Characterization of Esophageal Cancer and Its Association with Influencing Factors in Guangzhou City, China
Abstract
1. Introduction
2. Materials and Methods
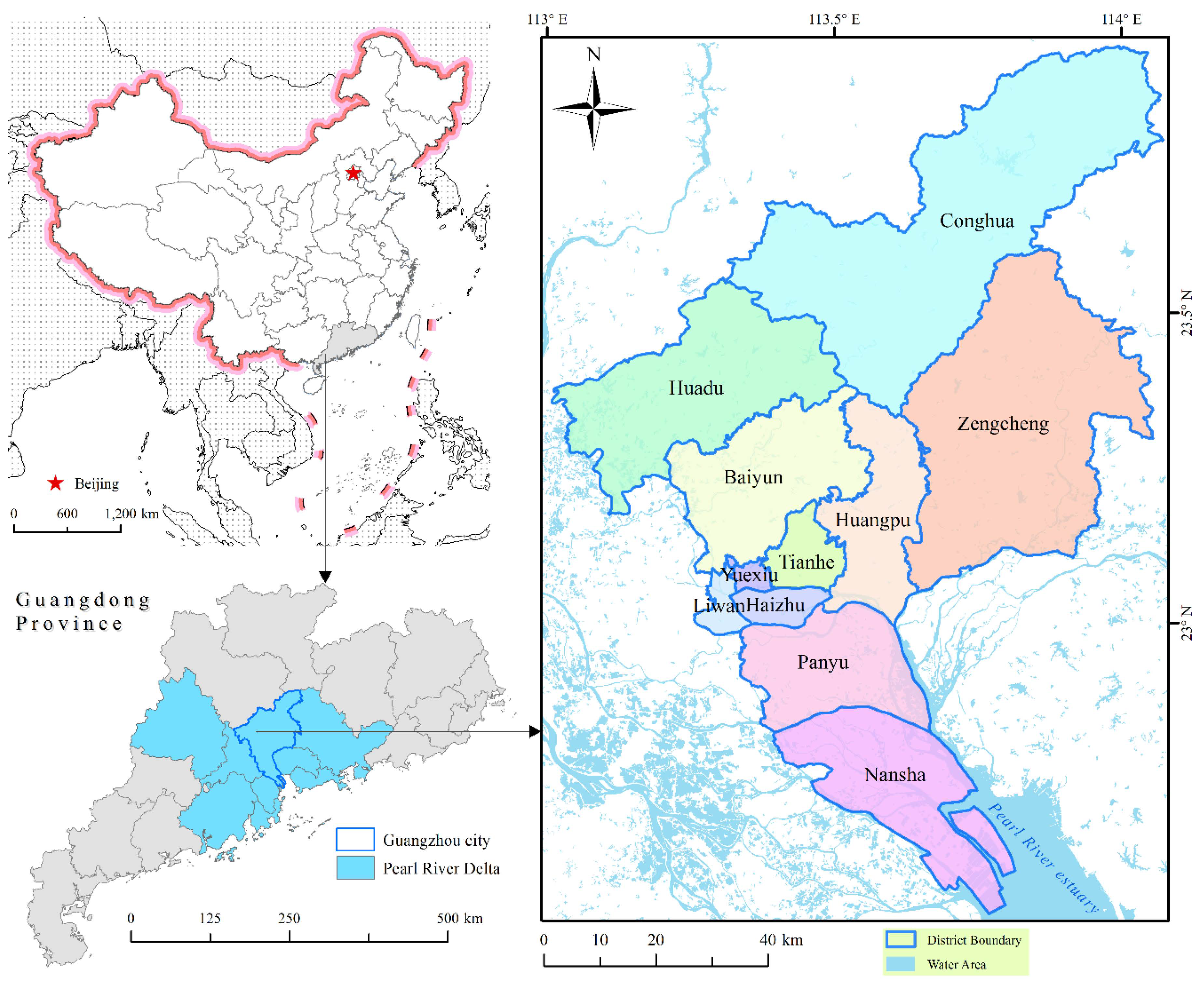
2.1. Study Area
2.2. Data Collection and Processing
2.3. Epidemiological and Statistical Analysis
2.4. Spatial Analysis
3. Results
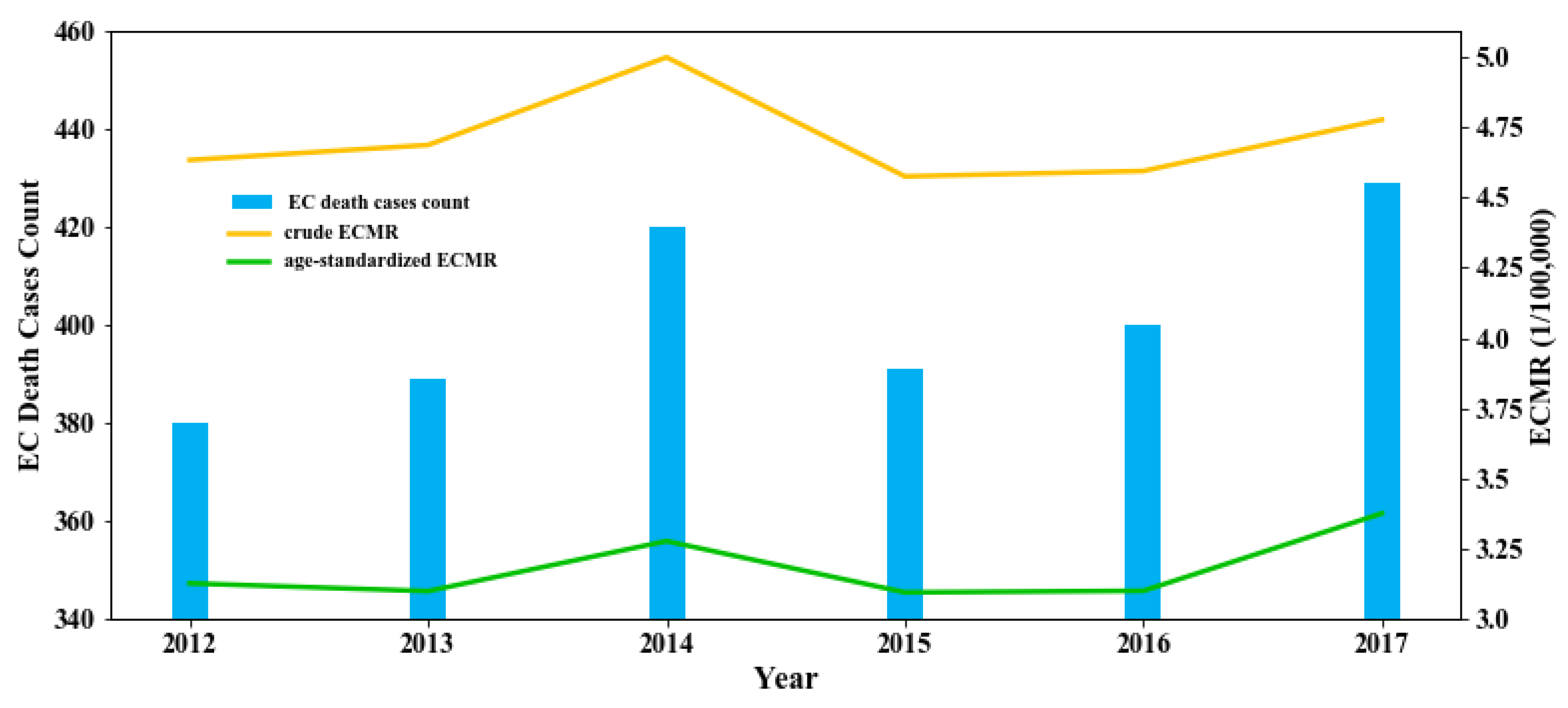
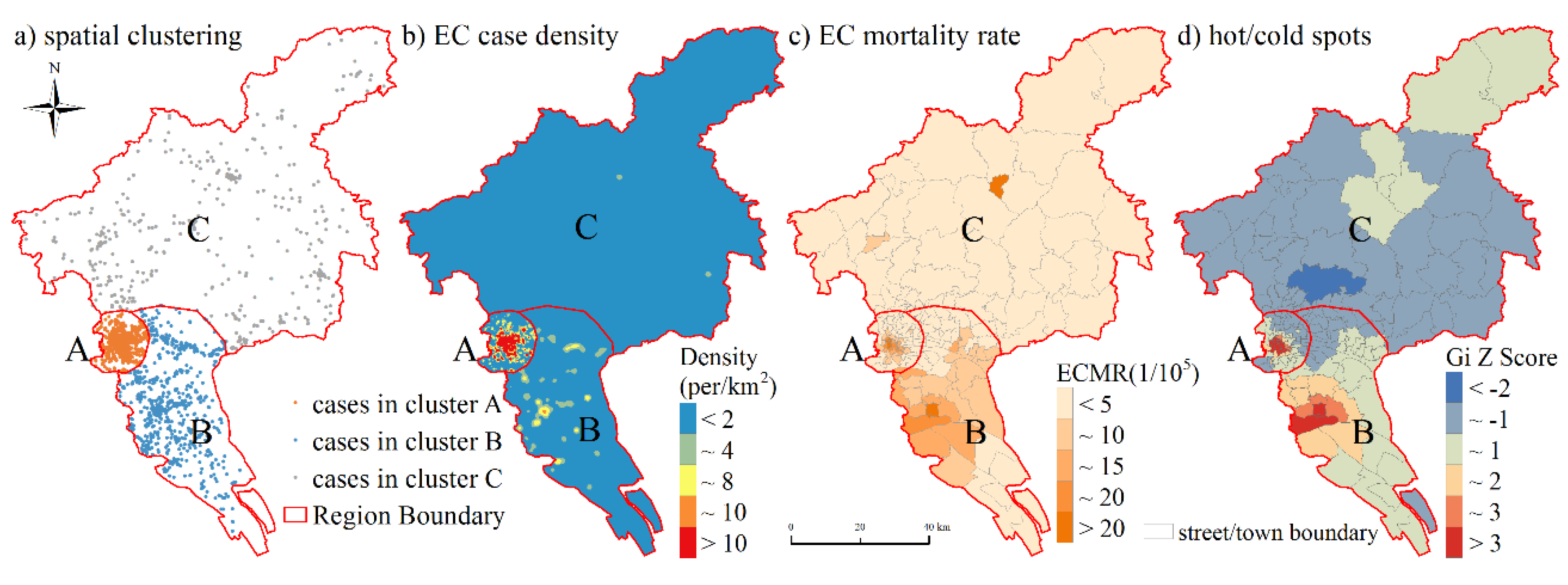
3.1. Temporal and Spatial Patterns of the EC Prevalence
3.2. Demographic Features and Health-Seeking Behaviors of EC Death Cases
3.3. Potential Influences of Socioeconomic Conditions on EC Epidemiological Features
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| EC | Esophageal Cancer |
| ECMR | Esophageal Cancer Mortality Rate |
| TMI | Top Medical Institution |
| MMI | Middle Medical Institution |
| BMI | Basic Medical Institution |
| RMIO | The Rate of Medical Institutions Occupancy per 10,000 |
| PMID | Proportion of the highest level of Medical Institution involved in the Diagnosis |
| PDP | Proportion of Death Place |
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.; Zheng, R.; Zhang, S.; Zuo, T.; Xia, C.; Zou, X.; Chen, W. Esophageal cancer statistics in China, 2011: Estimates based on 177 cancer registries. Thorac. Cancer 2016, 7, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, G.K.; Yanala, U.; Ravipati, A.; Follet, M.; Vijayakumar, M.; Are, C. Global trends in esophageal cancer. J. Surg. Oncol. 2017, 115, 564–579. [Google Scholar] [CrossRef] [PubMed]
- Pakzad, R.; Mohammadian-Hafshejani, A.; Khosravi, B.; Soltani, S.; Pakzad, I.; Mohammadian, M.; Salehiniya, H.; Momenimovahed, Z. The incidence and mortality of esophageal cancer and their relationship to development in Asia. Ann. Transl. Med. 2016, 4, 29. [Google Scholar]
- Huang, F.L.; Yu, S.J. Esophageal cancer: Risk factors, genetic association, and treatment. Asian J. Surg. 2018, 41, 210–215. [Google Scholar] [CrossRef]
- Zhang, X.; Pei, G.; Xu, Z.; Yao, W.; Feng, L. Meta-analysis on the risk factors of esophageal cancer in China. Mod. Prev. Med. 2009, 36, 819–822. [Google Scholar]
- Abnet, C.C.; Arnold, M.; Wei, W.Q. Epidemiology of Esophageal Squamous Cell Carcinoma. Gastroenterology 2018, 154, 360–373. [Google Scholar] [CrossRef]
- Zhang, N.; Yu, C.; Wen, D.; Chen, J.; Ling, Y.; Terajima, K.; Akazawa, K.; Shan, B.; Wang, S. Association of Nitrogen Compounds in Drinking Water with Incidence of Esophageal Squamous Cell Carcinoma in Shexian, China. Tohoku J. Exp. Med. 2012, 226, 11–17. [Google Scholar] [CrossRef]
- Yang, C.S. Research on esophageal cancer in China: A review. Cancer Res. 1980, 40, 2633–2644. [Google Scholar]
- Castro, C.; Peleteiro, B.; Lunet, N. Modifiable factors and esophageal cancer: A systematic review of published meta-analyses. J. Gastroenterol. 2018, 53, 37–51. [Google Scholar] [CrossRef]
- Chen, X.; Winckler, B.; Lu, M.; Cheng, H.; Yuan, Z.; Yang, Y.; Jin, L.; Ye, W. Oral microbiota and risk for esophageal squamous cell carcinoma in a high-risk area of China. PLoS ONE 2015, 10, e0143603. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Chen, X.; Yu, H.; Zhou, H.; Xu, S. Oral Microbiota as Promising Diagnostic Biomarkers for Gastrointestinal Cancer: A Systematic Review. OncoTargets Ther. 2019, 12, 11131–11144. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Wang, H.; Wang, Z.; Du, H.; Tao, D.; Mu, X.; Chen, H.; Lei, Y.; Matsuo, K.; Tajima, K. Risk factors for esophageal cancer: A case-control study in South-western China. Asian Pac. J. Cancer Prev. 2005, 6, 48–53. [Google Scholar] [PubMed]
- Tang, W.R.; Chen, Z.J.; Lin, K.; Su, M.; Au, W.W. Development of esophageal cancer in Chaoshan region, China: Association with environmental, genetic and cultural factors. Int. J. Hyg. Environ. Health 2015, 218, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Hajizadeh, B.; Jessri, M.; Moasheri, S.M.; Houshiar Rad, A.; Rashidkhani, B. Fruits and vegetables consumption and esophageal squamous cell carcinoma: A case-control study. Nutr. Cancer 2011, 63, 707–713. [Google Scholar] [CrossRef] [PubMed]
- Tran, P.N.; Taylor, T.H.; Klempner, S.J.; Zell, J.A. The impact of gender, race, socioeconomic status, and treatment on outcomes in esophageal cancer: A population-based analysis. J. Carcinog. 2017, 16, 3. [Google Scholar]
- Kou, K.; Baade, P.D.; Gatton, M.; Cramb, S.M.; Sun, J.; Lu, Z.; Fu, Z.; Chu, J.; Xu, A.; Guo, X. Individual and area-level socioeconomic inequalities in oesophageal cancer survival in Shandong Province, China: A multilevel analysis. Cancer Epidemiol. Prev. Biomark. 2019, 28, 1427–1434. [Google Scholar] [CrossRef]
- Bao, H.L.; Wang, N.; Wang, B.H. Study on Hospitalization Timeliness and Related Influencing Factors in Patients with Stomach and Esophagus Cancer in Rural Areas. Chin. Gen. Pract. 2014, 17, 2486–2489. [Google Scholar]
- Bus, P.; Aarts, M.J.; Lemmens, V.E.; van Oijen, M.G.; Creemers, G.-J.; Nieuwenhuijzen, G.A.; van Baal, J.W.; Siersema, P.D. The effect of socioeconomic status on staging and treatment decisions in esophageal cancer. J. Clin. Gastroenterol. 2012, 46, 833–839. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Hamilton, W.; Whiteman, D.C.; Jiang, J.Y.; Qiao, Y.; Fung, F.D.H.; Wang, H.H.X.; Chiu, P.W.Y.; Ng, E.K.W.; Wu, J.C.Y.; et al. Global Incidence and mortality of oesophageal cancer and their correlation with socioeconomic indicators temporal patterns and trends in 41 countries. Sci. Rep. 2018, 8, 4522. [Google Scholar] [CrossRef]
- Wu, C.C.; Chang, C.M.; Hsu, T.W.; Lee, C.H.; Chen, J.H.; Huang, C.Y.; Lee, C.C. The effect of individual and neighborhood socioeconomic status on esophageal cancer survival in working-age patients in Taiwan. Medicine 2016, 95, e4140. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Zheng, R.; Zhang, S.; Zeng, H.; Zuo, T.; Xia, C.; Yang, Z.; He, J. Cancer incidence and mortality in China in 2013: An analysis based on urbanization level. Chin. J. Cancer Res. 2017, 29, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.; Zhao, D.; Liu, Y.; Liu, Y.; Yuan, Z.; Wang, J.; Xue, F. The long-term spatial-temporal trends and burden of esophageal cancer in one high-risk area: A population-registered study in Feicheng, China. PLoS ONE 2017, 12, e0173211. [Google Scholar] [CrossRef]
- Chen, R.; Zheng, R.S.; Zhang, S.W.; Zeng, H.M.; Wang, S.M.; Sun, K.X.; Gu, X.Y.; Wei, W.Q.; He, J. Analysis of incidence and mortality of esophageal cancer in China, 2015. Chin. J. Prev. Med. 2019, 53, 1094–1097. [Google Scholar]
- Zhang, S.W.; Zheng, R.S.; Zuo, T.T.; Zeng, H.M.; Chen, W.Q.; He, J. Mortality and survival analysis of esophageal cancer in China. Chin. J. Oncol. 2016, 38, 709–715. [Google Scholar]
- Zuo, T.T.; Zheng, R.S.; Zeng, H.M.; Zhang, S.W.; Chen, W.Q.; He, J. Incidence and trend analysis of esophageal cancer in China. Chin. J. Oncol. 2016, 38, 703–708. [Google Scholar]
- Guo, K.; Zhou, M.G.; Shi, Y.Y.; Pan, X.P. Trends and characteristics of mortality of esophageal cancer in China, 2006–2012. Mod. Prev. Med. 2015, 42, 7–10. [Google Scholar]
- Gao, X.; Wang, Z.; Kong, C.; Yang, F.; Wang, Y.; Tan, X. Trends of esophageal cancer mortality in rural China from 1989 to 2013: An age-period-cohort analysis. Int. J. Environ. Res. Public Health 2017, 14, 218. [Google Scholar] [CrossRef]
- Guangzhou Statistics Bureau. Guangzhou Statistical Yearbook (2017); China Statistics Press: Beijing, China, 2018. [Google Scholar]
- Cui, X.; Li, S.; Wang, X.; Xue, X. Driving factors of urban land growth in Guangzhou and its implications for sustainable development. Front. Earth Sci. 2019, 13, 464–477. [Google Scholar] [CrossRef]
- Wu, J.; Zhao, Z.; Jiang, S.; Tao, L. The Research on Spatial Accessibility to Healthcare Services Resources in Tianhe, Guangzhou. In Proceedings of the International Conference on Smart Health, Shenzhen, China, July 2019; pp. 96–105. [Google Scholar]
- Zhou, C.; Tong, X.; Wang, J.; lai, S. Spatial differentiation and the formation mechanism of population aging in Guangzhou in 2000–2010. Geogr. Res. 2018, 37, 103–118. [Google Scholar]
- Fu, J.; Jiang, D.; Huang, Y. 1 km grid population dataset of China (2005, 2010). Glob. Chang. Res. Data Publ. Repos. 2014. [Google Scholar]
- Huang, Y.; Jiang, D.; Fu, J. 1 km grid GDP dataset of China (2005, 2010). Glob. Chang. Res. Data Publ. Repos. 2014. [Google Scholar]
- Cohen, D.A.; Farley, T.A.; Mason, K. Why is poverty unhealthy? Social and physical mediators. Soc. Sci. Med. 2003, 57, 1631–1641. [Google Scholar] [CrossRef]
- Mosadeghrad, A.M. Factors affecting medical service quality. Iran. J. Public Health 2014, 43, 210. [Google Scholar]
- Song, X.L. Incidence and Mortality of Malignant Tumors in Guangzhou, China, 1997–2006. Mater’s Thesis, Southern Medical University, Guangzhou City, China, 2007. [Google Scholar]
- Lin, Y.P.; Chu, H.J.; Wu, C.F.; Chang, T.K.; Chen, C.Y. Hotspot analysis of spatial environmental pollutants using kernel density estimation and geostatistical techniques. Int. J. Environ. Res. Public Health 2011, 8, 75–88. [Google Scholar] [CrossRef] [PubMed]
- Reynolds, D.A.; Rose, R.C. Robust text-independent speaker identification using Gaussian mixture speaker models. IEEE Trans. Speech Audio Process. 1995, 3, 72–83. [Google Scholar] [CrossRef]
- Anselin, L.; Getis, A. Spatial statistical analysis and geographic information systems. Ann. Reg. Sci. 1992, 26, 19–33. [Google Scholar] [CrossRef]
- Ord, J.K.; Getis, A. Local spatial autocorrelation statistics: Distributional issues and an application. Geogr. Anal. 1995, 27, 286–306. [Google Scholar] [CrossRef]
- Cui, C.; Wang, B.; Ren, H.; Wang, Z. Spatiotemporal Variations in Gastric Cancer Mortality and Their Relations to Influencing Factors in S County, China. Int. J. Environ. Res. Public Health 2019, 16, 784. [Google Scholar] [CrossRef]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Prettenhofer, P.; Weiss, R.; Dubourg, V.; et al. Scikit-learn: Machine learning in Python. J. Med. Learn. Res. 2011, 12, 2825–2830. [Google Scholar]
- Zheng, R.S.; Sun, K.; Zhang, S.W.; Zeng, H.M.; Zou, X.N.; Chen, R.; Gu, X.Y.; Wei, W.Q.; He, J. Report of cancer epidemiology in China, 2015. Chin. J. Oncol. 2019, 41, 19–28. [Google Scholar]
- Zhang, Y.H.; Li, Y.Y.; He, J.Y.; Liang, B.H.; Yu, C.; Zhang, W.W.; Huang, J. Food consumption and nutrients intake among residents in Guangzhou city. Chin. J. Public Health 2017, 33, 969–971. [Google Scholar]
- Ma, Z.; Yin, S.; Qiao, W.; Li, Z.; Wu, Q. Spatial Equilibrium State and Its Time Evolution of Medical Health Resource Supply Level in China. Sci. Geogr. Sin. 2018, 38, 869–876. [Google Scholar]
- Qi, L.S. Income, Income Inequality and Health: The Impacts of Rural-urban Gap and Occupational Status. Econ. Res. J. 2006, 11, 16–26. [Google Scholar]
- Streeter, J.L. Socioeconomic factors affecting food consumption and nutrition in China: Empirical evidence during the 1989–2009 period. Chin. Econ. 2017, 50, 168–192. [Google Scholar] [CrossRef]
- He, X.T.; Fan, C.X.; Liu, G.N.; Ma, S.B. Cognition and Behavior About Esophagus Carcinoma Among Undergraduates in 6 Universities of Guangzhou. Chin. J. Sch. Health 2009, 30, 30–32. [Google Scholar]
- Van Vliet, E.; Eijkemans, M.; Steyerberg, E.; Kuipers, E.; Tilanus, H.; van der Gaast, A.; Siersema, P. The role of socio-economic status in the decision making on diagnosis and treatment of oesophageal cancer in The Netherlands. Br. J. Cancer 2006, 95, 1180–1185. [Google Scholar] [CrossRef]
- Wei, W.Q.; Chen, Z.F.; He, Y.T.; Feng, H.; Hou, J.; Lin, D.M.; Li, X.Q.; Guo, C.L.; Li, S.S.; Wang, G.Q.; et al. Long-Term Follow-Up of a Community Assignment, One-Time Endoscopic Screening Study of Esophageal Cancer in China. J. Clin. Oncol. 2015, 33, 1951–1957. [Google Scholar] [CrossRef]

| Influencing Factors | Dataset | Time | Resolution | Source |
|---|---|---|---|---|
| Population density | Gridded population density | 2015 | 1 km | www.resdc.cn |
| GDP density | Gridded GDP density | 2015 | 1 km | |
| Medical resources | Medical institutions | 2016 | Vector (point) | data.gz.gov.cn; wjw.gz.gov.cn |
| Ageing degree | The Sixth National Population Census | 2010 | Street/town | www.stats.gov.cn |
| Region | % of EC Cases | Density (Cases/km2) | Crude ECMR (1/105) | Gender Ratio (Male to Female) | Mean Value of Death Age (Year) | Mean/Median Value of Temporal Interval between Diagnosis and Death (Month) |
|---|---|---|---|---|---|---|
| Region A | 44.17% | 4.69 | 6.41 | 5.06:1 | 67.4 | 13.5/8.0 |
| Region B | 34.83% | 0.55 | 5.51 | 10.49:1 | 63.9 | 15.7/12.0 |
| Region C | 21.00% | 0.09 | 2.56 | 5.85:1 | 65.9 | 13.9/8.0 |
| Guangzhou city | 100% | 0.33 | 4.71 | 6.46:1 | 65.8 | 14.4/9.0 |
| Region | Death_Hosp | Death_Home | Death_Other | Death_Total | |
|---|---|---|---|---|---|
| Guangzhou city | Diag_TMI | 903 | 689 | 38 | 1630 (67.66%) |
| Diag_MMI | 192 | 254 | 17 | 463 (19.22%) | |
| Diag_BMI | 68 | 216 | 14 | 298 (12.37%) | |
| Diag_Other | 2 | 15 | 1 | 18 (0.75%) | |
| Diag_Total | 1165 (48.36%) | 1174 (48.73%) | 70 (2.91%) | 2409 (100%) | |
| Region A | Diag_TMI | 681 | 141 | 27 | 849(79.79%) |
| Diag_MMI | 127 | 27 | 11 | 165 (15.51%) | |
| Diag_BMI | 16 | 24 | 6 | 46 (4.32%) | |
| Diag_Other | 1 | 3 | 0 | 4 (0.38%) | |
| Diag_Total | 825 (77.54%) | 195 (18.33%) | 44 (4.14%) | 1064 (100%) | |
| Region B | Diag_TMI | 136 | 363 | 4 | 503 (59.95%) |
| Diag_MMI | 41 | 96 | 4 | 141 (16.81%) | |
| Diag_BMI | 37 | 139 | 5 | 181 (21.57%) | |
| Diag_Other | 1 | 12 | 1 | 14 (1.67%) | |
| Diag_Total | 215 (25.63%) | 610 (72.71%) | 14 (1.67%) | 839 (100.00%) | |
| Region C | Diag_TMI | 86 | 185 | 7 | 278 (54.94%) |
| Diag_MMI | 24 | 131 | 2 | 157 (31.03%) | |
| Diag_BMI | 15 | 53 | 3 | 71 (14.03%) | |
| Diag_Other | 0 | 0 | 0 | 0(0.00%) | |
| Diag_Total | 125 (24.70%) | 369 (72.92%) | 12 (2.37%) | 506 (100.00%) |
| POP | GDP | DistTMI | Beds | RMIOTMI | RMIOMMI | RMIOBMI | RMIOall | |
|---|---|---|---|---|---|---|---|---|
| Ageing | 0.557 ** | 0.480 ** | −0.084 | 0.324 ** | 0.311 ** | 0.138 | 0.291 ** | 0.279 ** |
| POP | 1 | 0.891 ** | −0.480 ** | 0.264 ** | 0.313 ** | 0.023 | 0.118 | 0.131 |
| GDP | 1 | −0.376 ** | 0.236 ** | 0.260 ** | 0.050 | 0.177 * | 0.161 * | |
| DistTMI | 1 | −0.332 ** | −0.284** | −0.204 ** | −0.232 ** | −0.296 ** | ||
| Beds | 1 | 0.870** | 0.610 ** | 0.412 ** | 0.776 ** | |||
| RMIOTMI | 1 | 0.140 | 0.216 ** | 0.401 ** | ||||
| RMIOMMI | 1 | 0.423 ** | 0.893 ** | |||||
| RMIOBMI | 1 | 0.738 ** | ||||||
| RMIOall | 1 | |||||||
| PMIDTMI | 0.387 ** | 0.313 ** | −0.444 ** | 0.178 * | 0.187* | 0.058 | 0.036 | 0.095 |
| PMIDMMI | −0.193 * | −0.200 ** | 0.371 ** | −0.082 | −0.099 | −0.002 | −0.072 | −0.052 |
| PMIDBMI | −0.320 ** | −0.210 ** | 0.230 ** | −0.151 * | −0.147 | −0.073 | 0.027 | −0.072 |
| PMIDother | −0.110 | −0.071 | 0.050 | −0.035 | −0.043 | −0.003 | 0.010 | −0.008 |
| PDPhosp | 0.640 ** | 0.541 ** | −0.487 ** | 0.310 ** | 0.284** | 0.170* | 0.194 * | 0.256 ** |
| PDPhome | −0.644 ** | −0.554 ** | 0.521 ** | −0.311 ** | −0.281** | −0.166* | −0.198 ** | −0.255 ** |
| PDPother | 0.028 | 0.083 | −0.137 | −0.001 | 0.001 | −0.007 | 0.035 | 0.010 |
| Region | POP | GDP | Ageing |
|---|---|---|---|
| Guangzhou City (N = 170) | 0.155 * | 0.093 (p = 0.227) | 0.466 ** |
| Control Ageing | −0.143 (p = 0.064) | −0.168 * (p = 0.029) | / |
| Region A (N = 61) | −0.105 (p = 0.419) | −0.132 (p = 0.312) | 0.565 ** |
| Control Ageing | −0.470 ** | −0.426** | / |
| Region B (N = 54) | −0.532 ** | −0.529 ** | 0.173 (p = 0.211) |
| Control Ageing | −0.524 ** | −0.511 ** | / |
| Region C (N = 55) | −0.140 (p = 0.308) | −0.105 (p = 0.448) | 0.003 (p = 0.982) |
| Control Ageing | −0.190 (p = 0.169) | −0.127 (p = 0.359) | / |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cui, C.; Dong, H.; Ren, H.; Lin, G.; Zhao, L. Characterization of Esophageal Cancer and Its Association with Influencing Factors in Guangzhou City, China. Int. J. Environ. Res. Public Health 2020, 17, 1498. https://doi.org/10.3390/ijerph17051498
Cui C, Dong H, Ren H, Lin G, Zhao L. Characterization of Esophageal Cancer and Its Association with Influencing Factors in Guangzhou City, China. International Journal of Environmental Research and Public Health. 2020; 17(5):1498. https://doi.org/10.3390/ijerph17051498
Chicago/Turabian StyleCui, Cheng, Hang Dong, Hongyan Ren, Guozhen Lin, and Lu Zhao. 2020. "Characterization of Esophageal Cancer and Its Association with Influencing Factors in Guangzhou City, China" International Journal of Environmental Research and Public Health 17, no. 5: 1498. https://doi.org/10.3390/ijerph17051498
APA StyleCui, C., Dong, H., Ren, H., Lin, G., & Zhao, L. (2020). Characterization of Esophageal Cancer and Its Association with Influencing Factors in Guangzhou City, China. International Journal of Environmental Research and Public Health, 17(5), 1498. https://doi.org/10.3390/ijerph17051498






