Parental Perception of Changes in Basic Life Needs of Children with Disabilities after Six Months of Therapeutic Horseback Riding: A Qualitative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Theoretical Framework
2.2. Study Design
2.2.1. Preparatory Phase of THR Lessons
2.2.2. Implementation Phase of THR Lessons
2.3. Participants
2.4. Data Collection
2.5. Data Analysis
2.6. Ethical Considerations
3. Results
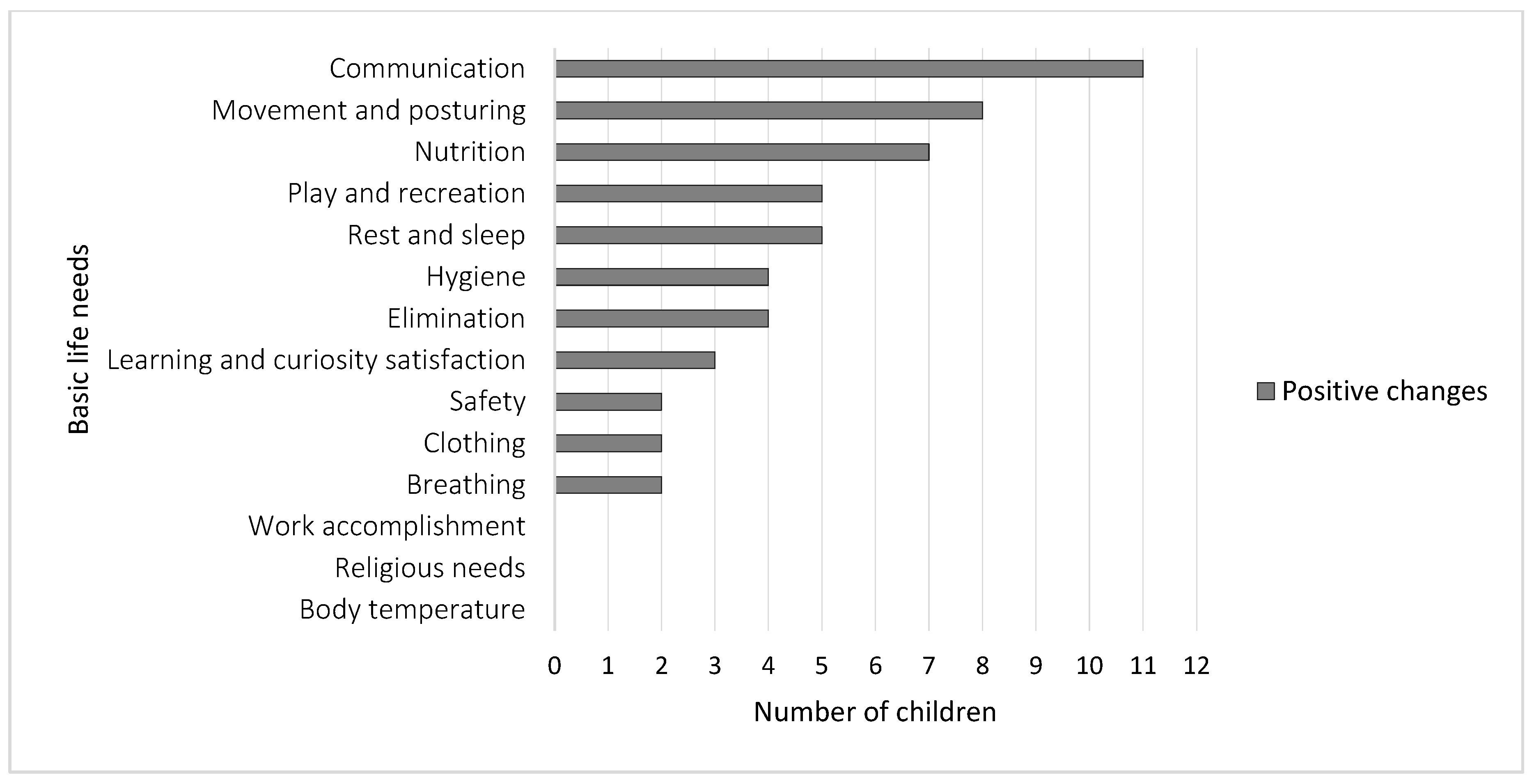
3.1. Parental Perception of Changes in Their Child’s Basic Life Needs
“Our child is content, happier, and laughs more. On every occasion, he is very pleased to meet the horse and THR instructors” (P9) and “Meeting new people is no longer a problem for our child. The child communicates with other people more often and with better quality. He used to say only 3 to 5 words, and now he pronounces up to 10 words in continuity” (P11).
“Our child has better movement control. He takes items more firmly and securely. For example, he no longer drops a pen or a glass so often” (P6).
“When we are walking, the child runs and jumps much more and gets less tired than before” (P4).
“My husband and I no longer have the usual long-lasting evening rituals of putting our child to sleep. Our child has a much peaceful sleep and does not wake up often during the night” (P3).
“For the past few years, our child has had constipation problems. She defecated every fourth to fifth day, with intense strain and frequent abdominal pain. The stool was often of very hard consistency. Now she defecates every other day, without accompanying pain” (P12);
“The irregular stool in our child now belongs to the past, although the child still uses medications that cause constipation as a side effect. This change in our child is precious” (P3); and “During the day, our child announces the urge to go to the toilet, so we use the usual absorbent products only during the night” (P6).
“Ever since our child has been included in THR activities, he has a much better appetite and drinks twice as much fluid than before” (P5) and “The child now consumes 3–4 meals a day. Previously, he rejected food and ate twice a day at most” (P1).
“At night, the child no longer suffers from episodes of rapid breathing and sleeps much calmer” (P2).
“Going out in nature and playing with friends became important to our child. Previously, he had separation anxieties and avoided the company of other kids” (P7).
“Finally! The child is separated from his cell-phone and goes to the park with his friends” (P5).
“Our child always had a problem with washing his hands, but now, without us reminding him, the child washes hands all on his own” (P9).
“Our child will have learning difficulties for their lifetime, but we recognized a greater desire for reading content about animals” (P2).
“It is amazing that the child now puts both socks on independently, which was very problematic earlier” (P6);
“The child always asks for protective equipment before horseback riding. Sometimes she asks for a headgear already in the car, on the way to the Equestrian Club” (P8).
3.2. Parental Perception of Factors that Caused Changes in Their Child’s Basic Life Needs
“There are obvious positive changes, but I think they are a result of several influencing factors, not just THR, for example, the impact of child’s development and the medication he uses daily” (P1);
“Simultaneously, our child attends neurofeedback and other forms of therapy, and we also work with the child every day. I do not believe that THR was crucial, but the improvements are a fact” (P4).
“I think my child’s contact with the horse is a key factor in all the improvements. This is indisputable. We had previously and unsuccessfully tried with various other therapies and failed. THR has improved our child’s quality of life” (P3).
4. Discussion
4.1. Parental Perception of Changes in Their Child’s Basic Life Needs
4.2. Parental Perception of Factors that Caused Changes in Their Child’s Basic Life Needs
4.3. Limitations and Recommendations for Future Research
4.4. Usefulness and Applicability of Study Results
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Stickney, M.A. A Qualitative Study of the Perceived Health Benefits of a Therapeutic Riding Program for Children with Autism Spectrum Disorders. Ph.D. Thesis, University of Kentucky, Lexington, KY, USA, 2010. Available online: http://uknowledge.uky.edu/gradschool_diss/40 (accessed on 15 October 2019).
- Kwon, S.; Sung, I.Y.; Ko, E.J.; Kim, H.S. Effects of therapeutic horseback riding on cognition and language in children with autism spectrum disorder or intellectual disability: A preliminary study. Ann. Rehabil. Med. 2019, 43, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Silkwood-Sherer, D.J.; Killian, C.B.; Long, T.M.; Martin, K.S. Hippotherapy—An intervention to habilitate balance deficits in children with movement disorders: A clinical trial. Phys. Ther. 2012, 92, 707–717. [Google Scholar] [CrossRef] [PubMed]
- Boyd, L.; le Roux, M. “When he’s up there he’s just happy and content”: Parents’ perceptions of therapeutic horseback riding. Afr. J. Disabil. 2017, 26, 307. [Google Scholar] [CrossRef] [PubMed]
- Sterba, J.A.; Rogers, B.T.; France, A.P.; Vokes, D.A. Horseback riding in children with cerebral palsy: Effect on gross motor function. Dev. Med. Child Neurol. 2002, 44, 301–308. [Google Scholar] [CrossRef] [PubMed]
- De Milander, M.; Bradley, S.; Fourie, R. Equine-assisted therapy as an intervention for motor proficiency in children with autism spectrum disorder: Case studies. SAJR SPER 2016, 38, 37–49. Available online: https://www.researchgate.net/publication/312628859 (accessed on 15 October 2019).
- Bass, M.M.; Duchowny, C.A.; Llabre, M.M. The effect of therapeutic horseback riding on social functioning in children with autism. J. Autism Dev. Disord. 2009, 39, 1261–1267. [Google Scholar] [CrossRef]
- Gabriels, R.L.; Pan, Z.; Dechant, B.; Agnew, J.A.; Brim, N.; Mesibov, G. Randomized controlled trial of therapeutic horseback riding in children and adolescents with autism spectrum disorder. J. Am. Acad. Child Adolesc. Psychiatry 2015, 54, 541–549. [Google Scholar] [CrossRef]
- Butt, M. Parents’ and Facilitators’ Perceptions of Children with Autism Spectrum Disorder in an Equine-Assisted Learning Programme. Master’s Thesis, Stellenbosch University, Stellenbosch, South Africa, 2017. Available online: https://pdfs.semanticscholar.org/845b/56f418218213167050dc046ed126fdf7dcd9.pdf (accessed on 15 October 2019).
- Scialli, A.L. Parent Perceptions of the Effectiveness of Therapeutic Horseback Riding for Children with Varying Disabilities. Ph.D. Thesis, Lynn University, Boca Raton, FL, USA, 2002. Available online: https://spiral.lynn.edu/etds/204 (accessed on 15 October 2019).
- Erdman, P.; Miller, D.; Jacobson, S. The impact of an equine facilitated learning program on youth with autism spectrum disorder. Hum. Anim. Interact. Bull. 2015, 3, 21–36. Available online: https://habricentral.org/resources/53358 (accessed on 15 October 2019).
- Ward, S.C.; Whalon, K.; Rusnak, K.; Wendell, K.; Paschall, N. The association between therapeutic horseback riding and the social communication and sensory reactions of children with autism. J. Autism Dev. Disord. 2013, 43, 2190–2198. [Google Scholar] [CrossRef]
- Cuypers, K.; De Ridder, K.; Strandheim, A. The effect of therapeutic horseback riding on 5 children with attention deficit hyperactivity disorder: A pilot study. J. Altern. Complement. Med. 2011, 17, 901–908. [Google Scholar] [CrossRef]
- Achenbach, T.M.; Ruffle, T.M. The child behaviour checklist and related forms for assessing behavioural/emotional problems and competencies. Pediatr. Rev. 2000, 21, 265–271. [Google Scholar] [CrossRef] [PubMed]
- Lanning, B.A.; Matyastik Baier, M.E.; Ivey-Hatz, J.; Krenek, N.; Tubbs, J.D. Effects of equine assisted activities on autism spectrum disorder. J. Autism Dev. Disord. 2014, 44, 1897–1907. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.H.; Alston, A.J. Therapeutic riding: An educational tool for children with disabilities as viewed by parents. J. South. Agric. Educ. Res. 2004, 54, 113–123. Available online: http://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.579.2920&rep=rep1&type=pdf (accessed on 15 October 2019).
- Elliott, S.; Funderburk, J.A.; Holland, J.M. The impact of the ‘Stirrup Some Fun’ therapeutic horseback riding program: A qualitative investigation. Am. J. Recreat. Ther. 2008, 7, 19–28. [Google Scholar] [CrossRef]
- Davis, E.; Davies, B.; Wolfe, R.; Raadsveld, R.; Heine, B.; Thomas, P.; Graham, H.K. A randomized controlled trial of the impact of therapeutic horse riding on the quality of life, health and function of children with cerebral palsy. Dev. Med. Child Neurol. 2009, 51, 111–119. [Google Scholar] [CrossRef] [PubMed]
- Alligood, M.R. Nursing Theorists and Their Work, 9th ed.; Mosby Elsevier: Maryland Heights, MO, USA, 2017. [Google Scholar]
- Henderson, V. ICN Basic Principles of Nursing Care; International Council of Nurses: Geneva, Switzerland, 2004. [Google Scholar]
- Younas, A.; Sommer, J. Integrating nursing theory and process into practice: Virginia Henderson’s need theory. Int. J. Caring Sci. 2015, 8, 443–450. Available online: http://www.internationaljournalofcaringsciences.org/docs/23_ahtisham.pdf (accessed on 15 October 2019).
- Bongers, B.C.; Takken, T. Physiological demands of therapeutic horseback riding in children with moderate to severe motor impairments: An exploratory study. Pediatr. Phys. Ther. 2012, 24, 252–257. [Google Scholar] [CrossRef]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm. Policy Ment. Health 2015, 42, 533–544. [Google Scholar] [CrossRef]
- Bengtsson, M. How to plan and perform a qualitative study using content analysis. Nurs. Open 2016, 2, 8–14. [Google Scholar] [CrossRef]
- Balcetis, E. Approach and avoidance as organizing structures for motivated distance perception. Emot. Rev. 2016, 8, 115–128. [Google Scholar] [CrossRef]
- Vetter, P.; Newen, A. Varieties of cognitive penetration in visual perception. Conscious. Cogn. 2014, 27, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef] [PubMed]
- Ghorban, H.; Sedigheh, R.D.; Marzieh, G.; Yaghoob, G. Effectiveness of therapeutic horseback riding on social skills of children with autism spectrum disorder in Shiraz, Iran. J. Educ. Learn. 2013, 2, 79–84. [Google Scholar] [CrossRef]
- Lovrić, R.; Prlić, N.; Milutinović, D.; Marjanac, I.; Žvanut, B. Changes in nursing students’ expectations of nursing clinical faculties’ competences: A longitudinal, mixed-methods study. Nurse Educ. Today 2017, 59, 38–44. [Google Scholar] [CrossRef]
- Nelson, K.; Axtell, J.; Derby, M.; Moug, R.; Berrera, S.; McLaughlin, T.F. A preliminary analysis of therapeutic horseback riding. Int. J. Soc. Sci. Educ. 2011, 1, 644–656. Available online: http://www.ijsse.com/ sites/default/files/issues/2011/v1i4/paper%2027/paper%2027.pdf (accessed on 15 October 2019).
- Surujlal, J.; Rufus, S. Perceptions of parents about equine therapy for children with intellectual disabilities. Afr. J. Phys. Health Educ. Recreat. Dance 2011, 1, 372–385. Available online: https://journals.co.za/content/ajpherd/17/sup-2/EJC121719 (accessed on 15 October 2019).
- Hauge, H.; Kvalem, I.L.; Berget, B.; Enders-Slegers, M.J.; Braastad, B.O. Equine-assisted activities and the impact on perceived social support, self-esteem and self-efficacy among adolescents–An intervention study. Int. J. Adolesc. Youth 2014, 19, 1–21. [Google Scholar] [CrossRef]
- Nqwena, Z.; Naidoo, R. The effect of therapeutic horseback riding on heart rate variability of children with disabilities. Afr. J. Disabil. 2016, 5, 248. [Google Scholar] [CrossRef]
- Land, G.; Errington Povalac, E.; Paul, S. The effects of therapeutic riding on sitting posture in individuals with disabilities. Occup. Ther. Health Care 2002, 14, 1–12. [Google Scholar] [CrossRef]
- Cherng, R.J.; Liao, H.F.; Leung, H.W.C.; Hwang, A.W. The effectiveness of therapeutic horseback riding in children with spastic cerebral palsy. Adapt. Phys. Act. Q. 2009, 21, 103–121. [Google Scholar] [CrossRef]
- Low, S.; Collins, G.; Dhagat, C.; Hanes, P.; Adams, J.; Fischbach, R. Therapeutic horseback riding: Its effects on gait and gross motor function in children with cerebral palsy. Sci. Educ. J. Ther. Rid. 2005, 11, 12–24. Available online: http://www.frdi.net/journal_abstracts.html#2005 (accessed on 15 October 2019).
- Wright, M.; Tancredi, A.; Yundt, B.; Larin, H.M. Sleep issues in children with physical disabilities and their families. Phys. Occup. Ther. Pediatr. 2006, 26, 55–72. [Google Scholar] [CrossRef] [PubMed]
- Tolaymat, A.; Liu, Z. Sleep disorders in childhood neurological diseases. Children 2017, 4, 84. [Google Scholar] [CrossRef] [PubMed]
- Levy, S.E.; Mandell, D.S.; Schultz, R.T. Autism. Lancet 2009, 374, 1627–1638. [Google Scholar] [CrossRef]
- Beaudry-Bellefeuille, I.; Booth, D.; Lane, S.J. Defecation-specific behaviour in children with functional defecation issues: A systematic review. Perm. J. 2017, 21, 17–47. [Google Scholar] [CrossRef]
- von Gontard, A. Urinary incontinence in children with special needs. Nat. Rev. Urol. 2013, 10, 667–674. [Google Scholar] [CrossRef]
- Al-Shirawi, M.E.; Al-zayer, R.H. The effect of therapeutic horseback riding on sensory processing of children with autism. Eur. Sci. J. 2018, 14, 1857–1881. [Google Scholar] [CrossRef][Green Version]
- Tseng, S.H.; Chen, H.C.; Tam, K.W. Systematic review and meta-analysis of the effect of equine assisted activities and therapies on gross motor outcome in children with cerebral palsy. Disabil. Rehabil. 2013, 35, 89–99. [Google Scholar] [CrossRef]
- Hasan, S.I. Links between Physical and Mental Health: Assessment of Therapeutic Riding’s Effect on Children with Special Needs. Bachelor’s Thesis, Brescia University College, London, UK, 2017. Available online: https://ir.lib.uwo.ca/brescia_psych uht/2 (accessed on 30 January 2020).
- Jenkins, S.R.; Reed, F.D.D. An experimental analysis of the effects of therapeutic horseback riding on the behavior of children with autism. Res. Autism Spectr. Disord. 2013, 7, 721–740. [Google Scholar] [CrossRef]
- Shefer, T. Adolescence. In Psychology: An Introduction; Swart, L., de la Ray, C., Duncan, N., Townsend, L., Eds.; Oxford University Press: Cape Town, South Africa, 2008; pp. 74–84. [Google Scholar]
- Bertoti, D.B. Effect of therapeutic horseback riding on posture in children with cerebral palsy. Phys. Ther. 1988, 68, 1505–1512. [Google Scholar]
| Component | Aspect of Component | Description |
|---|---|---|
| 1. Breathing | Physiological | Breathe normally |
| 2. Nutrition | Physiological | Eat and drink adequately |
| 3. Elimination | Physiological | Eliminate body wastes |
| 4. Movement and posturing | Physiological | Move and maintain desirable postures |
| 5. Rest and sleep | Physiological | Rest and sleep |
| 6. Select suitable clothes | Physiological | Select suitable clothes |
| 7. Body temperature | Physiological | Maintain normal body temperature |
| 8. Hygiene | Physiological | Keep the body clean and well-groomed |
| 9. Safety | Physiological | Avoid dangers in the environment and avoid injuring others |
| 10. Communication | Psychological | Communicate with others in expressing emotions, moods, opinions |
| 11. Religious needs | Spiritual and moral | Worship according to one’s faith |
| 12. Work accomplishment | Sociological | Work in such a way that there is a sense of accomplishment |
| 13 Play and recreation | Sociological | Play or participate in various forms of recreation |
| 14. Learning and curiosity satisfaction | Psychological | Learn, discover, or satisfy the curiosity |
| Parents | Child | Child’s Disabilities |
|---|---|---|
| P1 | C1 | Intellectual disabilities Speech and language impairment in voice communication, and learning disabilities |
| P2 | C2 | Physical activity and attention disorders Speech and language impairment in voice communication, and learning disabilities Intellectual disabilities |
| P3 | C3 | Autism spectrum disorder Speech and language impairment in voice communication, and learning disabilities Intellectual disabilities Sensory integration disorder |
| P4 | C4 | Intellectual disabilities Visual impairment Sensory integration disorder |
| P5 | C5 | Intellectual disabilities |
| P6 | C6 | Lack of expected normal physiological development Speech and language impairment in voice communication, and learning disabilities Intellectual disabilities |
| P7 | C7 | Autism spectrum disorder Speech and language impairment in voice communication, and learning disabilities Behavioural disorders and mental health impairment Sensory integration disorder |
| P8 | C8 | Down syndrome Speech and language impairment in voice communication, and learning disabilities Psychophysical development retardation |
| P9 | C9 | Intellectual disabilities Psychophysical development retardation Behavioural disorders and mental health impairment |
| P10 | C10 | DiGeorge syndrome Intellectual disabilities |
| P11 | C11 | Cerebral palsy Intellectual disabilities Psychophysical development retardation |
| P12 | C12 | Cerebral palsy Psychophysical development retardation |
| P13 | C13 | Hyperkinetic disorders Speech and language impairment in voice communication Psychophysical development retardation |
| GC | Category | Code (Changes in Children Basic Life Needs) | Parents’ Reports (P1–P13) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P1 | P2 | P3 | P4 | P5 | P6 | P7 | P8 | P9 | P10 | P11 | P12 | P13 | |||
| GC 1 | Breathing | Easier breathing during the day | X | X | |||||||||||
| Breathing is not accelerated at rest | X | X | |||||||||||||
| Breathing more peacefully during sleep | X | ||||||||||||||
| Food and fluid intake | Better appetite | X | X | X | X | X | X | ||||||||
| Ingestion of more fluid | X | X | X | X | X | X | |||||||||
| Consuming various types of food | X | X | |||||||||||||
| Elimination of body wastes | More frequent and copious stool | X | X | X | X | ||||||||||
| Announcing the urge to go to the toilet | X | X | |||||||||||||
| Better control of urine output | X | ||||||||||||||
| Going to the toilet alone | X | ||||||||||||||
| Movement and posturing | More flexible wrist and leg joints | X | X | X | X | X | X | X | X | ||||||
| Better coordination of movements | X | X | X | X | |||||||||||
| Better physical fitness | X | X | |||||||||||||
| Better body posture and balance when walking | X | X | X | X | |||||||||||
| More independence in moving | X | X | X | X | |||||||||||
| Rest and sleep | Easier bedtime | X | X | X | X | ||||||||||
| A more peaceful dream | X | X | X | X | |||||||||||
| Longer sleep | X | X | X | X | |||||||||||
| Going to sleep alone | X | X | |||||||||||||
| Clothing | More independence in clothing | X | X | ||||||||||||
| Maintaining personal hygiene | More frequent maintenance of personal hygiene | X | X | X | X | ||||||||||
| More independence in maintaining personal hygiene | X | X | X | X | |||||||||||
| Safety | Desire to wear protective gear before horseback riding | X | X | ||||||||||||
| Relationships and child’s communication with other people (emotions, fears, moods, opinions) | Better mood throughout the day | X | X | X | X | X | X | X | X | X | X | ||||
| A higher level of calmness and patience | X | X | X | X | X | ||||||||||
| Higher self-esteem | X | X | X | X | |||||||||||
| More audible speech | X | X | |||||||||||||
| Establishing more communication with other people | X | X | X | X | |||||||||||
| Lower levels of fear of strangers and animals | X | X | X | X | |||||||||||
| Less aggression towards people | X | ||||||||||||||
| Play and recreation | More interest in playing and recreation | X | X | X | X | X | |||||||||
| Desire to stay in nature | X | X | |||||||||||||
| Reduced use of cell-phone for entertainment | X | X | |||||||||||||
| Learning and curiosity satisfaction | More interest in learning | X | X | X | |||||||||||
| Easier acquisition of school material | X | X | X | ||||||||||||
| GC 2 | Positive changes due to therapeutic and situational factors | The child’s growth and development | X | ||||||||||||
| Effect of other forms of therapeutic work and medication | X | X | X | ||||||||||||
| Positive changes due to therapeutic horseback riding | Child’s contact with the horse’s body | X | X | X | X | X | X | X | X | ||||||
| Horse movements | X | X | X | ||||||||||||
| Contact with people, exposure to sounds and sensory stimuli | X | X | X | ||||||||||||
| Aspect of Assessment | Professional Reports | Children (C1–C13) |
|---|---|---|
| Collaboration | Better collaboration; better execution of verbal instructions and tasks; better acceptance of therapy. | C5, C7, C8 |
| Communication | Establishing communication independently; better quality of communication; more frequently asked questions. | C1, C3, C7 |
| Attention and mental concentration | Improved focus on activities; longer attention; better mental concentration. | C5, C8, C9, C12 |
| Motor skills | Better posture; better movement coordination and balance in standing and walking. | C2, C4, C6, C8, C11 |
| Spatial and temporal orientation | Improved spatial orientation in moving. | C2 |
| Emotional control | Better control of emotions. | C5, C7, C9 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lovrić, R.; Farčić, N.; Mikšić, Š.; Gvozdanović Debeljak, A. Parental Perception of Changes in Basic Life Needs of Children with Disabilities after Six Months of Therapeutic Horseback Riding: A Qualitative Study. Int. J. Environ. Res. Public Health 2020, 17, 1213. https://doi.org/10.3390/ijerph17041213
Lovrić R, Farčić N, Mikšić Š, Gvozdanović Debeljak A. Parental Perception of Changes in Basic Life Needs of Children with Disabilities after Six Months of Therapeutic Horseback Riding: A Qualitative Study. International Journal of Environmental Research and Public Health. 2020; 17(4):1213. https://doi.org/10.3390/ijerph17041213
Chicago/Turabian StyleLovrić, Robert, Nikolina Farčić, Štefica Mikšić, and Aleksandra Gvozdanović Debeljak. 2020. "Parental Perception of Changes in Basic Life Needs of Children with Disabilities after Six Months of Therapeutic Horseback Riding: A Qualitative Study" International Journal of Environmental Research and Public Health 17, no. 4: 1213. https://doi.org/10.3390/ijerph17041213
APA StyleLovrić, R., Farčić, N., Mikšić, Š., & Gvozdanović Debeljak, A. (2020). Parental Perception of Changes in Basic Life Needs of Children with Disabilities after Six Months of Therapeutic Horseback Riding: A Qualitative Study. International Journal of Environmental Research and Public Health, 17(4), 1213. https://doi.org/10.3390/ijerph17041213






