Psychological Quality of Life in People with Physical Disability: The Effect of Internalized Stigma, Collective Action and Resilience
Abstract
1. Introduction
1.1. The Rejection-Identification Model
1.2. Resilience, Stigma and Quality of Life
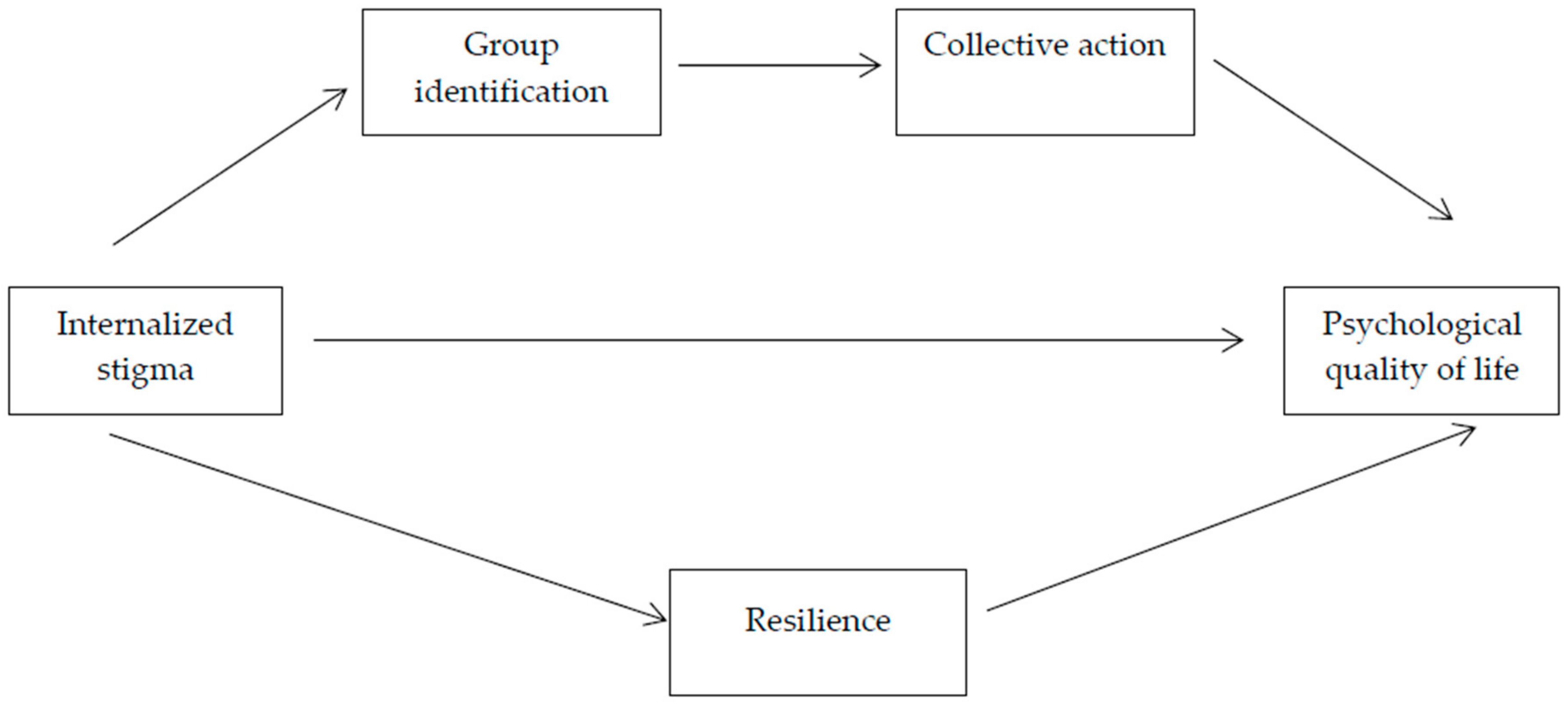
1.3. Goals and Hypotheses
2. Method
2.1. Participants
2.2. Measures
2.3. Procedure
2.4. Statistical Analysis
3. Results
3.1. Model Testing
3.2. Mediation Analyses
4. Discussion
4.1. Practical Implications
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Goffman, E. Stigma: Notes on the Management of Spoiled Identity; PrenticeHall: Englewood Cliffs, NJ, USA, 1963. [Google Scholar]
- Crocker, J.; Major, B.; Steele, C. Social stigma. In Handbook of Social Psychology, 4th ed.; Gilbert, D.T., Fiske, S.T., Eds.; McGrawHill: Boston, MA, USA, 1998. [Google Scholar]
- Dovidio, J.F.; Major, B.; Crocker, J. Stigma: Introduction and overview. In The Social Psychology of Stigma; Heatherton, T.F., Kleck, R.E., Hebl, M.R., Hull, J.G., Eds.; The Guilford Press: New York, NY, USA, 2000. [Google Scholar]
- Hebl, M.R.; Dovidio, J.F. Promoting the “Social” in the Examination of Social Stigmas. Pers. Soc. Psychol. Rev. 2005, 9, 156–162. [Google Scholar] [CrossRef]
- Chang, C.C.; Lin, C.Y.; Gronholm, P.C.; Wu, T.H. Cross-validation of two commonly used selfStigma measures, Taiwan versions of the Internalized Stigma Mental Illness scale and SelfStigma ScaleShort, for people with mental illness. Assessment 2018, 25, 777–792. [Google Scholar] [CrossRef]
- Krahe, B.; Altwasser, C. Changing negative attitudes towards persons with physical disability: An experimental intervention. J. Community Psychol. 2006, 16, 59–69. [Google Scholar] [CrossRef]
- Park, J.H.; Faulkner, J.; Schaller, M. Evolved diseaseAvoidance processes and contemporary antiSocial behavior: Prejudicial attitudes and avoidance of people with physical disability. J. Nonverbal Behav. 2003, 27, 65–87. [Google Scholar] [CrossRef]
- Hebl, M.R.; Tickle, J.; Heatherton, N.T.F. Akwards moments in interactions between nonstigmatized and stigmatized individuals. In The Social Psychology of Stigma; Heatherton, T.F., Kleck, R.E., Hebl, M.R., Hull, J.G., Eds.; The Guilford Press: New York, NY, USA, 2000. [Google Scholar]
- Block, L. Stereotypes about People with Disability. Available online: https://www.disabilitymuseum.org/dhm/edu/essay.html?id=24 (accessed on 16 January 2020).
- Barg, C.J.; Armstrong, B.D.; Hetz, S.P.; Latimer, A.E. Physical disability, stigma, and physical activity in children. Int. J. Disabil. Dev. Educ. 2010, 57, 371–382. [Google Scholar] [CrossRef]
- Pérez-Garín, D.; Molero, F.; Bos, A.E.R. The effect of personal and group discrimination on the subjective well-being of people with mental illness: The role of internalized stigma and collective action intention. Psychol. Health Med. 2017, 22, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Herek, G.M.; Gillis, J.R.; Cogan, J.G. Internalized stigma among sexual minority adults: Insights from a social psychological perspective. J. Couns. Psychol. 2009, 56, 1–32. [Google Scholar] [CrossRef]
- Cavelti, M.; Kvrgic, S.; Beck, E.M.; Rüsch, N.; Vauth, R. SelfStigma and its relationship with insight, demoralization, and clinical outcome among people with schizophrenia spectrum disorders. Compr. Psyquatry 2012, 53, 468–479. [Google Scholar] [CrossRef]
- Cheng, C.M.; Chang, C.C.; Wang, J.-D.; Chang, K.C.; Ting, S.Y.; Lin, C.Y. Negative impacts of selfStigma on the quality of life of patients in methadone maintenance treatment: The mediated roles of psychological distress and social functioning. Int. J. Environ. Res. Public Health 2019, 16, 1299. [Google Scholar] [CrossRef]
- Chang, K.C.; Lin, C.Y.; Chang, C.C.; Ting, S.Y.; Cheng, C.M.; Wang, J.-D. SelfStigma, psychological distress, and quality of life in opioid-dependent individuals. PLoS ONE 2019, 14, e0211033. [Google Scholar]
- Huang, W.Y.; Chen, S.P.; Pakpour, A.H.; Lin, C.Y. The mediation role of self-esteem for selfStigma on quality of life for people with schizophrenia: A retrospectively longitudinal study. J. Pac. Rim Psychol. 2018, 12, e10. [Google Scholar] [CrossRef]
- Lin, C.Y.; Chang, C.C.; Wu, T.H.; Wang, J.-D. Dynamic changes of selfStigma, quality of life, somatic complaints, and depression among people with schizophrenia: A pilot study applying kernel smoothers. Stigma Health 2016, 1, 29–43. [Google Scholar] [CrossRef]
- Chang, C.C.; Wu, T.H.; Chen, C.Y.; Lin, C.Y. Comparing internalized stigma between people with different mental disorders in Taiwan. J. Nerv. Ment. Dis. 2016, 204, 547–553. [Google Scholar] [CrossRef]
- Wu, T.H.; Chang, C.C.; Chen, C.Y.; Wang, J.-D.; Lin, C.Y. Further psychometric evaluation of the SelfStigma ScaleShort: Measurement invariance across mental illness and gender. PLoS ONE 2015, 10, e0117592. [Google Scholar] [CrossRef]
- Chang, C.C.; Wu, T.H.; Chen, C.Y.; Wang, J.-D.; Lin, C.Y. Psychometric evaluation of the Internalized Stigma of Mental Illness Scale for patients with mental illnesses: Measurement invariance across time. PLoS ONE 2014, 9, e98786. [Google Scholar] [CrossRef] [PubMed]
- Saffari, M.; Lin, C.Y.; Koenig, H.G.; O’Garo KG, N.; Broström, A.; Pakpour, A.H. A Persian version of the Affiliate Stigma Scale in caregivers of people with dementia. Health Promot. Perspect. 2019, 9, 31–39. [Google Scholar] [CrossRef]
- Chang, C.C.; Su, J.A.; Chang, K.C.; Lin, C.Y.; Koschorke, M.; Thornicroft, G. Perceived stigma of caregivers: Psychometric evaluation for Devaluation of Consumer Families Scale. International. J. Clin. Health Psychol. 2018, 18, 170–178. [Google Scholar] [CrossRef]
- Chang, C.C.; Yen, C.F.; Jang, F.-L.; Su, J.A.; Lin, C.Y. Comparing affiliate stigma between family caregivers of people with different severe mental illness in Taiwan. J. Nerv. Ment. Dis. 2017, 542–549. [Google Scholar] [CrossRef]
- Chang, C.C.; Su, J.A.; Lin, C.Y. Using the Affiliate Stigma Scale on caregivers of people with dementia: Psychometric evaluation. Alzheimer’s Res. Ther. 2016, 8, 45. [Google Scholar] [CrossRef]
- Chang, C.C.; Su, J.A.; Tsai, C.S.; Yen, C.F.; Liu, J.H.; Lin, C.Y. Rasch analysis suggested three unidimensional domains for Affiliate Stigma Scale: Additional psychometric evaluation. J. Clin. Epidemiol. 2015, 68, 674–683. [Google Scholar] [CrossRef]
- Chang, C.C.; Su, J.A.; Chang, K.C.; Lin, C.Y.; Koschorke, M.; Rüsch, N.; Thornicroft, G. Development of the Family Stigma Stress Scale (FSSS) for detecting stigma stress in caregivers of people with mental illness. Eval. Health Prof. 2019, 42, 148–168. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.; Chan, Y.Y.; Cheng, S.L.; Chow, M.Y.; Tsang, Y.W.; Lee, C.; Lin, C.Y. Investigating quality of life and selfStigma in Hong Kong children with specific learning disabilities. Res. Dev. Disabil. 2017, 68, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.Y.; Oveisi, S.; Burri, A.; Pakpour, A.H. Theory of Planned Behavior including selfStigma and perceived barriers explain helpSeeking behavior for sexual problems in Iranian women suffering from epilepsy. Epilepsy Behav. 2017, 68, 123–128. [Google Scholar] [CrossRef]
- Fung, X.C.C.; Pakpour, A.H.; Wu, K.Y.; Fan, C.W.; Lin, C.Y.; Tsang, H.H.W. Psychosocial variables related to weight-related selfStigma in physical activity among young adults across weight status. Int. J. Environ. Res. Public Health 2019, 17, 64. [Google Scholar] [CrossRef] [PubMed]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Griffiths, M.D.; Su, J.A.; Latner, J.D.; Marshall, R.D.; Pakpour, A.H. A prospective study on the link between weight-related selfStigma and binge eating: Role of food addiction and psychological distress [Epub ahead of print]. Int. J. Eat. Disord. 2020. [Google Scholar] [CrossRef]
- Lin, C.Y.; Tsai, M.C.; Liu, C.H.; Lin, Y.C.; Hsieh, Y.P.; Strong, C. Psychological pathway from obesity-related stigma to depression via internalized stigma and self-esteem among adolescents in Taiwan. Int. J. Environ. Res. Public Health 2019, 16, 4410. [Google Scholar] [CrossRef]
- Alimoradi, Z.; Golboni, F.; Griffiths, M.D.; Broström, A.; Lin, C.Y.; Pakpour, A.H. Weight-related stigma and psychological distress: A systematic review and metaAnalysis [Epub ahead of print]. Clin. Nutr. 2019. [Google Scholar] [CrossRef]
- Lin, C.Y. Weight stigma, coping strategies, and mental health among children with overweight. Soc. Health Behav. 2019, 2, 133–138. [Google Scholar] [CrossRef]
- Lin, C.Y.; Imani, V.; Cheung, P.; Pakpour, A.H. Psychometric testing on two weight stigma instruments in Iran: Weight SelfStigma Questionnaire and Weight Bias Internalized Scale. Eat. Weight Disord. 2019. [Google Scholar] [CrossRef]
- Chan, K.L.; Lee, C.S.C.; Cheng, C.M.; Hui, L.Y.; So, W.T.; Yu, T.S.; Lin, C.Y. Investigating the relationship between weight-related selfStigma and mental health for overweight/obese children in Hong Kong. J. Nerv. Ment. Dis. 2019, 207, 637–641. [Google Scholar] [CrossRef]
- Pakpour, A.H.; Tsai, M.C.; Lin, Y.C.; Strong, C.; Latner, J.D.; Fung, X.C.C.; Lin, C.Y.; Tsang, H.W.H. Psychometric properties and measurement invariance of the Weight SelfStigma Questionnaire and Weight Bias Internalization Scale in Hongkongese children and adolescents. Int. J. Clin. Health Psychol. 2019, 19, 150–159. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.Y.; Strong, C.; Latner, J.D.; Lin, Y.C.; Tsai, M.C.; Cheung, P. Mediated effects of eating disturbances in the association of perceived weight stigma and emotional distress [Epub ahead of print]. Eat. Weight Disord. 2019. [Google Scholar] [CrossRef] [PubMed]
- Cheng, M.Y.; Wang, S.M.; Lam, Y.Y.; Luk, H.T.; Man, Y.C.; Lin, C.Y. The relationships between weight bias, perceived weight stigma, eating behavior and psychological distress among undergraduate students in Hong Kong. J. Nerv. Ment. Dis. 2018, 206, 705–710. [Google Scholar] [CrossRef] [PubMed]
- Wong, P.C.; Hsieh, Y.P.; Ng, H.H.; Kong, S.F.; Chan, K.L.; Au, T.Y.A.; Lin, C.Y.; Fung, X.C.C. Investigating the selfStigma and quality of life for overweight/obese children in Hong Kong: A preliminary study. Child Indic. Res. 2019, 12, 1065–1082. [Google Scholar] [CrossRef]
- Lee, R.S.; Kochman, A.; Sikkema, K.J. Internalized stigma among people living with HIVAIDS. AIDS Behav. 2002, 6, 309–319. [Google Scholar] [CrossRef]
- Parker, R.; Aggleton, P. HIV and AIDS-related stigma and discrimination: A conceptual framework and implications for action. Soc. Sci. Med. 2003, 57, 13–24. [Google Scholar] [CrossRef]
- Visser, M.J.; Kershaw, T.; Makin, J.D.; Forsyth, B.W. Development of parallel scales to measure HIV-related stigma. Aids Behav. 2008, 12, 759–771. [Google Scholar] [CrossRef] [PubMed]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and commitment therapy: Model, processes and outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Switaj, S.; Ggrygiel, P.; Chrostek, A.; Nowak, I.; Wciórka, J.; Anczewska, M. The relationship between internalized stigma and quality of life among people with mental illness: Are self-esteem and sense of coherence sequential mediators? Qual. Life Res. 2017, 26, 2471–2478. [Google Scholar] [CrossRef]
- Post, F.; Pardeller, S.; FranjoApor, B.; Kemmler, G.; Sodermann, C.; Hausmann, A.; Fleischhacker, W.; Mizuno, Y.; Uchida, H.; Hofer, A. Quality of life in stabilized outpatients with bipolar I disorder: Associations with resilience, internalized stigma, and residual symptoms. J. Affect. Disord. 2018, 238, 399–404. [Google Scholar] [CrossRef]
- Branscombe, N.R.; Schmitt, M.T.; Harvey, R.D. Perceiving pervasive discrimination among African Americans: Implications for group identification and well-being. J. Pers. Soc. Psychol. 1999, 77, 135–149. [Google Scholar] [CrossRef]
- Bogart, K.R. Disability identity predicts lower anxiety and depression in Multiple Sclerosis. Rehabil. Psychol. 2015, 69, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Cronin, T.; Levin, S.; Branscombe, N.R.; van Laar, C.; Tropp, L.R. Ethnic identification in response to perceived discrimination protects well-being and promotes activism: A longitudinal study of Latino college students. Group Process. Intergroup Relat. 2012, 15, 393–407. [Google Scholar] [CrossRef]
- Garstka, T.A.; Schmitt, M.T.; Branscombe, N.R.; Hummert, M. How young and older adults differ in their responses to perceived age discrimination. Psychol. Aging 2004, 19, 326–335. [Google Scholar] [CrossRef]
- Leonardelli, G.J.; Tormala, Z.L. The negative impact of perceiving discrimination on collective well-being: The mediating role of perceived ingroup status. Eur. J. Soc. Psychol. 2003, 33, 507–514. [Google Scholar] [CrossRef]
- Armenta, B.E.; Hunt, J.S. Responding to societal devaluation: Effects of perceived personal and group discrimination on the ethnic group identification and personal self-esteem of Latino/Latina adolescents. Group. Process. Intergroup Relat. 2009, 12, 23–39. [Google Scholar] [CrossRef]
- Bourguignon, D.; Seron, E.; Yzerbyt, V.; Herman, G. Perceived group and personal discrimination: Differential effects on personal self-esteem. Eur. J. Soc. Psychol. 2006, 36, 773–789. [Google Scholar] [CrossRef]
- Fernández, S.; Branscombe, N.R.; Gómez, Á.; Morales, J.F. Influence of the social context on use of surgical-lengthening and group-empowering coping strategies among people with dwarfism. Rehabil. Psychol. 2012, 57, 224–235. [Google Scholar] [CrossRef]
- Eccleston, C.P.; Major, B.N. Attributions to discrimination and self-esteem: The role of group identification and appraisals. Group Process. Intergroup Relat. 2006, 9, 147–162. [Google Scholar] [CrossRef]
- Fuster-Ruiz de Apodaca, M.J.; Molero, F.; Holgado, F.P.; Mayordomo, S. Enacted and internalized stigma and quality of life among people with HIV: The role of group identity. Qual. Life Res. 2014, 23, 1967–1975. [Google Scholar] [CrossRef]
- Ellemers, N. Individual upward mobility and the perceived legitimacy of intergroup relations. In The Psychology of Legitimacy; Jost, T., Major, B., Eds.; Cambridge University Press: Cambridge, UK, 2001. [Google Scholar]
- Stürmer, S.; Simon, B. Collective action: Towards a dualPathway model. Eur. Rev. Soc. Psychol. 2004, 15, 59–99. [Google Scholar] [CrossRef]
- Stürmer, S.; Simon, B. The role of collective identification in social movement participation: A panel study in the context of the German gay movement. Pers. Soc. Psychol. Bull. 2004, 30, 263–277. [Google Scholar] [CrossRef] [PubMed]
- Dirth, T.P.; Branscombe, N.R. The social identity approach to disability: Bridging disability studies and psychological science. Psychol. Bull. 2018. [Google Scholar] [CrossRef] [PubMed]
- Moriano, J.A.; Molero, F.; Topa, G.; Lévy Mangin, J.P. The influence of transformational leadership and organizational identification on intrapreneurship. Int. Entrep. Manag. J. 2014, 10, 103–119. [Google Scholar] [CrossRef]
- Molero, F.; Fuster, M.J.; Jetten, J.; Moriano, J.A. Living with HIV/AIDS: A psychosocial perspective on coping with prejudice and discrimination. J. Appl. Soc. Psycho. 2011, 41, 609–626. [Google Scholar] [CrossRef]
- Nouvilas-Pallejá, E.; Silván-Ferrero, P.; Fuster-Ruiz de Apodaca, M.J.; Molero, F. Stigma consciousness and subjective well-being in lesbians and gays. J. Happiness Stud. 2017, 19, 1115–1133. [Google Scholar] [CrossRef]
- Nario-Redmond MR Oleson, K.C. Disability group identification and disability-rights advocacy: Contigencies among emerging and other adults. Emerg. Adulthood 2016, 4, 207–218. [Google Scholar] [CrossRef]
- Migerode, F.; Maes, B.; Buysse, A. Quality of life in adolescents with a disability and their parents: The mediating role of social support and resilience. J. Dev. Phys. Disabil. 2012, 24, 487–503. [Google Scholar] [CrossRef]
- Grotberg, E. A Guide to Promoting Resilience in Children: Strengthening the Human Spirit. Available online: https://files.eric.ed.gov/fulltext/ED383424.pdf (accessed on 16 January 2020).
- Davydov, D.M.; Stewart, R.; Ritchie, K.; Chaudieu, I. Resilience and mental health. Clin. Psychol. Rev. 2010, 30, 479–495. [Google Scholar] [CrossRef]
- Richardson, G.E. The metatheory of resilience and resiliency. J. Clin. Psychiatry 2002, 58, 307–321. [Google Scholar] [CrossRef]
- Richardson, G.E.; Waite, P.J. Mental health promotion through resilience and resiliency education. Int. J. Emerg. Ment. Health 2002, 4, 65–75. [Google Scholar]
- Suriá, R.; García, J.M.; Ortigosa, J.M. Perfiles resilientes y su relación con las habilidades sociales en personas con discapacidad motora. Psicología Conductual 2015, 23, 35–49. [Google Scholar]
- Saavedra, E.; Villalta, M. Estudio comparativo en resiliencia con sujetos discapacitados motores. Revista Investigaciones en Educación 2008, 8, 81–90. [Google Scholar]
- Uriarte, J.D. La perspectiva comunitaria. Psicología Política 2013, 47, 7–18. [Google Scholar]
- Vinaccia, S.; Quiceno, J.M.; Moreno, E. Resiliencia en adolescentes. Revista Colombiana de Psicología 2007, 16, 139–146. [Google Scholar]
- Fletcher, D.; Hanton, S.; Mellalieu, S.D. An organizational stress review: Conceptual and theoretical issues in competitive sport. In Literature Reviews in Sport Psychology; Hanton, S., Mellalieu, S.D., Eds.; Nova Science: Hauppauge, NY, USA, 2006. [Google Scholar]
- Fletcher, D.; Sarkar, M. A Review and Critique of Definitions, Concepts, and Theory. Eur. Psychol. 2013, 18, 12–23. [Google Scholar] [CrossRef]
- Luthar, S.S.; Cicchetti, D.; Becker, B. The construct of resilience: A critical evaluation and guidelines for future work. Child Dev. 2000, 71, 543–562. [Google Scholar] [CrossRef]
- Cameron, C.A.; Ungar, M.; Liebenberg, L. Cultural understandings of resilience: Roots for wings in the development of affective resources for resilience. Child Adolesc. Psychiatr. Clin. N. Am. 2007, 16, 285–301. [Google Scholar] [CrossRef]
- Hofer, A.; Mizuno, Y.; Watelsteiner, F.; Fleischhacker, W.; Frajo-Apor, B.; Kemmler, G.; Mimura, M.; Pardeller, S.; Sondermann, C.; Sizuki, T.; et al. Quality of life in schizophrenia and bipolar disorder: The impact of symptomatic remission and resilience. Eur. Psychiatry 2017, 46, 42–47. [Google Scholar] [CrossRef]
- Taylor, S.E.; Stanton, A.L. Coping resources, coping processes, and mental health. Annu. Rev. Clin. Psychol. 2007, 3, 377–401. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; SpringerPub: New York, NY, USA, 1984. [Google Scholar]
- Rutter, M. Implications of resilience concepts for scientific understanding. Ann. N. Y. Acad. Sci. 2006, 1094, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Gooding, P.A.; Hurst, A.; Johnson, J.; Tarrier, N. Psychological resilience in young and older adults. Int. J. Geriatr. Psychiatry 2012, 27, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, D.; Scott, M. Psychological stress in sports coaches: A review of concepts, theory and research. J. Sports Sci. 2010, 28, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, D.; Fletcher, J. A meta-model of stress, emotions and performance: Conceptual foundations, theoretical framework, and research directions [Abstract]. J. Sports Sci. 2005, 23, 157–158. [Google Scholar] [CrossRef]
- Hofer, M.A. Evolutionary basis of adaptation in resilience and vulnerability: Response to Cicchetti and Blender. Ann. N. Y. Acad. Sci. 2006, 1094, 259–262. [Google Scholar] [CrossRef] [PubMed]
- Mizuno, Y.; Hofer, A.; Suzuki, T.; Frajo-Apor, B.; Watelsteiner, F.; Kemmler, G.; Saruta, J.; Tsukinoki, K.; Mimura, M.; Fleischhacker, W.W.; et al. Clinical and biological correlates of resilience in patients with schizophrenia and bipolar disorder: A cross-sectional study. Schizophr. Res. 2016, 175, 148–153. [Google Scholar] [CrossRef]
- Wartelsteiner, F.; Mizuno, Y.; Frajo-Apor, B.; Kemmler, G.; Pardeller, S.; Sondermann, C.; Welte, A.; Fleischhacker, W.W.; Uchida, H.; Hofer, A. Quality of life in stabilized patients with schizophrenia is mainly associated with resilience and self-esteem. Acta Psychiatr. Scand. 2016, 134, 360–367. [Google Scholar] [CrossRef]
- Feder, A.; Nestler, E.J.; Charmney, D.S. Psychobiology and molecular genetics of resilience. Nat. Rev. Neurosci. 2009, 10, 446–457. [Google Scholar] [CrossRef]
- Battalio, S.L.; Silverman, A.M.; Ehde, D.M.; Amtmann, D.; Edwards, K.A.; Jensen, M.P. Resilience and function in Adults with physical disability: An observational study. Arch. Phys. Med. Rehabil. 2017, 98, 1158–1164. [Google Scholar] [CrossRef]
- Edwards, K.A.; Alschuler, K.A.; Ehde, D.M.; Battalio, S.L.; Jensen, M.P. Changes in resilience predict function in adults with physical disability: A longitudinal study. Arch. Phys. Med. Rehabil. 2017, 98, 329–336. [Google Scholar] [CrossRef]
- Suriá, R. Discapacidad motora y resiliencia: Análisis en función de la edad, grado y etapa en la que se adquiere la discapacidad. Rev. Española Sobre Incapacidad Intelect. 2014, 45, 6–17. [Google Scholar]
- Terrill, A.L.; Molton, I.R.; Ehde, D.M.; Amtmann, D.; Bombardier, C.H.; Smith, A.E.; Jensen, M.P. Resilience, age, and perceived symptoms in persons with long-term physical disability. J. Health Psychol. 2014, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rao, D.; Choi, S.W.; Victorson, D.; Bode, R.; Peterman, A.; Heinemann, A.; Cella, D. Measuring Stigma Across Neurological Conditions: The Development of the Stigma Scale for Chronic Illness (SSCI). Qual. Life Res. 2009, 18, 585–595. [Google Scholar] [CrossRef] [PubMed]
- Molero, F.; Recio, P.; García-Ael, C.; Pérez-Garín, D. Consequences of perceived personal and group discrimination against people with physical disability. Rehabil. Psychol. 2019, 64, 212–220. [Google Scholar] [CrossRef]
- Silván-Ferrero, P.; Recio, P.; Nouvilas-Pallejà, E. Estigma internalizado en personas con discapacidad: Propiedades psicométricas de la versión reducida de la SSCI. (Internalized stigma in people with disability: Psychometric properties of the reduced versión of the SCCI). In Proceedings of the III International Conference of the Spanish Scientific Society of Psychology and the XIV National conference of Social Psychology, Cuenca, Spain, 4–6 October 2018. [Google Scholar]
- Mael, F.; Ashforth, B.E. Loyal from day one: Biodata, organizational identification, and turnover among newcomers. Pers. Psychol. 1995, 48, 309–333. [Google Scholar] [CrossRef]
- Connor, K.M.; Davidson, J.R.T. Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depress Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Notario-Pacheco, B.; Solera-Martínez, M.; Serrano-Parra, M.D.; Bartolomé-Gutiérrez, R.; García-Campayo, J.; Martínez-Vizcaino, V. Reliability and validity of the Spanish version of the 10-item Connor-Davidson Resilience Scale (10-item CD-RISC) in young adults. Health Qual. Life Outcomes 2011, 9, 63–68. [Google Scholar] [CrossRef]
- Lucas-Carrasco, R. Versión Española del Whoqol; Ergón: Madrid, Spain, 1998. [Google Scholar]
- Lucas-Carrasco, R. The WHO quality of life (WHOQOL) questionnaire: Spanish development and validation studies. Qual. Life Res. 2012, 21, 161–165. [Google Scholar] [CrossRef]
- Bentler, P.M. EQS 6 Structural Equations Program Manual; Multivariate Software INC: Encino, CA, USA, 2006. [Google Scholar]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Su, C.T.; Ng, H.S.; Yang, A.L.; Lin, C.Y. Psychometric evaluation of the Short Form 36 Health Survey (SF-36) and the World Health Organization Quality of Life Scale Brief Version (WHOQOL-BREF) for patients with schizophrenia. Psychol. Assess. 2014, 26, 980–989. [Google Scholar] [CrossRef]
- Brown, T.A. Confirmatory Factor Analysis for Applied Research; The Guilford Press: New York, NY, USA, 2006. [Google Scholar]
- Kline, R.B. Principles and Practice of Structural Equation Modelling, 3rd ed.; The Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Yiqing, Y.; Ming, W. Psychological resilience and the onset of activity of daily living disability among older adults in china: A nationwide longitudinal analysis. J. Gerontol. Series B 2014, 70, 470–480. [Google Scholar] [CrossRef]
- Gifre, M.; del Valle, A.; Yuguero, M.; Gil, I.; Origüen, A.; Monreal, P. La mejora de la calidad de vida de las personas con lesión medular: La transición del centro rehabilitador a la vida cotidiana desde la perspectiva de los usuarios. (Quality of life improvement in people with spinal cord injury: The transition from rehabilitation hospital to the everyday life from users perspective). Athenea Digit. Rev. Pensam. Investig. Soc. 2010, 18, 3–15. [Google Scholar]
- Breslow, A.S.; Brewster, M.E.; Velez, B.L.; Wong, S.; Geiger, E.; Soderstrom, B. Resilience and Collective Action: Exploring Buffers Against Minority Stress for Transgender Individuals. Psychol. Sex. Orientat. Gend. Divers. 2015, 2, 253–265. [Google Scholar] [CrossRef]
- Levine, S. The changing terrains in medical sociology: Emergent concern with quality of life. J. Health Soc. Behav. 1987, 28, 1–6. [Google Scholar] [CrossRef]
- Albrecht, G.L.; Devlieger, P.J. The disability paradox: High quality of life against all odds. Soc. Sci. Med. 1999, 48, 977–988. [Google Scholar] [CrossRef]
- Pérez-Garín, D.; Recio, P.; Silván-Ferrero, P.; Nouvilas, E.; Fuster-Ruiz de Apodaca, M.J. How to cope with disability: Development and psychometric properties of the Coping with Disability Difficulties Scale (CDDS). Rehabil. Psychol. 2019. [Google Scholar] [CrossRef]
- Hayes, S.C.; Levin, M.E.; Plumb-Vilardaga, J.; Villatte, J.L.; Pistorello, J. Acceptance and commitment therapy and contextual behavioral science: Examining the progress of a distinctive model of behavioral and cognitive therapy. Behav. Ther. 2013, 44, 180–198. [Google Scholar] [CrossRef]
- McCracken, L.M.; Vowles, K.E. Acceptance and commitment therapy and mindfulness for chronic pain: Model, process, and progress. Am. Psychol. 2014, 69, 178–187. [Google Scholar] [CrossRef]
- Vowles, K.E.; McCracken, L.M. Acceptance and values-based action in chronic pain: A study of treatment effectiveness and process. J. Consult. Clin. Psychol. 2008, 76, 397–407. [Google Scholar] [CrossRef]
- Bradshaw, B.; Richardson, G.E.; Kunmpfer, K.; Carlson, J.; Stanchfield, J.; Overall, J.; Brooks, A.M.; Kulkarni, K. Determining the efficacy of a resiliency training approach in adults with type 2 diabetes. Diabetes Educ. 2007, 33, 650–659. [Google Scholar] [CrossRef]
- Steinhardt, M.A.; Brown, S.A.; Dubois, S.K.; Harrison, L.J.; Lehrer, H.M.; Jaggars, S. A resilience intervention in African-American adults with type 2 diabetes. Am. J. Health Behav. 2015, 39, 507–518. [Google Scholar] [CrossRef] [PubMed]
- Sadler, E.; Sarre, S.; Tinker, A.; Bhalla, A.; McKevitt, C. Developing a novel peer support intervention to promote resilience after stroke. Health Soc. Care Community 2016, 25, 1590–1600. [Google Scholar] [CrossRef] [PubMed]
- Arakkathara, J.G.; Bance, L.O. Promotion of Well-being, Resilience and Stress Management (POWER): An intervention program for mothers of children with intellectual disability: A pilot study. Indian J. Posit. Psychol. 2019, 10, 294–299. [Google Scholar]
- Noone, S.J.; Hastings, R.P. Building psychological resilience in support staff caring for people with intellectual disabilities. J. Intellect. Disabil. 2009, 13, 43–53. [Google Scholar] [CrossRef]
- Edraki, M.; Haghshenas, M.; Yektatalab, S.; Dehghani, S.M.; Haghpanah, S. The effect of Educational-psychological Interventions on the Resilience of the Moders of 1-to-3-year-old Children with Chronic Liver Disease Learning to Cirrhosis. Int. J. Pharm. Res. 2018, 10, 222–226. [Google Scholar]
- Bonanno, G.A.; Westphal, M.; Mancini, A.D. Resilience to lost and potential trauma. Annu. Rev. Clin. Psychol. 2011, 7, 511–535. [Google Scholar] [CrossRef]
- Arrington, E.G.; Wilson, M.N. A re-examination of risk and resilience during adolescence: Incorporating culture and diversity. J. Child. Fam. Stud. 2000, 9, 221–239. [Google Scholar] [CrossRef]
- Deb, A. Psychology of resilience. In Psychology Interventions for Health and Well-Being; Misra, G., Ed.; Springer: Berlin/Heidelberg, Germany, 2018. [Google Scholar]
- Dymecka, J.; Bidzan, M. Biomedical Variables and Adaptation to Disease and Health-Related Quality of Life in Polish Patients with MS. Int. J. Environ. Res. Public Health 2018, 15, 2678. [Google Scholar] [CrossRef]

| M | SD | 1 | 2 | 3 | 4 | 5 | |
|---|---|---|---|---|---|---|---|
| 1. Internalized stigma | 1.98 | 0.71 | - | 0.18 ** | –0.01 | –0.55 ** | –0.51 ** |
| 2. Group identification | 2.69 | 0.78 | - | 0.53 ** | 0.07 | 0.03 | |
| 3. Collective action | 3.16 | 0.69 | - | 0.23 ** | 0.13 | ||
| 4. Resilience | 3.00 | 0.63 | - | 0.62 ** | |||
| 5. Psychological quality of life | 3.34 | 0.55 | - |
| Mediational Analysis | Direct Beta without Mediator | Direct Beta with Mediator | Indirect Beta [CI] | |
|---|---|---|---|---|
| IE → GI and CA → Resilience | No mediation | −0.53 *** | −0.55 *** | 0.02 ** [0.008 – 0.043] |
| IE → GI → CA | No mediation | −0.01 | 0.09 ** | 0.03 [0.036 – 0.158] |
| IE → Resilience → PQL | Partial mediation | −0.61 *** | −0.32 *** | −0.29* [−0.223 – −0.371] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silván-Ferrero, P.; Recio, P.; Molero, F.; Nouvilas-Pallejà, E. Psychological Quality of Life in People with Physical Disability: The Effect of Internalized Stigma, Collective Action and Resilience. Int. J. Environ. Res. Public Health 2020, 17, 1802. https://doi.org/10.3390/ijerph17051802
Silván-Ferrero P, Recio P, Molero F, Nouvilas-Pallejà E. Psychological Quality of Life in People with Physical Disability: The Effect of Internalized Stigma, Collective Action and Resilience. International Journal of Environmental Research and Public Health. 2020; 17(5):1802. https://doi.org/10.3390/ijerph17051802
Chicago/Turabian StyleSilván-Ferrero, Prado, Patricia Recio, Fernando Molero, and Encarnación Nouvilas-Pallejà. 2020. "Psychological Quality of Life in People with Physical Disability: The Effect of Internalized Stigma, Collective Action and Resilience" International Journal of Environmental Research and Public Health 17, no. 5: 1802. https://doi.org/10.3390/ijerph17051802
APA StyleSilván-Ferrero, P., Recio, P., Molero, F., & Nouvilas-Pallejà, E. (2020). Psychological Quality of Life in People with Physical Disability: The Effect of Internalized Stigma, Collective Action and Resilience. International Journal of Environmental Research and Public Health, 17(5), 1802. https://doi.org/10.3390/ijerph17051802





