Diagnostic Accuracy of Videofluoroscopy for Symptomatic Cervical Spine Injury Following Whiplash Trauma
Abstract
1. Introduction
2. Methods
3. Results
3.1. Model 1
3.2. Model 2
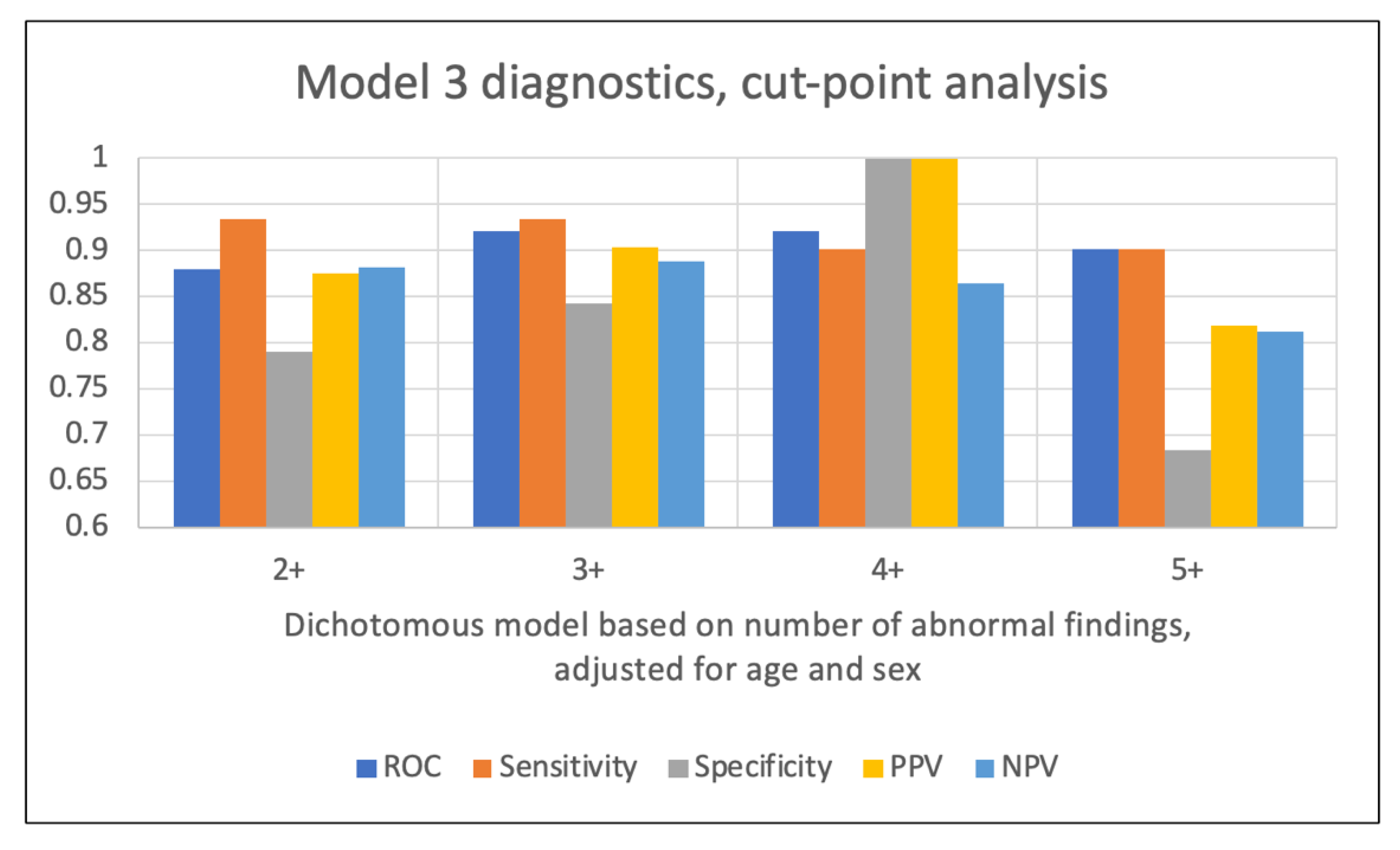
3.3. Model 3
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Hoy, D.G.; Protani, M.; De, R.; Buchbinder, R. The epidemiology of neck pain. Best. Pract. Res. Clin. Rheumatol. 2010, 24, 783–792. [Google Scholar] [CrossRef] [PubMed]
- Nolet, P.S.; Emary, P.C.; Kristman, V.L.; Murnaghan, K.; Zeegers, M.P.; Freeman, M.D. Exposure to a Motor Vehicle Collision and the Risk of Future Neck Pain: A Systematic Review and Meta-Analysis. PM&R. Available online: http://www.ncbi.nlm.nih.gov/pubmed/31020768 (accessed on 12 June 2019).
- Insurance Research Council. Auto Injury Insurance Claims: Countrywide Patterns in Treatment, Cost, and Compensation; Insurance Research Council: Malvern, PA, USA, 2008. [Google Scholar]
- McConnell, W.E.; Howard, R.P.; Guzman, H.M.; Bomar, J.B.; Raddin, J.H.; Benedict, J.V.; Smith, H.L.; Hatsell, C.P. Analysis of Human Test Subject Kinematic Responses to Low Velocity Rear End Impacts. In SAE Technical Paper 930889; SAE International: Warrendale, PA, USA, 1993. [Google Scholar]
- Westergren, H.; Larsson, J.; Freeman, M.; Carlsson, A.; Jöud, A.; Malmström, E.-M. Sex-based differences in pain distribution in a cohort of patients with persistent post-traumatic neck pain. Disabil. Rehabil. 2018, 40, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Ivancic, P.; Ito, S.; Tominaga, Y.; Rubin, W.; Coe, M.; Ndu, A.; Carlson, E.J.; Panjabi, M.M. Whiplash causes increased laxity of cervical capsular ligament. Clin. Biomech. 2008, 23, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Tominaga, Y.; Ndu, A.B.; Coe, M.P.; Valenson, A.J.; Ivancic, P.C.; Ito, S.; Rubin, W.; Panjabi, M.M. Neck ligament strength is decreased following whiplash trauma. BMC Musculoskelet. Disord. 2006, 7, 103. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Steilen, D.; Hauser, R.; Woldin, B.; Sawyer, S. Chronic neck pain: Making the connection between capsular ligament laxity and cervical instability. Open Orthop, J. 2014, 8, 326–345. [Google Scholar] [CrossRef] [PubMed]
- Uhrenholt, L.; Gregersen, M.; Charles, A.V.; Hauge, E.M.; Nielsen, E. Examinations of the deceased can contribute to the understanding of whiplash injuries after traffic accidents. Ugeskr. Laeger. 2010, 172, 3129. [Google Scholar] [PubMed]
- Cholewicki, J.; McGill, S.; Wells, R.; Vernon, H. Method for measuring vertebral kinematics from videofluoroscopy. Clin. Biomech. 1991, 8, 73–78. [Google Scholar] [CrossRef]
- Derrick, L.J.; Chesworth, B.M. Post-motor vehicle accident alar ligament laxity. J. Orthop. Sports. Phys. Ther. 1992, 16, 6–11. [Google Scholar] [CrossRef] [PubMed]
- Krakenes, J.; Kaale, B.; Moen, G.; Nordli, H.; Gilhus, N.; Rorvik, J. MRI assessment of the alar ligaments in the late stage of whiplash injury—A study of structural abnormalities and observer agreement. Neuroradiology 2002, 44, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Croft, A.C.; Krage, J.; Pate, D.; Young, D. Videofluoroscopy in cervical spine trauma: An interinterpreter reliability study. J. Manipulative. Physiol. Ther. 1994, 17, 20–24. [Google Scholar] [PubMed]
- Daffner, R.H. Imaging of Vertebral Trauma, 3rd ed.; Cambridge University Press: Cambridge, UK, 2011; p. 163. [Google Scholar]
- Park, M.S.; Moon, S.-H.; Lee, H.-M.; Kim, S.W.; Kim, T.-H.; Suh, B.-K.; Riew, K.D. The natural history of degenerative spondylolisthesis of the cervical spine with 2- to 7- year follow-up. Spine 2013, 38, E205–E210. [Google Scholar] [CrossRef] [PubMed]
- Kopacz, K.J.; Connolly, P.J. The prevalence of cervical spondylolisthesis. Orthopedics 1999, 22, 677–679. [Google Scholar] [PubMed]
- Rondinelli, R.D.; Genovese, E.; Brigham, C.R.; American Medical Association. Guides to the Evaluation of Permanent Impairment, 6th ed.; American Medical Association: Chicago, IL, USA, 2008; p. 634. [Google Scholar]
- Siegmund, G.P.; Winkelstein, B.A.; Ivancic, P.C.; Svensson, M.Y.; Vasavada, A. The Anatomy and Biomechanics of Acute and Chronic Whiplash Injury. Traffic. Inj. Prev. 2009, 10, 101–112. [Google Scholar] [CrossRef] [PubMed]
- Pettersson, K.; Hildingsson, C.; Toolanen, G.; Fagerlund, M.; Björnebrink, J. MRI and neurology in acute whiplash trauma: No correlation in prospective examination of 39 cases. Acta Orthop. Scand. 1994, 65, 525–528. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, R.; Kwan, O.; Russell, A.S.; Pearce, J.M.; Schrader, H. The best approach to the problem of whiplash? One ticket to Lithuania, please. Clin. Exp. Rheumatol. 1999, 17, 321–326. [Google Scholar] [PubMed]
- Schmand, B.; Lindeboom, J.; Schagen, S.; Heijt, R.; Koene, T.; Hamburger, H.L. Cognitive complaints in patients after whiplash injury: The impact of malingering. J. Neurol. Neurosurg. Psychiatry 1998, 64, 339–343. [Google Scholar] [CrossRef] [PubMed]
- Yoganandan, N.; Cusick, J.F.; Pintar, F.A.; Rao, R.D. Whiplash injury determination with conventional spine imaging and cryomicrotomy. Spine 2001, 26, 2443–2448. [Google Scholar] [CrossRef] [PubMed]
| Anatomical/Biomechanical Parameter (View) | Vertebral Level | VF motion Examination/View Details | Measurement Details | Expected Normal Values |
|---|---|---|---|---|
| Lateral overhang (AP) | C1-2 | A-P open mouth, R and L lateral flexion | Maximum difference in lateral translation (in mm) of the lateral margin of the lateral mass of C1 relative to the lateral margin of the superior articular facet of C2, between sides | 2 mm or less overhang difference between sides |
| Peri-odontoid space symmetry (AP) | C1-2 | A-P open mouth, R and L lateral flexion | Bilateral symmetry of gap between dens of C2 and medial margin of lateral mass of C1, observed at extreme R and L flexion | Symmetrical gap maintained |
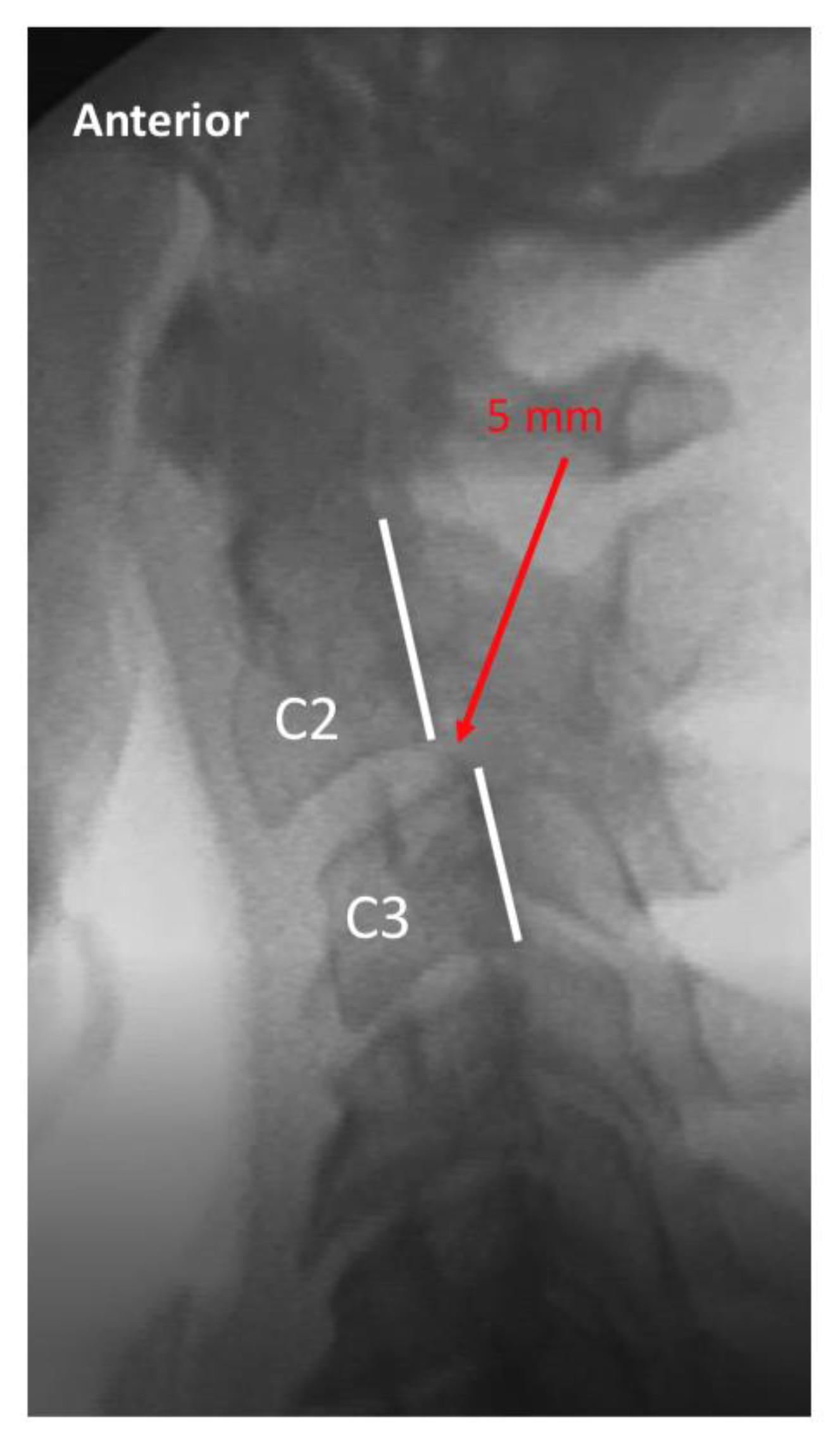
| Translation (lat) | C2-7 | Lateral flexion-extension | Maximum anterior (in flexion) or posterior (in extension) translation of vertebral body relative to adjacent inferior vertebra, measured at posterior vertebral body line | 2 mm or less anterior or posterior translation |
| Intervertebral angulation (lat) | C2-7 | Lateral flexion-extension | Angle between adjacent posterior vertebral body lines in maximum flexion | 10 degrees or less |
| SP engagement (lat) | C2-7 | Lateral flexion-extension | Degree of synchronous movement between adjacent spinous processes during flexion from neutral | Inter-spinous process distance increases commensurately with flexion |
| SP coupled movement (AP) | C2-7 | AP c-spine R and L lateral flexion | Degree of coupled spinous process rotation with ipsilateral flexion | Spinous process rotates during lateral flexion |
| Facet gapping (AP) | C2-7 | AP c-spine R and L lateral flexion | Degree of separation at facet during maximal lateral flexion | No appreciable gapping at maximum lateral flexion |
| Facet gapping (obl) | C2-7 | R and L oblique c-spine flexion-extension | Degree of separation at facet during maximal forward flexion | No appreciable gapping at maximum forward flexion |
| Facet symmetry (obl) | C2-7 | R and L oblique c-spine flexion-extension | Degree of symmetrical movement at facets during flexion and extension, comparing right and left | Movement and degree of gapping is symmetrical between sides |
| Measurements | Dichotomous Recode | |
|---|---|---|
| C1-2 lateral overhang (AP view) | 0–2 mm | 0–2 mm > 2 mm |
| > 2–4 mm | ||
| > 4–6 mm | ||
| > 6 mm | ||
| C1-2 peri-odontoid symmetry (AP view) | Symmetrical | Symmetrical Asymmetrical |
| Mildly-Asymmetrical | ||
| Asymmetrical | ||
| C2-7 translation (lat view) | 0–2 mm | 0–2 mm > 2 mm |
| > 2–3 mm | ||
| > 3–4 mm | ||
| > 4 mm | ||
| C2-7 inter-vertebral angulation (lat view) | < 10 degrees | < 10 degrees 10 + degrees |
| 10 + degrees | ||
| C2-7 SP engagement (lat view) | In sequence | In sequence Not in sequence |
| Moderately out of sequence | ||
| Markedly out of sequence | ||
| C2-7 SP coupled movement (AP view) | In sequence | In sequence Not in sequence |
| Moderately out of sequence | ||
| Markedly out of sequence | ||
| C2-7 Facet gapping (AP view) | Insignificant | Insignificant Not insignificant |
| Noticeable | ||
| Marked | ||
| C2-7 Facet gapping (obl view) | Insignificant | InsignificantNot insignificant |
| Noticeable | ||
| Marked | ||
| C2-7 facet symmetry (obl view) | Symmetrical | Symmetrical Asymmetrical |
| Mildly-Asymmetrical | ||
| Asymmetrical |
| Symptomatic, n = 119 | Asymptomatic, n = 77 | p-Value * | |
|---|---|---|---|
| Demographic (%) | |||
| Female, n (%) | 90 (75.6) | 36 (46.8) | < 0.0001 |
| Age, mean (se) | 40.5 (1.26) | 33.9 (1.36) | 0.0006 |
| Abnormal VF finding count (%) | |||
| Total abnormal VF findings, mean (se) | 1.2 (0.16) | 0.13 (0.04) | < 0.0001 |
| C1-C2 lat overhang (AP), n (%) | 75 (63.6) | 25 (32.5) | < 0.0001 |
| C1-C2 peri-odontoid (AP), n (%) | 34 (28.8) | 3 (3.9) | < 0.0001 |
| C2-7 translation (lat), n (%) | |||
| C2-C3 | 38 (31.9) | 2 (2.6) | < 0.0001 |
| C3-C4 | 13 (11.0) | 9 (11.7) | 0.88 |
| C4-C5 | 58 (48.7) | 19 (24.7) | 0.001 |
| C5-C6 | 23 (19.3) | 2 (2.6) | 0.001 |
| C6-C7 | 3 (2.5) | 0 (0) | 0.16 |
| C2-7 intervertebral angulation (lat), n (%) | |||
| C2-C3 | 5 (4.2) | 0 (0) | 0.07 |
| C3-C4 | 8 (6.7) | 1 (1.3) | 0.08 |
| C4-C5 | 30 (25.2) | 6 (7.8) | 0.002 |
| C5-C6 | 10 (8.4) | 3 (3.9) | 0.22 |
| C6-C7 | 4 (3.4) | 0 (0) | 0.1 |
| C2-7 SP engagement (lat), n (%) | |||
| C2-C3 | 2 (1.7) | 0 (0) | 0.25 |
| C3-C4 | 15 (12.6) | 1 (1.3) | 0.005 |
| C4-C5 | 28 (23.7) | 0 (0) | < 0.0001 |
| C5-C6 | 30 (25.2) | 0 (0) | < 0.0001 |
| C6-C7 | 12 (10.2) | 0 (0) | 0.004 |
| C2-7 SP coupled motion (AP), n (%) | |||
| C2-C3 | 3 (2.6) | 0 (0) | 0.16 |
| C3-C4 | 11 (9.4) | 0 (0) | 0.006 |
| C4-C5 | 32 (27.4) | 0 (0) | < 0.0001 |
| C5-C6 | 49 (41.9) | 3 (3.9) | < 0.0001 |
| C6-C7 | 9 (7.7) | 4 (5.2) | 0.5 |
| C2-7 facet gapping (AP), n (%) | |||
| C2-C3 | 1 (0.9) | 0 (0) | 0.41 |
| C3-C4 | 14 (12.1) | 0 (0) | 0.002 |
| C4-C5 | 40 (34.5) | 3 (3.9) | < 0.0001 |
| C5-C6 | 44 (37.9) | 0 (0) | < 0.0001 |
| C6-C7 | 15 (12.9) | 1 (1.3) | 0.004 |
| C2-7 facet gapping (obl), n (%) | |||
| C2-C3 | 3 (2.6) | 0 (0) | 0.16 |
| C3-C4 | 14 (12.0) | 0 (0) | 0.002 |
| C4-C5 | 56 (47.9) | 1 (1.3) | < 0.0001 |
| C5-C6 | 49 (41.9) | 2 (2.6) | < 0.0001 |
| C6-C7 | 33 (28.2) | 2 (2.6) | < 0.0001 |
| C2-7 facet symmetry (obl), n (%) | |||
| C2-C3 | 3 (2.6) | 0 (0) | 0.16 |
| C3-C4 | 10 (8.6) | 0 (0) | 0.008 |
| C4-C5 | 32 (27.4) | 3 (3.9) | < 0.0001 |
| C5-C6 | 22 (18.8) | 4 (5.2) | 0.007 |
| C6-C7 | 15 (12.9) | 1 (1.3) | 0.004 |
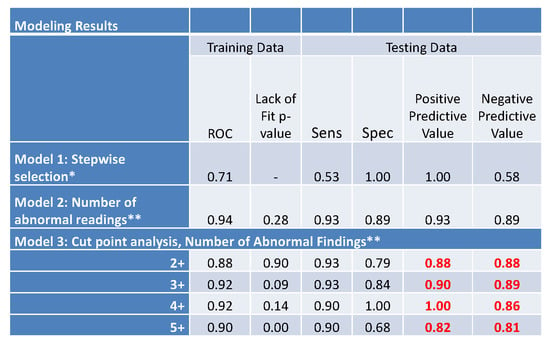
| Training Data | Testing Data | |||||
|---|---|---|---|---|---|---|
| ROC | Lack of Fit p-Value | Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value | |
| Model 1: Stepwise selection * | 0.71 | - | 0.53 | 1.00 | 1.00 | 0.58 |
| Model 2: Number of abnormal readings ** | 0.94 | 0.28 | 0.93 | 0.89 | 0.93 | 0.89 |
| Model 3: Cut point analysis, Number of Abnormal Findings ** | ||||||
| 2+ | 0.88 | 0.90 | 0.93 | 0.79 | 0.88 | 0.88 |
| 3+ | 0.92 | 0.09 | 0.93 | 0.84 | 0.90 | 0.89 |
| 4+ | 0.92 | 0.14 | 0.90 | 1.00 | 1.00 | 0.86 |
| 5+ | 0.90 | 0.00 | 0.90 | 0.68 | 0.82 | 0.81 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Freeman, M.D.; Katz, E.A.; Rosa, S.L.; Gatterman, B.G.; Strömmer, E.M.F.; Leith, W.M. Diagnostic Accuracy of Videofluoroscopy for Symptomatic Cervical Spine Injury Following Whiplash Trauma. Int. J. Environ. Res. Public Health 2020, 17, 1693. https://doi.org/10.3390/ijerph17051693
Freeman MD, Katz EA, Rosa SL, Gatterman BG, Strömmer EMF, Leith WM. Diagnostic Accuracy of Videofluoroscopy for Symptomatic Cervical Spine Injury Following Whiplash Trauma. International Journal of Environmental Research and Public Health. 2020; 17(5):1693. https://doi.org/10.3390/ijerph17051693
Chicago/Turabian StyleFreeman, Michael D., Evan A. Katz, Scott L. Rosa, Bryan G. Gatterman, Ellen M. F. Strömmer, and Wendy M. Leith. 2020. "Diagnostic Accuracy of Videofluoroscopy for Symptomatic Cervical Spine Injury Following Whiplash Trauma" International Journal of Environmental Research and Public Health 17, no. 5: 1693. https://doi.org/10.3390/ijerph17051693
APA StyleFreeman, M. D., Katz, E. A., Rosa, S. L., Gatterman, B. G., Strömmer, E. M. F., & Leith, W. M. (2020). Diagnostic Accuracy of Videofluoroscopy for Symptomatic Cervical Spine Injury Following Whiplash Trauma. International Journal of Environmental Research and Public Health, 17(5), 1693. https://doi.org/10.3390/ijerph17051693