Association between Neighborhood Environment and Quality of Sleep in Older Adult Residents Living in Japan: The JAGES 2010 Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
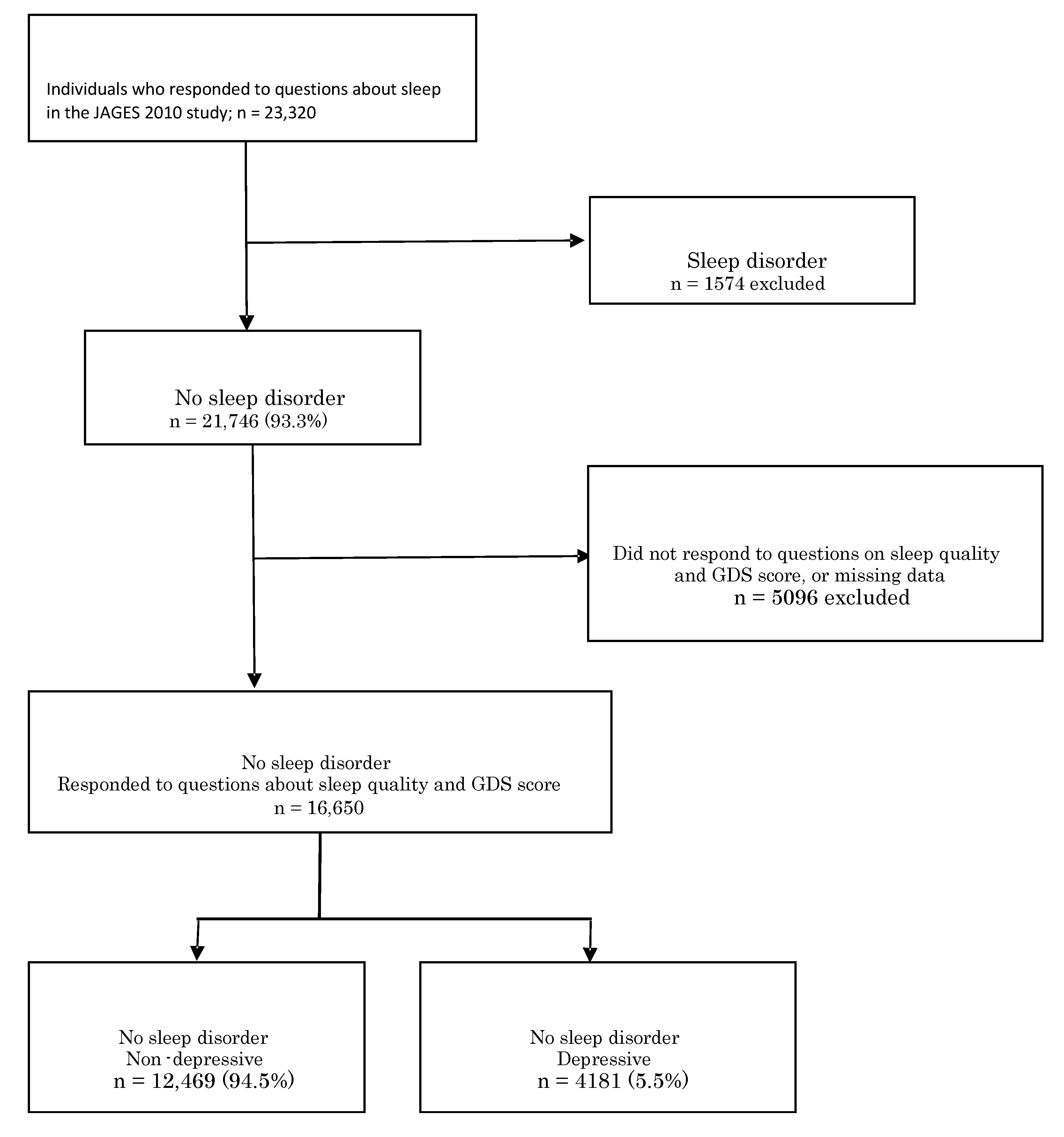
2.1. Participants
2.2. Definition of Sleep Quality
2.3. Explanatory Variables
2.3.1. Individual-Level Variables
2.3.2. Neighborhood-Level Variables
2.4. Statistical Analysis
2.5. Ethical Considerations
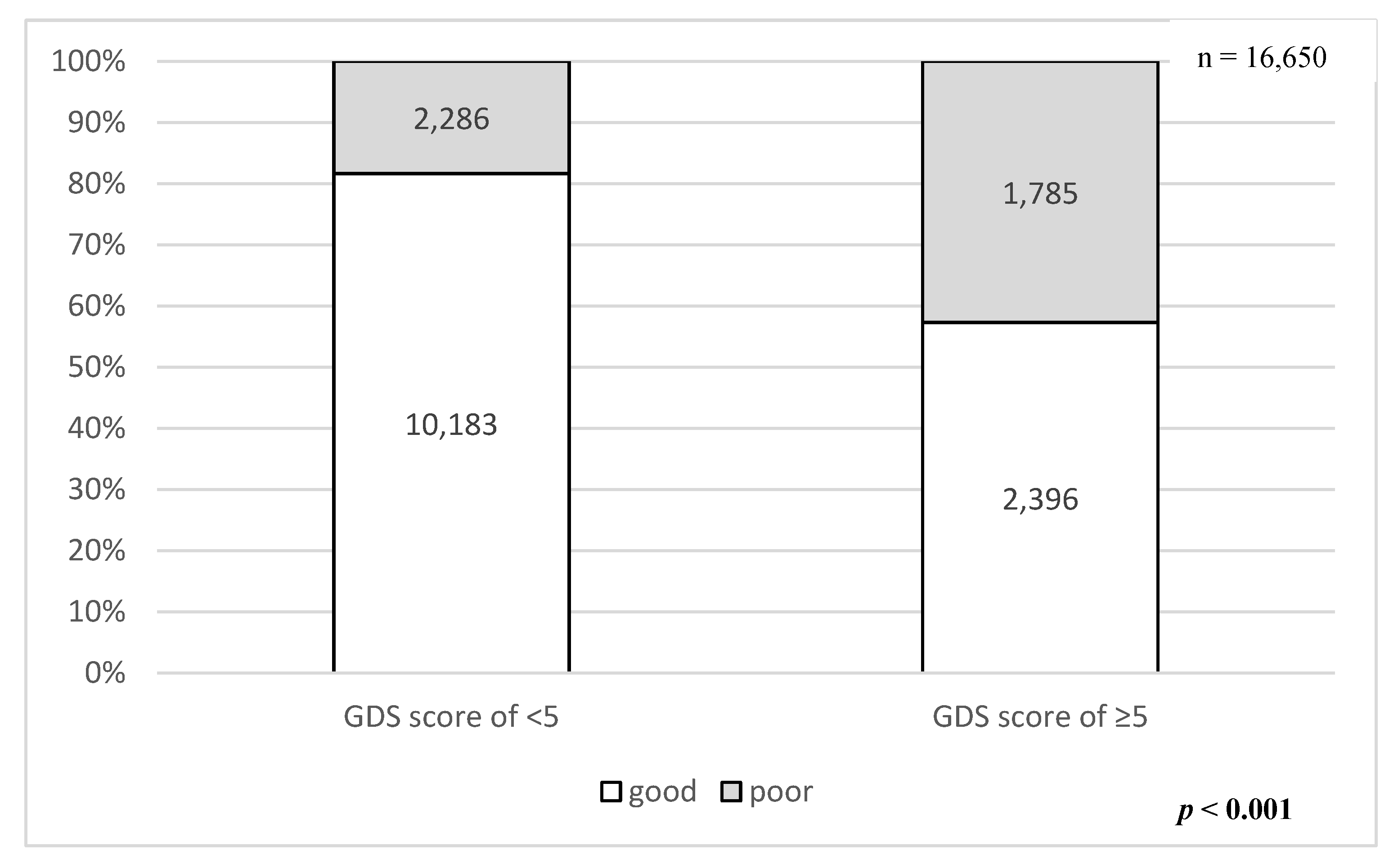
3. Results
3.1. Characteristics of the Respondents
3.2. Variety of Sleep Quality among the Neighborhood Level
3.3. Individual and Neighborhood Factors Associated with Sleep Quality
3.3.1. Whole Respondents
3.3.2. Non-Depressive Respondents (GDS Score of <5)
3.3.3. Depressive Respondents (GDS Score of ≥5)
4. Discussion
Strengths and Limitations of the Study
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Luyster, F.F.S. Sleep: A Health Imperative. Sleep 2012, 35, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.Y.; Kang, G.; Kim, S.W.; Kim, J.M.; Yoon, J.S.; Shin, I.S. Associations between sleep duration and abnormal serum lipid levels: Data from the Korean National Health and Nutrition Examination Survey (KNHANES). Sleep Med. 2016, 24, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.C. The Link of Self-Reported Insomnia Symptoms and Sleep Duration with Metabolic Syndrome: A Chinese Population-Based Study. Sleep 2016, 39, 1261–1266. [Google Scholar] [CrossRef] [PubMed]
- Baglioni, C.; Battagliese, G.; Feige, B.; Spiegelhalder, K.; Nissen, C.; Voderholzer, U.; Lombardo, C.; Riemann, D. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 2011, 135, 10–19. [Google Scholar] [CrossRef] [PubMed]
- Hidaka, B.H. Depression as a disease of modernity: Explanations for increasing prevalence. J. Affect. Disord. 2012, 140, 205–214. [Google Scholar] [CrossRef]
- Cable, N.; Chandola, T.; Aida, J.; Sekine, M.; Netuveli, G. Can sleep disturbance influence changes in mental health status? Longitudinal research evidence from ageing studies in England and Japan. Sleep Med. 2017, 30, 216–221. [Google Scholar] [CrossRef]
- Tafaro, L.; Cicconetti, P.; Baratta, A.; Brukner, N.; Ettorre, E.; Marigliano, V.; Cacciafesta, M. Sleep quality of centenarians: Cognitive and survival implications. Arch. Gerontol. Geriatr. 2007, 44, 385–389. [Google Scholar] [CrossRef]
- Suh, S.W.; Han, J.W.; Lee, J.R.; Byun, S.; Kwon, S.J.; Oh, S.H.; Lee, K.H.; Han, G.; Hong, J.W.; Kwak, K.P.; et al. Sleep and Cognitive Decline: A Prospective Non-demented Elderly Cohort Study. Ann. Neurol. 2018, 83, 472–482. [Google Scholar] [CrossRef]
- Sexton, C.E.; Zsoldos, E.; Filippini, N.; Griffanti, L.; Winkler, A.; Mahmood, A.; Allan, C.L.; Topiwala, A.; Kyle, S.D.; Spiegelhalder, K.; et al. Associations between self-reported sleep quality and white matter in community-dwelling older adults: A prospective cohort study. Hum. Brain Mapp. 2017, 38, 5465–5473. [Google Scholar] [CrossRef]
- Liu, X.; Uchiyama, M.; Kim, K.; Okawa, M.; Shibui, K.; Kudo, Y.; Doi, Y.; Minowa, M.; Ogihara, R. Sleep loss and daytime sleepiness in the general adult population of Japan. Psychiatry Res. 2000, 93, 1–11. [Google Scholar] [CrossRef]
- Luo, J.; Zhu, G.; Zhao, Q.; Guo, Q.; Meng, H.; Hong, Z.; Ding, D. Prevalence and risk factors of poor sleep quality among chinese elderly in an urban community: Results from the Shanghai aging study. PLoS ONE 2013, 8, e81261. [Google Scholar] [CrossRef] [PubMed]
- Cochen, V.; Arbus, C.; Soto, M.E.; Villars, H.; Tiberge, M.; Montemayor, T.; Hein, C.; Veccherini, M.F.; Onen, S.H.; Ghorayeb, I. Sleep disorders and their impacts on healthy, dependent, and frail older adults. J. Nutr. Health Aging 2009, 13, 322–329. [Google Scholar] [CrossRef] [PubMed]
- Stone, K.L.; Xiao, Q. Impact of Poor Sleep on Physical and Mental Health in Older Women. Sleep Med. Clin. 2018, 13, 457–465. [Google Scholar] [CrossRef] [PubMed]
- WHO. Adelaide Statement on Health in All Policies Moving Towards a Shared Governance for Health and Well-Being; WHO: Geneva, Switzerland, 2010; pp. 1–4. [Google Scholar]
- Pugh, C.R.; Nguyen, K.T.; Gonyea, J.L.; Fleshner, M.; Watkins, L.R.; Maier, S.F.; Rudy, J.W. Role of interleukin-1 beta in impairment of contextual fear conditioning caused by social isolation. Behav. Brain Res. 1999, 106, 109–118. [Google Scholar] [CrossRef]
- Paine, S.J.; Harris, R.; Cormack, D.; Stanley, J. Racial Discrimination and Ethnic Disparities in Sleep Disturbance: The 2002/03 New Zealand Health Survey. Sleep 2016, 39, 477–485. [Google Scholar] [CrossRef]
- Gu, D.; Sautter, J.; Pipkin, R.; Zeng, Y. Sociodemographic and health correlates of sleep quality and duration among very old Chinese. Sleep 2010, 33, 601–610. [Google Scholar] [CrossRef] [PubMed]
- Nomura, K.; Yamaoka, K.; Nakao, M.; Yano, E. Social determinants of self-reported sleep problems in South Korea and Taiwan. J. Psychosom. Res. 2010, 69, 435–440. [Google Scholar] [CrossRef]
- Johnson, D.A.; Lisabeth, L.; Hickson, D.; Johnson-Lawrence, V.; Samdarshi, T.; Taylor, H.; Diez Roux, A.V. The Social Patterning of Sleep in African Americans: Associations of Socioeconomic Position and Neighborhood Characteristics with Sleep in the Jackson Heart Study. Sleep 2016, 39, 1749–1759. [Google Scholar] [CrossRef]
- Bassett, E.; Moore, S. Neighbourhood disadvantage, network capital and restless sleep: Is the association moderated by gender in urban-dwelling adults? Soc. Sci. Med. 2014, 108, 185–193. [Google Scholar] [CrossRef]
- Kondo, K. Progress in Aging Epidemiology in Japan: The JAGES Project. J. Epidemiol. 2016, 26, 331–336. [Google Scholar] [CrossRef]
- Kondo, N. Socioeconomic disparities and health: Impacts and pathways. J. Epidemiol. 2012, 22, 2–6. [Google Scholar] [CrossRef]
- Wallace, M.L.; Stone, K.; Smagula, S.F.; Hall, M.H.; Simsek, B.; Kado, D.M.; Redline, S.; Vo, T.N.; Buysse, D.J.; Osteoporotic Fractures in Men Study Research Group. Which Sleep Health Characteristics Predict All-Cause Mortality in Older Men? An Application of Flexible Multivariable Approaches. Sleep 2018, 41. [Google Scholar] [CrossRef] [PubMed]
- Tani, Y.; Sasaki, Y.; Haseda, M.; Kondo, K.; Kondo, N. Eating alone and depression in older men and women by cohabitation status: The JAGES longitudinal survey. Age Ageing 2015, 44, 1019–1026. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, Y.; Aida, J.; Tsuji, T.; Miyaguni, Y.; Tani, Y.; Koyama, S.; Matsuyama, Y.; Sato, Y.; Tsuboya, T.; Nagamine, Y.; et al. Does the Type of Residential Housing Matter for Depressive Symptoms in the Aftermath of a Disaster? Insights from the Great East Japan Earthquake and Tsunami. Am. J. Epidemiol. 2017, 187, 455–464. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.A.; Simonelli, G.; Moore, K.; Billings, M.; Mujahid, M.S.; Rueschman, M.; Kawachi, I.; Redline, S.; Diez Roux, A.V.; Patel, S.R. The Neighborhood Social Environment and Objective Measures of Sleep in the Multi-Ethnic Study of Atherosclerosis. Sleep 2017, 40. [Google Scholar] [CrossRef] [PubMed]
- Saito, M.; Kondo, K.; Kondo, N.; Abe, A.; Ojima, T.; Suzuki, K. Relative deprivation, poverty, and subjective health: JAGES cross-sectional study. PLoS ONE 2014, 9, e111169. [Google Scholar] [CrossRef] [PubMed]
- Fujihara, S.; Tsuji, T.; Miyaguni, Y.; Aida, J.; Saito, M.; Koyama, S.; Kondo, K. Does Community-Level Social Capital Predict Decline in Instrumental Activities of Daily Living? A JAGES Prospective Cohort Study. Int. J. Environ. Res. Public Health 2019, 16, 828. [Google Scholar] [CrossRef] [PubMed]
- Hanibuchi, T.; Murata, Y.; Ichida, Y.; Hirai, H.; Kondo, K. An evaluation of an area’s social capital by public health nurses. Jpn. J. Public Health 2008, 55, 716–723. [Google Scholar]
- Zhang, J.; Kai, F.Y. What’s the relative risk?: A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 1998, 280, 1690–1691. [Google Scholar] [CrossRef]
- Peltzer, K.; Pengpid, S. Loneliness correlates and associations with health variables in the general population in Indonesia. Int. J. Ment. Health Syst. 2019, 13, 24. [Google Scholar] [CrossRef]
- Balfour, J.L.; Kaplan, G.A. Neighborhood environment and loss of physical function in older adults: Evidence from the Alameda County Study. Am. J. Epidemiol. 2002, 155, 507–515. [Google Scholar] [CrossRef] [PubMed]
- Murayama, H.; Wakui, T.; Arami, R.; Sugawara, I.; Yoshie, S. Contextual effect of different components of social capital on health in a suburban city of the greater Tokyo area: A multilevel analysis. Soc. Sci. Med. 2012, 75, 2472–2480. [Google Scholar] [CrossRef] [PubMed]
- Hanibuchi, T.; Kondo, K.; Nakaya, T.; Shirai, K.; Hirai, H.; Kawachi, I. Does walkable mean sociable? Neighborhood determinants of social capital among older adults in Japan. Health Place 2012, 18, 229–239. [Google Scholar] [CrossRef] [PubMed]
- Okabe, D.; Tsuji, T.; Hanazato, M.; Miyaguni, Y.; Asada, N.; Kondo, K. Neighborhood Walkability in Relation to Knee and Low Back Pain in Older People: A Multilevel Cross-Sectional Study from the JAGES. Int. J. Environ. Res. Public Health 2019, 16, 4598. [Google Scholar] [CrossRef]
- Murayama, H.H. Contextual effect of neighborhood environment on homebound elderly in a Japanese community. Arch. Gerontol. Geriatr. 2012, 54, 67–71. [Google Scholar] [CrossRef]
- Reid, K.J.; Baron, K.G.; Lu, B.; Naylor, E.; Wolfe, L.; Zee, P.C. Aerobic exercise improves self-reported sleep and quality of life in older adults with insomnia. Sleep Med. 2010, 11, 934–940. [Google Scholar] [CrossRef]
- Driver, H.S.; Taylor, S.R. Exercise and sleep. Sleep Med. Rev. 2000, 4, 387–402. [Google Scholar] [CrossRef]
- Badger, T.A. Depression, Physical Health Impairment and Service Use Among Older Adults. Public Health Nurs. 1998, 15, 136–145. [Google Scholar] [CrossRef]
- Cabinet, O. The Section 1st, Annual Report on the Aging Society, 2018; Cabinet: Tokyo, Japan, 2019; Volume 2019. [Google Scholar]
- Ministry of Health, Labour and Welfare. National Health and Nutrition Survey; The National Institute of Health and Nutrition: Tokyo, Japan, 2002; Volume 2017.
- Murayama, H.; Fujiwara, Y.; Kawachi, I. Social capital and health: A review of prospective multilevel studies. J. Epidemiol. 2012, 22, 179–187. [Google Scholar] [CrossRef]
- Kawachi, I.; Kennedy, B.P.; Glass, R. Social capital and self-rated health: A contextual analysis. Am. J. Public Health 1999, 89, 1187–1193. [Google Scholar] [CrossRef]
- Putnam, R.D. Bowling Alone: The Collapse and Revival of American Community; Simon & Schuster Paperbacks: New York, NY, USA, 2000; p. 541. [Google Scholar]
- Desantis, A.S.; Diez Roux, A.V.; Moore, K.; Baron, K.G.; Mujahid, M.S.; Nieto, F.J. Associations of neighborhood characteristics with sleep timing and quality: The Multi-Ethnic Study Of Atherosclerosis. Sleep 2013, 36, 1543–1551. [Google Scholar] [CrossRef]
- Hikichi, H.; Kondo, N.; Kondo, K.; Aida, J.; Takeda, T.; Kawachi, I. Effect of a community intervention programme promoting social interactions on functional disability prevention for older adults: Propensity score matching and instrumental variable analyses, JAGES Taketoyo study. J. Epidemiol. Community Health 2015, 69, 905–910. [Google Scholar] [CrossRef]
- Van Cauwenberg, J.; De Bourdeaudhuij, I.; De Meester, F.; Van Dyck, D.; Salmon, J.; Clarys, P.; Deforche, B. Relationship between the physical environment and physical activity in older adults: A systematic review. Health Place 2011, 17, 458–469. [Google Scholar] [CrossRef] [PubMed]
- Hanibuchi, T.; Nakaya, T.; Yonejima, M.; Honjo, K. Perceived and objective measures of neighborhood walkability and physical activity among adults in japan: A multilevel analysis of a nationally representative sample. Int. J. Environ. Res. Public Health 2015, 12, 13350–13364. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, S.; Yamaoka, K.; Inoue, M.; Muto, S.; Teikyo Ishinomaki Research Group; Health and Life Revival Council in the Ishinomaki district (RCI). Social ties may play a critical role in mitigating sleep difficulties in disaster-affected communities: A cross-sectional study in the Ishinomaki area, Japan. Sleep 2014, 37, 137–145. [Google Scholar] [PubMed]
- Stamatakis, K.A.; Kaplan, G.A.; Roberts, R.E. Short Sleep Duration Across Income, Education, and Race/Ethnic Groups: Population Prevalence and Growing Disparities During 34 Years of Follow-Up. Ann. Epidemiol. 2007, 17, 948–955. [Google Scholar] [CrossRef]
- Scott-Lennix, J.A.; Lennox, R.D. Sex—Race differences in social support and depression in older low-income adults. In Structural Equation Modeling: Concepts, Issues, and Applications; Hoyle, R.H., Ed.; Sage Publications, Inc.: Thousand Oaks, CA, USA, 1995. [Google Scholar]
- Inoue, Y.; Stickley, A.; Yazawa, A.; Shirai, K.; Amemiya, A.; Kondo, N.; Kondo, K.; Ojima, T.; Hanazato, M.; Suzuki, N. Neighborhood characteristics and cardiovascular risk among older people in Japan: Findings from the JAGES project. PLoS ONE 2016, 11, e0164525. [Google Scholar] [CrossRef]
- Haseda, M.; Kondo, N.; Ashida, T.; Tani, Y.; Takagi, D.; Kondo, K. Community social capital, built environment, and income-based inequality in depressive symptoms among older people in Japan: An ecological study from the JAGES project. J. Epidemiol. 2017, 28, 108–116. [Google Scholar] [CrossRef]
- Gero, K.; Kondo, K.; Kondo, N.; Shirai, K.; Kawachi, I. Associations of relative deprivation and income rank with depressive symptoms among older adults in Japan. Soc. Sci. Med. 2017, 189, 138–144. [Google Scholar] [CrossRef]
- Yu, J.; Rawtaer, I.; Fam, J.; Jiang, M.J.; Feng, L.; Kua, E.H.; Mahendran, R. Sleep correlates of depression and anxiety in an elderly Asian population. Psychogeriatr. Off. J. Jpn. Psychogeriatr. Soc. 2016, 16, 191–195. [Google Scholar] [CrossRef]
- Sukegawa, T.; Itoga, M.; Seno, H.; Miura, S.; Inagaki, T.; Saito, W.; Uegaki, J.; Miyaoka, T.; Momose, I.; Kasahara, K.; et al. Sleep disturbances and depression in the elderly in Japan. Psychiatry Clin. Neurosci. 2003, 57, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Spira, A.P.; Kaufmann, C.N.; Kasper, J.D.; Ohayon, M.M.; Rebok, G.W.; Skidmore, E.; Parisi, J.M.; Reynolds, C.F., 3rd. Association between insomnia symptoms and functional status in U.S. older adults. J. Gerontol. Ser. B Psychol. Sci. Soc. Sci. 2014, 69, S35–S41. [Google Scholar]
- Kim, W.J.; Joo, W.T.; Baek, J.; Sohn, S.Y.; Namkoong, K.; Youm, Y.; Kim, H.C.; Park, Y.R.; Chu, S.H.; Lee, E. Factors Associated with Insomnia among the Elderly in a Korean Rural Community. Psychiatry Investig. 2017, 14, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Dehghankar, L.; Ghorbani, A.; Yekefallah, L.; Hajkarimbaba, M.; Rostampour, A. Association of sleep quality with socio-demographic characteristics in elderly referred to health centers in Qazvin, Iran. Sleep Hypn. 2018, 20, 227–232. [Google Scholar] [CrossRef]
- Murayama, H.; Fujiwara, T.; Tani, Y.; Amemiya, A.; Matsuyama, Y.; Nagamine, Y.; Kondo, K. Long-term Impact of Childhood Disadvantage on Late-Life Functional Decline Among Older Japanese: Results From the JAGES Prospective Cohort Study; Oxford University Press: Oxford, UK, 2018; Volume 73, pp. 973–979. [Google Scholar]
- Troxel, W.M.; Buysse, D.J.; Matthews, K.A.; Kip, K.E.; Strollo, P.J.; Hall, M.; Drumheller, O.; Reis, S.E. Sleep symptoms predict the development of the metabolic syndrome. Sleep 2010, 33, 1633–1640. [Google Scholar] [CrossRef]
- Reichmuth, K.J.; Austin, D.; Skatrud, J.B.; Young, T. Association of sleep apnea and type II diabetes: A population-based study. Am. J. Respir. Crit. Care Med. 2005, 172, 1590–1595. [Google Scholar] [CrossRef]
- Kawakami, N.; Takatsuka, N.; Shimizu, H. Sleep disturbance and onset of type 2 diabetes. Diabetes Care 2004, 27, 282–283. [Google Scholar] [CrossRef]
- Yanagi, N.; Hata, A.; Kondo, K.; Fujiwara, T. Association between childhood socioeconomic status and fruit and vegetable intake among older Japanese: The JAGES 2010 study. Prev. Med. 2018, 106, 130–136. [Google Scholar] [CrossRef]
| Characteristic | Variable | Good (n = 12,579) | Poor (n = 4071) | |||
|---|---|---|---|---|---|---|
| n | % | n | % | p * | ||
| Sex | male | 6227 | 49.5 | 1875 | 46.06 | <0.001 |
| female | 6352 | 50.5 | 2196 | 53.94 | ||
| Age (years) | 65–69 | 3948 | 31.39 | 1356 | 33.31 | 0.002 |
| 70–74 | 3662 | 29.11 | 1249 | 30.68 | ||
| 75–79 | 2663 | 21.17 | 807 | 19.82 | ||
| 80–84 | 1556 | 12.37 | 446 | 10.96 | ||
| ≥85 | 750 | 5.96 | 213 | 5.23 | ||
| Living alone | no | 11,089 | 88.15 | 3460 | 84.99 | <0.001 † |
| yes | 1355 | 10.77 | 562 | 13.8 | ||
| missing | 135 | 1.07 | 49 | 1.2 | ||
| Self-rated health | fair | 10,729 | 85.29 | 2732 | 67.11 | <0.001 † |
| poor | 1668 | 13.26 | 1276 | 31.34 | ||
| missing | 182 | 1.45 | 63 | 1.55 | ||
| Job | having | 2996 | 23.82 | 757 | 18.59 | <0.001 † |
| no | 8581 | 68.22 | 2969 | 72.93 | ||
| missing | 1002 | 7.97 | 345 | 8.47 | ||
| Equivalent income | <200 | 6783 | 53.92 | 2525 | 62.02 | <0.001 † |
| (million yen) | 200–400 | 4402 | 34.99 | 1244 | 30.56 | |
| ≥400 | 1394 | 11.08 | 302 | 7.42 | ||
| Education (year) | <6 | 247 | 1.96 | 105 | 2.58 | <0.001 |
| 6–9 | 5375 | 42.73 | 1868 | 45.89 | ||
| 10–12 | 4517 | 35.91 | 1377 | 33.82 | ||
| ≥13 | 2256 | 17.93 | 641 | 15.75 | ||
| other | 59 | 0.47 | 32 | 0.79 | ||
| missing | 125 | 0.99 | 48 | 1.18 | ||
| Walking time (min) | <60 | 7780 | 61.85 | 2778 | 68.24 | <0.001 † |
| ≥60 | 4162 | 33.09 | 1082 | 26.58 | ||
| missing | 637 | 5.06 | 211 | 5.18 | ||
| Treatment | yes | 8378 | 66.6 | 2917 | 71.65 | <0.001 † |
| no | 3316 | 26.36 | 843 | 20.71 | ||
| missing | 885 | 7.04 | 311 | 7.64 | ||
| Depressive status | GDS score of <5 | 10,183 | 80.95 | 2286 | 56.15 | <0.001 |
| GDS score of ≥5 | 2396 | 19.05 | 1785 | 43.85 | ||
| Volunteer group | ≥ 1/month | 8818 | 70.1 | 2931 | 72 | 0.027 † |
| < 1/month | 1198 | 9.52 | 338 | 8.3 | ||
| missing | 2563 | 20.38 | 802 | 19.7 | ||
| Sports group | ≥ 1/month | 7930 | 63.04 | 2720 | 66.81 | <0.001 † |
| < 1/month | 2540 | 20.19 | 660 | 16.21 | ||
| missing | 2109 | 16.77 | 691 | 16.97 | ||
| Hobby activity | ≥ 1/month | 6675 | 53.06 | 2305 | 56.62 | <0.001 † |
| < 1/month | 4074 | 32.39 | 1173 | 28.81 | ||
| missing | 1830 | 14.55 | 593 | 14.57 | ||
| Community trust | very | 9136 | 72.63 | 2528 | 62.1 | <0.001 † |
| slightly | 2931 | 23.3 | 1400 | 34.39 | ||
| missing | 512 | 4.07 | 143 | 3.51 | ||
| Norms of reciprocity | very | 7374 | 58.62 | 1959 | 48.12 | <0.001 † |
| slightly | 4652 | 36.98 | 1967 | 48.32 | ||
| missing | 553 | 4.4 | 145 | 3.56 | ||
| Community attachment | very | 10,590 | 84.19 | 3023 | 74.26 | <0.001 † |
| slightly | 1783 | 14.17 | 1003 | 24.64 | ||
| missing | 206 | 1.64 | 45 | 1.11 | ||
| Receive emotional support | no | 11,338 | 90.13 | 3574 | 87.79 | <0.001 † |
| any one | 611 | 4.86 | 325 | 7.98 | ||
| missing | 630 | 5.01 | 172 | 4.23 | ||
| Provide emotional support | no | 11,115 | 88.36 | 3503 | 86.05 | <0.001 † |
| any one | 781 | 6.21 | 365 | 8.97 | ||
| missing | 683 | 5.43 | 203 | 4.99 | ||
| Receive instrumental | no | 11,607 | 92.27 | 3633 | 89.24 | <0.001 † |
| support | any one | 415 | 3.3 | 289 | 7.1 | |
| missing | 557 | 4.43 | 149 | 3.66 | ||
| Locations with graffiti or garbage | present | 3349 | 26.62 | 1246 | 30.61 | <0.001 † |
| absent | 9009 | 71.62 | 2764 | 67.89 | ||
| missing | 221 | 1.76 | 61 | 1.5 | ||
| Parks/foot paths suitable for exercise/walking | present | 9009 | 71.62 | 2629 | 64.58 | <0.001 † |
| absent | 3419 | 27.18 | 1408 | 34.59 | ||
| missing | 151 | 1.2 | 34 | 0.84 | ||
| Locations difficult for walking (hills or steps) | present | 4939 | 39.26 | 1722 | 42.3 | 0.002 † |
| absent | 7523 | 59.81 | 2316 | 56.89 | ||
| missing | 117 | 0.93 | 33 | 0.81 | ||
| Roads/crossroads with risk of traffic accidents | present | 8152 | 64.81 | 2792 | 68.58 | <0.001 † |
| absent | 4291 | 34.11 | 1239 | 30.43 | ||
| missing | 136 | 1.08 | 40 | 0.98 | ||
| Fascinating views | present | 5088 | 40.45 | 1378 | 33.85 | <0.001 † |
| or buildings | absent | 7298 | 58.02 | 2636 | 64.75 | |
| missing | 193 | 1.53 | 57 | 1.4 | ||
| Shops or facilities selling | present | 9427 | 74.94 | 2816 | 69.17 | <0.001 † |
| fresh fruits & vegetables | absent | 3006 | 23.9 | 1229 | 30.19 | |
| missing | 146 | 1.16 | 26 | 0.64 | ||
| Dangerous places for | present | 7444 | 59.18 | 2552 | 62.69 | <0.001 † |
| walking alone at night | absent | 4973 | 39.53 | 1473 | 36.18 | |
| missing | 162 | 1.29 | 46 | 1.13 | ||
| Houses or facilities where you feel free to drop in | present | 5279 | 41.97 | 1337 | 32.84 | <0.001 † |
| absent | 7137 | 56.74 | 2682 | 65.88 | ||
| missing | 163 | 1.3 | 52 | 1.28 | ||
| GDS Score of <5 (n = 12,469) | GDS Score of ≥5 (n = 4181) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Good (n = 10,183) | Poor (n = 2286) | Good (n = 2396) | Poor (n = 1785) | ||||||||
| n | % | n | % | p * | n | % | n | % | p * | ||
| Sex | male | 5029 | 49.4 | 1011 | 44.2 | <0.001 | 1198 | 50.0 | 864 | 48.4 | 0.307 |
| female | 5154 | 50.6 | 1275 | 55.8 | 1198 | 50.0 | 921 | 51.6 | |||
| Age (years) | 65–69 | 3304 | 32.5 | 830 | 36.3 | <0.001 † | 644 | 26.9 | 526 | 29.5 | 0.008 |
| 70–74 | 3010 | 29.6 | 723 | 31.6 | 652 | 27.2 | 526 | 29.5 | |||
| 75–79 | 2135 | 21.0 | 421 | 18.4 | 528 | 22.0 | 386 | 21.6 | |||
| 80–84 | 1206 | 11.8 | 239 | 10.5 | 350 | 14.6 | 207 | 11.6 | |||
| ≥85 | 528 | 5.2 | 73 | 3.2 | 222 | 9.3 | 140 | 7.8 | |||
| Living alone | no | 9052 | 88.9 | 1996 | 87.3 | 0.030 † | 2037 | 85.0 | 1464 | 82.0 | 0.021 |
| yes | 1021 | 10.0 | 270 | 11.8 | 334 | 13.9 | 292 | 16.4 | |||
| missing | 110 | 1.1 | 20 | 0.9 | 25 | 1.0 | 29 | 1.6 | |||
| Self-rated health | fair | 9126 | 89.6 | 1812 | 79.3 | <0.001 † | 1603 | 66.9 | 920 | 51.5 | <0.001 † |
| poor | 920 | 9.0 | 443 | 19.4 | 748 | 31.2 | 833 | 46.7 | |||
| missing | 137 | 1.4 | 31 | 1.4 | 45 | 1.9 | 32 | 1.8 | |||
| Job | having | 2591 | 25.4 | 487 | 21.3 | <0.001 † | 405 | 16.9 | 270 | 15.1 | <0.001 |
| no | 6805 | 66.8 | 1631 | 71.4 | 1776 | 74.1 | 1338 | 75.0 | |||
| missing | 787 | 7.7 | 168 | 7.4 | 215 | 9.0 | 177 | 9.9 | |||
| Equivalent income (million yen) | <200 | 5170 | 50.8 | 1270 | 55.6 | <0.001 † | 1613 | 67.3 | 1255 | 70.3 | 0.087 |
| 200–400 | 3761 | 36.9 | 801 | 35.0 | 641 | 26.8 | 443 | 24.8 | |||
| ≥400 | 1252 | 12.3 | 215 | 9.4 | 142 | 5.9 | 87 | 4.9 | |||
| Education (year) | <6 | 162 | 1.6 | 43 | 1.9 | 0.476 | 85 | 3.6 | 62 | 3.5 | 0.420 |
| 6–9 | 4211 | 41.4 | 975 | 42.7 | 1164 | 48.6 | 893 | 50.0 | |||
| 10–12 | 3737 | 36.7 | 834 | 36.5 | 780 | 32.6 | 543 | 30.4 | |||
| ≥13 | 84 | 0.8 | 17 | 0.7 | 41 | 1.7 | 31 | 1.7 | |||
| other | 1944 | 19.1 | 404 | 17.7 | 312 | 13.0 | 237 | 13.3 | |||
| missing | 45 | 0.4 | 13 | 0.6 | 14 | 0.6 | 19 | 1.1 | |||
| Walking time (min) | <60 | 6104 | 59.9 | 1466 | 64.1 | <0.001 † | 1676 | 70.0 | 1312 | 73.5 | 0.042 |
| ≥60 | 3585 | 35.2 | 703 | 30.8 | 577 | 24.1 | 379 | 21.2 | |||
| missing | 494 | 4.9 | 117 | 5.1 | 143 | 6.0 | 94 | 5.3 | |||
| Treatment | yes | 6655 | 65.4 | 1582 | 69.2 | <0.001 † | 1723 | 71.9 | 1335 | 74.8 | 0.065 |
| no | 2835 | 27.8 | 535 | 23.4 | 481 | 20.1 | 308 | 17.3 | |||
| missing | 693 | 6.8 | 169 | 7.4 | 192 | 8.0 | 142 | 8.0 | |||
| Volunteer group | ≥1/month | 7083 | 69.6 | 1592 | 69.6 | 0.692 | 1735 | 72.4 | 1339 | 75.0 | 0.161 |
| <1/month | 1077 | 10.6 | 253 | 11.1 | 121 | 5.1 | 85 | 4.8 | |||
| missing | 2023 | 19.9 | 441 | 19.3 | 540 | 22.5 | 361 | 20.2 | |||
| Sports group | ≥1/month | 6254 | 61.4 | 1427 | 62.4 | 0.572 | 1676 | 70.0 | 1293 | 72.4 | 0.147 |
| <1/month | 2269 | 22.3 | 487 | 21.3 | 271 | 11.3 | 173 | 9.7 | |||
| missing | 1660 | 16.3 | 372 | 16.3 | 449 | 18.7 | 319 | 17.9 | |||
| Hobby activity | ≥1/month | 5157 | 50.6 | 1139 | 49.8 | 0.439 | 1518 | 63.4 | 1166 | 65.3 | 0.423 |
| <1/month | 3602 | 35.4 | 840 | 36.8 | 472 | 19.7 | 333 | 18.7 | |||
| missing | 1424 | 14.0 | 307 | 13.4 | 406 | 16.9 | 286 | 16.0 | |||
| Community trust | very | 7704 | 75.7 | 1598 | 69.9 | <0.001 † | 1432 | 59.8 | 930 | 52.1 | <0.001 † |
| slightly | 2079 | 20.4 | 613 | 26.8 | 852 | 35.6 | 787 | 44.1 | |||
| missing | 400 | 3.9 | 75 | 3.3 | 112 | 4.7 | 68 | 3.8 | |||
| Norms of reciprocity | very | 6302 | 61.9 | 1255 | 54.9 | <0.001 † | 1072 | 44.7 | 704 | 39.4 | <0.001 † |
| slightly | 3451 | 33.9 | 951 | 41.6 | 1201 | 50.1 | 1016 | 56.9 | |||
| missing | 430 | 4.2 | 80 | 3.5 | 123 | 5.1 | 65 | 3.6 | |||
| Community attachment | very | 8836 | 86.8 | 1884 | 82.4 | <0.001 † | 1754 | 73.2 | 1139 | 63.8 | <0.001 |
| slightly | 1174 | 11.5 | 382 | 16.7 | 609 | 25.4 | 621 | 34.8 | |||
| missing | 173 | 1.7 | 20 | 0.9 | 33 | 1.4 | 25 | 1.4 | |||
| Receive emotional support | no | 389 | 3.8 | 92 | 4 | 0.135 | 222 | 9.3 | 233 | 13.1 | <0.001 † |
| any one | 9285 | 91.2 | 2102 | 92 | 2053 | 85.7 | 1472 | 82.5 | |||
| missing | 509 | 5 | 92 | 4 | 121 | 5.1 | 80 | 4.5 | |||
| Provide emotional support | no | 467 | 4.6 | 112 | 4.9 | 0.288 | 314 | 13.1 | 253 | 14.2 | 0.541 |
| any one | 9176 | 90.1 | 2070 | 90.6 | 1939 | 80.9 | 1433 | 80.3 | |||
| missing | 540 | 5.3 | 104 | 4.6 | 143 | 6 | 99 | 5.6 | |||
| Receive instrumental support | no | 244 | 2.4 | 78 | 3.41 | 0.007 | 171 | 7.1 | 211 | 11.8 | <0.001 † |
| any one | 9500 | 93.29 | 2126 | 93 | 2107 | 87.9 | 1507 | 84.4 | |||
| missing | 439 | 4.3 | 82 | 3.6 | 118 | 4.9 | 67 | 3.8 | |||
| Locations with graffiti or garbage | present | 7844 | 77.0 | 1688 | 73.8 | 0.002 † | 1583 | 66.1 | 1128 | 63.2 | 0.429 |
| absent | 2221 | 21.8 | 583 | 25.5 | 785 | 32.8 | 646 | 36.2 | |||
| missing | 118 | 1.2 | 15 | 0.7 | 28 | 1.2 | 11 | 0.6 | |||
| Parks/foot paths suitable for exercise/walking | present | 7502 | 73.7 | 1589 | 69.5 | <0.001 † | 1507 | 62.9 | 1040 | 58.3 | 0.004 † |
| absent | 2564 | 25.2 | 683 | 29.9 | 855 | 35.7 | 725 | 40.6 | |||
| missing | 117 | 1.2 | 14 | 0.6 | 34 | 1.4 | 20 | 1.1 | |||
| Locations difficult for walking (hills or steps) | present | 3859 | 37.9 | 924 | 40.4 | 0.047 | 1080 | 45.1 | 798 | 44.7 | 0.972 |
| absent | 6231 | 61.2 | 1347 | 58.9 | 1292 | 53.9 | 969 | 54.3 | |||
| missing | 93 | 0.9 | 15 | 0.7 | 24 | 1.0 | 18 | 1.0 | |||
| Roads/crossroads with risk of traffic accidents | present | 6518 | 64.0 | 1545 | 67.6 | 0.004 † | 1634 | 68.2 | 1247 | 69.9 | 0.454 |
| absent | 3556 | 34.9 | 723 | 31.6 | 735 | 30.7 | 516 | 28.9 | |||
| missing | 109 | 1.1 | 18 | 0.8 | 27 | 1.1 | 22 | 1.2 | |||
| Fascinating views or buildings | present | 4329 | 42.5 | 874 | 38.2 | <0.001 † | 1583 | 66.1 | 1128 | 63.2 | 0.051 |
| absent | 5701 | 56.0 | 1383 | 60.5 | 785 | 32.8 | 646 | 36.2 | |||
| missing | 153 | 1.5 | 29 | 1.3 | 28 | 1.2 | 11 | 0.6 | |||
| Shops or facilities selling fresh fruits & vegetables | present | 7844 | 77.0 | 1688 | 73.8 | <0.001 † | 704 | 29.4 | 460 | 25.8 | 0.017 |
| absent | 2221 | 21.8 | 583 | 25.5 | 1658 | 69.2 | 1303 | 73.0 | |||
| missing | 118 | 1.2 | 15 | 0.7 | 34 | 1.4 | 22 | 1.2 | |||
| Dangerous places for walking alone at night | present | 7844 | 77.0 | 1688 | 73.8 | 0.017 † | 1583 | 66.1 | 1128 | 63.2 | 0.643 |
| absent | 2221 | 21.8 | 583 | 25.5 | 785 | 32.8 | 646 | 36.2 | |||
| missing | 118 | 1.2 | 15 | 0.7 | 28 | 1.2 | 11 | 0.6 | |||
| Houses or facilities where you feel free to drop in | present | 4575 | 44.9 | 877 | 38.4 | <0.001 † | 704 | 29.4 | 460 | 25.8 | 0.028 † |
| absent | 5479 | 53.8 | 1379 | 60.3 | 1658 | 69.2 | 1303 | 73.0 | |||
| missing | 129 | 1.3 | 30 | 1.3 | 34 | 1.4 | 22 | 1.2 | |||
| Model 1 | Model 2 | Model 3 | Model 4 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PR | 95% CI | PR | 95% CI | PR | 95% CI | ||||||||
| Individual factors | |||||||||||||
| Depressive status | GDS score of <5 | ref | |||||||||||
| GDS score of ≥5 | 1.93 | 1.80 | 2.07 | 1.93 | 1.80 | 2.07 | 1.92 | 1.79 | 2.06 | ||||
| Age (years) | 65–69 | ref | |||||||||||
| 70–74 | 0.96 | 0.89 | 1.04 | 0.96 | 0.89 | 1.04 | 0.96 | 0.89 | 1.04 | ||||
| 75–79 | 0.82 | 0.75 | 0.90 | 0.82 | 0.75 | 0.90 | 0.82 | 0.75 | 0.90 | ||||
| 80–84 | 0.74 | 0.66 | 0.83 | 0.74 | 0.66 | 0.84 | 0.75 | 0.66 | 0.84 | ||||
| ≥85 | 0.68 | 0.58 | 0.80 | 0.68 | 0.58 | 0.80 | 0.69 | 0.59 | 0.80 | ||||
| Sex | male | ref | |||||||||||
| female | 1.12 | 1.05 | 1.19 | 1.12 | 1.05 | 1.19 | 1.12 | 1.05 | 1.19 | ||||
| Living alone | no | ref | |||||||||||
| yes | 1.15 | 1.05 | 1.26 | 1.15 | 1.04 | 1.26 | 1.14 | 1.04 | 1.26 | ||||
| Self-rated health | fair | ref | |||||||||||
| poor | 1.67 | 1.55 | 1.80 | 1.67 | 1.55 | 1.81 | 1.67 | 1.55 | 1.81 | ||||
| Equivalent income (million yen) | <200 | ref | |||||||||||
| 200–400 | 0.95 | 0.88 | 1.02 | 0.94 | 0.88 | 1.01 | 0.94 | 0.88 | 1.01 | ||||
| ≥400 | 0.83 | 0.74 | 0.94 | 0.83 | 0.73 | 0.94 | 0.83 | 0.73 | 0.94 | ||||
| Job | yes | ref | |||||||||||
| no | 1.11 | 1.02 | 1.21 | 1.11 | 1.02 | 1.21 | 1.11 | 1.02 | 1.20 | ||||
| Education (years) | <6 | ref | |||||||||||
| 6–9 | 0.94 | 0.76 | 1.18 | 0.94 | 0.75 | 1.17 | 0.94 | 0.75 | 1.17 | ||||
| 10–12 | 0.94 | 0.75 | 1.17 | 0.93 | 0.74 | 1.16 | 0.93 | 0.74 | 1.16 | ||||
| ≥13 | 0.94 | 0.75 | 1.19 | 0.93 | 0.74 | 1.18 | 0.93 | 0.74 | 1.18 | ||||
| other | 1.25 | 0.81 | 1.92 | 1.24 | 0.81 | 1.90 | 1.24 | 0.81 | 1.90 | ||||
| Walking time (min) | <60 | ref | |||||||||||
| ≥60 | 0.91 | 0.85 | 0.98 | 0.91 | 0.85 | 0.98 | 0.91 | 0.85 | 0.98 | ||||
| Treatment | yes | ref | |||||||||||
| no | 0.87 | 0.80 | 0.94 | 0.87 | 0.80 | 0.94 | 0.87 | 0.80 | 0.94 | ||||
| Social environment | |||||||||||||
| (Social Capital) | |||||||||||||
| Civic participant | every 10% increase | 1.14 | 0.91 | 1.44 | |||||||||
| Social cohesion | every 10% increase | 1.00 | 0.80 | 1.25 | |||||||||
| Reciprocity | every 10% increase | 0.83 | 0.48 | 1.43 | |||||||||
| Physical environment | |||||||||||||
| No location with graffiti or garbage | every 10% increase | 0.83 | 0.51 | 1.33 | |||||||||
| Parks or foot paths suitable for exercise or walking | every 10% increase | 1.00 | 0.72 | 1.37 | |||||||||
| No difficult locations for walking such as hills or steps | every 10% increase | 0.84 | 0.68 | 1.04 | |||||||||
| No risky roads or crossroads with risk of traffic accidents | every 10% increase | 0.83 | 0.51 | 1.35 | |||||||||
| Fascinating views or buildings | every 10% increase | 0.99 | 0.73 | 1.33 | |||||||||
| Shops or facilities selling fresh fruits and vegetables | every 10% increase | 1.09 | 0.82 | 1.45 | |||||||||
| No dangerous places for walking alone at night | every 10% increase | 1.33 | 0.79 | 2.23 | |||||||||
| Houses or facilities where you feel free to drop in | every 10% increase | 0.59 | 0.36 | 0.95 | |||||||||
| Intercept | 0.27 | 0.27 | 0.28 | 0.03 | -0.49 | 0.11 | 0.25 | -0.09 | 0.60 | 0.14 | 0.02 | 0.26 | |
| Random effects | |||||||||||||
| Community-level variance (SE) | 0.0004 | (−0.0003) | 0.0002 | (−0.0003) | 0.0001 | (−0.0003) | 2.97 × 10−11 | (5.5 × 10−11) | |||||
| PCV | 0.50 | 0.75 | 0.99 | ||||||||||
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PR | 95% CI | PR | 95% CI | PR | 95% CI | |||||||
| Individual factors | ||||||||||||
| Age (years) | 65–69 | ref | ||||||||||
| 70–74 | 0.94 | 0.85 | 1.04 | 0.96 | 0.87 | 1.07 | 0.94 | 0.85 | 1.05 | |||
| 75–79 | 0.75 | 0.66 | 0.85 | 0.77 | 0.68 | 0.87 | 0.75 | 0.66 | 0.85 | |||
| 80–84 | 0.71 | 0.6 | 0.83 | 0.74 | 0.63 | 0.87 | 0.71 | 0.6 | 0.84 | |||
| ≥85 | 0.52 | 0.4 | 0.68 | 0.55 | 0.42 | 0.72 | 0.52 | 0.4 | 0.69 | |||
| Sex | male | ref | ||||||||||
| female | 1.16 | 1.06 | 1.27 | 1.15 | 1.05 | 1.26 | 1.17 | 1.07 | 1.28 | |||
| Living alone | no | ref | ||||||||||
| yes | 1.16 | 1.01 | 1.33 | 1.14 | 0.99 | 1.31 | 1.15 | 1 | 1.32 | |||
| Self-rated health | fair | ref | ||||||||||
| poor | 1.97 | 1.76 | 2.2 | 1.93 | 1.73 | 2.16 | 1.97 | 1.76 | 2.2 | |||
| Equivalent income (million yen) | <200 | ref | ||||||||||
| 200–400 | 0.92 | 0.84 | 1.01 | 0.92 | 0.83 | 1.01 | 0.92 | 0.83 | 1.01 | |||
| ≥400 | 0.82 | 0.71 | 0.95 | 0.82 | 0.71 | 0.96 | 0.82 | 0.7 | 0.95 | |||
| Job | yes | ref | ||||||||||
| no | 1.16 | 1.04 | 1.29 | 1.13 | 1.02 | 1.27 | 1.15 | 1.03 | 1.28 | |||
| Education (years) | <6 | ref | ||||||||||
| 6–9 | 0.84 | 0.6 | 1.16 | 1 | 0.91 | 1.09 | 0.82 | 0.59 | 1.14 | |||
| 10–12 | 0.84 | 0.6 | 1.17 | 1.06 | 0.57 | 1.97 | 0.82 | 0.59 | 1.14 | |||
| ≥13 | 0.81 | 0.58 | 1.14 | 0.88 | 0.8 | 0.97 | 0.79 | 0.56 | 1.11 | |||
| other | 0.96 | 0.49 | 1.87 | 0.83 | 0.75 | 0.93 | 0.96 | 0.49 | 1.88 | |||
| Walking time (min) | <60 | ref | ||||||||||
| ≥60 | 0.88 | 0.8 | 0.96 | 0.88 | 0.8 | 0.97 | 0.88 | 0.8 | 0.96 | |||
| Treatment | yes | ref | ||||||||||
| no | 0.84 | 0.76 | 0.94 | 0.83 | 0.75 | 0.93 | 0.84 | 0.76 | 0.94 | |||
| Social environment | ||||||||||||
| (Social Capital) | ||||||||||||
| Civic participant | every 10% increase | 1.21 | 0.88 | 1.67 | ||||||||
| Social cohesion | every 10% increase | 1.04 | 0.77 | 1.4 | ||||||||
| Reciprocity | every 10% increase | 0.96 | 0.44 | 2.1 | ||||||||
| Physical environment | ||||||||||||
| No location with graffiti or garbage | every 10% increase | 0.68 | 0.36 | 1.29 | ||||||||
| Parks or foot paths suitable for exercise or walking | every 10% increase | 0.99 | 0.64 | 1.54 | ||||||||
| No difficult locations for walking such as hills or steps | every 10% increase | 0.75 | 0.56 | 0.99 | ||||||||
| No risky roads or crossroads with risk of traffic accidents | every 10% increase | 0.92 | 0.47 | 1.79 | ||||||||
| Fascinating views or buildings | every 10% increase | 0.98 | 0.66 | 1.47 | ||||||||
| Shops or facilities selling fresh fruits and vegetables | every 10% increase | 1.21 | 0.82 | 1.78 | ||||||||
| No dangerous places for walking alone at night | every 10% increase | 1.41 | 0.7 | 2.86 | ||||||||
| Houses or facilities where you feel free to drop in | every 10% increase | 0.51 | 0.26 | 0.98 | ||||||||
| Intercept | 0.2 | 0.19 | 0.21 | 0.12 | 0.07 | 0.19 | 0.08 | 0.01 | 0.66 | 0.14 | 0.66 | 0.34 |
| Random effects | ||||||||||||
| Community-level variance (SE) | 0.00074 | (0.00038) | 0.06 | (0.00061) | 0.00045 | 0.00055 | (0.00044) | 0.00025 | (0.00041) | |||
| PCV | 0.176 | 0.257 | 0.662 | |||||||||
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PR | 95% CI | PR | 95% CI | PR | 95% CI | |||||||
| Individual-level | ||||||||||||
| Age (years) | 65–69 | ref | ||||||||||
| 70–74 | 0.99 | 0.87 | 1.12 | 1 | 0.88 | 1.13 | 0.99 | 0.87 | 1.12 | |||
| 75–79 | 0.92 | 0.8 | 1.05 | 0.94 | 0.82 | 1.09 | 0.92 | 0.8 | 1.06 | |||
| 80–84 | 0.79 | 0.67 | 0.94 | 0.83 | 0.7 | 0.99 | 0.8 | 0.67 | 0.95 | |||
| ≥85 | 0.83 | 0.68 | 1.01 | 0.86 | 0.7 | 1.06 | 0.84 | 0.68 | 1.02 | |||
| Sex | male | ref | ||||||||||
| female | 1.06 | 0.96 | 1.17 | 1.06 | 0.96 | 1.16 | 1.06 | 0.96 | 1.17 | |||
| Living alone | no | ref | ||||||||||
| yes | 1.14 | 1 | 1.29 | 1.11 | 0.97 | 1.26 | 1.14 | 1 | 1.29 | |||
| Self-rated health | fair | ref | ||||||||||
| poor | 1.49 | 1.35 | 1.65 | 1.46 | 1.32 | 1.62 | 1.49 | 1.35 | 1.65 | |||
| Equivalent income | <200 | ref | ||||||||||
| (million yen) | 200–400 | 0.97 | 0.87 | 1.09 | 0.99 | 0.88 | 1.11 | 0.97 | 0.87 | 1.08 | ||
| ≥400 | 0.86 | 0.69 | 1.08 | 0.89 | 0.71 | 1.11 | 0.86 | 0.69 | 1.07 | |||
| Job | have | ref | ||||||||||
| no | 1.04 | 0.91 | 1.19 | 1.04 | 0.91 | 1.19 | 1.04 | 0.91 | 1.19 | |||
| Education (years) | <6 | ref | ||||||||||
| 6–9 | 1.07 | 0.79 | 1.44 | 1.11 | 0.82 | 1.5 | 1.07 | 0.79 | 1.44 | |||
| 10–12 | 1.05 | 0.77 | 1.42 | 1.09 | 0.8 | 1.49 | 1.05 | 0.77 | 1.42 | |||
| ≥13 | 1.12 | 0.82 | 1.54 | 1.15 | 0.84 | 1.6 | 1.12 | 0.82 | 1.55 | |||
| other | 1.54 | 0.88 | 2.69 | 1.63 | 0.92 | 2.89 | 1.53 | 0.88 | 2.67 | |||
| Walking time (min) | <60 | ref | ||||||||||
| ≥60 | 0.97 | 0.86 | 1.08 | 0.96 | 0.86 | 1.08 | 0.97 | 0.86 | 1.09 | |||
| Treatment | yes | ref | ||||||||||
| no | 0.92 | 0.81 | 1.06 | 0.92 | 0.8 | 1.05 | 0.92 | 0.81 | 1.06 | |||
| Social environment | ||||||||||||
| (Social Capital) | ||||||||||||
| Civic participation | every 10% increase | 0.98 | 0.7 | 1.38 | ||||||||
| Social cohesion | every 10% increase | 1.05 | 0.76 | 1.47 | ||||||||
| Reciprocity | every 10% increase | 0.83 | 0.38 | 1.83 | ||||||||
| Physical environment | ||||||||||||
| No location with graffiti or garbage | every 10% increase | 1 | 0.49 | 2.04 | ||||||||
| Parks or foot paths suitable | every 10% increase | 1 | 0.62 | 1.61 | ||||||||
| for exercise or walking | ||||||||||||
| No difficult locations for | every 10% increase | 0.99 | 0.73 | 1.35 | ||||||||
| walking such as hills or steps | ||||||||||||
| No risky roads or crossroads | every 10% increase | 0.75 | 0.36 | 1.55 | ||||||||
| with risk of traffic accidents | ||||||||||||
| Fascinating views or buildings | every 10% increase | 1.01 | 0.64 | 1.57 | ||||||||
| Shops or facilities selling | every 10% increase | 0.96 | 0.63 | 1.45 | ||||||||
| fresh fruits and vegetables | ||||||||||||
| No dangerous places for | every 10% increase | 1.17 | 0.54 | 2.53 | ||||||||
| walking alone at night | ||||||||||||
| Houses or facilities where | every 10% increase | 0.72 | 0.35 | 1.47 | ||||||||
| you feel free to drop in | ||||||||||||
| Intercept | 0.47 | 0.45 | 0.25 | 0.15 | 0.43 | 0.28 | 0.03 | 2.41 | 0.31 | 0.14 | 0.67 | |
| Random effects | ||||||||||||
| Community-level variance (SE) | 4.6 × 10−21 | (1.09 × 10−20) | 9.22 × 10−18 | (1.79 × 10−17) | 2.04 × 10−19 | (4.87 × 10−19) | (1.6 × 10−11) | (3.9 × 10−19) | ||||
| PCV | - | - | - | |||||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watanabe, M.; Shobugawa, Y.; Tashiro, A.; Ota, A.; Suzuki, T.; Tsubokawa, T.; Kondo, K.; Saito, R. Association between Neighborhood Environment and Quality of Sleep in Older Adult Residents Living in Japan: The JAGES 2010 Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 1398. https://doi.org/10.3390/ijerph17041398
Watanabe M, Shobugawa Y, Tashiro A, Ota A, Suzuki T, Tsubokawa T, Kondo K, Saito R. Association between Neighborhood Environment and Quality of Sleep in Older Adult Residents Living in Japan: The JAGES 2010 Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2020; 17(4):1398. https://doi.org/10.3390/ijerph17041398
Chicago/Turabian StyleWatanabe, Michiko, Yugo Shobugawa, Atsushi Tashiro, Asami Ota, Tsubasa Suzuki, Tomoko Tsubokawa, Katsunori Kondo, and Reiko Saito. 2020. "Association between Neighborhood Environment and Quality of Sleep in Older Adult Residents Living in Japan: The JAGES 2010 Cross-Sectional Study" International Journal of Environmental Research and Public Health 17, no. 4: 1398. https://doi.org/10.3390/ijerph17041398
APA StyleWatanabe, M., Shobugawa, Y., Tashiro, A., Ota, A., Suzuki, T., Tsubokawa, T., Kondo, K., & Saito, R. (2020). Association between Neighborhood Environment and Quality of Sleep in Older Adult Residents Living in Japan: The JAGES 2010 Cross-Sectional Study. International Journal of Environmental Research and Public Health, 17(4), 1398. https://doi.org/10.3390/ijerph17041398








