012, 130, 11. [Google Scholar] [CrossRef]
- Salameh, P.R.; Baldi, I.; Brochard, P.; Raherison, C.; Saleh, B.A.; Salamon, R. Respiratory symptoms in children and exposure to pesticides. Eur. Respir. J. 2003, 22, 507–512. [Google Scholar] [CrossRef]
- Salam, M.T.; Li, Y.F.; Langholz, B.; Gilliland, F.D. Early-life environmental risk factors for asthma: Findings from the children’s health study. Environ. Health Perspect. 2004, 112, 760–765. [Google Scholar] [CrossRef]
- Xu, X.; Nembhard, W.N.; Kan, H.; Becker, A.; Talbott, E.O. Residential pesticide use is associated with children’s respiratory symptoms. J. Occup. Environ. Med. 2012, 54, 1281–1287. [Google Scholar] [CrossRef]
- Bukalasa, J.S.; Brunekreef, B.; Brouwer, M.; Koppelman, G.H.; Wijga, A.H.; Huss, A.; Gehring, U. Associations of residential exposure to agricultural pesticides with asthma prevalence in adolescence: The PIAMA birth cohort. Environ. Int. 2018, 121, 435–442. [Google Scholar] [CrossRef]
- Raanan, R.; Harley, K.G.; Balmes, J.R.; Bradman, A.; Lipsett, M.; Eskenazi, B. Early-life exposure to organophosphate pesticides and pediatric respiratory symptoms in the CHAMACOS cohort. Environ. Health Perspect. 2015, 123, 179–185. [Google Scholar] [CrossRef]
- Raanan, R.; Balmes, J.R.; Harley, K.G.; Gunier, R.B.; Magzamen, S.; Bradman, A.; Eskenazi, B. Decreased lung function in 7-year-old children with early-life organophosphate exposure. Thorax 2016, 71, 148–153. [Google Scholar] [CrossRef]
- Perla, M.E.; Rue, T.; Cheadle, A.; Krieger, J.; Karr, C.J. Biomarkers of Insecticide Exposure and Asthma in Children: A National Health and Nutrition Examination Survey (NHANES) 1999-2008 Analysis. Arch. Environ. Occup. Heal. 2015, 70, 309–322. [Google Scholar] [CrossRef] [PubMed]
- Reardon, A.M.; Perzanowski, M.S.; Whyatt, R.M.; Chew, G.L.; Perera, F.P.; Miller, R.L. Associations between prenatal pesticide exposure and cough, wheeze, and IgE in early childhood. J. Allergy Clin. Immunol. 2009, 124, 852–854. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, F.P. Pesticides, environment, and food safety. Food Energy Secur. 2017, 6, 48–60. [Google Scholar] [CrossRef]
- Mamane, A.; Tessier, J.-F.; Bouvier, G.; Salamon, R.; Lebailly, P.; Raherison, C.; Baldi, I.; Baldi, I. Increase in the Risk of Respiratory Disorders in Adults and Children Related to Crop-Growing in Niger. J. Environ. Public Health 2016, 2016, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Rutgers, C.; Colon, C.; Thapa, R.R.; Heikens, A.; Gutmann, B.; Biraghi, E.; Buj, V. UNICEF Understanding the Impacts of Pesticides on Children: A Discussion Paper; UNICEF: New York, NY, USA, 2018; pp. 1–26. [Google Scholar]
- Carneiro, F.F.; Augusto, L.G.S.; Rigotto, R.M.; Friedrich, K.; Búrigo, A.C. Dossiê ABRASCO: Um Alerta Sobre os Impactos dos Agrotóxicos na Saúde; Expressão Popular: São Paulo, Brasil, 2015; ISBN 978-85-9876-880-9. [Google Scholar]
- Negatu, B.; Kromhout, H.; Mekonnen, Y.; Vermeulen, R. Occupational pesticide exposure and respiratory health: A large-scale cross-sectional study in three commercial farming systems in Ethiopia. Thorax 2017, 72, 1–8. [Google Scholar] [CrossRef]
- Quansah, R.; Bend, J.R.; Abdul-Rahaman, A.; Armah, F.A.; Luginaah, I.; Essumang, D.K.; Iddi, S.; Chevrier, J.; Cobbina, S.J.; Nketiah-Amponsah, E.; et al. Associations between pesticide use and respiratory symptoms: A cross-sectional study in Southern Ghana. Environ. Res. 2016, 150, 245–254. [Google Scholar] [CrossRef]
- Faria, N.M.X.; Facchini, L.A.; Fassa, A.G.; Tomasi, E. Pesticides and respiratory symptoms among farmers. Rev. Saúde Pública 2005, 39, 973–981. [Google Scholar] [CrossRef]
- U.N. Human Rights Council Report of the Special Rapporteur on the Right to Food. Rep. Spec. Rapp. Right Food Hilal Elver 2017, 01059, 24. [Google Scholar]
- Muñoz-Quezada, M.T.; Lucero, B.A.; Barr, D.B.; Steenland, K.; Levy, K.; Ryan, P.B.; Iglesias, V.; Alvarado, S.; Concha, C.; Rojas, E.; et al. Neurodevelopmental effects in children associated with exposure to organophosphate pesticides: A systematic review. Neurotoxicology 2013, 39, 158–168. [Google Scholar] [CrossRef]
- Froes Asmus, C.I.R.; Camara, V.M.; Landrigan, P.J.; Claudio, L. A Systematic Review of Children’s Environmental Health in Brazil. Ann. Glob. Heal. 2016, 82, 132–148. [Google Scholar] [CrossRef]
- Van Wendel de Joode, B.; Mora, A.M.; Lindh, C.H.; Hernández-Bonilla, D.; Córdoba, L.; Wesseling, C.; Hoppin, J.A.; Mergler, D. Pesticide exposure and neurodevelopment in children aged 6–9 years from Talamanca, Costa Rica. Cortex 2016, 85, 137–150. [Google Scholar] [CrossRef] [PubMed]
- Runkle, J.; Flocks, J.; Economos, J.; Tovar-Aguilar, J.A.; McCauley, L. Occupational risks and pregnancy and infant health outcomes in florida farmworkers. Int. J. Environ. Res. Public Health 2014, 11, 7820–7840. [Google Scholar] [CrossRef] [PubMed]
- Gascon, M.; Sunyer, J.; Martínez, D.; Guerra, S.; Lavi, I. Persistent organic pollutants and children ’ s respiratory health: The role of cytokines and inflammatory biomarkers. Environ. Int. 2014, 69, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Weselak, M.; Arbuckle, T.E.; Wigle, D.T.; Krewski, D. In utero pesticide exposure and childhood morbidity. Environ. Res. 2007, 103, 79–86. [Google Scholar] [CrossRef] [PubMed]
- López-Gálvez, N.; Wagoner, R.; Quirós-Alcalá, L.; Van Horne, Y.O.; Furlong, M.; Avila, E.; Beamer, P. Systematic literature review of the take-home route of pesticide exposure via biomonitoring and environmental monitoring. Int. J. Environ. Res. Public Health 2019, 16, 2177. [Google Scholar] [CrossRef]
- Dayasiri, K.C.; Jayamanne, S.F.; Jayasinghe, C.Y. Patterns of acute poisoning with pesticides in the paediatric age group. Int. J. Emerg. Med. 2017, 10, 1–7. [Google Scholar] [CrossRef]
- Tagiyeva, N.; Devereux, G.; Semple, S.; Sherriff, A.; Henderson, J.; Elias, P.; Ayres, J.G. Parental occupation is a risk factor for childhood wheeze and asthma. Eur. Respir. J. 2010, 35, 987–993. [Google Scholar] [CrossRef]
- Benka-Coker, W.; Loftus, C.; Karr, C.; Magzamen, S.; Loftus, C.; Karr, C.; Magzamen, S.; Benka-coker, W.; Loftus, C.; Karr, C.; et al. Association of Organophosphate Pesticide Exposure and a Marker of Asthma Morbidity in an Agricultural Community Association of Organophosphate Pesticide Exposure and a Marker of Asthma Morbidity in an Agricultural Community. J. Agromed. 2019, 1, 1–9. [Google Scholar]
- Benka-Coker, W.; Loftus, C.; Karr, C.; Magzamen, S. Characterizing the joint effects of pesticide exposure and criteria ambient air pollutants on pediatric asthma morbidity in an agricultural community. Environ. Epidemiol. 2019, 3, e046. [Google Scholar] [CrossRef]
- Raanan, R.; Gunier, R.B.; Balmes, J.R.; Beltran, A.J.; Harley, K.G.; Bradman, A.; Eskenazi, B. Elemental sulfur use and associations with pediatric lung function and respiratory symptoms in an agricultural community (California, USA). Environ. Health Perspect. 2017, 125, 1–8. [Google Scholar] [CrossRef]
- Gunier, R.B.; Raanan, R.; Castorina, R.; Holland, N.T.; Harley, K.G.; Balmes, J.R.; Fouquette, L.; Eskenazi, B.; Bradman, A. Residential proximity to agricultural fumigant use and respiratory health in 7-year old children. Environ. Res. 2018, 164, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Raherison, C.; Baldi, I.; Pouquet, M.; Berteaud, E.; Moesch, C.; Bouvier, G.; Canal-raffin, M. Pesticides Exposure by Air in Vineyard Rural Area and Respiratory Health in Children: A pilot study. Environ. Res. 2019, 169, 189–195. [Google Scholar] [CrossRef] [PubMed]
- Duramad, P.; Harley, K.; Lipsett, M.; Bradman, A.; Eskenazi, B.; Holland, N.T.; Tager, I.B. Early environmental exposures and intracellular Th1/Th2 cytokine profiles in 24-month-old children living in an agricultural area. Environ. Health Perspect. 2006, 114, 1916–1922. [Google Scholar] [CrossRef] [PubMed]
- Kudagammana, S.T.; Mohotti, K. Environmental exposure to agrochemicals and allergic diseases in preschool children in high grown tea plantations of Sri Lanka. Allergy Asthma Clin. Immunol. 2018, 14, 1–5. [Google Scholar] [CrossRef]
- Dallaire, F.; Dewailly, É.; Muckle, G.; Vézina, C.; Jacobson, S.W.; Jacobson, J.L.; Ayotte, P. Acute infections and environmental exposure to organochlorines in Inuit infants from Nunavik. Environ. Health Perspect. 2004, 112, 1359–1364. [Google Scholar] [CrossRef] [PubMed]
- Meng, G.; Feng, Y.; Nie, Z.; Wu, X.; Wei, H.; Wu, S. Internal exposure levels of typical POPs and their associations with childhood asthma in Shanghai, China. Environ. Res. 2016, 146, 125–135. [Google Scholar] [CrossRef]
- Cupul-Uicab, L.A.; Terrazas-Medina, E.A.; Hernández-Ávila, M.; Longnecker, M.P. Prenatal Exposure to p,p′-DDE and p,p′-DDT in Relation to Lower Respiratory Tract Infections in Boys From a Highly Exposed Area of Mexico. Environ. Res. 2014, 132, 19–23. [Google Scholar] [CrossRef]

| Author, Year and Country | Study Design | Study Sample | Pesticides Addressed | Exposure Pathway and Activity | Exposure Assessment Method | Period of Exposure | Health Effect and Assessment Method | Results |
|---|---|---|---|---|---|---|---|---|
| Duramad, P. et al. 2006/USA | Longitudinal birth cohort (CHAMACOS) | 412 children aged up to 24 months | OP | Children who reside in agricultural settings | Questionnaire-based interviews with home visits | Prenatal up to 24 months | Respiratory symptoms through questionnaire-based interviews, medical records, and Th1 and Th2 cytokines as biomarkers of allergic asthma. | Asthma and wheeze outcomes in children at 24 months of age were associated with elevated Th2 status in children at early age. |
| Raanan, R. et al. 2015/USA | Longitudinal birth cohort (CHAMACOS) | 364 children aged 5y and 7y | OP | At least 1 agriculture worker in household | Maternal interviews and urinary DAP | Prenatal and childhood until age 5y and 7y | Respiratory symptoms through questionnaire (ISAAC) | Higher prenatal and childhood DAP [] were non-significantly associated with respiratory symptoms at 5y and 7y. |
| Raanan, R. et al. 2016/USA | Longitudinal birth cohort (CHAMACOS) | 279 children aged 7y | OP | At least 1 agriculture worker in household | Maternal interviews, home visits, six urinary DAP measured during pregnancy and five times in childhood | Prenatal and childhood until 7y | Spirometry | Childhood diethyl, dimethyl and total DAP [] were associated with significant decreases in lung function at age 7. Significantly lower FEV1 (ß = −0.16, 95%CI: −0.30; −0.02), and FVC (ß = −0.17, 95% CI: −0.34; 0.01) were observed per 10-fold increase of children’s total DAP levels. |
| Benka-Coker, WO. et al. 2019a/USA | Longitudinal cohort with 4 months follow-up | 16 asthmatic children aged 6 to 16y from agricultural communities | OP and joint effects with PM2.5 and Ozone | Residential proximity to crop areas, and parents involvement in agriculture | Repetitive urine samples for DAP (summative measures), and PM2.5 and Ozone [] data from local monitoring stations | Not clear | Asthma assessed through urinary uLTE4 collected every 6 days during the study period | Higher exposures to OP were associated with increases in the LTE4 levels, and concurrent short-term exposure to PM 2.5 was associated with an increase in a marker of asthma morbidity. |
| Benka-Coker, WO. et al. 2019b/USA | Longitudinal cohort with 4 months follow-up | 16 asthmatic children aged 6–16y from agricultural communities | OP | Residential proximity to crop areas, and parents’ involvement in agriculture | Repetitive urine samples for DAP, and comparison with another population-based cohort (NHANES). The total OP exposure was estimated through summative DAP measures, rather than individual measures | Not clear | Asthma assessed through urinary LTE4 collected every 6 days during the study period | Distribution of summed DAPs in this study were significantly higher than NHANES levels. Increase in uLTE4 levels were associated with increased exposures to DAPs, being significant only for EDE levels, after adjustment: 8.7 (95%CI: 2.8, 14.6). |
| Author, Year and Country | Study Sample | Study Design | Pesticides Addressed | Exposure Pathway and Activity | Exposure Assessment Method | Period of Exposure | Health Effect and Assessment Method | Results |
|---|---|---|---|---|---|---|---|---|
| Dallaire, F. et al. 2004/Canada | 199 Inuit infants up to 12 months | Review of medical charts | DDE | Environmental exposure, especially the consumption of fish and marine mammal fat | Maternal plasma during delivery and infant plasma at 7 months of age | Prenatal and at infancy | Comparison of incidence rates of upper and lower respiratory tract infections (URTIs and LRTIs, respectively) in two follow-ups (6 and 12 months) | Compared to rates for infants in the first quartile of DDE exposure (least exposed), adjusted RR for infants in higher quartiles ranged between 1.15 and 1.56 for URTIs, and 0.96 and 1.40 for LRTIs at the 6 months follow-up, while it ranged from 1.09 to 1.34 for URTIs, and from 0.98 to 1.13 for LRTIs at the 12 months follow-up, suggesting a possible association between prenatal exposure to OCs and acute infections early in life. Despite most RR were > 1.0, only URTIs at the 2nd quartile were statistically significant at both follow-up. |
| Gascon M., et al. 2007/Spain | 405 children aged up to 14y | Longitudinal birth cohort | DDE | Non-specific environmental exposure | DDE [] at cord blood samples, and immune biomarkers at age 4y | Prenatal exposure to DDE | Occurrence of wheeze, chest infections and asthma through questionnaire-based interviews at years 1, 2, 3, 4, 6.5, 10 and 14y | Prenatal DDE exposure was associated with wheeze at age 4y (RR per double of [] = 1.35; 95%CI: 1.07; 1.71), but not thereafter. Prenatal exposure was associated with children’s respiratory outcomes at different ages, but no associations were found between the immune biomarkers and DDE. |
| Cupul-Uicab, L.A. et al. 2014/Mexico | 747 newborn singleton boys | Longitudinal birth cohort | DDE and DDT | Chiapas where DDT was applied in crops until 1991 and for malaria control until 1998 | Maternal serum samples, and home visits | Prenatal exposure and from 12 months to 21 months | Mothers report on doctor diagnosis of pneumonia, bronchitis or other illness such as LRTI | Higher prenatal exposure to p,p-DDE and p,p-DDT were not associated with higher risk of LRTI before or after adjustment for confounders. |
| Meng, G. et al. 2016/China | 620 asthmatic children, and 218 non-asthmatic children aged 3–6y | Hospital-based Case-Control | OC | Environmental exposure, mainly from agriculture and residential use | Self-completed questionnaire | Not clear | Physician-diagnosed asthma by questionnaire and spirometry, and questionnaire to assess allergy symptoms (rhinitis and eczema) | Asthmatic children presented significantly higher levels of 7 OC pesticides (α-HCH, HCB, β-HCH, γ-HCH, Heptachlor, p,p’-DDE and o,p’-DDT) than non-asthmatic children. |
| Author, Year and Country | Study Sample | Study Design | Pesticides Addressed | Exposure Pathway and Activity | Exposure Assessment Method | Period of Exposure | Health Effect and Assessment Method | Results |
|---|---|---|---|---|---|---|---|---|
| Salameh, PR. et al. 2003/Lebanon | 3291 children aged 5–16y | Cross-sectional | Multiple pesticides | Environmental exposure of children from a randomly selected sample of public schools | Standardized questionnaire and residential exposure score, based on residential, para-occupational and domestic exposures | Not clear | Respiratory symptoms assessed by using the American Thoracic Society (ATS) questionnaire | Compared to non-exposed children, those exposed to pesticides had significantly higher odds of having respiratory disease (OR = 1.71; 95%CI: 1.20–2.43), asthma (OR = 1.73; 95%CI: 1.02–2.97), chronic phlegm (OR = 1.90; 95%CI: 1.26–2.87), recurrent wheezing (OR = 2.10; 95%CI: 1.39–3.18), and ever wheezing (OR = 1.99; 95%CI: 1.43–2.78), after adjustment for potential confounders. |
| Salam, MT. et al. 2004/EUA | 4000 school-aged children in 12 Southern California | Case-control | Multiple herbicides and pesticides | Children who had early-life environmental exposure to pesticides and other contaminants | Questionnaire and telephone interviews with mothers to collect additional exposure and asthma history | Prenatal and at first year of life | Physician-diagnosed asthma by age 5, and controls were asthma-free at study entry, frequency-matched on age, sex, and local of residence | Asthma diagnosis before 5y was significantly associated with pesticide exposure in the first year of life to herbicides (OR = 4.58; 95% CI, 1.36–15.43), and pesticides (OR = 2.39; 95% CI, 1.17–4.89). |
| Weselak, M. et al. 2007/Canada | 3405 children aged 0–12y or more, from family farmers | Retrospective cohort | Multiple pesticides | Living on a family farm | Questionnaires on pesticide use and involvement in agricultural activities | Prenatal | Respiratory symptoms through a questionnaire about health status | The odds of allergies and hay fever were significantly elevated in children who lived on farms with reported use of any pesticide, herbicides, fungicides, insecticides, OP, phenoxy, and 2,4-D during the pregnancy period, compared to children living on farms with no pesticide use. No associations were observed for persistent cough, bronchitis and asthma among the offspring of farm families. |
| Reardon AM. et al. 2009/EUA | 652 children aged 5y | Prospective birth cohort study | OP (chlorpyrifos and diazinon), and pyrethroids (cis-permethrin and trans-permethrin) | Elementary school children in California having a mother working in agriculture | Retrospective questionnaire, and measurement of prenatal levels of pesticide | Prenatal and first year of life | Questionnaire about wheeze and analysis of IgE production (5y); increased levels of TH2 cytokines in children (2y) | Prenatal exposures to pesticides may influence the risk of early cough, wheeze, and IgE production. Individual pesticides may differ in regard to risk. |
| Tagiyeva, G. et al. 2010/England | 13,971 children aged up to 102 months | Birth cohort-Avon Longitudinal Study of Parents and Children (ALSPAC) | Biocides and fungicides | Parental occupational exposure to pesticides, along with other contaminants | Questionnaire and clinic evaluations | Up to 102 months | Questionnaire, clinical assessments | Maternal postnatal occupational exposure to biocide/fungicide increased the likelihood of childhood wheeze (OR = 1.22; 95%CI: 1.02–2.05). |
| Perla, ME. et al. 2014/USA | 10,077 children aged from 6y to 16y | Cross-sectional population-based (NHANES) | Survey questionnaires and exposure biomarkers for OP (DAP) and DDT | Environmental exposures | Blood and urine tests | Up to 16 years old | Questionnaire, blood and urine tests | No clear associations between asthma and biomarkers of DAP or DDT insecticides among school aged children in the USA. Exposure to DAP and DDT is widespread and variable in U.S. children but higher metabolite levels were observed among Mexican Americans. |
| Runkle, J. et al. 2014/USA | Snowball sample with 170 farmworker mothers (mostly from Mexico, but also indigenous from Central America and others) | Cross-sectional survey with participatory approach(CBPR) | Multiple pesticides | Mother’s involvement in agriculture at nurseries (n = 62) and ferneries (n = 108), pesticide handling activities, father’s work as a farmer | Interviews about current and past work conditions (e.g., duration of work in agriculture while pregnant, father’s work in agriculture) | Prenatal until 1y (~52% worked the entire pregnancy period and ~48% worked partially) | Interview about outcomes during last pregnancy, infant’s health for the first year of life and doctor-diagnosed respiratory and breathing problems | Most self-reported child health problems were respiratory-related (~76%). Significantly more mothers working in ferneries reported child diagnosis of any health problem and were 2.7 times more likely to report child diagnosis of respiratory condition, compared to nursery workers. |
| Raanan, R. et al. 2017/USA | 347 children aged 7y living in an agricultural community | Longitudinal birth cohort (CHAMACOS) | Elemental sulfur | Residential proximity to agricultural areas with elemental sulfur applications | Sulfur application within 0.5, 1, and 3km of residences during the week, month, and 12 months prior to pulmonary evaluation using California’s Pesticide Use Report (PUR) data | Short-term exposure (week, month and a year) before the pulmonary assessment | Respiratory symptoms through questionnaires (ISAAC) with mothers, and spirometry with children at 7y | Sulfur applications within 0.5 and 1 km radii were associated with respiratory outcomes. Asthma medication use [OR = 3:51; 95% CI: 1.50; 8.23] and respiratory symptoms [OR = 2:09; 95% CI: 1.27; 3.46] significantly increased (both p = 0.004) and FEV1 significantly decreased (b = −0.14; 95% CI: −0:248, −0:039; p = 0:008) per 10-fold increase in the estimated amount of sulfur used within 1km of the residence during the year before pulmonary assessment. |
| Dayasiri, KC. et al. 2017/Sri Lanka | 155 children aged 9 months to 12y with pesticide poisoning | Retrospective and prospective hospital-based multisite study (admissions from 2007 to 2014) | Most frequent: OP (41%), CM (23%) and herbicides (12%) | 51.3% were exposed at cultivation sites, 18.9% at home gardens, and 16.2% at home kitchens | Questionnaire-based interviews in hospital admission | Not clear | Prevalence of respiratory symptoms among poisoned children, along with other symptoms | ~74% had less than 5y. About 58% of children had at least one parent engaged in farming activities and 50% use pesticide in farming. Only 8.6%–10.8% (depending on which hospital) of poisoned children presented respiratory symptoms. |
| Kudagammana, ST.; Mohotti, K. 2018/Sri Lanka | 182 preschool children aged 1–5y from an organic area (n = 81) and conventional area (n = 101) | Cross-sectional | Multiple pesticides | Children living close to tea plantations (conventional vs. organic) | Children from a conventional tea plantation were compared to children from an organic tea cultivation area | Not clear | Prevalence of allergic diseases through a questionnaire-based interview using the modified International Study of Asthma and allergies (ISAAC) | Wheezing was noted in 41.2% of children from the organic estate and 59.8% from the conventional estate. The respective percentages for allergic rhinitis were as 37.7% and 82.5% while for eczema they were 17.5% and 20.3%. |
| Gunier, RB. et al. 2018/USA | 294 children living in an agricultural area | Longitudinal birth cohort CHAMACOS | Fumigants (methyl bromide, chloropicrin, metam sodium and 1,3-dichloropropene) | Residential proximity to agricultural areas using fumigants | Fumigant use within 3, 5 and 8 km of residences during pregnancy and from birth to age 7 using PUR data | Prenatal and from cumulative exposure from birth to 7y | Respiratory symptoms (ISAAC) and asthma medication use through questionnaires with mothers, and spirometry with children at 7y | No significant associations were observed between residential proximity to fumigants use and respiratory symptoms, use of asthma medication, and lung function measurements. |
| Raherison, C. et al. 2019/France | 281 children aged 3–10y from 4 rural schools of a French vineyard region | Cross-sectional with two phases: during winter with no pesticide exposure, and summer, when pesticides are regularly applied | Multiple pesticides (insecticides, herbicides and fungicides) in outdoor air around schools, and phthalimides and dithiocarbamate fungicides in urine (ETU) | Proximity of schools from the edge of vineyards | Mobile stations located close to the schools for air monitoring, and urine measurements in a subset (n = 96) of studied children | Not clear | Asthma and rhinitis through ISAAC, and respiratory symptoms. A symptom score was made to classify children into low, moderate and high scores. Bronchial obstruction was measured to assess the FEV1 and FEV6 of the FVC, and spirometry was performed among children aged over 6y | 12 pesticides were detected in the schoolyards (89% fungicides and 11% insecticides), and significantly higher values of urine ETU [] were observed in the higher pesticide use period (p = 0.012). Urinary ETU [] was significantly associated with an increased risk of asthma and rhinitis (OR: 3.6 [1.04–12.1], after adjustment. No significant associations were found between lung function changes and pesticide exposure in air, or urinary ETU. |
| Region | Number of Articles | % | Countries (n, %) |
|---|---|---|---|
| Asia | 4 | 19.0 | Sri Lanka (n = 2, 9.5%); Lebanon and China (n = 1 each, 4.8%) |
| Europe | 3 | 14.3 | France, England, and Spain (n = 1 each, 4.8%) |
| North America | 14 | 66.7 | United States (n = 11, 52.4%); Canada (n = 2, 9.5%); Mexico (n = 1, 4.8%) |
| Total | 21 | 100 | 10 countries in total |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buralli, R.J.; Dultra, A.F.; Ribeiro, H. Respiratory and Allergic Effects in Children Exposed to Pesticides—A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 2740. https://doi.org/10.3390/ijerph17082740
Buralli RJ, Dultra AF, Ribeiro H. Respiratory and Allergic Effects in Children Exposed to Pesticides—A Systematic Review. International Journal of Environmental Research and Public Health. 2020; 17(8):2740. https://doi.org/10.3390/ijerph17082740
Chicago/Turabian StyleBuralli, Rafael Junqueira, Amana Freitas Dultra, and Helena Ribeiro. 2020. "Respiratory and Allergic Effects in Children Exposed to Pesticides—A Systematic Review" International Journal of Environmental Research and Public Health 17, no. 8: 2740. https://doi.org/10.3390/ijerph17082740
APA StyleBuralli, R. J., Dultra, A. F., & Ribeiro, H. (2020). Respiratory and Allergic Effects in Children Exposed to Pesticides—A Systematic Review. International Journal of Environmental Research and Public Health, 17(8), 2740. https://doi.org/10.3390/ijerph17082740





