Dental Practice Integration into Primary Care: A Microsimulation of Financial Implications for Practices
Abstract
1. Introduction
2. Materials and Methods
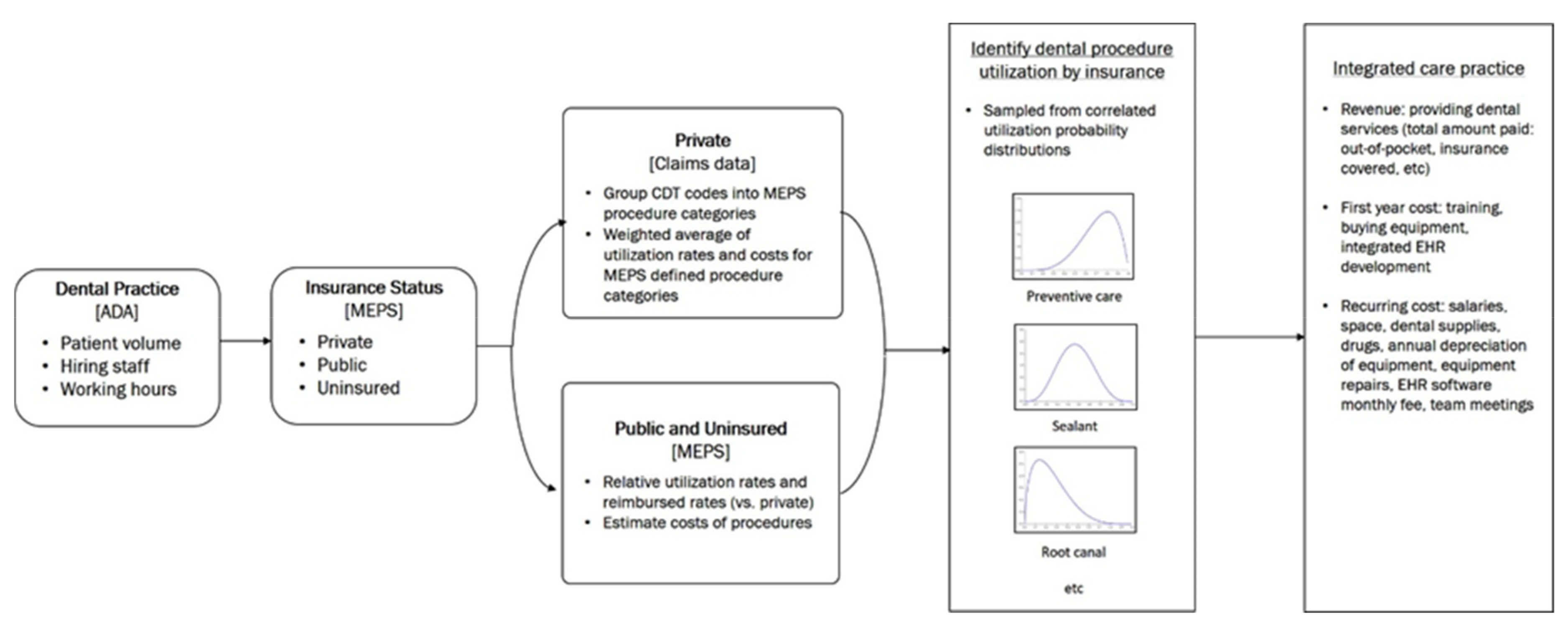
2.1. Study Design
2.2. Model Assumption
2.3. Data Sources
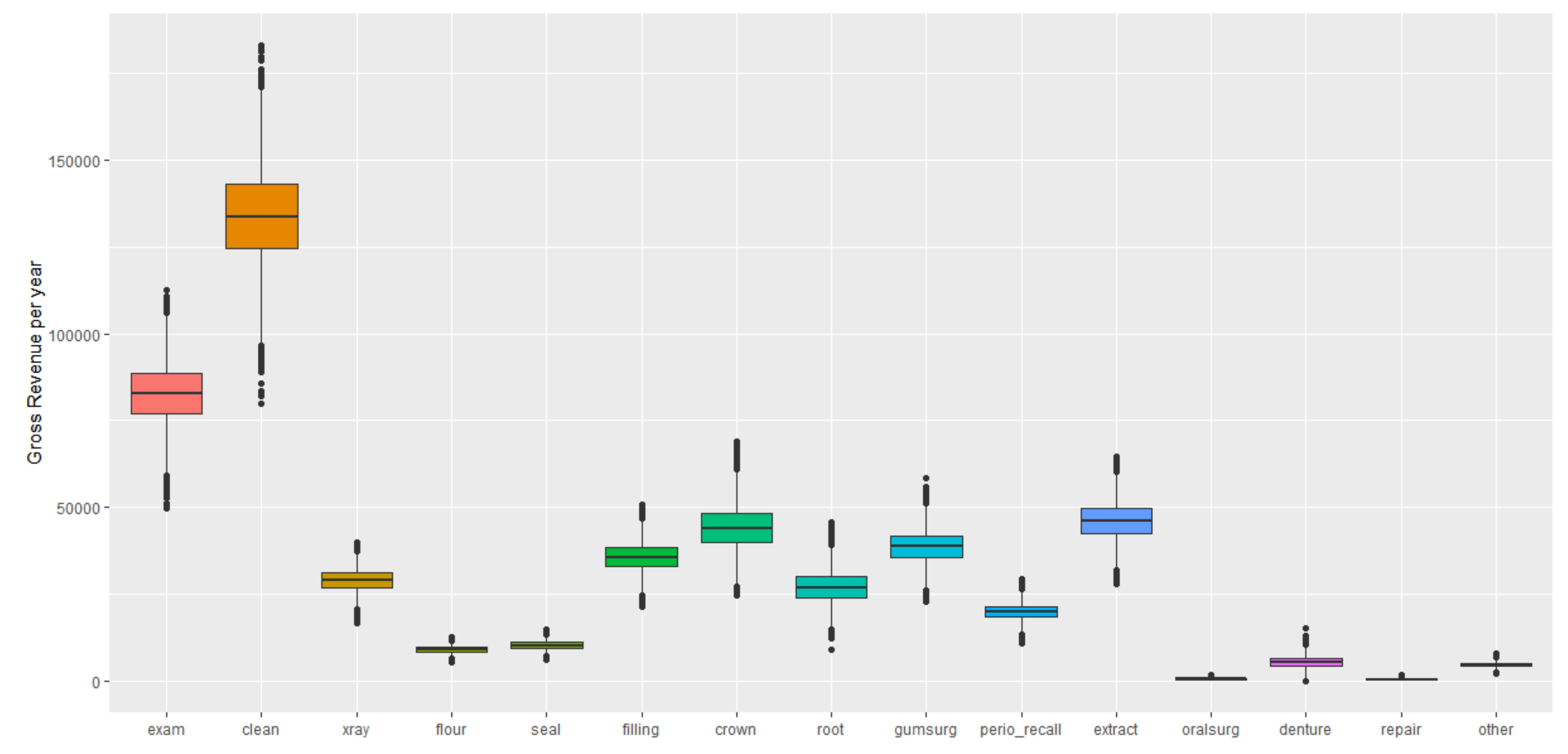
2.4. Cost and Revenue Estimates from Dental–Medical Integration
2.5. Primary and Secondary Outcome Metrics
2.6. Sensitivity Analyses
3. Results
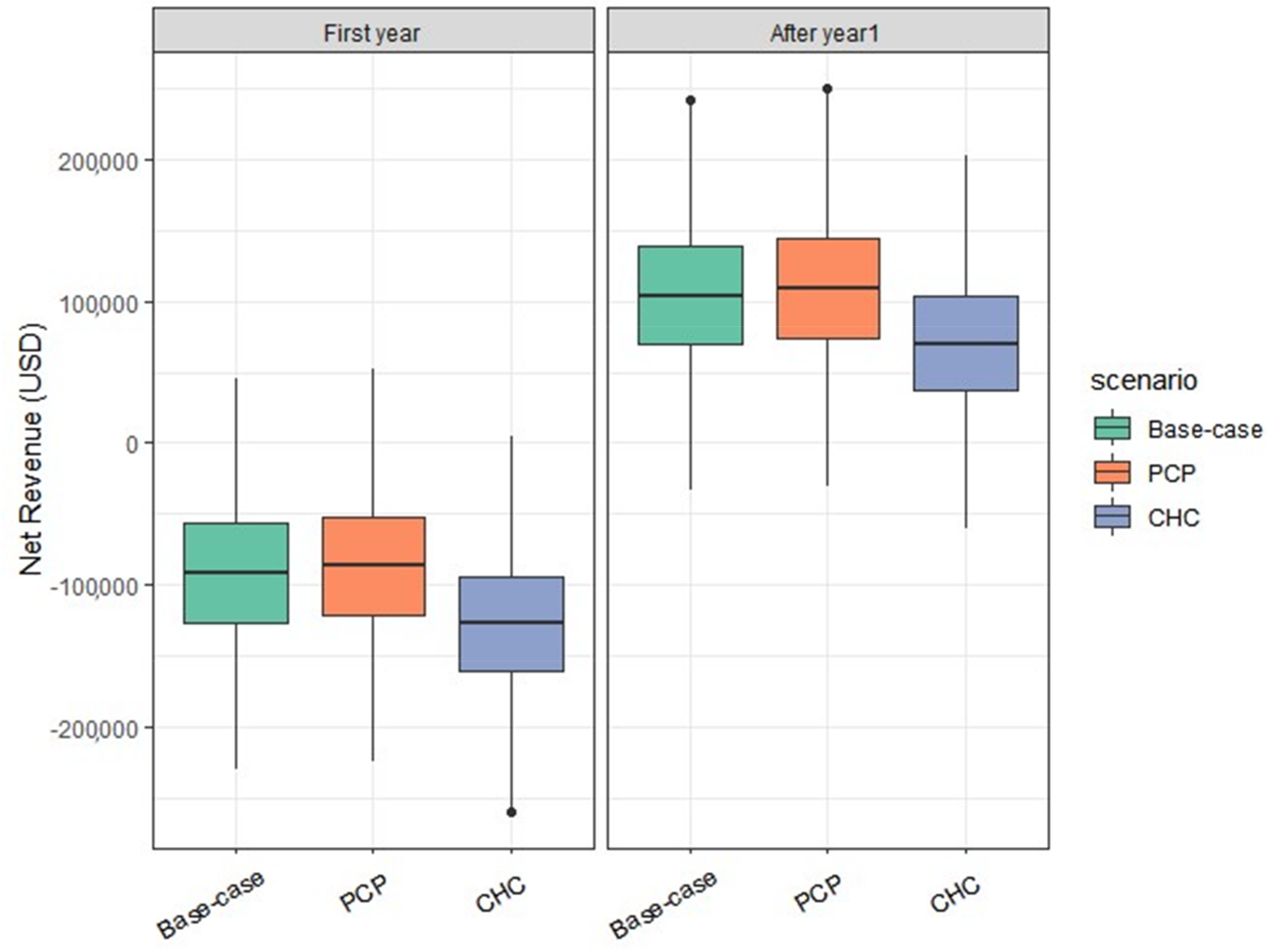
3.1. Base-Case Analyses
3.2. Sensitivity Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Simon, L. Overcoming Historical Separation between Oral and General Health Care: Interprofessional Collaboration for Promoting Health Equity. AMA J. Ethics 2016, 18, 941–949. [Google Scholar] [CrossRef] [PubMed]
- Mayo Clinic. Oral Health: A Window to Your Overall Health. Available online: https://www.mayoclinic.org/healthy-lifestyle/adult-health/in-depth/dental/art-20047475 (accessed on 31 March 2019).
- Dietrich, T.; Webb, I.; Stenhouse, L.; Pattni, A.; Ready, D.; Wanyonyi, K.L.; White, S.; Gallagher, J.E. Evidence summary: the relationship between oral and cardiovascular disease. Br. Dent. J. 2017, 222, 381–385. [Google Scholar] [CrossRef] [PubMed]
- Kholy, K.E.; Genco, R.J.; Van Dyke, T.E. Oral infections and cardiovascular disease. Trends Endocrinol. Metab. 2015, 26, 315–321. [Google Scholar] [CrossRef] [PubMed]
- Preshaw, P.M.; Alba, A.L.; Herrera, D.; Jepsen, S.; Konstantinidis, A.; Makrilakis, K.; Taylor, R. Periodontitis and diabetes: a two-way relationship. Diabetologia 2012, 55, 21–31. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine. Advancing Oral Health in America. Available online: https://www.hrsa.gov/sites/default/files/publichealth/clinical/oralhealth/advancingoralhealth.pdf (accessed on 1 August 2019).
- Institute of Medicine. Improving Access to Oral Health Care for Vulnerable and Underserved Populations. Available online: https://www.hrsa.gov/sites/default/files/publichealth/clinical/oralhealth/improvingaccess.pdf (accessed on 16 March 2019).
- Choi, S.E.; Sima, C.; Pandya, A. Impact of Treating Oral Disease on Preventing Vascular Diseases: A Model-Based Cost-effectiveness Analysis of Periodontal Treatment Among Patients With Type 2 Diabetes. Diabetes Care 2019. [Google Scholar] [CrossRef] [PubMed]
- American Dental Association. Dental Care in Accountable Care Organizations: Insights from 5 Case Studies. Available online: http://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_0615_1.ashx (accessed on 29 March 2019).
- American Dental Association. Dental Care Within Accountable Care Organizations: Challenges and Opportunities. Available online: http://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIBrief_0316_2.pdf (accessed on 29 March 2019).
- Jones, J.A.; Snyder, J.J.; Gesko, D.S.; Helgeson, M.J. Integrated Medical-Dental Delivery Systems: Models in a Changing Environment and Their Implications for Dental Education. J. Dent. Educ. 2017, 81, eS21–eS29. [Google Scholar] [CrossRef] [PubMed]
- Centers for Medicare & Medicaid Services. EHR Incentive Programs in 2015 through 2017 Health Information Exchange. Available online: https://nam.edu/integration-of-oral-health-and-primary-care-communication-coordination-and-referral/ (accessed on 25 March 2019).
- Farhad, S.Z.; Amini, S.; Khalilian, A.; Barekatain, M.; Mafi, M.; Barekatain, M.; Rafei, E. The effect of chronic periodontitis on serum levels of tumor necrosis factor-alpha in Alzheimer disease. Dent. Res. J. 2014, 11, 549–552. [Google Scholar]
- McKernan, S.C.; Kuthy, R.A.; Reynolds, J.C.; Tuggle, L.; Garcia, D.T. Medical-Dental Integration in Public Health Settings: An Environmental Scan. Available online: http://ppc.uiowa.edu/sites/default/files/ced_environmental_scan.pdf (accessed on 21 October 2019).
- Crall, J.J.; Pourat, N.; Inkelas, M.; Lampron, C.; Scoville, R. Improving The Oral Health Care Capacity Of Federally Qualified Health Centers. Health Aff. 2016, 35, 2216–2223. [Google Scholar] [CrossRef] [PubMed]
- Colorado Medical-Dental Integration Project. One Year Highlights: Colorado Medical-Dental Integration Project. Available online: https://www.deltadentalcofoundation.org/wp-content/uploads/COMDI_Handout_web.pdf (accessed on 20 March 2019).
- Crall, J.J.; Illum, J.; Martinez, A.; Pourat, N. An Innovative Project Breaks Down Barriers to Oral Health Care for Vulnerable Young Children in Los Angeles County. UCLA Health Policy Res 2016, PB2016-5. 1–8. [Google Scholar]
- Basu, S.; Landon, B.E.; Williams, J.W., Jr.; Bitton, A.; Song, Z.; Phillips, R.S. Behavioral Health Integration into Primary Care: A Microsimulation of Financial Implications for Practices. J. Gen. Intern. Med. 2017, 32, 1330–1341. [Google Scholar] [CrossRef] [PubMed]
- Briggs, A.H.; Weinstein, M.C.; Fenwick, E.A.; Karnon, J.; Sculpher, M.J.; Paltiel, A.D. Model parameter estimation and uncertainty analysis: A report of the ISPOR-SMDM Modeling Good Research Practices Task Force Working Group-6. Med. Decis. Mak. 2012, 32, 722–732. [Google Scholar] [CrossRef] [PubMed]
- Robert, C.P.; Casella, G. Introducing Monte Carlo Methods with R; Springer Verlag: New York, NY, USA, 2009. [Google Scholar]
- American Dental Association. Characteristics of Private Dental Practices: Selected 2017 Results from the Survey of Dental Practice. Available online: https://www.ada.org/en/science-research/health-policy-institute/data-center/dental-practice (accessed on 20 March 2019).
- Agency for Healthcare Research and Quality. Medical Expenditure Panel Survey. Available online: https://www.meps.ahrq.gov/mepsweb/ (accessed on 20 March 2019).
- Bureau of Labor Statistics. Occupational Outlook Handbook. Available online: https://www.bls.gov/ooh/ (accessed on 22 March 2019).
- Medical Group Management Association. DataDive. Available online: https://www.mgma.com/data (accessed on 23 March 2019).
- American Dental Association. Survey of Dental Practice (Annual Expenses of Operating a Private Practice). Available online: https://success.ada.org/en/practice-management/survey-of-dental-practice (accessed on 22 March 2019).
- Delta Dental. Improving Oral Health by Integrating Medical and Dental Care—EMR/EDR. Available online: http://medicaldentalintegration.org/building-mdi-models/building-co-mdi-space/ehredr/ (accessed on 5 December 2019).
- American Dental Association. The Real Cost of Owning a Dental Practice. Available online: http://marketplace.ada.org/blog/the-real-cost-of-owning-a-dental-practice/ (accessed on 20 March 2019).
- Liu, C.F.; Rubenstein, L.V.; Kirchner, J.E.; Fortney, J.C.; Perkins, M.W.; Ober, S.K.; Pyne, J.M.; Chaney, E.F. Organizational cost of quality improvement for depression care. Health Serv. Res. 2009, 44, 225–244. [Google Scholar] [CrossRef] [PubMed]
- Silk, H.; Sachs Leicher, E.; Alvarado, V.; Cote, E.; Cote, S. A multi-state initiative to implement pediatric oral health in primary care practice and clinical education. J. Public Health Dent. 2018, 78, 25–31. [Google Scholar] [CrossRef] [PubMed]
- The Physicians Foundation. Survey of America’s Physician. Available online: https://physiciansfoundation.org/wp-content/uploads/2018/09/physicians-survey-results-final-2018.pdf (accessed on 24 April 2019).
- American Dental Association. Code on Dental Procedures and Nomenclature (CDT Code). Available online: https://www.ada.org/en/publications/cdt (accessed on 20 March 2019).
- Maryland Department of Health. Maryland Medicaid Dental Fee Schedule and Procedure Codes. Available online: https://mmcp.health.maryland.gov/Documents/2018%20CDT%20Fee%20Schedule%20FINAL%20 (accessed on 14 December 2019).
- American Dental Association. Income, Gross Billings, and Expenses: Selected 2017 Results from the Survey of Dental Practice. Available online: https://www.ada.org/en/science-research/health-policy-institute/dental-statistics/income-billing-and-other-dentistry-statistics (accessed on 20 March 2019).
- American Dental Association. Employment of Dental Practice Personnel: Selected 2013 Results from the Survey of Dental Practice. Available online: https://www.ada.org/en/science-research/health-policy-institute/data-center/dental-practice (accessed on 2 April 2019).
- Florida Blue Dental. Oral Health for Overall Health. Available online: https://www.floridabluedental.com/members/oral-health-for-overall-health/ (accessed on 12 February 2019).
- United Concordia Dental. Smile for Health—Wellness. Available online: https://www.unitedconcordia.com/dental-insurance/employer/dental-plans/innovative-solutions-dental-plans/product-smile-for-health-wellness/ (accessed on 12 February 2019).
- Delta Dental. SmileWay Wellness Benefits. Available online: https://www.deltadentalins.com/individuals/guidance/smileway-wellness-benefits.html (accessed on 12 February 2019).
- American Dental Association. Supply and Profile of Dentists. Available online: https://www.ada.org/en/science-research/health-policy-institute/data-center/supply-and-profile-of-dentists (accessed on 30 March 2019).
- National Association of Community Health Centers. Community Health Center Chartbook. Available online: http://www.nachc.org/wp-content/uploads/2017/06/Chartbook2017.pdf (accessed on 20 April 2019).
- Gillis. K.D. Physicians’ Patient Mix—A Snapshot from the 2016 Benchmark Survey and Changes Associated with the ACA. Available online: https://www.ama-assn.org/sites/ama-assn.org/files/corp/media-browser/public/health-policy/PRP-2017-physician-benchmark-survey-patient-mix.pdf (accessed on 22 March 2020).
- Kalenderian, E.; Halamka, J.D.; Spallek, H. An EHR with Teeth. Appl. Clin. Inform. 2016, 7, 425–429. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tan, K.B.; Earn Lee, C. Integration of Primary Care with Hospital Services for Sustainable Universal Health Coverage in Singapore. Health Syst. Reform 2019, 5, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Alvarez, C.; Sanz, M.; Berthold, P. Basic sciences education in the dental curriculum in Southern Europe. Eur. J. Dent. Educ. 2001, 5, 63–66. [Google Scholar] [CrossRef] [PubMed]
- Nasseh, K.; Vujicic, M.; Glick, M. The Relationship between Periodontal Interventions and Healthcare Costs and Utilization. Evidence from an Integrated Dental, Medical, and Pharmacy Commercial Claims Database. Health Econ. 2017, 26, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Jeffcoat, M.K.; Jeffcoat, R.L.; Gladowski, P.A.; Bramson, J.B.; Blum, J.J. Impact of periodontal therapy on general health: Evidence from insurance data for five systemic conditions. Am. J. Prev. Med. 2014, 47, 166–174. [Google Scholar] [CrossRef] [PubMed]
- Centers for Medicare & Medicaid Services. Medicaid Analytic eXtract (MAX) Chartbooks. Available online: https://www.cms.gov/Research-Statistics-Data-and-Systems/Computer-Data-and-Systems/MedicaidDataSourcesGenInfo/MAX_Chartbooks.html (accessed on 29 March 2019).
| Parameters | Value | Source |
|---|---|---|
| Practice/patient characteristics | ||
| Number of patient visits per dentist (including hygienist appointment) per year | 3415 (347) | ADA HPI [21] |
| Number of patient visits per dentist (excluding hygienist appointment) per year | 1831 (127) | ADA HPI [21] |
| Number of patient visits per hour | 2.3 | ADA HPI [21] |
| Number of hours spent on patient visits per day | 6.1 | ADA HP I[21] |
| Health insurance payer distribution of overall population (proportion with dental insurance in each group) | MEPS [22] | |
| Private | 0.66 (0.01) [0.69 (0.01)] | |
| Public | 0.25 (0.01) [0.02 (0.01)] | |
| Uninsured | 0.08 (0.01) [0.04 (0.01)] | |
| Dental insurance payer distribution | MEPS [22] | |
| Private | 0.52 (0.05) | |
| Public | 0.19 (0.03) | |
| Uninsured | 0.29 (0.01) | |
| Utilization rates | ||
| CDT procedure level utilization rate (privately insured) | Supplementary Table S1 | Aetna Warehouse |
| Relative scales of utilization rates (public and uninsured) | Supplementary Table S1 | MEPS [22] |
| Costs of dental procedures | ||
| CDT procedure level costs (privately insured) | Supplementary Table S2 | Aetna Warehouse |
| Reimbursement rates relative to private insurance | Supplementary Table S3 | MEPS [22] |
| Expenses | ||
| Dentist salary | 152,210 (20,830) | ADA HPI [21] |
| Hygienist | 74,070 (12,680) | Bureau of Labor Statistics [23] |
| Chairside assistant | 37,630 (6870) | Bureau of Labor Statistics [23] |
| Primary care physician (hourly) | $98 (7) | MGMA [24] |
| Medical Assistant (hourly) | $15.1(2) | Bureau of Labor Statistics [23] |
| Recurring costs | ||
| Clinical space | $1014 (290) | MGMA [24] |
| Dental supplies | 6.4% of gross billing | ADA [25] |
| Drugs | 0.3% of gross billing | ADA [25] |
| Dental lab charges | 6.4% of gross billing | ADA [25] |
| Repairs of dental equipment | 0.7% of gross billing | ADA [25] |
| Annual depreciation cost on dental equipment | 2.2% of gross billing | ADA [25] |
| EHR software monthly fee | $135 (25) | Delta Dental [26] |
| Transition Costs (applied to the first year) | ||
| Equipment, computers, software | $195,000 (2000) | ADA [27] |
| Integrated EHR development | $5000 | Delta Dental [26] |
| Planning, coordination, informatics and workflow revision, and quality improvement during setup period | $1411 (73) | Prior pilot projects in other disciplines [28,29] |
| Cost, Year 1 (USD) | Cost, after Year 1 (USD) | Gross Revenue (USD) | Net Revenue, Year 1 (USD) | Net Revenue, After Year 1 (USD) | |
|---|---|---|---|---|---|
| Base case | 585,927 (585,335, 586,519) | 389,514 (388,923, 390,104) | 493,830 (492,831, 494,828) | −92,053 (−93,054, −91,052) | 104,316 (103,315, 105,316) |
| Overall utilization (patient visit volume) change | |||||
| 50% | 546,758 (546,184, 547,331) | 350,372 (349,799, 350,944) | 247,654 (247,148, 248,160) | −299,227 (−299,929, −298,526) | −102,717 (−103,416, −102,019) |
| 60% | 554,582 (554,006, 555,158) | 358,180 (357,604, 358,755) | 296,759 (296,157, 297,362) | −257,842 (−258,595, −257,089) | −61,420 (−62,170, −60,669) |
| 70% | 562,408 (562,408, 561,829) | 366,018 (365,439, 366,596) | 346,057 (345,354, 346,760) | −216,448 (−217,256, −215,639) | −19,960 (−20,768, −19,152) |
| 80% | 570,238 (569,655, 570,821) | 373,822 (373,240, 374,404) | 395,141 (394,341, 395,940) | −175,034 (−175,904, −174,164) | 21,318 (20,450, 22,186) |
| 90% | 578,076 (577,489, 578,663) | 381,689 (381,103, 382,275) | 444,617 (443,719, 445,516) | −133,575 (−134,507, −132,644) | 62,928 (61,994, 63,862) |
| 110% | 593,784 (593,188, 594,381) | 397,350 (396,777, 397,966) | 543,252 (542,160, 544,344) | −50,490 (−51,557, −49,421) | 145,880 (144,812, 146,948) |
| 120% | 601,601 (601,000, 602,202) | 405,067 (404,582, 405,782) | 592,374 (591,183, 593,564) | −9145 (−10,287, −8004) | 187,191 (186,052, 188,330) |
| Preventive service utilization change with additional dental hygienist | |||||
| 50% increase | 673,080 (672,304, 673,857) | 476,603 (475,843, 477,363) | 576,377 (575,362, 577,391) | −96,703 (−97,787, −95,620) | 99,774 (98,657, 100,889) |
| 60% increase | 675,706 (674,927, 676,484) | 479,228 (478,469, 479,988) | 592,887 (591,868, 593,907) | −82,818 (−83,897, −81,738) | 113,659 (112,539, 114,778) |
| 70% increase | 678,331 (677,550, 679,112) | 481,854 (481,094, 482,613) | 609,399 (608,373, 610,425) | −68,932 (−70,008, −67,856) | 127,545 (126,421, 128,669) |
| 80% increase | 680,955 (680,171, 681,738) | 484,477 (483,717, 485,237) | 625,899 (624,868, 626,931) | −55,055 (−56,127, −53,982) | 141,422 (140,294, 142,550) |
| 90% increase | 683,580 (682,795, 684,366) | 487,103 (486,343, 487,863) | 642,413 (64,1374, 643,452) | −41,167 (−42,236, −40,097) | 155,310 (154,178, 156,442) |
| 100% increase(full capacity) | 686,208 (685,420, 686,995) | 489,730 (488,970, 490,491) | 658,939 (657,894, 659,985) | −27,268 (−28,335, −26,201) | 169,208 (168,071, 170,345) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, S.E.; Simon, L.; Barrow, J.R.; Palmer, N.; Basu, S.; Phillips, R.S. Dental Practice Integration into Primary Care: A Microsimulation of Financial Implications for Practices. Int. J. Environ. Res. Public Health 2020, 17, 2154. https://doi.org/10.3390/ijerph17062154
Choi SE, Simon L, Barrow JR, Palmer N, Basu S, Phillips RS. Dental Practice Integration into Primary Care: A Microsimulation of Financial Implications for Practices. International Journal of Environmental Research and Public Health. 2020; 17(6):2154. https://doi.org/10.3390/ijerph17062154
Chicago/Turabian StyleChoi, Sung Eun, Lisa Simon, Jane R. Barrow, Nathan Palmer, Sanjay Basu, and Russell S. Phillips. 2020. "Dental Practice Integration into Primary Care: A Microsimulation of Financial Implications for Practices" International Journal of Environmental Research and Public Health 17, no. 6: 2154. https://doi.org/10.3390/ijerph17062154
APA StyleChoi, S. E., Simon, L., Barrow, J. R., Palmer, N., Basu, S., & Phillips, R. S. (2020). Dental Practice Integration into Primary Care: A Microsimulation of Financial Implications for Practices. International Journal of Environmental Research and Public Health, 17(6), 2154. https://doi.org/10.3390/ijerph17062154




