1. Introduction
Assessment of exposure to environmental pollutants requires a wide range of exposure factors to evaluate air, food, and water intakes and frequency and duration of exposure, together with their concentrations in air, water, food, and soil [
1]. Since individual exposure to hazardous substances may significantly vary depending on the exposure factors related to human behaviors and characteristics, a number of aspects should be considered for accurate exposure estimation.
Children’s pattern of exposure to environmental hazards significantly differs from that of adults. Children can be exposed to hazardous substances in the following ways: breastfeeding, hand-to-mouth contact, and their dynamic developmental physiology [
2]. Children are more likely to be exposed to environmental pollutants because their inhalation rates and food/water intakes per body weight are higher than those of adults. According to a World Health Organization (WHO) report, children are exposed to 2.3 times more air, 4.8 times more drinking water, and 6.1 times more foods per body weight than adults [
3]. As children are particularly sensitive to chemical exposure, careful attention should be paid to the development and assessment of exposure factors in children. Young children are also known to have higher exposure to pesticides as they frequently come in contact with soil and dust on surfaces, toys, and other objects [
4]. Previous studies have found that exposure to hazardous substances at young or early juvenile age disrupts neural development or causes neurobehavioral damages [
5,
6].
The United States Environmental Protection Agency (EPA) has created a handbook on exposure factors for children by compiling related data from various sources [
7]. China has developed exposure factor resources for children, but these data are currently not available in English. While Korea published an exposure factor handbook for adults in 2014 [
8], there has been an increasing need to separately assess various factors related to exposure assessment in sensitive groups such as children. Recently, in Korea, children’s risk of exposure to environmental pollutants was potentially over/underestimated in risk assessment by applying default values or exposure factors used in other countries, including the United States. Additionally, exposure factors that represent Korean children’s unique characteristics should also be determined to ensure accurate risk assessment and to better establish relevant environmental national standards [
9]. We have been studying the general exposure factors in Korean children since 2013; the results were published in 2017 [
10]. In contrast, this study was carried out for international comparative evaluation by adding updated national statistics and new experiments, such as those for the rates of soil and dust ingestion and unintentional exposure through hand-to-mouth contact.
This study aimed to propose the representative or recommended values for exposure factors by analyzing the characteristics and behavioral patterns of Korean children and to provide a foundation for more accurate exposure and risk assessment. This would be helpful to establish relevant environmental regulations, standards, and policies for the first time in Korea.
2. Materials and Methods
In this study, we proposed the means, standard deviations, percentages, and other statistical values for Korean children aged ≤18 years for the following five categories: physiological variables, inhalation rates, food and water intake, time–activity patterns, and soil and dust ingestion. The latest data from national organizations, such as Statistics Korea, were used to develop the general exposure factors, and measurements and questionnaire surveys were performed if there were no existing data.
2.1. Categories of Exposure Factors and Age Groups
We obtained the representative or recommended values of the following five categories: physiological variables (body weight and surface area), inhalation rate, food (grains, meat, fish and shellfish, vegetables, fruits, and processed foods) and water intake, time–activity patterns (times spent at microenvironments and in vehicles), and non-dietary ingestion (soil and dust ingestion).
Each legislation has different age criteria for children: ≤13 years in the Environmental Health Act of the Ministry of Environment (MOE) [
11] and <18 years in the Child Welfare Act of the Ministry of Health and Welfare in Korea [
12]. Children are internationally defined as individuals aged <18 years. Therefore, we categorized children into several similar time–activity groups: infant group (age: <1 year), toddler group (age: 1–2 years), preschooler group (age: 3–6 years), elementary school student group (age: 7–12 years), and middle/high school student group (age: 13 and 18 years). Each group was divided into subgroups as necessary to calculate the recommended values for each exposure factor.
2.2. Physiological Exposure Factors
The average daily doses are typically determined by calculating the level of exposure to environmental hazards through breathing and dermal contact based on the specific group’s average body weight. Children, in particular, need to use the recommended values because their weight varies considerably with age.
We used the body weight data of 6290 children aged >1 year from the Korea National Health and Nutrition Examination Survey (KNHANES, 2013–2016) and body weight data of 406 infants aged <12 months from the 5th Size Korea survey conducted by the Korean Agency for Technology and Standards under the Ministry of Industry and Energy (2003–2004).
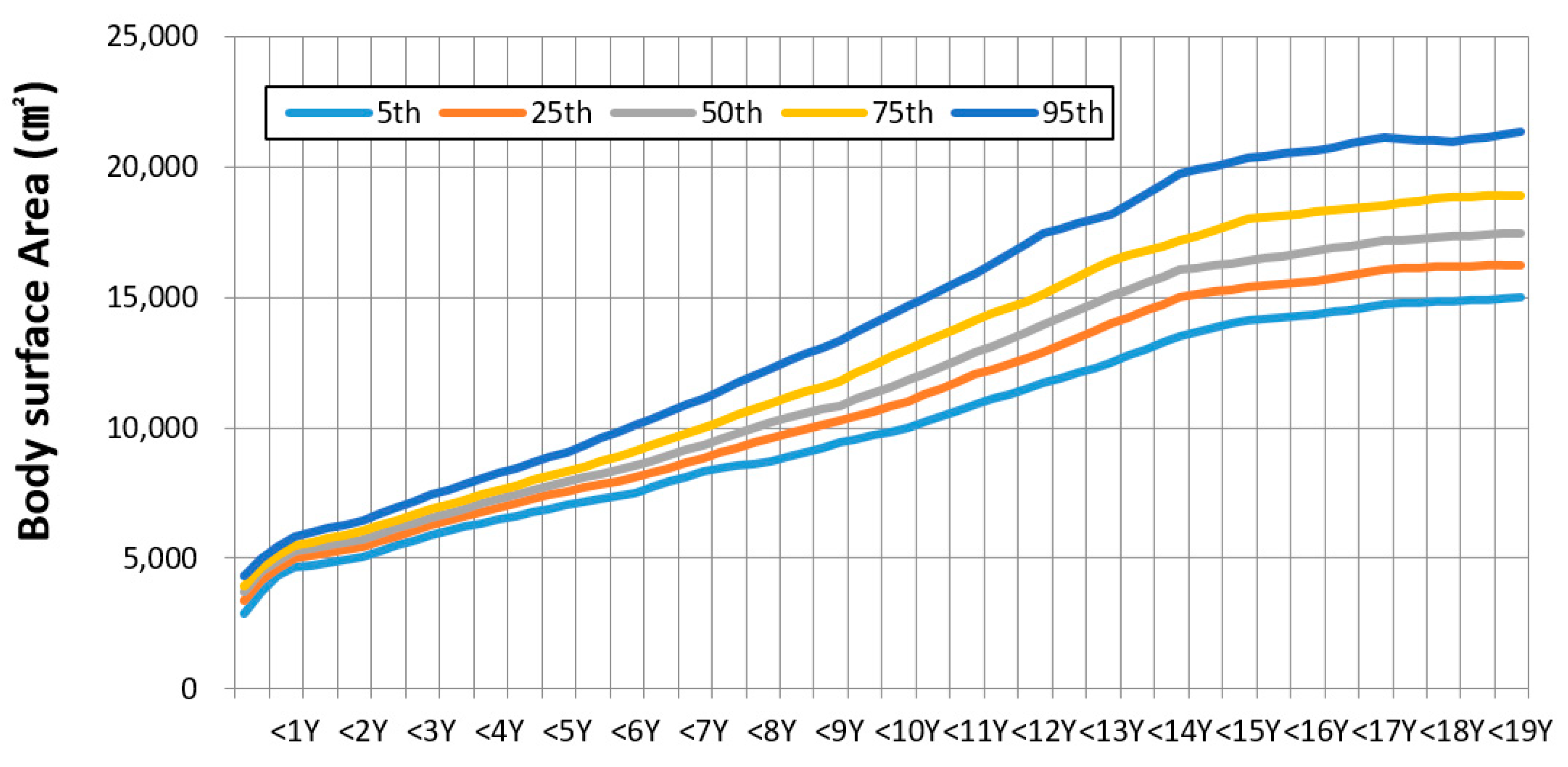
Body surface area (BSA) is one of the major exposure factors required for estimating the extent of dermal exposure to chemicals. As BSA measurement requires considerable time and efforts, regression equations have been proposed, in which the body weight and height of a specific population size were directly measured to predict BSA [
13]. This study used a regression equation formulated based on actual measurements of 305 children (aged 8–18 years) reported by the Korea Ministry of Food and Drug Administration [
14]. The recommended BSA values were calculated for different age groups using their average weights (W) and heights (H):
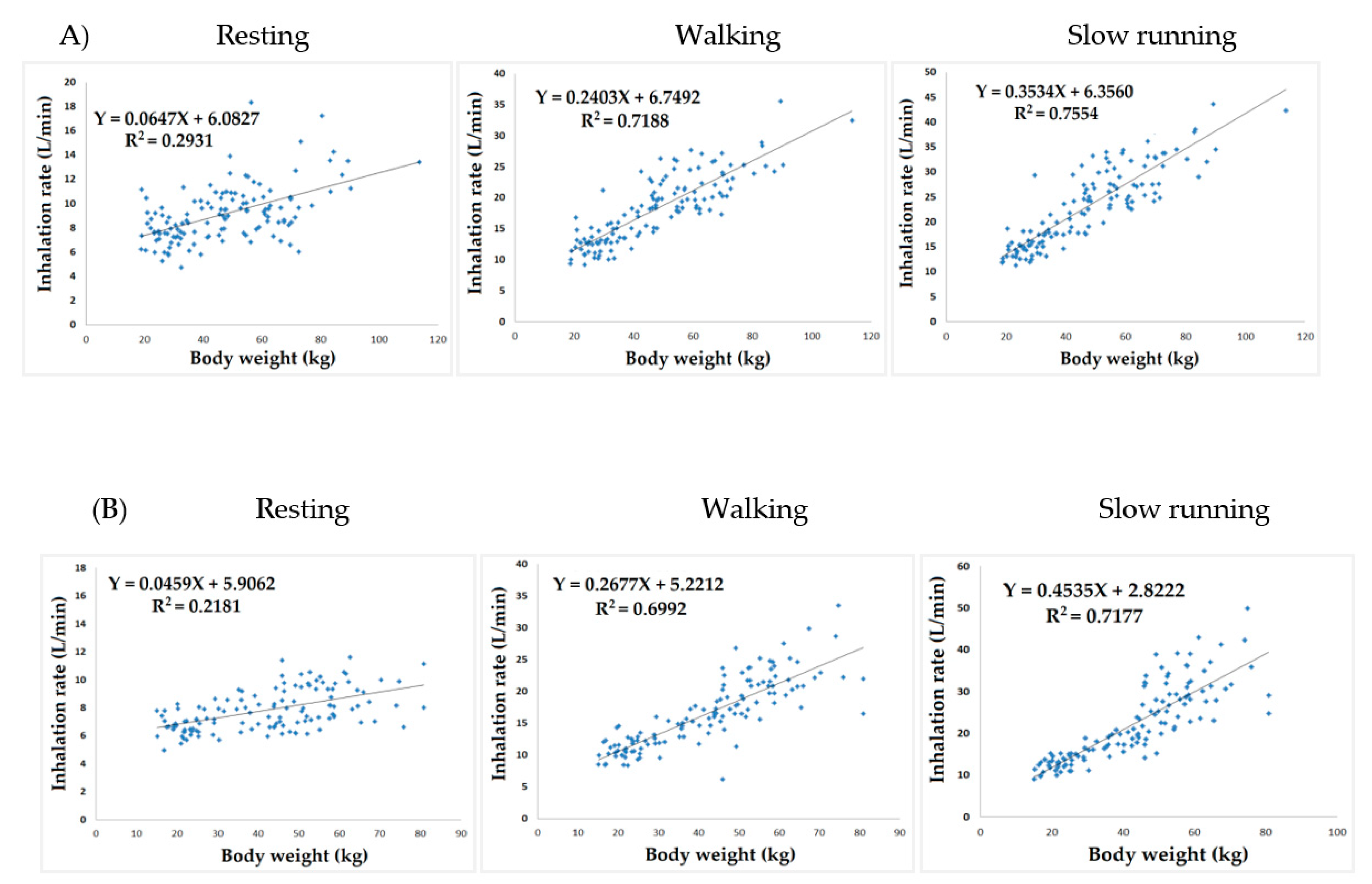
2.3. Inhalation Rate
During the study, there were no data available to calculate the recommended levels for inhalation rate. Thus, the present study performed a direct measurement and data analysis. We measured the body weights and respiratory volumes of 262 children aged ≥5 years who were grouped into preschoolers, elementary school students, and middle/high school students, considering sex and age in 2017. With regard to respiratory volumes, we measured children’s oxygen consumption, metabolism, and ventilation at different activity phases, including resting (in a sedentary state), walking (at 2–3 km/h), and slow running (at 3–4 km/h) for 5–10 min, respectively, using a gas analyzer (Quark b2, COSMED, Italy). Moreover, physical activity patterns were recorded every 10 min using a time–activity diary for 3 days. The respiratory volumes according to the different activity phases were combined with the physical activity patterns. Subsequently, daily inhalation rates (m
3/day) were calculated [
15]. For the group aged <4 years, their daily inhalation rates were estimated using a regression equation based on the correlation between inhalation rate and body weight because measurements of inhalation rates were unattainable.
2.4. Food and Drinking Water Intake
The KNHANES (
http://www.mohw.go.kr/) is one of the key surveys that represent Koreans’ food and nutrient intake. This study analyzed the data of 5,823 children or adolescents aged ≤18 years among the participants of the 2013–2016 surveys. We compiled a list of food items consumed by the surveyed group and categorized them into 14 food groups, including grains, vegetables, fruits, meat, fish/shellfish, and seaweed. To adjust for water loss from different cooking methods, we applied different criteria for calculating consumption depending on whether each food group was consumed as cooked or raw ingredients. This study recategorized the food groups according to the criteria used in the previous study [
7].
2.5. Time–Activity Patterns
To analyze children’s time–activity patterns, a questionnaire survey using a time–activity diary was conducted on 2080 children aged ≤9 years according to sex in 2013–2014. The children’s parents recorded the information using a time–activity diary, and activity information was collected in 10-min intervals. The activities were organized according to the following classification: main activity, additional activity, transportation, indoors, and outdoors. Children aged less than 10 years were selected using a stratified sampling method with the proportional and square root allocation for the country. Their time–activities were analyzed by sex, age, residential area, time (weekdays/weekends), and season. The time–activity pattern data of 27,716 children aged 10–18 years were obtained using the time-use survey method of the Korea National Statistical Office (
http://www.survey.go.kr/lifestyle). The diary classification of this survey included residential indoor, school classroom, and transportation by sex and age (weekdays/weekends).
2.6. Hand-To-Mouth and Object-To-Mouth Activities
A questionnaire survey and videotaping of children’s mouthing behaviors, such as hand-to-mouth and object-to-mouth behaviors were conducted at home and in a kindergarten school where they spent the majority of their time during 2014–2015. We surveyed three metropolitan cities (Incheon, Gwangju, and Daegu), and samples were selected based on the 2014 Statistics of Registered Population of the Ministry of the Interior and Safety. The surveyed children were divided into two groups: children aged 1–2 years and those aged 3–6 years. Two to four camcorders were set up at each daycare center to investigate the frequency (contacts/h) and time (sec/contact) of 147 children’s hand-to-mouth and object-to-mouth activities per hour [
16,
17]. In their houses, the children’s behaviors were observed with a video recording on a mobile phone for 1 h. The children’s contacts with pacifiers were excluded. We analyzed the video recordings of children’s mouthing behavior patterns and crosschecked the findings to reduce errors between analyzers.
2.7. Soil and Dust Ingestion
Children may be exposed to polluted soil or dust when they unintentionally put their hands or objects into their mouths. The present study investigated the soil intake of children and calculated its recommended levels based on the results. The limiting tracer method was used to estimate children’s soil and dust ingestion rates [
18]. First, the concentrations of tracers in children’s feces, neighborhood soil, and indoor dust at home were measured. For the tracers used in the measurement, aluminum, silicon, titanium, and zirconium were selected because of their low levels of consumption via food and their low intestinal absorption rates, although they are abundant in soil. As a result, soil intakes were calculated based on the aluminum concentration. Based on the assumption that soil ingestion could not exceed the lowest concentration value among the tracers, children’s soil and dust ingestion was estimated according to the equation by Binder et al. (1986) [
19]:
where Ti, e is subject i’s estimated ingestion of soil and dust based on the concentration of tracer e (g/day), f i, e is the concentration of tracer e in subject i’s feces (mg/g), F i is the weight of subject i’s dried feces (g/day), and S i, e is the concentration of tracer e in dust and soil in subject i’s living environment (mg/g).
A total of 113 children aged 1–6 years living in metropolitan cities (Incheon, Daegu, and Gwangju) and small/medium-sized cities (Cheongju, Gyeongsan, and Yangpyeong) participated in the investigation. Their concentrations of tracers in children’s feces, neighborhood soil, and indoor dust were analyzed in 2016–2017. The feces of children for 48 h and the soil near their major activity places (home and day-care center) were collected to analyze the concentration of tracers. The collected soil was treated using the EPA’s process testing method, and indoor dust collected using polyvinyl chloride filters was digested using a microwave [
7]. The treated samples were analyzed using inductively coupled plasma atomic emission spectroscopy (Agilent Tech.). To adjust for dietary and other sources of tracer intakes, three children who did not engage in outdoor activities formed the control group. Ultimately, the recommended values for soil and dust ingestion were calculated by accounting for the background concentration of each tracer.
2.8. Statistical Analysis
All data were statistically analyzed using the t-test and the one-way analysis of variance. Regression analysis was used to analyze the association between respiratory volumes and body weights. All data were analyzed using the Statistical Package for the Social Sciences version 18.0 (IBM, USA). This study was approved by the Institutional Review Board (CUIRB-2016-0104) at Daegu Catholic University.
4. Discussion
The risk assessment of hazards in children’s products should be conducted based on exposure scenarios that incorporate the ages, body weights, BSAs, and behavioral patterns of children who use the products [
20]. In general, children’s body weight is proportional to the inhalation rates and BSAs, which may result in differences in the body burden of chemicals even when identical amounts are absorbed in their bodies.
Although the difference in age grouping among countries restricts the direct comparison of body weights across all ages, we identified that the average body weight of Korean children aged 16–18 years is 62.4 kg (67.3 kg for boys and 56.8 kg for girls). These values are lower than the average body weights of Australian children of the same age group, which were 75.0 kg for boys and 61.9 kg for girls [
21]. As average exposures to chemicals are standardized based on the average body weight of the relevant age group, applying the body weight values of Australia and other Western countries to Korean children may result in the underestimated exposure levels [
22].
Inhalation rates are required to assess the level of exposure to hazardous substances absorbed in the respiratory system. Because it is not possible to directly measure the inhalation rates in participants who are wearing gas analyzers on a daily basis, the inhalation rate has been generally measured through heart rate monitoring, metabolic equivalent task, and doubly labeled water method [
23]. The average inhalation rate of Korean children aged 5–6 years was estimated to be 10.8 m
3/day, which is similar to that of European children aged 4–6 years (11 m
3/day) [
24]. The average inhalation rate of Korean children was relatively similar to that of Japanese children (9.9 m
3/day) [
25]. On the contrary, the average inhalation rate of Korean children was lower than that of US children (12.16 m
3/day) [
25]. These differences among countries may be attributable to the difference in gas analyzers used and in the measurement methods for metabolic equivalent task and inhalation rate. However, the inhalation rates in Korean and Japanese children are relatively lower than those in children from Western countries.
With regard to food intake, we divided the foods into 14 groups (e.g., grains, seaweed, vegetables, nuts) to determine the dietary characteristics of Korean children. Meat consumption per body weight among Korean children ranged from 3.06 g/kg/day to 4.16 g/kg/day, which increased to 38% to 87% in the past 15 years. The daily intakes of grains, vegetables, and fruits among US children aged 1–2 years were 6.4 g/kg/day, 6.7 g/kg/day, and 7.8 g/kg/day, respectively [
26]. The average intake of fish/shellfish in Korean preschoolers was 2.26–3.00 g/kg/day, which was approximately 9.4–11.5 times higher than that of the corresponding American children [
26]. On the contrary, Korean children consumed only 47.6%–53.6% of the total percentage of dairy products consumed by US children. The consumption rates of vegetables and fish/shellfish were similar between Korean and Japanese children ranging from 144.1 to 238.6 g/day and from 40.3 to 75.2 g/day, respectively; however, the fruit intake of Korean children was two times higher than that of Japanese children ranging from 91.9 to 104.3 g/day [
27].
The time–activity patterns of the population constitute the most essential data for assessing the level of exposure to environmental pollutants. The duration and frequency of exposure depend on the activity patterns of individuals and the time spent at the location of each activity [
28]. In one of the exposure assessment methods, the concentration of air pollutants in microenvironments and the time spent therein were applied to a mathematical model [
29]. On weekdays, Korean children aged ≤9 years and 10–18 years spent 16.86 h and 12.92 h in houses and 0.72 h and 2.30 h in other indoor locations, including private tutoring institutions, respectively. The total time spent indoors by German, American, and Canadian adolescents was 20.6 h, 20.93 h, and 20.98 h, respectively [
30,
31]. The Korean children spent more time indoors (22.62 h) than children from other countries, which suggests the importance of managing indoor air quality at main indoor locations such as homes, kindergartens, and schools. The time spent outdoors by Korean children aged 3–9 years was 0.73 h, which was a weighted average of weekdays and weekend. The time spent outdoors was only 36.7%–43.7% of the average times spent outdoors by US children aged 3–10 years and Canadian children aged ≤10 years, which are 1.99 and 1.67 h, respectively [
31].
The average hand-to-mouth and object-to-mouth contacts per hour for Korean children between 1 and 2 years were 2.17 and 2.91, respectively. The average duration of object-to-mouth activities was 8.5 min/h, which was similar to the value of 8.9 min/h (7.3–10.5 min/h) reported by Greene’s study [
32]. The object-to-mouth contact frequency was one-third lower in the 3-6 year age group than in the corresponding US (10 contacts/h) and Taiwanese (13.8 contacts/h) children groups [
33]. To minimize the possible uncertainties caused by a recall-based survey, we also recorded children’s object-to-mouth and hand-to-mouth activities; the recorded samples were greater than those reported in similar studies conducted in other countries. However, video recording was conducted only once per day for 30 min, which may have limitations in terms of replicability. Despite these limitations, the reasons for the relatively low values might be as follows: children spent a significant amount of time playing computer games indoors [
34] and Korean mothers specifically prohibit their children from putting their hands into their mouth.
One of the main exposure routes of pollutants in young children is non-dietary exposure such as soil and dust ingestion. The US EPA reported that the unintentional soil and dust intake by children aged between 1 and 6 years is 80 mg/day, which consisted of soil intake of 40 mg/day and dust intake of 40 mg/day [
35]. Using EPA’s stochastic exposure and dose simulation model for multimedia pollutants, the mean and 95th percentile of the amount of ingested of soil and dust were predicted through children mouthing patterns and were found to be 68 and 224 mg/day for children aged 3 to <6 years, respectively [
36]. These values were similar to the corresponding values obtained from this study (70 mg/day as mean, 200 mg/day as the 95th percentile for Korean children aged <7 years). The Korean Exposure Factors Handbook by the MOE reported that children unintentionally ingest 118 mg/day dust and soil, while this study estimated a non-dietary ingestion amount of 70 mg/day, indicating a gradual decrease in soil and dust ingestion when compared with that via other sources [
8]. These findings may be partially attributable to the increasing percentage of playgrounds with urethane floors.
This study has some limitations. First, we only estimated the amount of soil and dust ingestion based on the concentration of tracers in children’s feces; hence, the contribution of tracers through foods and their bioavailability in human bodies were not considered. Second, a long-term investigation was not conducted on a large number of participants due to inherent characteristics and various physiological uncertainties. However, these limitations are common among previous international studies.
Despite some limitations, exposure factors for Korean children could be used as the most fundamental and critical data for estimating the level of exposure to environmental pollutants. Our findings were based on the body weights/BSAs of 6700 children, the food intake of 6000 children, and the time–activity patterns of 9100 children, which represent the reliability among the recently available data in terms of the representativeness of population groups, sample sizes, and being up-to-date. Additionally, while previous studies estimated the breathing rates from heart rates and metabolic equivalents, we significantly reduced the measurement errors by measuring inhalation rates using gas analyzers and treadmills. However, the recommended values for mouthing activity and soil and dust ingestion, which are the main exposure routes in children, were limited considering the lack of accessibility and high cost of requirements.
The US EPA’s Exposure Factors handbook has consistently updated its contents with the latest data to revise recommendations and to add susceptible populations over recent decades. In the future, these factors need to be continuously updated, along with more extensive survey areas and improved measurement methods for inhalation rate, soil and dust ingestion, and other factors.