The Mediating Role of the Patient Health Engagement Model on the Relationship Between Patient Perceived Autonomy Supportive Healthcare Climate and Health Literacy Skills
Abstract
1. Introduction
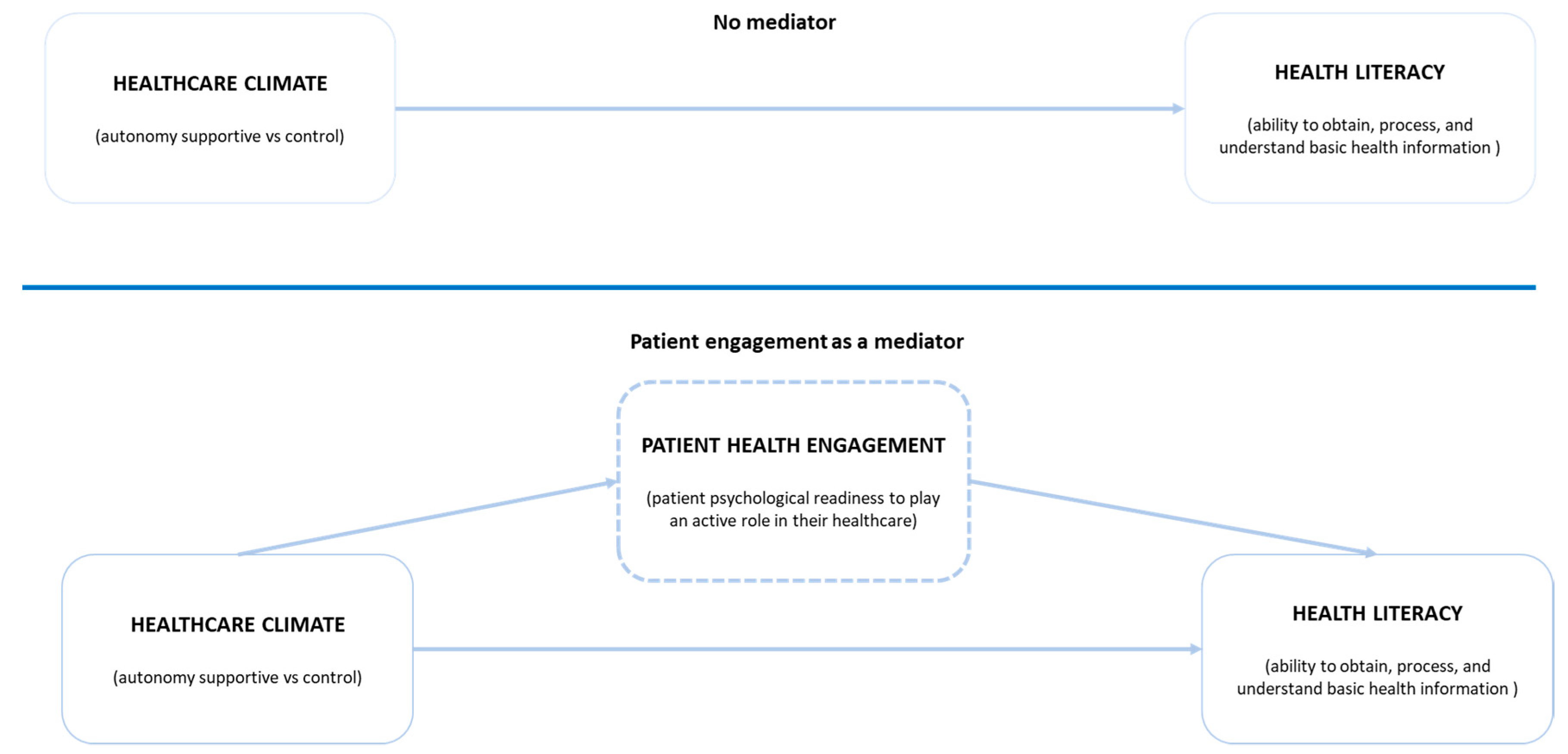
2. Theory and Hypotheses
3. Methodology
3.1. Study Design and Participants
3.2. Measures
3.3. Data Analysis
3.4. Ethics
4. Results
4.1. Socio-Demographics and Clinical Characteristics
4.2. Descriptive Characteristics
4.3. Measurement Model
4.4. Structural Model and Hypotheses Testing
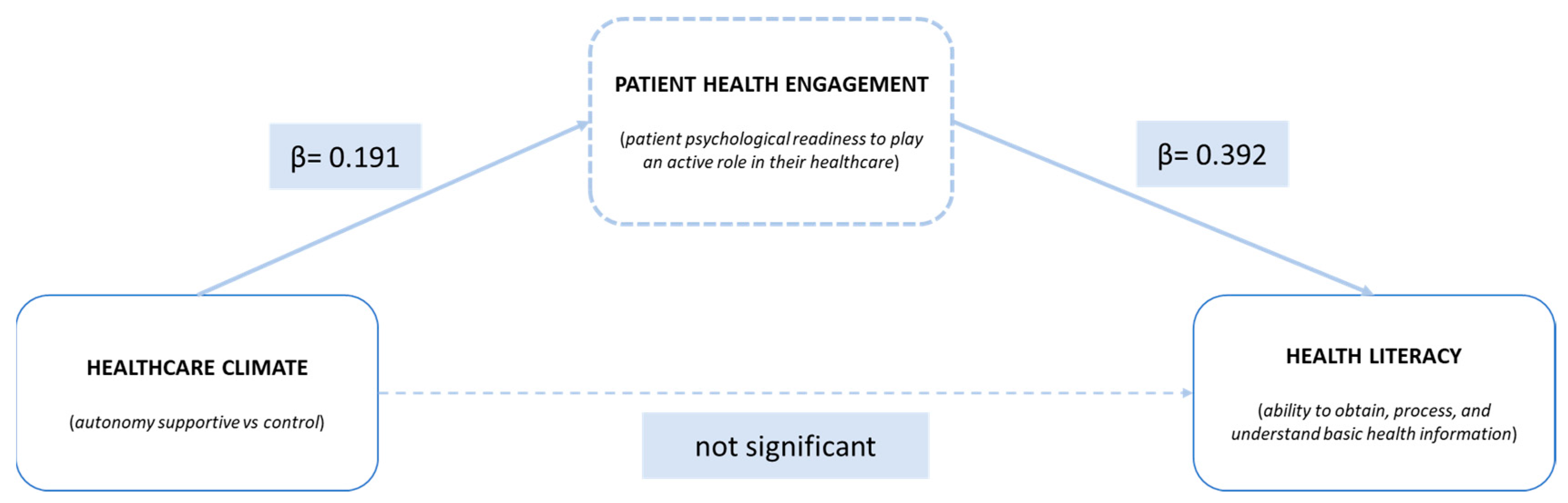
4.5. Mediating Effect and H4
5. Discussion
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ishikawa, H.; Yano, E. Patient health literacy and participation in the health-care process. Health Expect. 2008, 11, 13–22. [Google Scholar] [CrossRef]
- Schapira, M.M.; Fletcher, K.E.; Hayes, A.; Eastwood, D.; Patterson, L.; Ertl, K.; Whittle, J. The development and validation of the hypertension evaluation of lifestyle and management knowledge scale. J. Clin. Hypertens. (Greenwich) 2012, 14, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Davis, T.C.; McCormack, L. Health literacy: What is it? J. Health Commun. 2010, 15, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Sudore, R.L.; Yaffe, K.; Satterfield, S.; Harris, T.B.; Mehta, K.M.; Simonsick, E.M.; Newman, A.B.; Rosano, C.; Rooks, R.; Rubin, S.M.; et al. Limited literacy and mortality in the elderly: The health, aging, and body composition study. J. Gen. Intern. Med. 2006. [Google Scholar] [CrossRef] [PubMed]
- Sudore, R.L.; Mehta, K.M.; Simonsick, E.M.; Harris, T.B.; Newman, A.B.; Satterfield, S.; Rosano, C.; Rooks, R.N.; Rubin, S.M.; Ayonayon, H.N.; et al. Limited literacy in older people and disparities in health and healthcare access. J. Am. Geriatr. Soc. 2006. [Google Scholar] [CrossRef]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011. [Google Scholar] [CrossRef]
- Paasche-Orlow, M.K.; Wolf, M.S. The causal pathways linking health literacy to health outcomes. Am. J. Health Behav. 2007. [Google Scholar] [CrossRef]
- Paasche-Orlow, M.K.; Parker, R.M.; Gazmararian, J.A.; Nielsen-Bohlman, L.T.; Rudd, R.R. The prevalence of limited health literacy. J. Gen. Intern. Med. 2005. [Google Scholar] [CrossRef]
- Paasche-Orlow, M.K.; Schillinger, D.; Greene, S.M.; Wagner, E.H. How health care systems can begin to address the challenge of limited literacy. J. Gen. Intern. Med. 2006. [Google Scholar] [CrossRef]
- Graffigna, G.; Barello, S. Spotlight on the Patient Health Engagement model (PHE model): A psychosocial theory to understand people’s meaningful engagement in their own health care. Patient Prefer. Adher. 2018, 12, 1261–1271. [Google Scholar] [CrossRef]
- Kaba, R.; Sooriakumaran, P. The evolution of the doctor-patient relationship. Int. J. Surg. 2007, 5, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Zeuner, R.; Frosch, D.L.; Kuzemchak, M.D.; Politi, M.C. Physicians’ perceptions of shared decision-making behaviours: A qualitative study demonstrating the continued chasm between aspirations and clinical practice. Health Expect. 2014. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Graffigna, G. Patient engagement in healthcare: Pathways for effective medical decision making. Neuropsychol. Trends 2015, 17. [Google Scholar] [CrossRef]
- Graffigna, G.; Barello, S.; Bonanomi, A. The role of Patient Health Engagement model (PHE-model) in affecting patient activation and medication adherence: A structural equation model. PLoS ONE 2017, 12, e0179865. [Google Scholar] [CrossRef]
- Schmidt, K.; Gensichen, J.; Petersen, J.J.; Szecsenyic, J.; Walther, M.; Williamse, G.; Freund, T. Autonomy support in primary care—Validation of the German version of the Health Care Climate Questionnaire. J. Clin. Epidemiol. 2012, 65, 206–211. [Google Scholar] [CrossRef]
- Greene, J.; Hibbard, J.H.; Alvarez, C.; Overton, V. Supporting patient behavior change: Approaches used by primary care clinicians whose patients have an increase in activation levels. Ann. Fam. Med. 2016, 14, 148–154. [Google Scholar] [CrossRef]
- Greene, J.; Hibbard, J.H. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J. Gen. Intern. Med. 2012, 27, 520–526. [Google Scholar] [CrossRef]
- Ryan, R.M.; Patrick, H.; Deci, E.L.; Williams, G.C. Facilitating health behaviour change and its maintenance: Interventions based on self-determination theory. Eur. Health Psychol. 2008. [Google Scholar] [CrossRef]
- Williams, G.C.; Gagné, M.; Ryan, R.M.; Deci, E.L. Facilitating autonomous motivation for smoking cessation. Health Psychol. 2002. [Google Scholar] [CrossRef]
- Barry, M.J.; Edgman-levitan, S.; Billingham, V. Shared decision making—The pinnacle of patient-centered care. N. Engl. J. Med. 2012, 366, 780–781. [Google Scholar] [CrossRef]
- Rathert, C.; Wyrwich, M.D.; Boren, S.A. Patient-centered care and outcomes: A systematic review of the literature. Med. Care Res. Rev. 2013. [Google Scholar] [CrossRef]
- Lyttle, D.J.; Ryan, A. Factors influencing older patients’ participation in care: A review of the literature. Int. J. Older People Nurs. 2010, 5, 274–282. [Google Scholar] [CrossRef] [PubMed]
- Williams, G.C.; Niemiec, C.P.; Patrick, H.; Ryan, R.M.; Deci, E.L. The importance of supporting autonomy and perceived competence in facilitating long-term tobacco abstinence. Ann. Behav. Med. 2009, 37, 315–324. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Williams, M.V.; Davis, T.; Parker, R.M.; Weiss, B.D. The role of health literacy in patient-physician communication. Fam. Med. 2002. [Google Scholar] [CrossRef]
- Clayman, M.L.; Pandit, A.U.; Bergeron, A.R.; Cameron, K.A.; Ross, E.; Wolf, M.S. Ask, understand, remember: A brief measure of patient communication self-efficacy within clinical encounters. J. Health Commun. 2010, 15, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Kaphingst, K.A.; Weaver, N.L.; Wray, R.J.; Brown, M.L.; Buskirk, T.; Kreuter, M.W. Effects of patient health literacy, patient engagement and a system-level health literacy attribute on patient-reported outcomes: A representative statewide survey. BMC Health Serv. Res. 2014, 14. [Google Scholar] [CrossRef] [PubMed]
- Capone, V. Patient communication self-efficacy, self-reported illness symptoms, physician communication style and mental health and illness in hospital outpatients. J. Health Psychol. 2016. [Google Scholar] [CrossRef]
- Gao, S.; Barello, S.; Chen, L.; Chen, C.; Che, G.; Cai, K.; Crisci, R.; D’Andrilli, A.; Droghetti, A.; Fu, X.; et al. Clinical guidelines on perioperative management strategies for enhanced recovery after lung surgery. Transl. Lung Cancer Res. 2019, 8, 1174–1187. [Google Scholar] [CrossRef]
- Sak, G.; Rothenfluh, F.; Schulz, P.J. Assessing the predictive power of psychological empowerment and health literacy for older patients’ participation in health care: A cross-sectional population-based study. BMC Geriatr. 2017. [Google Scholar] [CrossRef]
- McCormack, L.; Thomas, V.; Lewis, M.A.; Rudd, R. Improving low health literacy and patient engagement: A social ecological approach. Patient Educ. Couns. 2017, 100, 8–13. [Google Scholar] [CrossRef]
- Edwards, M.; Wood, F.; Davies, M.; Edwards, A. The development of health literacy in patients with a long-term health condition: The health literacy pathway model. BMC Public Health 2012, 12, 130. [Google Scholar] [CrossRef]
- Graffigna, G.; Barello, S.; Bonanomi, A.; Edwards, A. The motivating function of healthcare professional in eHealth and mHealth interventions for Type 2 Diabetes patients and the mediating role of patient engagement. J. Diabetes Res. 2016, 2016, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Coulter, A.; Ellins, J. Effectiveness of strategies for informing, educating, and involving patients. BMJ 2007. [Google Scholar] [CrossRef] [PubMed]
- Flickinger, T.E.; Saha, S.; Moore, R.D.; Beach, M.C. Higher quality communication and relationships are associated with improved patient engagement in HIV care. J. Acquir. Immune. Defic. Syndr. 2013. [Google Scholar] [CrossRef] [PubMed]
- Casu, G.; Gremigni, P.; Sommaruga, M. The Patient-Professional Interaction Questionnaire (PPIQ) to assess patient centered care from the patient’s perspective. Patient Educ. Couns. 2019. [Google Scholar] [CrossRef] [PubMed]
- Lamiani, G.; Barello, S.; Browning, D.M.; Vegni, E.; Meyer, E.C. Uncovering and validating clinicians’ experiential knowledge when facing difficult conversations: A cross-cultural perspective. Patient Educ. Couns. 2012, 87, 307–312. [Google Scholar] [CrossRef] [PubMed]
- Provenzi, L.; Barello, S.; Fumagalli, M.; Graffigna, G.; Sirgiovanni, I.; Savarese, M.; Montirosso, R. A comparison of maternal and paternal experiences of becoming parents of a very preterm infant. J. Obstet. Gynecol. Neonatal Nurs. 2016, 45, 528–541. [Google Scholar] [CrossRef]
- Barello, S.; Graffigna, G.; Vegni, E.; Savarese, M.; Lombardi, F.; Bosio, A.C. ‘Engage me in taking care of my heart’: A grounded theory study on patient-cardiologist relationship in the hospital management of heart failure. BMJ Open 2015, 5. [Google Scholar] [CrossRef]
- Snow, J. The Complete Research Suite: A Step by Step Guide to Using Qualtrics; Qualtrics: Provo, UT, UAS, 2011. [Google Scholar]
- Williams, G.C.; Minicucci, D.S.; Kouides, R.W.; Deci, E.L. Self-determination, smoking, diet and health. Health Educ. Res. 2002, 17, 512–521. [Google Scholar]
- Czajkowska, Z.; Wang, H.; Hall, N.C.; Sewitch, M.; Körner, A. Validation of the English and French versions of the Brief Health Care Climate Questionnaire. Health Psychol. Open 2017, 4. [Google Scholar] [CrossRef]
- Chew, L.D.; Bradley, K.A.; Boyko, E.J. Brief questions to identify patients with inadequate health literacy. Fam. Med. 2004, 36, 588–594. [Google Scholar]
- Press, V.G.; Shapiro, M.I.; Mayo, A.M.; Meltzer, D.O.; Arora, V.M. More than meets the eye: Relationship between low health literacy and poor vision in hospitalized patients. J. Health Commun. 2013, 18, 197–204. [Google Scholar] [CrossRef][Green Version]
- Lorini, C.; Santomauro, F.; Grazzini, M.; Mantwill, S.; Vettori, V.; Lastrucci1, V.; Bechini, A.; Boccalini, S.; Bussotti, A.; Bonaccorsi, G. Health literacy in Italy: A cross-sectional study protocol to assess the health literacy level in a population-based sample, and to validate health literacy measures in the Italian language. BMJ Open 2017, 7, 1–7. [Google Scholar] [CrossRef]
- Graffigna, G.; Barello, S.; Bonanomi, A.; Lozza, E. Measuring patient engagement: Development and psychometric properties of the Patient Health Engagement (PHE) Scale. Front. Psychol. 2015, 6, 274. [Google Scholar] [CrossRef] [PubMed]
- JASP Team. JASP (0.11.1); JASP: Amsterdam, The Netherlands, 2019. [Google Scholar]
- Anderson, J.C.; Gerbing, D.W. Structural equation modeling in practice: A review and recommended two-step approach. Psychol. Bull. 1988, 103, 411–423. [Google Scholar] [CrossRef]
- Beavers, A.S.; Lounsbury, J.W.; Richards, J.K.; Huck, S.W.; Skolits, G.J.; Esquivel, S.L. Practical considerations for using exploratory factor analysis in educational research. Pract. Assess. Res. Eval. 2013, 18, 1–13. [Google Scholar]
- Fornell, C.; Larcker, D.F. Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 1981, 18, 39–50. [Google Scholar] [CrossRef]
- Schumacker, R.E.; Lomax, R.G. A Beginner’s Guide to Structural Equation Modeling, 2nd ed.; Psychology Press: East Sussex, UK, 2004. [Google Scholar]
- Hooper, D.; Coughlan, J.; Mullen, M.R. Structural equation modelling: Guidelines for determining model fit. Electron. J. Bus. Res. Methods 2008, 6, 53–60. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Navarro, A.; Acedo, F.J.; Losada, F.; Ruzo, E. Integrated model of export activity: Analysis of heterogeneity in managers’ orientations and perceptions on strategic marketing management in foreign markets. J. Mark. Theory Pract. 2011, 19, 187–204. [Google Scholar] [CrossRef]
- IBM SPSS. Amos (21.0.0, build 1178); IBM: Armonk, NY, USA, 2012. [Google Scholar]
- Jacobs, R.J.; Lou, J.Q.; Ownby, R.L.; Caballero, J. A systematic review of eHealth interventions to improve health literacy. Health Inform. J. 2014, 22, 81–98. [Google Scholar] [CrossRef]
- Durand, M.-A.; Carpenter, L.; Dolan, H.; Bravo, P.; Mann, M.; Bunn, F.; Elwyn, G. Do interventions designed to support shared decision-making reduce health inequalities? A systematic review and meta-analysis. PLoS ONE 2014, 9, e94670. [Google Scholar] [CrossRef]
- Yin, H.S.; Jay, M.; Maness, L.; Zabar, S.; Kalet, A. Health literacy: An educationally sensitive patient outcome. J. Gen. Intern. Med. 2015, 30, 1363–1368. [Google Scholar] [CrossRef]
- Schillinger, D.; Piette, J.; Grumbach, K.; Wang, F.; Wilson, C.; Daher, C.; Leong-Grotz, K.; Castro, C.; Bindman, A.B. Closing the loop: Physician communication with diabetic patients who have low health literacy. Arch. Intern. Med. 2003. [Google Scholar] [CrossRef] [PubMed]
- Schillinger, D.; Bindman, A.; Wang, F.; Stewart, A.; Piette, J. Functional health literacy and the quality of physician-patient communication among diabetes patients. Patient Educ. Couns. 2004. [Google Scholar] [CrossRef]
- Rademakers, J.; Nijman, J.; Brabers, A.E.; de Jong, J.D.; Hendriks, M. The relative effect of health literacy and patient activation on provider choice in the Netherlands. Health Policy 2014, 114, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Barello, S.; Graffigna, G. Engaging patients to recover life projectuality: An Italian cross-disease framework. Qual. Life Res. 2015, 24, 1087–1096. [Google Scholar] [CrossRef]
| Variables | n | % |
|---|---|---|
| Gender | ||
| Female | 676 | 67.1 |
| Male | 331 | 32.9 |
| Age | ||
| 18–30 | 131 | 13.0 |
| 31–50 | 483 | 48.0 |
| 51–70 | 358 | 35.6 |
| >70 | 35 | 3.4 |
| Hospitalized last year | ||
| Yes | 188 | 18.7 |
| No | 819 | 81.3 |
| Disease condition | ||
| Cardiovascular disease | 127 | 12.6 |
| Thyroid disease | 124 | 12.3 |
| Autoimmune disease | 117 | 11.6 |
| Arthritis | 100 | 9.9 |
| Pulmonary disease | 100 | 9.9 |
| Cancer | 98 | 9.8 |
| Diabetes | 75 | 7.4 |
| Migraine | 60 | 6.0 |
| Multiple sclerosis | 55 | 5.5 |
| Gastrointestinal disease | 20 | 2.0 |
| Skin disease | 17 | 1.7 |
| Osteoporosis | 13 | 1.3 |
| Other diseases | 101 | 10.0 |
| Patient Health Engagement (PHE-S) | ||
| Blackout | 61 | 6.1 |
| Alert | 380 | 37.7 |
| Adherence | 458 | 45.5 |
| Eudaimonic Project | 108 | 10.7 |
| Variables | Mean | Median | Std. Dev. | Skewness (S.E.) | Kurtosis (S.E.) |
|---|---|---|---|---|---|
| Autonomy-Supportive Healthcare Climate (HCCQ) | |||||
| Item 1 | 4.20 | 4 | 1.68 | −0.33 (0.08) | −0.55 (0.15) |
| Item 2 | 4.88 | 5 | 1.63 | −0.67 (0.08) | −0.15 (0.15) |
| Item 3 | 5.15 | 5 | 1.56 | −0.80 (0.08) | 0.19 (0.15) |
| Item 4 | 5.07 | 5 | 1.53 | −0.77 (0.08) | 0.21 (0.15) |
| Item 5 | 5.09 | 5 | 1.61 | −0.81 (0.08) | 0.09 (0.15) |
| Item 6 | 4.83 | 5 | 1.48 | −0.54 (0.08) | −0.02 (0.15) |
| Patient Health Engagement (PHE-S) | |||||
| Item 1 | 4.28 | 5 | 1.48 | −0.29 (0.08) | −0.31 (0.15) |
| Item 2 | 4.46 | 5 | 1.38 | −0.27 (0.08) | −0.12 (0.15) |
| Item 3 | 4.54 | 5 | 1.55 | 0.14 (0.08) | −0.90 (0.15) |
| Item 4 | 4.44 | 5 | 1.63 | −0.20 (0.08) | −0.53 (0.15) |
| Item 5 | 4.60 | 5 | 1.56 | −0.07 (0.08) | −0.62 (0.15) |
| Health Literacy (BHLS) | |||||
| Item 1 | 1.30 | 1 | 0.99 | 0.24 (0.08) | −0.72 (0.15) |
| Item 2 | 1.35 | 1 | 1.06 | 0.55 (0.08) | −0.20 (0.15) |
| Item 3 | 1.40 | 1 | 1.13 | 0.36 (0.08) | −0.73 (0.15) |
| Variables | Index | HCCQ | PHE-S | BHLS |
|---|---|---|---|---|
| HCCQ | Spearman’s rho | — | ||
| p-value | — | |||
| PHE-S | Spearman’s rho | 0.198 | — | |
| p-value | <0.001 | — | ||
| BHLS | Spearman’s rho | −0.136 | −0.404 | — |
| p-value | <0.001 | <0.001 | — |
| Variables | Factor Loadings | Cronbach’s α | CR | AVE |
|---|---|---|---|---|
| Autonomy-Supportive Healthcare Climate (HCCQ) | 0.927 | 0.84 | 0.48 | |
| Item 1 | 0.599 | |||
| Item 2 | 0.928 | |||
| Item 3 | 0.916 | |||
| Item 4 | 0.850 | |||
| Item 5 | 0.899 | |||
| Item 6 | 0.777 | |||
| Patient Health Engagement (PHE-S) | 0.914 | 0.89 | 0.48 | |
| Item 1 | 0.798 | |||
| Item 2 | 0.839 | |||
| Item 3 | 0.822 | |||
| Item 4 | 0.828 | |||
| Item 5 | 0.840 | |||
| Health Literacy (BHLS) | 0.636 | 0.64 | 0.39 | |
| Item 1 | 0.848 | |||
| Item 2 | 0.375 | |||
| Item 3 | 0.642 |
| Hypothesis | Path | Std. Beta | p-Value |
|---|---|---|---|
| H1 | HCCQ -> BHLS | −0.136 | <0.001 |
| H2 | PHE-S -> BHLS | −0.393 | <0.001 |
| H3 | HCCQ -> PHE-S | 0.198 | <0.001 |
| Path | Std. Beta | p-Value |
|---|---|---|
| Total (HCCQ -> BHLS) | −0.136 | p < 0.001 |
| Direct (HCCQ-> BHLS) | −0.058 | p = 0.152 |
| Indirect (HCCQ -> PHE-S -> BHLS) | −0.078 | p < 0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barello, S.; Palamenghi, L.; Graffigna, G. The Mediating Role of the Patient Health Engagement Model on the Relationship Between Patient Perceived Autonomy Supportive Healthcare Climate and Health Literacy Skills. Int. J. Environ. Res. Public Health 2020, 17, 1741. https://doi.org/10.3390/ijerph17051741
Barello S, Palamenghi L, Graffigna G. The Mediating Role of the Patient Health Engagement Model on the Relationship Between Patient Perceived Autonomy Supportive Healthcare Climate and Health Literacy Skills. International Journal of Environmental Research and Public Health. 2020; 17(5):1741. https://doi.org/10.3390/ijerph17051741
Chicago/Turabian StyleBarello, Serena, Lorenzo Palamenghi, and Guendalina Graffigna. 2020. "The Mediating Role of the Patient Health Engagement Model on the Relationship Between Patient Perceived Autonomy Supportive Healthcare Climate and Health Literacy Skills" International Journal of Environmental Research and Public Health 17, no. 5: 1741. https://doi.org/10.3390/ijerph17051741
APA StyleBarello, S., Palamenghi, L., & Graffigna, G. (2020). The Mediating Role of the Patient Health Engagement Model on the Relationship Between Patient Perceived Autonomy Supportive Healthcare Climate and Health Literacy Skills. International Journal of Environmental Research and Public Health, 17(5), 1741. https://doi.org/10.3390/ijerph17051741





