Inequalities in Rotavirus Vaccine Uptake in Ethiopia: A Decomposition Analysis
Abstract
1. Introduction
2. Methods
2.1. Data and Variables
2.2. Measurement of Socioeconomic Status
2.3. Measuring Inequality in Rotavirus Vaccination
2.4. Decomposition Analysis
- yi is rotavirus vaccine uptake (yi = 1 if the child took two doses of rotavirus vaccine and yi = 0 if not);
- xki: a set of k explanatory variables for rotavirus vaccine uptake;
- βk: regression coefficients of explanatory variables xk;
- εi: error term.
3. Results
3.1. Descriptive Statistics
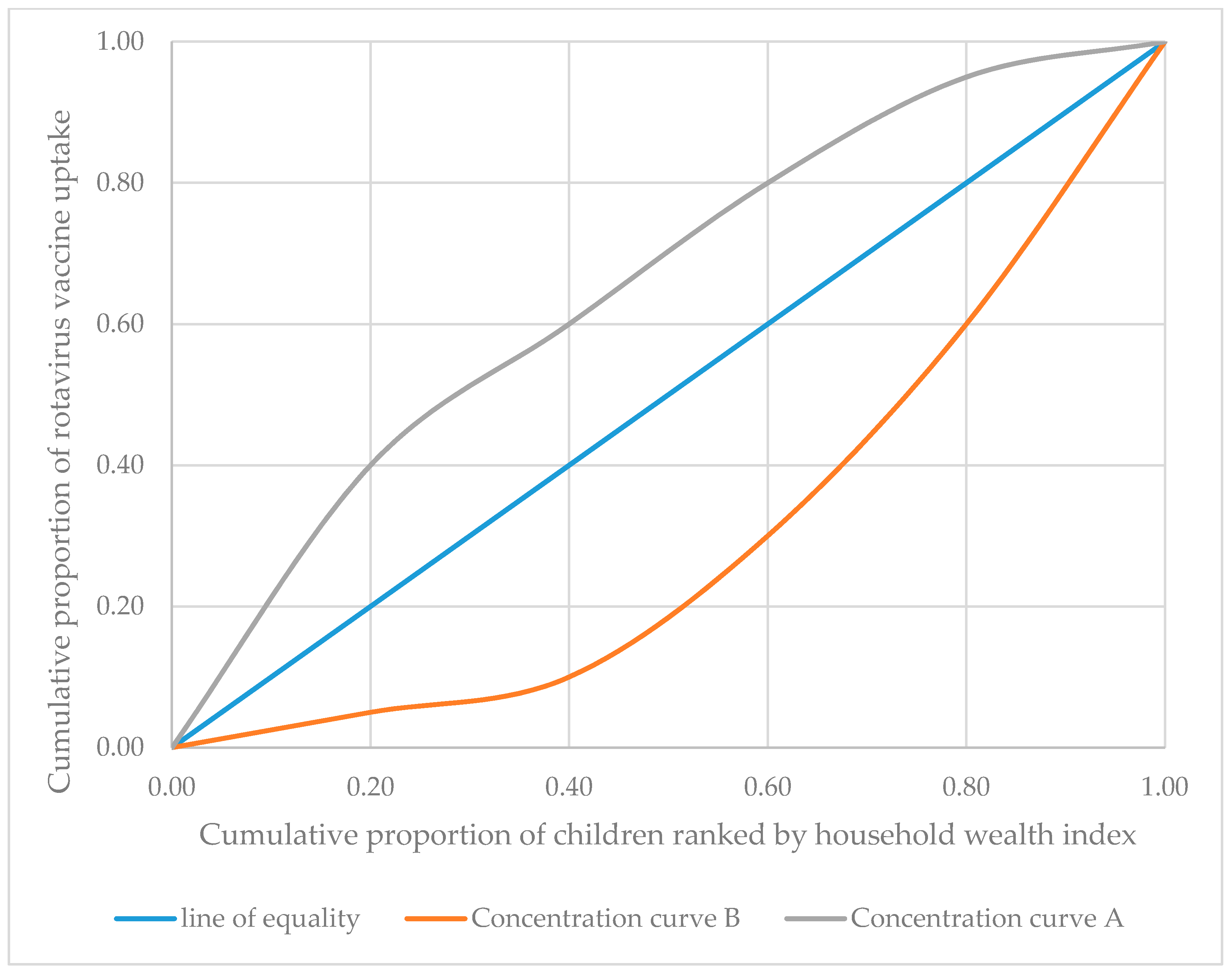
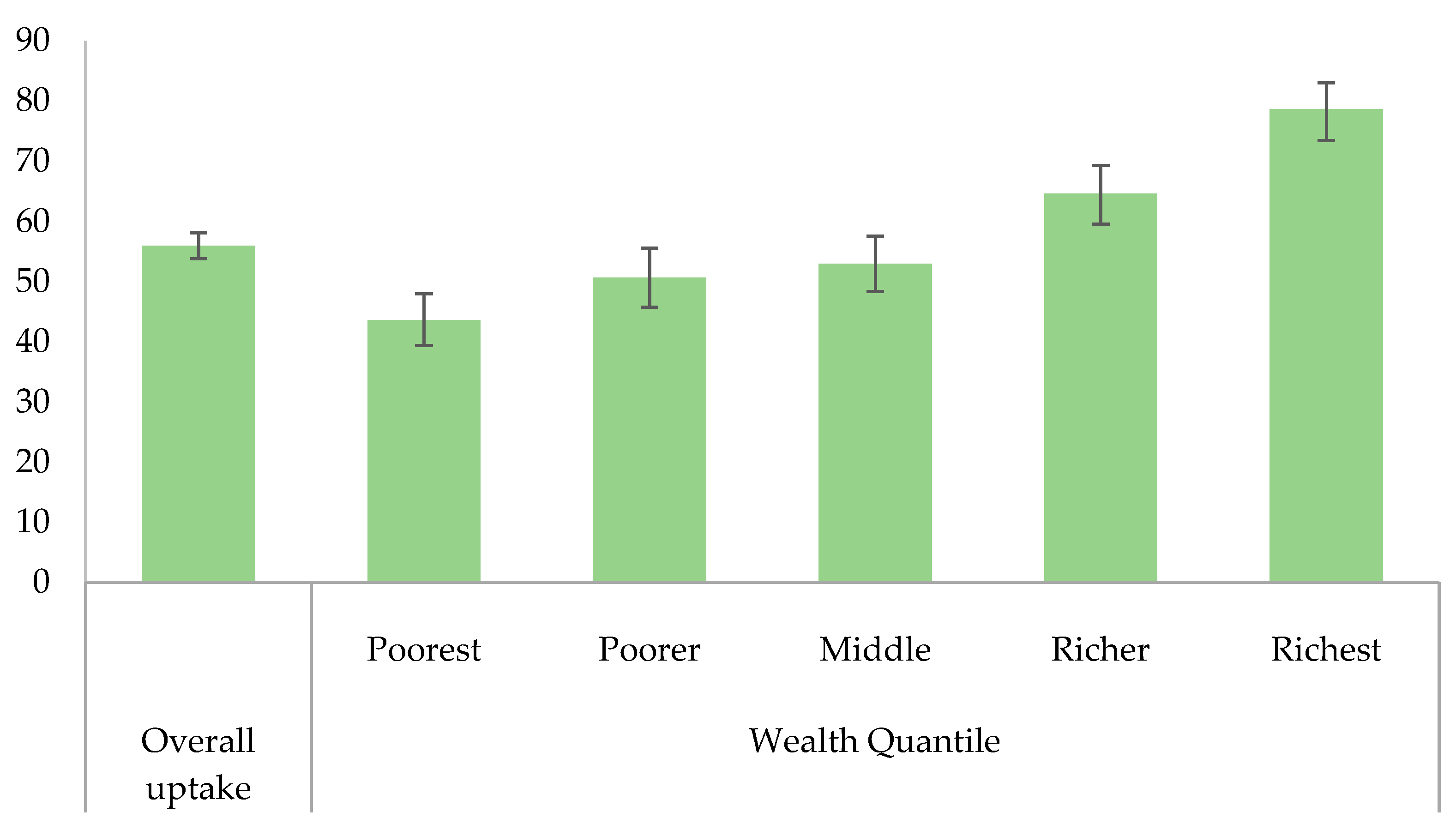
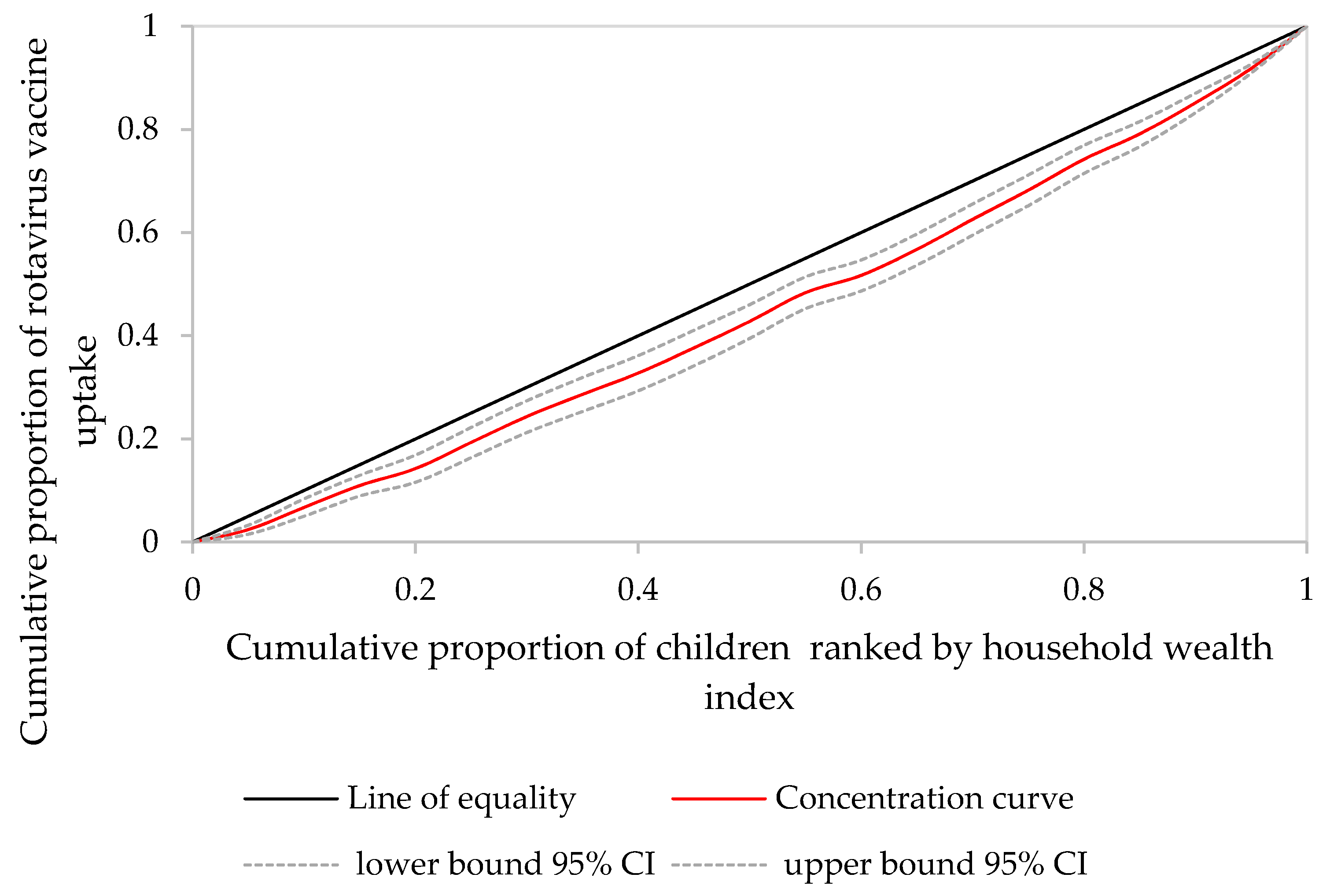
3.2. Wealth-Related Inequality of Rotavirus Vaccine Uptake
3.3. Results of Decomposition Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Doherty, M.; Buchy, P.; Standaert, B.; Giaquinto, C.; Prado- Cohrs, D. Vaccine impact: Benefits for human health. Vaccine 2016, 34, 6707–6714. [Google Scholar] [CrossRef] [PubMed]
- Gavi Immunisation and the Sustainable Development. Available online: https://www.gavi.org/about/ghd/sdg/ (accessed on 28 February 2019).
- WHO. WHO|10 Facts on Immunization. Available online: https://www.who.int/features/factfiles/immunization/en/ (accessed on 28 February 2019).
- WHO. Immunization Coverage. Available online: https://www.who.int/en/news-room/fact-sheets/detail/immunization-coverage (accessed on 28 February 2019).
- Wang, H.; Bhutta, Z.A.; Coates, M.M.; Coggeshall, M.; Dandona, L.; Diallo, K.; Franca, E.B.; Fraser, M.; Fullman, N.; Gething, P.W.; et al. Global, regional, national, and selected subnational levels of stillbirths, neonatal, infant, and under-5 mortality, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1725–1774. [Google Scholar] [CrossRef]
- Troeger, C.; Khalil, I.A.; Rao, P.C.; Cao, S.; Blacker, B.F.; Ahmed, T.; Armah, G.; Bines, J.E.; Brewer, T.G.; Colombara, D.V.; et al. Rotavirus Vaccination and the Global Burden of Rotavirus Diarrhea Among Children Younger Than 5 Years. JAMA Pediatr. 2018, 172, 958. [Google Scholar] [CrossRef] [PubMed]
- Abebe, A.; Getahun, M.; Mapaseka, S.L.; Beyene, B.; Assefa, E.; Teshome, B.; Tefera, M.; Kebede, F.; Habtamu, A.; Haile-Mariam, T.; et al. Impact of rotavirus vaccine introduction and genotypic characteristics of rotavirus strains in children less than 5 years of age with gastroenteritis in Ethiopia: 2011–2016. Vaccine 2018, 36, 7043–7047. [Google Scholar] [CrossRef]
- Mwenda, J.M.; Parashar, U.D.; Cohen, A.L.; Tate, J.E. Impact of rotavirus vaccines in Sub-Saharan African countries. Vaccine 2018, 36, 7119–7123. [Google Scholar] [CrossRef]
- Phillips, D.E.; Dieleman, J.L.; Lim, S.S.; Shearer, J. Determinants of effective vaccine coverage in low and middle-income countries: A systematic review and interpretive synthesis. BMC Health Serv. Res. 2017, 17, 681. [Google Scholar] [CrossRef]
- Rainey, J.J.; Watkins, M.; Ryman, T.K.; Sandhu, P.; Bo, A.; Banerjee, K. Reasons related to non-vaccination and under-vaccination of children in low and middle income countries: Findings from a systematic review of the published literature, 1999–2009. Vaccine 2011, 29, 8215–8221. [Google Scholar] [CrossRef]
- Van Malderen, C.; Ogali, I.; Khasakhala, A.; Muchiri, S.N.; Sparks, C.; Van Oyen, H.; Speybroeck, N. Decomposing Kenyan socio-economic inequalities in skilled birth attendance and measles immunization. Int. J. Equity Health 2013, 12, 3. [Google Scholar] [CrossRef]
- Debnath, A.; Bhattacharjee, N. Wealth-based inequality in child immunization in India: A decomposition approach. J. Biosoc. Sci. 2018, 50, 312–325. [Google Scholar] [CrossRef]
- Lauridsen, J.; Pradhan, J. Socio-economic inequality of immunization coverage in India. Health Econ. Rev. 2011, 1, 11. [Google Scholar] [CrossRef]
- Ataguba, J.E.; Ojo, K.O.; Ichoku, H.E. Explaining socio-economic inequalities in immunization coverage in Nigeria. Health Policy Plan. 2016, 31, 1212–1224. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.Y.; Riumallo-Herl, C.; Perales, N.A.; Clark, S.; Clark, A.; Constenla, D.; Garske, T.; Jackson, M.L.; Jean, K.; Jit, M.; et al. The Equity Impact Vaccines May Have on Averting Deaths and Medical Impoverishment in Developing Countries. Health Aff. 2018, 37, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Riumallo-Herl, C.; Chang, A.Y.; Clark, S.; Constenla, D.; Clark, A.; Brenzel, L.; Verguet, S. Poverty reduction and equity benefits of introducing or scaling up measles, rotavirus and pneumococcal vaccines in low-income and middle-income countries: A modelling study. BMJ Glob. Health 2018, 3, e000613. [Google Scholar] [CrossRef] [PubMed]
- CSA [Ethiopia]; ICF. Ethiopia Demographic and Health Survey 2016; CSA: Addis Ababa, Ethiopia; ICF: Rockville, MD, USA, 2016.
- Wondimu, A.; Cao, Q.; Wilschut, J.C.; Postma, M.J. Factors associated with the uptake of newly introduced childhood vaccinations in Ethiopia: The cases of rotavirus and pneumococcal conjugate vaccines. BMC Public Health 2019, 19, 1656. [Google Scholar] [CrossRef] [PubMed]
- UNDP. National Human Development Report 2014—Ethiopia; UNDP: New York, NY, USA, 2015. [Google Scholar]
- Rutstein, S.O.; Johnson, K. The DHS Program—Wealth Index Construction; USAID: Washington, DC, USA, 2004.
- O’Donnell, O.; van Doorslaer, E.; Wagstaff, A.; Lindelow, M. Analyzing Health Equity Using Household Survey Data A Guide to Techniques and Their Implementation Analyzing Health Equity Using Household Survey Data; The International Bank for Reconstruction and Development/The World Bank: Washington, DC, USA, 2008; ISBN 9780821369333. [Google Scholar]
- Wagstaff, A.; Paci, P.; van Doorslaer, E. On the measurement of inequalities in health. Soc. Sci. Med. 1991, 33, 545–557. [Google Scholar] [CrossRef]
- Erreygers, G. Correcting the Concentration Index. J. Health Econ. 2009, 28, 504–515. [Google Scholar] [CrossRef]
- Erreygers, G.; Van Ourti, T. Measuring socioeconomic inequality in health, health care and health financing by means of rank-dependent indices: A recipe for good practice. J. Health Econ. 2011, 30, 685–694. [Google Scholar] [CrossRef]
- Kjellsson, G.; Gerdtham, U.-G. On correcting the concentration index for binary variables. J. Health Econ. 2013, 32, 659–670. [Google Scholar] [CrossRef]
- Zhu, D.; Guo, N.; Wang, J.; Nicholas, S.; Wang, Z.; Zhang, G.; Shi, L.; Wangen, K.R. Socioeconomic inequality in Hepatitis B vaccination of rural adults in China. Hum. Vaccin. Immunother. 2018, 14, 464–470. [Google Scholar] [CrossRef]
- Ngandu, N.K.; Van Malderen, C.; Goga, A.; Speybroeck, N. Wealth-related inequality in early uptake of HIV testing among pregnant women: An analysis of data from a national cross-sectional survey, South Africa. BMJ Open 2017, 7, e013362. [Google Scholar] [CrossRef]
- Umuhoza, S.M.; Ataguba, J.E. Inequalities in health and health risk factors in the Southern African Development Community: Evidence from World Health Surveys. Int. J. Equity Health 2018, 17, 52. [Google Scholar] [CrossRef] [PubMed]
- Dorjdagva, J.; Batbaatar, E.; Dorjsuren, B.; Kauhanen, J. Income-related inequalities in health care utilization in Mongolia, 2007/2008–2012. Int. J. Equity Health 2015, 14, 57. [Google Scholar] [CrossRef] [PubMed]
- Makate, M.; Makate, C. The evolution of socioeconomic status-related inequalities in maternal health care utilization: Evidence from Zimbabwe, 1994–2011. Glob. Health Res. Policy 2017, 2, 1. [Google Scholar] [CrossRef] [PubMed]
- Kraft, A.D.; Nguyen, K.-H.; Jimenez-Soto, E.; Hodge, A. Stagnant Neonatal Mortality and Persistent Health Inequality in Middle-Income Countries: A Case Study of the Philippines. PLoS ONE 2013, 8, e53696. [Google Scholar] [CrossRef]
- Wagstaff, A.; van Doorslaer, E.; Watanabe, N. On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. J. Econ. 2003, 112, 207–223. [Google Scholar] [CrossRef]
- Van de Poel, E.; O’Donnell, O.; Van Doorslaer, E. Urbanization and the spread of diseases of affluence in China. Econ. Hum. Biol. 2009, 7, 200–216. [Google Scholar] [CrossRef]
- Allin, S.; Hurley, J. Inequity in publicly funded physician care: What is the role of private prescription drug insurance? Health Econ. 2009, 18, 1218–1232. [Google Scholar] [CrossRef]
- Erreygers, G.; Kessels, R. Regression-based decompositions of rankdependent indicators of socioeconomic inequality of health. In Research on Economic Inequality; Pedro, R.D., Owen, O., Eds.; JAI Press: Stamford, CT, USA, 2013; Volume 21, pp. 227–259. ISBN 9781781905531. [Google Scholar]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson Education Limited: Harlow, UK, 2014. [Google Scholar]
- Hu, Y.; Wang, Y.; Chen, Y.; Li, Q. Determinants of inequality in the up-to-date fully immunization coverage among children aged 24–35 months: Evidence from Zhejiang province, East China. Hum. Vaccin. Immunother. 2017, 13, 1902–1907. [Google Scholar] [CrossRef]
- Joe, W.; Mishra, U.S.; Navaneetham, K. Socio-economic inequalities in child health: Recent evidence from India. Glob. Public Health 2010, 5, 493–508. [Google Scholar] [CrossRef]
- Rheingans, R.; Atherly, D.; Anderson, J. Distributional impact of rotavirus vaccination in 25 GAVI countries: Estimating disparities in benefits and cost-effectiveness. Vaccine 2012, 30, A15–A23. [Google Scholar] [CrossRef]
- Pearson, L.; Gandhi, M.; Admasu, K.; Keyes, E.B. User fees and maternity services in Ethiopia. Int. J. Gynecol. Obstet. 2011, 115, 310–315. [Google Scholar] [CrossRef] [PubMed]
- Kea, A.Z.; Tulloch, O.; Datiko, D.G.; Theobald, S.; Kok, M.C. Exploring barriers to the use of formal maternal health services and priority areas for action in Sidama zone, southern Ethiopia. BMC Pregnancy Childbirth 2018, 18, 96. [Google Scholar] [CrossRef] [PubMed]
- Warren, C. Care seeking for maternal health: Challenges remain for poor women. Ethiop. J. Health Dev. 2010, 24, 100–104. [Google Scholar] [CrossRef]
- Ethiopian Public Health Institute. Ethiopia Service Provision Assessment Plus Survey 2014; Ethiopian Public Health Institute (EPHI) Federal Ministry of Health ICF International: Addis Ababa, Ethiopia, 2014. [Google Scholar]
- Birmeta, K.; Dibaba, Y.; Woldeyohannes, D. Determinants of maternal health care utilization in Holeta town, central Ethiopia. BMC Health Serv. Res. 2013, 13, 1–10. [Google Scholar] [CrossRef]
- Shiferaw, S.; Spigt, M.; Godefrooij, M.; Melkamu, Y.; Tekie, M. Why do women prefer home births in Ethiopia? BMC Pregnancy Childbirth 2013, 13, 5. [Google Scholar] [CrossRef]
- Wolde, H.F.; Tsegaye, A.T.; Sisay, M.M. Late initiation of antenatal care and associated factors among pregnant women in Addis Zemen primary hospital, South Gondar, Ethiopia. Reprod. Health 2019, 16, 73. [Google Scholar] [CrossRef]
- Jalu, M.T.; Ahmed, A.; Hashi, A.; Tekilu, A. Exploring barriers to reproductive, maternal, child and neonatal (RMNCH) health-seeking behaviors in Somali region, Ethiopia. PLoS ONE 2019, 14, e0212227. [Google Scholar] [CrossRef]
- Regassa, N.; Bird, Y.; Moraros, J. Preference in the use of full childhood immunizations in Ethiopia: The role of maternal health services. Patient Prefer. Adherence 2019, 13, 91–99. [Google Scholar]
- Yenit, M.K.; Gelaw, Y.A.; Shiferaw, A.M. Mothers’ health service utilization and attitude were the main predictors of incomplete childhood vaccination in east-central Ethiopia: A case-control study. Arch. Public Health 2018, 76, 14. [Google Scholar] [CrossRef]
- Hajizadeh, M. Socioeconomic inequalities in child vaccination in low/middle-income countries: What accounts for the differences? J. Epidemiol. Community Health 2018, 72, 719–725. [Google Scholar] [CrossRef]
- Ajaero, C.K.; Odimegwu, C.; Ajaero, I.D.; Nwachukwu, C.A. Access to mass media messages, and use of family planning in Nigeria: A spatio-demographic analysis from the 2013 DHS. BMC Public Health 2016, 16, 427. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, M.A.; Loken, B.; Hornik, R.C. Use of mass media campaigns to change health behaviour. Lancet 2010, 376, 1261–1271. [Google Scholar] [CrossRef]
- Kumar, A.; Mohanty, S.K. Socio-economic differentials in childhood immunization in India, 1992–2006. J. Popul. Res. 2011, 28, 301–324. [Google Scholar] [CrossRef]
- Bbaale, E. Factors influencing childhood immunization in Uganda. J. Health Popul. Nutr. 2013, 31, 118–129. [Google Scholar] [CrossRef] [PubMed]
- Abadura, S.A.; Lerebo, W.T.; Kulkarni, U.; Mekonnen, Z.A. Individual and community level determinants of childhood full immunization in Ethiopia: A multilevel analysis. BMC Public Health 2015, 15, 972. [Google Scholar] [CrossRef]
- Egondi, T.; Oyolola, M.; Mutua, M.K.; Elung’ata, P. Determinants of immunization inequality among urban poor children: Evidence from Nairobi’s informal settlements. Int. J. Equity Health 2015, 14, 24. [Google Scholar] [CrossRef]
- Ensor, T.; Cooper, S. Overcoming barriers to health service access: Influencing the demand side. Health Policy Plan. 2004, 19, 69–79. [Google Scholar] [CrossRef]
- Greenaway, E.S.; Leon, J.; Baker, D.P. Understanding the association between maternal education and use of health services in Ghana: Exploring the role of health knowledge. J. Biosoc. Sci. 2012, 44, 733–747. [Google Scholar] [CrossRef]
- Oh, J.H. Educational expansion and health disparities in Ethiopia, 2005–2016. Soc. Sci. Med. 2019, 235, 112316. [Google Scholar] [CrossRef]
- Tesema, M.T.; Braeken, J. Regional inequalities and gender differences in academic achievement as a function of educational opportunities: Evidence from Ethiopia. Int. J. Educ. Dev. 2018, 60, 51–59. [Google Scholar] [CrossRef]
- Abiy, D.S.; Kabeta, G.G.; Mihiretie, D.M. Developing a lifelong learning system in Ethiopia: Contextual considerations and propositions. Int. Rev. Educ. 2014, 60, 639–660. [Google Scholar] [CrossRef]
- Girmay, A.; Dadi, A.F. Full Immunization Coverage and Associated Factors among Children Aged 12–23 Months in a Hard-to-Reach Areas of Ethiopia. Int. J. Pediatr. 2019, 2019, 1924941. [Google Scholar] [CrossRef] [PubMed]
- Mohamud, A.N.; Feleke, A.; Worku, W.; Kifle, M.; Sharma, H.R. Immunization coverage of 12–23 months old children and associated factors in Jigjiga District, Somali National Regional State, Ethiopia. BMC Public Health 2014, 14, 865. [Google Scholar] [CrossRef] [PubMed]
- Wado, Y.D.; Afework, M.F.; Hindin, M.J. Childhood vaccination in rural southwestern Ethiopia: The nexus with demographic factors and women’s autonomy. Pan Afr. Med. J. 2014, 17, 9. [Google Scholar] [CrossRef]
- Sullivan, M.C.; Tegegn, A.; Tessema, F.; Galea, S.; Hadley, C. Minding the immunization gap: Family characteristics associated with completion rates in rural Ethiopia. J. Community Health 2010, 35, 53–59. [Google Scholar] [CrossRef]
- United Nations Children’s Fund. Building Trust in Immunization Partnering with Religious Leaders and Groups; United Nations Children’s Fund: New York, NY, USA, 2004. [Google Scholar]
- Sibeudu, F.T.; Uzochukwu, B.S.; Onwujekwe, O.E. Rural–urban comparison of routine immunization utilization and its determinants in communities in Anambra States, Nigeria. SAGE Open Med. 2019, 7, 7. [Google Scholar] [CrossRef]
- Okwaraji, Y.B.; Mulholland, K.; Schellenberg, J.; Andarge, G.; Admassu, M.; Edmond, K.M. The association between travel time to health facilities and childhood vaccine coverage in rural Ethiopia. A community based cross sectional study. BMC Public Health 2012, 12, 476. [Google Scholar] [CrossRef]
- Ndiritu, M.; Cowgill, K.D.; Ismail, A.; Chiphatsi, S.; Kamau, T.; Fegan, G.; Feikin, D.R.; Newton, C.R.; Scott, J.A.G. Immunization coverage and risk factors for failure to immunize within the Expanded Programme on Immunization in Kenya after introduction of new Haemophilus influenzae type b and hepatitis b virus antigens. BMC Public Health 2006, 6, 132. [Google Scholar] [CrossRef]
- Toikilik, S.; Tuges, G.; Lagani, J.; Wafiware, E.; Posanai, E.; Coghlan, B.; Morgan, C.; Sweeney, R.; Miller, N.; Abramov, A.; et al. Are hard-to-reach populations being reached with immunization services? Findings from the 2005 Papua New Guinea national immunization coverage survey. Vaccine 2010, 28, 4673–4679. [Google Scholar] [CrossRef]
- Jani, J.V.; De Schacht, C.; Jani, I.V.; Bjune, G. Risk factors for incomplete vaccination and missed opportunity for immunization in rural Mozambique. BMC Public Health 2008, 8, 161. [Google Scholar] [CrossRef]
- Naimoli, J.F.; Challa, S.; Schneidman, M.; Kostermans, K. Toward a grounded theory of why some immunization programmes in sub-Saharan Africa are more successful than others: A descriptive and exploratory assessment in six countries. Health Policy Plan. 2008, 23, 379–389. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mills, E.; Jadad, A.R.; Ross, C.; Wilson, K. Systematic review of qualitative studies exploring parental beliefs and attitudes toward childhood vaccination identifies common barriers to vaccination. J. Clin. Epidemiol. 2005, 58, 1081–1088. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, A.; Laxminarayan, R. Demand- and supply-side determinants of diphtheria-pertussis-tetanus nonvaccination and dropout in rural India. Vaccine 2017, 35, 1087–1093. [Google Scholar] [CrossRef] [PubMed]
- Kessels, R.; Erreygers, G. Structural equation modeling for decomposing rank-dependent indicators of socioeconomic inequality of health: An empirical study. Health Econ. Rev. 2016, 6, 56. [Google Scholar] [CrossRef]
- McKenzie, D.J. Measuring inequality with asset indicators. J. Popul. Econ. 2005, 18, 229–260. [Google Scholar] [CrossRef]
| Variable | N ‡ (%) |
|---|---|
| Sex of child | |
| Male | 926 (46.2) |
| Female | 1078 (53.8) |
| Place of Residence | |
| Rural | 1772 (88.4) |
| Urban | 232 (11.6) |
| Region | |
| Established regions | 1821 (90.9) |
| Emerging regions | 122 (6.0) |
| Addis Ababa and Dire Dawa | 62 (3.1) |
| Wealth quintile * | |
| Poorest | 504 (25.2) |
| Poorer | 396 (19.8) |
| Middle | 450 (22.4) |
| Richer | 366 (18.3) |
| Richest | 288 (14.4) |
| Determinant | Coefficient | CI | Contribution | % Contribution |
|---|---|---|---|---|
| Mother’s age in years (reference is 20–34) | 0.1 | |||
| 15–19 | −0.021 (0.0904) | −0.018 (0.0029) *** | 0.000 (0.0000) *** | 0.1 (0.0131) *** |
| 35–49 | −0.001 (0.0438) | 0.009 (0.0011) *** | 0.000 (0.0000) * | 0.0 (0.0179) * |
| Maternal educational level (reference is no education) | 9.7 | |||
| Primary | 0.084 (0.0428) | 0.104 (0.0009) *** | 0.010 (0.0002) *** | 3.8 (0.0716) *** |
| Secondary and higher | 0.069 (0.0766) | 0.744 (0.0011) *** | 0.017 (0.0006) *** | 6.2 (0.2271) *** |
| Mother’s with employment status of working | −0.006 (0.0359) | 0.075 (0.0007) *** | −0.001 (0.0002) *** | −0.2 (0.0630) *** |
| Religion (reference is Orthodox) | 6.1 | |||
| Protestant | −0.065 (0.0448) | 0.102 (0.0012) *** | −0.006 (0.0002) *** | −2.3 (0.0646) *** |
| Muslim | −0.112 (0.0421) ** | −0.140 (0.0008) *** | 0.025 (0.0003) *** | 9.3 (0.1362) *** |
| Others | 0.035 (0.1077) | −0.446 (0.0034) *** | −0.002 (0.0002) *** | −0.8 (0.0990) *** |
| Administrative regions (reference is Established regions) | 3.8 | |||
| Emerging regions | −0.027 (0.0413) | −0.439 (0.0011) *** | 0.003 (0.0001) *** | 1.0 (0.0521) *** |
| Addis Ababa and Dire Dawa | 0.074 (0.0535) | 0.836 (0.0006) *** | 0.007 (0.0002) *** | 2.8 (0.0696) *** |
| Female child | 0.004 (0.0346) | 0.020 (0.0006) *** | 0.000 (0.0001) *** | 0.1 (0.0243) *** |
| Antenatal care use | 0.179 (0.0409) *** | 0.108 (0.0005) *** | 0.049 (0.0004) *** | 18.4 (0.1700) *** |
| Institutional delivery | 0.056 (0.0433) | 0.265 (0.0008) *** | 0.021 (0.0005) *** | 8.1 (0.2098) *** |
| Urban residence | 0.040 (0.0692) | 0.735 (0.0015) *** | 0.014 (0.0007) *** | 5.3 (0.2807) *** |
| Exposure to media | 0.090 (0.0528) | 0.510 (0.0012) *** | 0.034 (0.0007) *** | 12.8 (0.2540) *** |
| Postnatal care use | 0.099 (0.0551) | 0.308 (0.0015) *** | 0.010 (0.0002) *** | 3.7 (0.0708) *** |
| A mother not considered distance to a health facility as a big problem | 0.039 (0.0360) | 0.212 (0.0007) *** | 0.013 (0.0004) *** | 4.6 (0.1486) *** |
| Partner’s educational level (reference is no education) | 1.3 | |||
| Primary | 0.020 (0.0436) | 0.057 (0.0008) *** | 0.002 (0.0001) *** | 0.8 (0.0511) *** |
| Secondary and higher | 0.004 (0.0662) | 0.583 (0.0012) *** | 0.002 (0.0006) ** | 0.5 (0.2420) * |
| Residual | 0.410 (0.0533) *** | 25.9 | ||
| ECI decomposed | 0.270 (0.0012) *** | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wondimu, A.; van der Schans, J.; van Hulst, M.; Postma, M.J. Inequalities in Rotavirus Vaccine Uptake in Ethiopia: A Decomposition Analysis. Int. J. Environ. Res. Public Health 2020, 17, 2696. https://doi.org/10.3390/ijerph17082696
Wondimu A, van der Schans J, van Hulst M, Postma MJ. Inequalities in Rotavirus Vaccine Uptake in Ethiopia: A Decomposition Analysis. International Journal of Environmental Research and Public Health. 2020; 17(8):2696. https://doi.org/10.3390/ijerph17082696
Chicago/Turabian StyleWondimu, Abrham, Jurjen van der Schans, Marinus van Hulst, and Maarten J. Postma. 2020. "Inequalities in Rotavirus Vaccine Uptake in Ethiopia: A Decomposition Analysis" International Journal of Environmental Research and Public Health 17, no. 8: 2696. https://doi.org/10.3390/ijerph17082696
APA StyleWondimu, A., van der Schans, J., van Hulst, M., & Postma, M. J. (2020). Inequalities in Rotavirus Vaccine Uptake in Ethiopia: A Decomposition Analysis. International Journal of Environmental Research and Public Health, 17(8), 2696. https://doi.org/10.3390/ijerph17082696




