Considering Health Literacy, Health Decision Making, and Health Communication in the Social Networks of Vulnerable New Mothers in Hawai‘i: A Pilot Feasibility Study
Abstract
1. Introduction
1.1. Background
1.2. Study Focus
1.3. Methodological Considerations
1.4. Specific Study Goals
2. Materials and Methods
2.1. Sampling
2.2. Measures
2.3. Analyses
3. Results
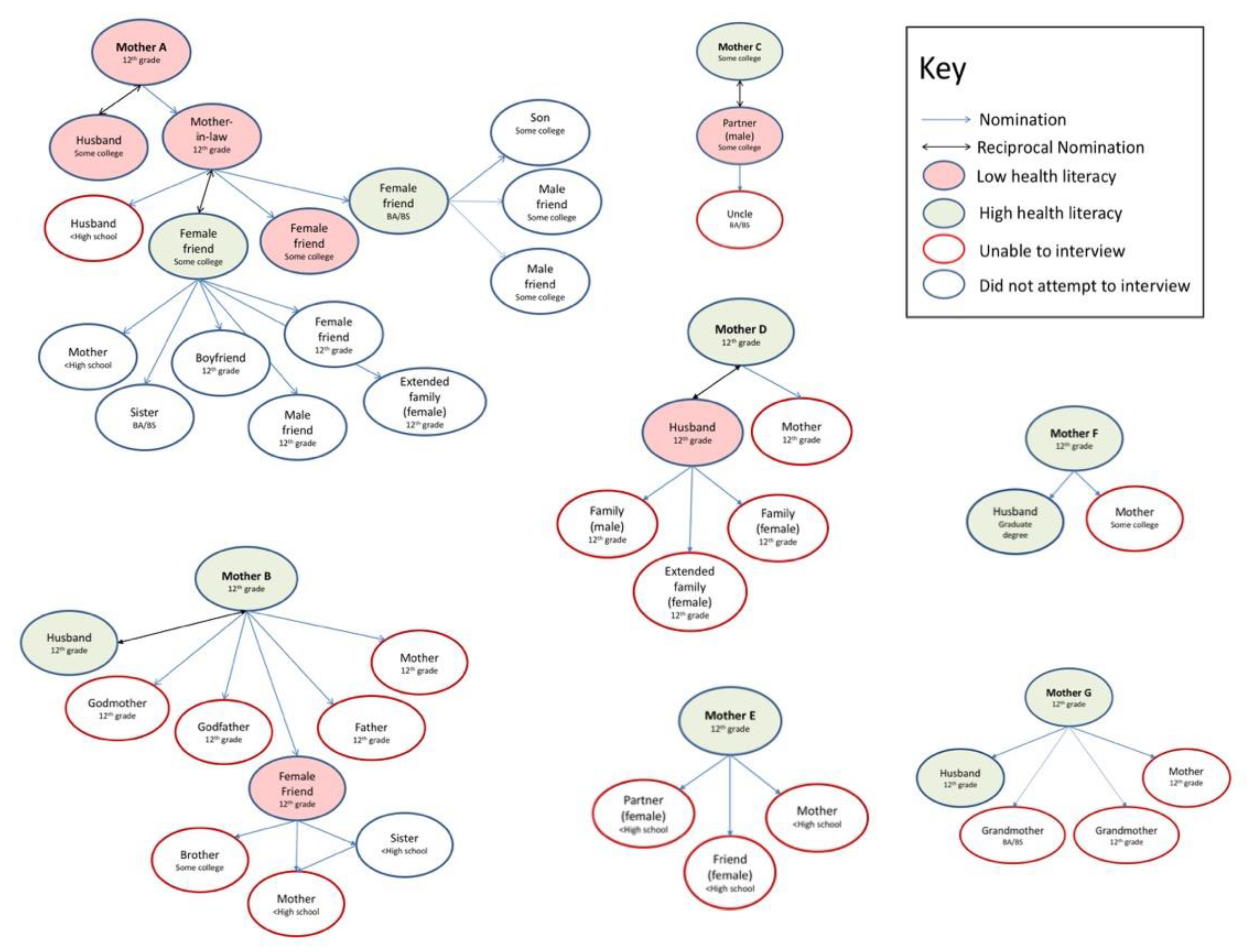
3.1. Overview of the Seven Networks
3.2. Feasibility
3.3. Characteristics of Interviewed Participants
3.4. Network Size
3.5. Rationale for Choosing Health Discussion Partners
3.6. Network Concordance by Health Literacy and Education
4. Discussion
4.1. Strategies
4.2. Considerations
4.3. Limitations and Future Studies
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ratzan, S.; Parker, R. Introduction. In National Library of Medicine Current Bibliographies in Medicine: Health Literacy; National Institutes of Health, U.S. Department of Health and Human Services: Bethesda, MD, USA, 2000. [Google Scholar]
- Sentell, T.L.; Pitt, R.; Buchthal, O.V. Health Literacy in a Social Context: Review of Quantitative Evidence. HLRP: Heal. Lit. Res. Pr. 2017, 1, e41–e70. [Google Scholar] [CrossRef]
- Lee, Y.K.; Low, W.Y.; Ng, C.J. Exploring Patient Values in Medical Decision Making: A Qualitative Study. PLoS ONE 2013, 8, e80051. [Google Scholar] [CrossRef] [PubMed]
- McKinn, S.; Linh, D.T.; Foster, K.; McCaffery, K. Distributed Health Literacy in the Maternal Health Context in Vietnam. HLRP Heal. Lit. Res. Pr. 2019, 3, e31–e42. [Google Scholar] [CrossRef] [PubMed]
- Abreu, L.; Nunes, J.A.; Taylor, P.; Silva, S. Distributed health literacy among people living with type 2 diabetes in Portugal: Defining levels of awareness and support. Heal. Soc. Care Community 2017, 26, 90–101. [Google Scholar] [CrossRef] [PubMed]
- Baker, D.W. The Meaning and the Measure of Health Literacy. J. Gen. Intern. Med. 2006, 21, 878–883. [Google Scholar] [CrossRef] [PubMed]
- Squiers, L.B.; Peinado, S.; Berkman, N.; Boudewyns, V.; McCormack, L. The Health Literacy Skills Framework. J. Heal. Commun. 2012, 17, 30–54. [Google Scholar] [CrossRef]
- Pitt, R.; Davis, T.; Manganello, J.; Massey, P.; Okan, O.; McFarlane, E.; Buchthal, O.; Davis, J.; Arnold, C.; Sentell, T. Health literacy in a social context: A meta-narrative review. In International Handbook of Health Literacy; Policy Press: Bristol, UK, 2019; pp. 665–688. ISBN 978-1-4473-4452-0. [Google Scholar]
- Pitt, R.; Davis, T.; Manganello, J.; Massey, P.; McFarlane, L.; Buchthal, V.; Davis, J.; Arnold, C.; Sentell, T.L. Health Literacy Beyond the Individual: A Meta-Narrative Review. Eur. J. Public Heal. 2017, 27, 27. [Google Scholar] [CrossRef][Green Version]
- Sentell, T.L.; Zhang, W.; Davis, J.; Baker, K.K.; Braun, K.L. The Influence of Community and Individual Health Literacy on Self-Reported Health Status. J. Gen. Intern. Med. 2013, 29, 298–304. [Google Scholar] [CrossRef]
- Nutbeam, D. The evolving concept of health literacy. Soc. Sci. Med. 2008, 67, 2072–2078. [Google Scholar] [CrossRef]
- Nutbeam, D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Heal. Promot. Int. 2000, 15, 259–267. [Google Scholar] [CrossRef]
- Latkin, C.A.; Knowlton, A.R. Social Network Assessments and Interventions for Health Behavior Change: A Critical Review. Behav. Med. 2015, 41, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.W.; Ramos, C.; Kim, K.; Azim, S.F. The Association of Racial and Ethnic Social Networks with Mental Health Service Utilization Across Minority Groups in the USA. J. Racial Ethn. Heal. Dispar. 2019, 6, 836–850. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y. Contextual effects on health care access among immigrants: Lessons from three ethnic communities in Hawaii. Soc. Sci. Med. 2009, 69, 1261–1271. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y. Seeking health care: Marshallese migrants in Hawai’i. Ethn. Heal. 2008, 13, 73–92. [Google Scholar] [CrossRef] [PubMed]
- Sentell, T.L.; Cruz, M.R.D.; Heo, H.-H.; Braun, K.L. Health literacy, health communication challenges, and cancer screening among rural native Hawaiian and Filipino women. J. Cancer Educ. 2013, 28, 325–334. [Google Scholar] [CrossRef]
- Fonseca-Becker, F.; Valente, T.W. Promoting breastfeeding in Bolivia: Do social networks add to the predictive value of traditional socioeconomic characteristics? J. Heal. Popul. Nutr. 2006, 24, 10. [Google Scholar]
- Chambers, D.; Wilson, P.; Thompson, C.; Harden, M. Social Network Analysis in Healthcare Settings: A Systematic Scoping Review. PLoS ONE 2012, 7, e41911. [Google Scholar] [CrossRef]
- Wasserman, S.; Faust, K. Social Network Analysis; Cambridge University Press: Cabridge, UK, 1994. [Google Scholar]
- Schrag, A.; Schmidt-Tieszen, A. Social Support Networks of Single Young Mothers. Child Adolesc. Soc. Work. J. 2014, 31, 315–327. [Google Scholar] [CrossRef]
- Simkhada, B.; Porter, M.; Van Teijlingen, E. The role of mothers-in-law in antenatal care decision-making in Nepal: A qualitative study. BMC Pregnancy Childbirth 2010, 10, 34. [Google Scholar] [CrossRef]
- Gayen, K.; Raeside, R. Social networks, normative influence and health delivery in rural Bangladesh. Soc. Sci. Med. 2007, 65, 900–914. [Google Scholar] [CrossRef]
- Valente, T.W. Social Networks and Health; Oxford University Press (OUP): Oxford, UK, 2010. [Google Scholar]
- VanderWeele, T.J. Sensitivity analysis for contagion effects in social networks. Sociol. Methods Res. 2011, 40, 240–255. [Google Scholar] [CrossRef] [PubMed]
- Valente, T.W.; Gallaher, P.; Mouttapa, M. Using Social Networks to Understand and Prevent Substance Use: A Transdisciplinary Perspective. Subst. Use Misuse 2004, 39, 1685–1712. [Google Scholar] [CrossRef]
- Christakis, N.A.; Fowler, J. The collective dynamics of smoking in a large social network. N. Engl. J. Med. 2008, 358, 2249–2258. [Google Scholar] [CrossRef] [PubMed]
- DeWalt, D.; Hink, A. Health Literacy and Child Health Outcomes: A Systematic Review of the Literature. Pediatrics 2009, 124, S265–S274. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, H.; Skipper, B.; Small, L.; Terry, T.; Mcgrew, M. Effect of Literacy on Breast-feeding Outcomes. South. Med. J. 2001, 94, 293–296. [Google Scholar] [CrossRef] [PubMed]
- Sanders, L.M.; Federico, S.; Klass, P.; Abrams, M.A.; Dreyer, B.P. Literacy and Child Health. Arch. Pediatr. Adolesc. Med. 2009, 163, 131. [Google Scholar] [CrossRef]
- Batterham, R.; Hawkins, M.; Collins, P.; Buchbinder, R.; Osborne, R.H. Health literacy: Applying current concepts to improve health services and reduce health inequalities. Public Heal. 2016, 132, 3–12. [Google Scholar] [CrossRef]
- Kim, Y.-C.; Lim, J.Y.; Park, K. Effects of Health Literacy and Social Capital on Health Information Behavior. J. Heal. Commun. 2015, 20, 1084–1094. [Google Scholar] [CrossRef]
- Edwards, J.B. Cultural Intelligence for Clinical Social Work Practice. Clin. Soc. Work. J. 2015, 44, 211–220. [Google Scholar] [CrossRef]
- Von Wagner, C.; Steptoe, A.; Wolf, M.S.; Wardle, J. Health Literacy and Health Actions: A Review and a Framework From Health Psychology. Heal. Educ. Behav. 2008, 36, 860–877. [Google Scholar] [CrossRef]
- Edwards, M.; Wood, F.; Davies, M.; Edwards, A. ‘Distributed health literacy’: Longitudinal qualitative analysis of the roles of health literacy mediators and social networks of people living with a long-term health condition. Heal. Expect. 2013, 18, 1180–1193. [Google Scholar] [CrossRef] [PubMed]
- Poorman, E.; Gazmararian, J.A.; Elon, L.; Parker, R.M. Is health literacy related to health behaviors and cell phone usage patterns among the text4baby target population? Arch. Public Heal 2014, 72, 13. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mynarska, M.; Riederer, B.; Jaschinski, I.; Krivanek, D.; Neyer, G.; Oláh, L. Vulnerability of Families with Children: Major Risks, Future Challenges and Policy Recommendations. Available online: http://www.familiesandsocieties.eu/wp-content/uploads/2015/11/WP49MynarskaEtAl2015.pdf (accessed on 26 March 2020).
- Esposito, T.; Delaye, A.; Chabot, M.; Trocmé, N.; Rothwell, D.; Hélie, S.; Robichaud, M.-J. The Effects of Socioeconomic Vulnerability, Psychosocial Services, and Social Service Spending on Family Reunification: A Multilevel Longitudinal Analysis. Int. J. Environ. Res. Public Health 2017, 14, 1040. [Google Scholar] [CrossRef] [PubMed]
- Breiner, H.; Ford, M.; Gadsden, V.L.; National Academies of Sciences, Engineering, and Medicine. Parenting Knowledge, Attitudes, and Practices. In Parenting Matters: Supporting Parents of Children Ages 0–8; Breiner, H., Ford, M., Gadsden, V.L., Eds.; National Academies Press: Washington, DC, USA, 2016. [Google Scholar]
- Porr, C.; Drummond, J.; Richter, S. Health literacy as an empowerment tool for low-income mothers. Fam. Community Health 2006, 29, 328–335. [Google Scholar] [CrossRef]
- Valdovinos D’Angelo, A.; Knas, E.; Holcomb, P.; Edin, K. The Role of Social Networks Among Low-Income Fathers: Findings from the PACT Evaluation; Findings from the PACT Evaluation. OPRE Report Number 2016-60; Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services: Washington, DC, USA, 2016.
- Kaholokula, J.K.; Ing, C.T.; Look, M.A.; Delafield, R.; Sinclair, K. Culturally responsive approaches to health promotion for Native Hawaiians and Pacific Islanders. Ann. Hum. Boil. 2018, 45, 249–263. [Google Scholar] [CrossRef]
- Williams, A.D.; Messer, L.C.; Kanner, J.; Ha, S.; Grantz, K.L.; Mendola, P. Ethnic Enclaves and Pregnancy and Behavior Outcomes Among Asian/Pacific Islanders in the USA. J. Racial Ethn. Health Dispar. 2019, 7, 224–233. [Google Scholar] [CrossRef]
- King, G.L.; McNeely, M.J.; Thorpe, L.E.; Mau, M.L.; Ko, J.; Liu, L.L.; Sun, A.; Hsu, W.C.; Chow, E.A. Understanding and Addressing Unique Needs of Diabetes in Asian Americans, Native Hawaiians, and Pacific Islanders. Diabetes Care 2012, 35, 1181–1188. [Google Scholar] [CrossRef]
- Wu, Y.; Braun, K.; Onaka, A.T.; Horiuchi, B.Y.; Tottori, C.J.; Wilkens, L. Life Expectancies in Hawai‘i: A Multi-ethnic Analysis of 2010 Life Tables. J. Asia Pac. Med. Public Health 2010, 76, 9–14. [Google Scholar]
- Uchima, O.; Wu, Y.Y.; Browne, C.; Braun, K.L. Disparities in Diabetes Prevalence Among Native Hawaiians/Other Pacific Islanders and Asians in Hawai‘i. Prev. Chronic Dis. 2019, 16, E22. [Google Scholar] [CrossRef]
- Look, M.; Trask-Batti, M.; Agres, R.; Mau, M.; Kaholokula, J. Assessment and Priorities for Health & Well-Being in Native Hawaiians & Other Pacific Peoples; Center for Native and Pacific Islander Research: Honolulu, HI, USA, 2013. [Google Scholar]
- Sentell, T.L.; Seto, T.B.; Young, M.M.; Vawer, M.; Quensell, M.L.; Braun, K.L.; Taira, D. Pathways to potentially preventable hospitalizations for diabetes and heart failure: A qualitative analysis of patient perspectives. BMC Health Serv. Res. 2016, 16, 300. [Google Scholar] [CrossRef]
- Abesamis, C.J.; Fruh, S.; Hall, H.; Lemley, T.; Zlomke, K. Cardiovascular Health of Filipinos in the United States: A Review of the Literature. J. Transcult. Nurs. 2015, 27, 518–528. [Google Scholar] [CrossRef] [PubMed]
- Malabed, J.M.; Taira, D.A.; Seto, T.B.; Braun, K.L.; Sentell, T. 2017 Writing Contest Undergraduate Winner: Pathways to Preventable Hospitalizations for Filipino Patients with Diabetes and Heart Disease in Hawai‘i. Hawaii J. Med. Public. Health 2018, 77, 155–160. [Google Scholar] [PubMed]
- Christakis, N.A.; Fowler, J. The Spread of Obesity in a Large Social Network over 32 Years. N. Engl. J. Med. 2007, 357, 370–379. [Google Scholar] [CrossRef] [PubMed]
- Parikh, N.S.; Parker, R.M.; Nurss, J.R.; Baker, D.W.; Williams, M.V. Shame and health literacy: The unspoken connection. Patient Educ. Couns. 1996, 27, 33–39. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Health Literacy. Health Literacy: A Prescription to End Confusion; Nielsen-Bohlman, L., Panzer, A.M., Kindig, D.A., Eds.; National Academies Press: Washington, DC, USA, 2004; ISBN 978-0-309-09117-6. [Google Scholar]
- Berkman, N.D.; Donahue, K.E.; Halpern, D.J.; Crotty, K.; Sheridan, S.L. Low Health Literacy and Health Outcomes: An Updated Systematic Review. Ann. Intern. Med. 2011, 155, 97. [Google Scholar] [CrossRef]
- Robins, G. Doing Social Network Research: Network-Based Research Design for Social Scientists; SAGE: Thousand Oaks, CA, USA, 2015. [Google Scholar]
- Sadler, G.R.; Lee, H.-C.; Seung-Hwan Lim, R.; Fullerton, J. Recruiting hard-to-reach United States population sub-groups via adaptations of snowball sampling strategy. Nurs. Health Sci. 2010, 12, 369–374. [Google Scholar] [CrossRef]
- Department of Health and Human Services. What is Home Visiting Evidence of Effectiveness? Home Visiting Evidence of Effectiveness. Available online: https://homvee.acf.hhs.gov/ (accessed on 29 January 2020).
- HRSA Maternal & Child Health Hawaii’s MIECHV Program FY; Congressional Research Service: Washington, DC, USA, 2018.
- Kelly, L.A.; Patel, S.A.; Narayan, K.M.V.; Prabhakaran, D.; Cunningham, S.A. Measuring Social Networks for Medical Research in Lower-Income Settings. PLoS ONE 2014, 9. [Google Scholar] [CrossRef]
- Heijmans, N.; Van Lieshout, J.; Wensing, M. Social networks of health care providers and patients in cardiovascular risk management: A study protocol. BMC Health Serv. Res. 2014, 14, 265. [Google Scholar] [CrossRef]
- Valente, T.W.; Saba, W.P. Mass Media and Interpersonal Influence in a Reproductive Health Communication Campaign in Bolivia. Commun. Res. 1998, 25, 96–124. [Google Scholar] [CrossRef]
- Zhang, S.; Xiang, W. Income gradient in health-related quality of life—The role of social networking time. Int. J. Equity Health 2019, 18, 44. [Google Scholar] [CrossRef]
- Cornwell, E.Y.; Cornwell, B. Access to Expertise as a Form of Social Capital: An Examination of Race- and Class-Based Disparities in Network Ties to Experts. Sociol. Perspect. 2008, 51, 853–876. [Google Scholar] [CrossRef]
- Mechanic, D.; Tanner, J. Vulnerable People, Groups, And Populations: Societal View. Health Aff. 2007, 26, 1220–1230. [Google Scholar] [CrossRef] [PubMed]
- Groot, W.; Brink, H.M.V.D.; Van Praag, B. The Compensating Income Variation of Social Capital. Soc. Indic. Res. 2006, 82, 189–207. [Google Scholar] [CrossRef]
- Perrier, M.-J.; Ginis, K.A.M. Changing health-promoting behaviours through narrative interventions: A systematic review. J. Heal. Psychol. 2016, 23, 1499–1517. [Google Scholar] [CrossRef]
- Sentell, T.L.; Kennedy, F.; Seto, T.; Vawer, M.; Chiriboga, G.; Valdez, C.; Garrett, L.M.; Paloma, D.; Taira, D. Sharing the Patient Experience: A “Talk Story” Intervention for Heart Failure Management in Native Hawaiians. J. Patient Exp. 2019. [Google Scholar] [CrossRef]
- Volandes, A.E.; Paasche-Orlow, M.K.; Davis, A.D.; Eubanks, R.; El-Jawahri, A.; Seitz, R. Use of Video Decision Aids to Promote Advance Care Planning in Hilo, Hawai’i. J. Gen. Intern. Med. 2016, 31, 1035–1040. [Google Scholar] [CrossRef]
- Sentell, T.L.; Baker, K.K.; Onaka, A.; Braun, K. Low Health Literacy and Poor Health Status in Asian Americans and Pacific Islanders in Hawai’i. J. Health Commun. 2011, 16, 279–294. [Google Scholar] [CrossRef]
- Bourdieu, P. The social space and the genesis of groups. Theory Soc. 1985, 14, 723–744. [Google Scholar] [CrossRef]
- Ferlander, S. The Importance of Different Forms of Social Capital for Health. Acta Sociol. 2007, 50, 115–128. [Google Scholar] [CrossRef]
- Berkman, L.F.; Glass, T.; Brissette, I.; Seeman, T. From social integration to health: Durkheim in the new millennium. Soc. Sci. Med. 2000, 51, 843–857. [Google Scholar] [CrossRef]
- De Leon, C.F.M.; Seeman, T.E.; Baker, D.I.; Richardson, E.D.; Tinetti, M.E. Self-efficacy, Physical Decline, and Change in Functioning in Community-Living Elders: A Prospective Study. J. Gerontol. Ser. B 1996, 51, S183–S190. [Google Scholar] [CrossRef] [PubMed]
- Cacioppo, J.T.; Fowler, J.; Christakis, N.A. Alone in the crowd: The structure and spread of loneliness in a large social network. J. Pers. Soc. Psychol. 2009, 97, 977–991. [Google Scholar] [CrossRef] [PubMed]
- Umberson, D.; Montez, J.K. Social relationships and health: A flashpoint for health policy. J. Heal. Soc. Behav. 2010, 51, S54–S66. [Google Scholar] [CrossRef] [PubMed]
- Field, J. Social Capital, Key Ideas; Routledge: London, UK, 2003. [Google Scholar]
- Perry, B.L.; Pescosolido, B.A. Social network activation: The role of health discussion partners in recovery from mental illness. Soc. Sci. Med. 2014, 125, 116–128. [Google Scholar] [CrossRef] [PubMed]
- Shakya, H.; Hughes, D.A.; Stafford, D.; Christakis, N.A.; Fowler, J.; Silverman, J.G. Intimate partner violence norms cluster within households: An observational social network study in rural Honduras. BMC Public Health 2016, 16, 233. [Google Scholar] [CrossRef]
- Banks, I. No Man’s Land: Men, Illness, and the NHS. BMJ 2001, 323, 1058–1060. [Google Scholar] [CrossRef]
- Wang, Y.; Hunt, K.; Nazareth, I.; Freemantle, N.; Petersen, I. Do men consult less than women? An analysis of routinely collected UK general practice data. BMJ Open 2013, 3, e003320. [Google Scholar] [CrossRef]
- Magnussen, L.; Shoultz, J.; Iannce-Spencer, C.; Braun, K.L. Testing a Talkstory Intervention to create Supportive and Safe Violence-Free Communities for Women. Hawai’i J. Med. Public Health J. Asia Pac. Med. Public Health 2019, 78, 169–174. [Google Scholar]
- Horowitz, C.; Lawlor, E. Community Approaches to Addressing Health Disparities—Challenges and Successes in Reducing Health Disparities—NCBI Bookshelf. In Challenges and Successes in Reducing Health Disparities: Workshop Summary; National Academies Press: Washington, DC, USA, 2008. [Google Scholar]
- Stovell, D.; Morrison, A.P.; Panayiotou, M.; Hutton, P. Shared treatment decision-making and empowerment-related outcomes in psychosis: Systematic review and meta-analysis. Br. J. Psychiatr. 2016, 209, 23–28. [Google Scholar] [CrossRef]
- Agner, J.; Braun, K.L. Patient empowerment: A critique of individualism and systematic review of patient perspectives. Patient Educ. Couns. 2018, 101, 2054–2064. [Google Scholar] [CrossRef]
- Pattien, E. Who Is Multiracial? Depends on How You Ask: Estimates of Multiracial Adults and Other Racial and Ethnic Groups Across Various Question Formats; Pew Research Center: Washington, DC, USA, 2015. [Google Scholar]
- Office of Hawaiian Affairs. Native Hawaiian Data Book: Racial-Ethnic Identification; Office of Hawaiian Affairs: Honolulu, HI, USA, 2019. [Google Scholar]
- McPherson, M.; Smith-Lovin, L.; Cook, J.M. Birds of a Feather: Homophily in Social Networks. Annu. Rev. Sociol. 2001, 27, 415–444. [Google Scholar] [CrossRef]
| Mothers | Interviewed Alters (Levels 1 and 2) | Non-Interviewed Alters (Levels 1 and 2) | |
|---|---|---|---|
| Participants (N = 31) | 7 | 11 | 20 |
| Percent Interviewed | 100% | 36% | |
| Education | n (%) | n (%) | n (%) |
| Less than HS | 0 (0) | 1 (9.1) | 5 (25.0) |
| High School Graduate | 7 (100) | 8 (72.7) | 11 (55.0) |
| Some College or Higher | 0 (0) | 2 (18.2) | 4 (20.0) |
| Gender | |||
| Female | 7 (100) | 6 (54.6) | 13 (65) |
| Male | 0 (0) | 5 (45.5) | 7 (35) |
| Mothers | Interviewed Alters (Levels 1 and 2) | |
|---|---|---|
| Participants | 7 | 11 |
| n (%) | n (%) | |
| Self-Reported Health Literacy (“How confident do you feel filling out medical forms?”) | ||
| Low (Not at all, A little bit, or Somewhat) | 1 (14) | 6 (55) |
| Adequate (Quite a bit or Extremely) | 6 (86) | 5 (45) |
| Ethnicity | ||
| Native Hawaiian | 4 (57) | 3 (27) |
| Filipino | 1 (14) | 3 (27) |
| Puerto Rican Mix | 2 (28) | 0 |
| Samoan/Tongan | 0 | 1 (9) |
| Japanese | 0 | 1 (9) |
| Other Pacific Islander | 0 | 3 (27) |
| Mean (SD) | Mean (SD) | |
| Age | 27 (3) | 31 (9) |
| Health Literacy Self-Reported | Education Self-Reported |
|---|---|
| Low | Grades 12 or GED |
| Adequate | Grades 12 or GED |
| Adequate | Grades 12 or GED |
| Adequate | Grades 12 or GED |
| Adequate | Grades 12 or GED |
| Adequate | Grades 12 or GED |
| Adequate | Grades 12 or GED |
| Low | College 1 to 3 yrs |
| Low | College 1 to 3 yrs |
| Adequate | College 1 to 3 yrs |
| Low | College 1 to 3 yrs |
| Adequate | Bachelor’s Degree |
| Low | Grades 12 or GED |
| Low | Grades 12 or GED |
| Adequate | Graduate degree |
| Adequate | Grades 12 or GED |
| Low | Grades 12 or GED |
| Adequate | Grades 9 thru 11 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sentell, T.; Agner, J.; Pitt, R.; Davis, J.; Guo, M.; McFarlane, E. Considering Health Literacy, Health Decision Making, and Health Communication in the Social Networks of Vulnerable New Mothers in Hawai‘i: A Pilot Feasibility Study. Int. J. Environ. Res. Public Health 2020, 17, 2356. https://doi.org/10.3390/ijerph17072356
Sentell T, Agner J, Pitt R, Davis J, Guo M, McFarlane E. Considering Health Literacy, Health Decision Making, and Health Communication in the Social Networks of Vulnerable New Mothers in Hawai‘i: A Pilot Feasibility Study. International Journal of Environmental Research and Public Health. 2020; 17(7):2356. https://doi.org/10.3390/ijerph17072356
Chicago/Turabian StyleSentell, Tetine, Joy Agner, Ruth Pitt, James Davis, Mary Guo, and Elizabeth McFarlane. 2020. "Considering Health Literacy, Health Decision Making, and Health Communication in the Social Networks of Vulnerable New Mothers in Hawai‘i: A Pilot Feasibility Study" International Journal of Environmental Research and Public Health 17, no. 7: 2356. https://doi.org/10.3390/ijerph17072356
APA StyleSentell, T., Agner, J., Pitt, R., Davis, J., Guo, M., & McFarlane, E. (2020). Considering Health Literacy, Health Decision Making, and Health Communication in the Social Networks of Vulnerable New Mothers in Hawai‘i: A Pilot Feasibility Study. International Journal of Environmental Research and Public Health, 17(7), 2356. https://doi.org/10.3390/ijerph17072356





