Effectiveness of An Educational Intervention of Breast Cancer Screening Practices Uptake, Knowledge, and Beliefs among Yemeni Female School Teachers in Klang Valley, Malaysia: A Study Protocol for a Cluster-Randomized Controlled Trial
Abstract
1. Introduction
- i.
- An increase in the proportion of their BCS uptake
- ii.
- An increase in their BC knowledge scores
- iii.
- An improvement in their BC health beliefs (perceived susceptibility, perceived seriousness, perceived benefits, perceived barriers, health motivation, confidence).
2. Materials and Methods
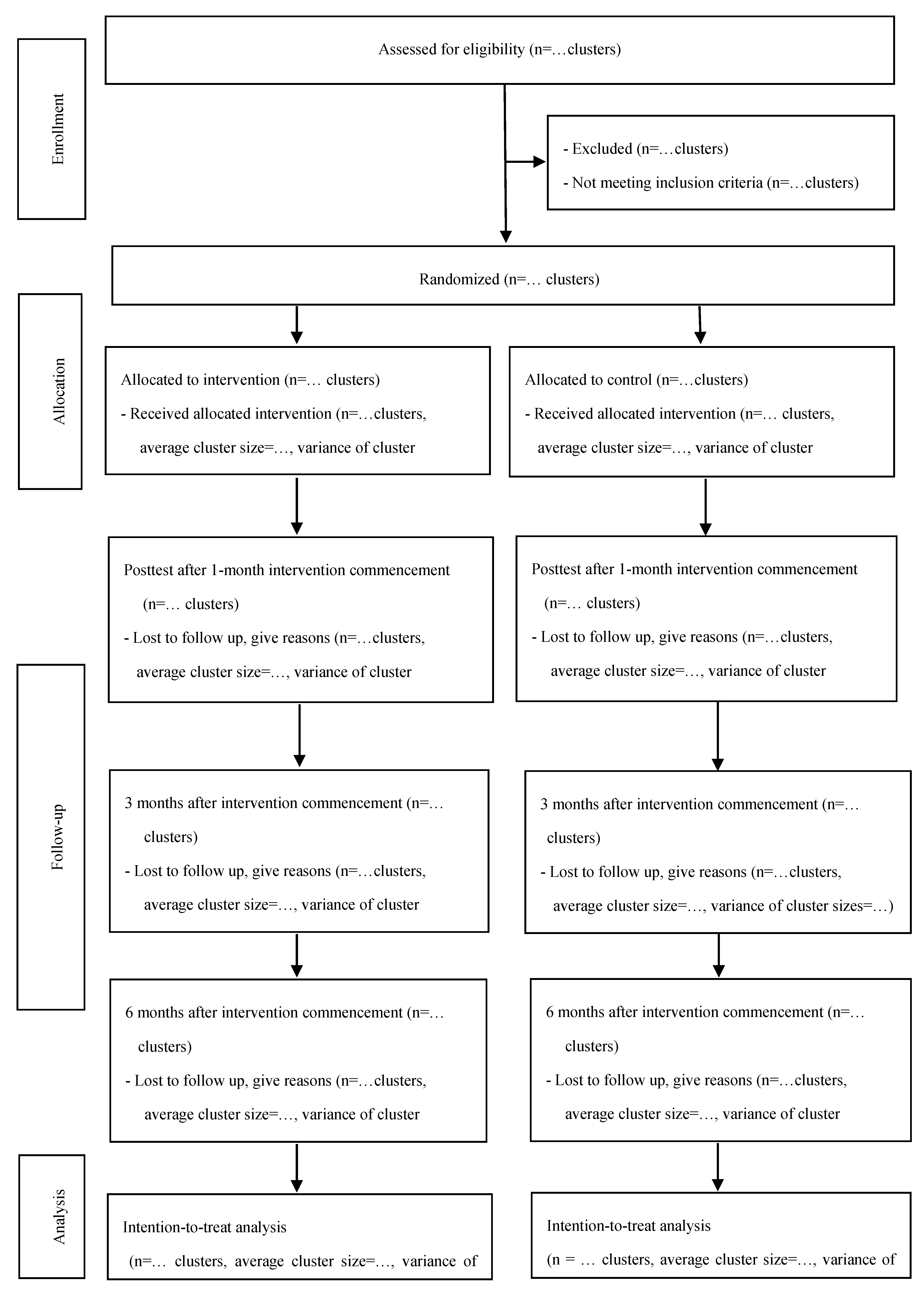
2.1. Study Design
2.2. Eligibility Criteria
2.3. Intervention
- (a)
- A 60-min PowerPoint presentation will be delivered along with a revised five-minute short video about BSE performance provided by the permission of Nuffield Health [28]. Another five-minute short video will be shown, highlighting the testimony made by one of the BC survivors. In other words, the BC survivor will share her experience with BC and give some advice on the importance of BCS and early detection.
- (b)
- A thirty-minute training session on BSE practice on a silicone breast model with several implanted lumps will be carried out. In this session, participants will acquire knowledge on palpation technique and search strategy as well as signs of BC in order to be aware of when examining the breast. Following that, participants will be asked to perform BSE based on what they have learnt.
- (c)
- At the end of the educational intervention, participants will be offered a copy of the relevant booklet containing all the information delivered to them in the educational intervention; they will be given CDs of the five-minute short video about BSE performance, and a BC logo sticker to be hung on the participants’ mirrors. The significance of distributing such materials lies in reminding the participants of the high importance of BCS practice. Along with encouraging the performance of BSE on a monthly basis, this aims at enhancing the intended messages.
- (d)
- All participants in the intervention group will continue to receive short reminder text messages for a period of 6 months. The text message will read as: “This is a gentle reminder of BSE monthly performance and BCS practice.” The key messages will provide recommendations about BCS behaviors to remind, motivate, and encourage participants to practice BCS behaviors.
Intervention Fidelity
2.4. Participant Privacy
2.5. Outcome Measures
2.5.1. Primary Outcomes
The Proportion of Participants Who Perform BSE Regularly and Proficiently
The Proportion of Participants Who Attend a Clinic for Screening CBE and Mammography
2.5.2. Secondary Outcomes
Knowledge of Breast Cancer
Beast Cancer Health Beliefs
2.5.3. Other Outcomes
Participants’ Personal Information
2.6. Translation of the Questionnaire and Study Module
2.7. Sample Size
2.8. Sampling Method
2.9. Participant Recruitment
2.10. Study Principles
2.11. Randomization
2.12. Allocation Concealment Mechanism
2.13. Statistical Analyses
2.14. Ethical Consideration
3. Discussion
4. Implication for Practice
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| BC | Breast cancer |
| BCS | Breast cancer screening |
| BSE | Breast self-examination |
| CBE | Clinical breast exam |
| HBM | Health Belief Model |
| Crct | Cluster-randomized controlled trial |
| CVI | Content validity index |
References
- Vahabi, M.; Lofters, A.; Kumar, M.; Glazier, R.H. Breast cancer screening disparities among urban immigrants: A population-based study in Ontario, Canada. BMC Public Health 2015, 15, 679. [Google Scholar] [CrossRef]
- Torre, L.A.; Islami, F.; Siegel, R.L.; Ward, E.M.; Jemal, A. Global Cancer in Women: Burden and Trends. AACR 2017, 26, 444–457. [Google Scholar] [CrossRef]
- Harhra, N.A.A.; Basaleem, H.O. Trends of Breast Cancer and its Management in the Last Twenty Years in Aden and Adjacent Governorates, Yemen. Asian Pac. J. Cancer Prev. 2012, 13, 4347–4351. [Google Scholar] [CrossRef]
- American Cancer Society, Inc. Breast Cancer Facts & Figures 2015–2016; American Cancer Society, Inc.: Atlanta, GA, USA, 2015. [Google Scholar]
- World Health Organization. Breast Cancer. Available online: https://www.who.int/cancer/prevention/diagnosis-screening/breast-cancer/en/ (accessed on 29 December 2018).
- Freund, A.; Cohen, M.; Azaiza, F.A. Culturally Tailored Intervention for Promoting Breast Cancer Screening Among Women From Faith-Based Communities in Israel: A Randomized Controlled Study. Res. Soc. Work Pract. 2017, 29, 375–388. [Google Scholar] [CrossRef]
- Tuzcu, A.; Bahar, Z.; Gözüm, S. Effects of Interventions Based on Health Behavior Models on Breast Cancer Screening Behaviors of Migrant Women in Turkey. Cancer Nurs. 2016, 39, E40–E50. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, M.; Sayın, Y.; Cengiz, H.Ö. The Effects of Training on Knowledge and Beliefs about Breast Cancer and Early Diagnosis Methods Among Women. Eur. J. Breast Health 2017, 13, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Al-Sakkaf, K.A.; Basaleem, H.O. Breast Cancer Knowledge, Perception and Breast Self- Examination Practices among Yemeni Women: An Application of the Health. Asian Pac. J. Cancer Prev. 2016, 17, 1463–1467. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, B.A. Awareness and Practice of Breast Cancer and Breast-self Examination among University Students in Yemen. Asian Pac. J. Cancer Prev. 2010, 11, 101–105. [Google Scholar]
- Heydari, E.; Noroozi, A. Comparison of Two Different Educational Methods for Teachers’ Mammography Based on the Health Belief Model. Asian Pac. J. Cancer Prev. 2015, 16, 6981–6986. [Google Scholar] [CrossRef]
- Akhtari-Zavare, M.; Juni, M.H.; Said, S.M.; Ismail, I.Z.; Latiff, L.A.; Eshkoor, S.A. Result of randomized control trial to increase breast health awareness among young females in Malaysia. BMC Public Health 2016, 16, 738. [Google Scholar] [CrossRef]
- Taymoori, P.; Molina, Y.; Roshani, D. Effects of a Randomized Controlled Trial to Increase Repeat Mammography Screening in Iranian Women. Cancer Nurs. 2015, 38, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Ghaffari, M.; Esfahani, S.N.; Rakhshanderou, S.; Koukamari, P.H. Evaluation of Health Belief Model-based intervention on breast cancer screening behaviors among health volunteers. J. Cancer Educ. 2018, 34, 904–912. [Google Scholar] [CrossRef] [PubMed]
- Champion, V.L. Instrument refinement for breast cancer screening behaviors. Nurs. Res. 1993, 42, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Champion, V.; Menon, U. Predicting mammography and breast selfexamination in African American women. Cancer Nurs. 1997, 20, 315–322. [Google Scholar] [CrossRef]
- Eskandari-Torbaghan, A.; Kalan-Farmanfarma, K.; Ansari-Moghaddam, A.; Zarei, Z. Improving breast cancer preventive behavior among female medical staff: The use of educational intervention based on health belief model. MJMS 2014, 21, 44–50. [Google Scholar]
- Mirmoammadi, A.; Parsa, P.; Khodakarami, B.; Roshanaei, G. Effect of consultation on adherence to clinical breast examination and mammography in Iranian Women: A randomized control trial. Asian Pac. J. Cancer Prev. 2018, 19, 3443–3449. [Google Scholar] [CrossRef]
- Masoudiyekta, L.; Rezaei-Bayatiyani, H.; Dashtbozorgi, B.; Gheibizadeh, M.; Malehi, A.S.; Moradi, M. Effect of education based on health belief model on the behavior of breast cancer screening in women. Asia Pac. J. Oncol. Nurs. 2018, 5, 114–120. [Google Scholar]
- Ouyang, Y.Q.; Hu, X. The effect of breast cancer health education on the knowledge, attitudes, and practice: A community health center catchment area. J. Cancer Educ. 2014, 29, 375–381. [Google Scholar] [CrossRef]
- Parsa, P.; Kandiah, M.; Zulkefli, N.A.M.; Abdul Rahman, H. Knowledge and Behavior Regarding Breast Cancer Screening among Female Teachers in Selangor, Malaysia. Asian Pac. J Cancer Prev. 2008, 9, 221–228. [Google Scholar]
- Alharbi, N.A.; Alshammari, M.S.; Almutairi, B.M.; Makboul, G.; El-Shazly, M.K. Knowledge, awareness, and practices concerning breast cancer among Kuwaiti female school teachers. Alexandria Med. J. 2012, 48, 75–82. [Google Scholar] [CrossRef]
- Alice, T.E.; Philomena, O. Breast self-examination among secondary school teachers in South-South, Nigeria: A survey of perception and practice. JPHE 2014, 6, 169–173. [Google Scholar]
- Temel, A.B.; Dağhan, S.; Kaymakçı, S.; Dönmez, R.Z.; Arabacı, Z. Effect of structured training programme on the knowledge and behaviors of breast and cervical cancer screening among the female teachers in Turkey. BMC Women’s Health 2017, 7, 123. [Google Scholar]
- Alameer, A.; Mahfouz, M.S.; Alamir, Y.; Ali, N.; Darraj, A. Effect of Health Education on Female Teachers’ Knowledge and Practices Regarding Early Breast Cancer Detection and Screening in the Jazan Area: A Quasi-Experimental Study. J. Cancer Educ. 2018, 34, 865–870. [Google Scholar] [CrossRef]
- New American Cancer Society Breast Cancer Screening Guidelines Continue Confusion, Controversy for Women and Their Providers. The North American Menopause Society. Available online: https://www.menopause.org/docs/default-source/professional/mcu1115.pdf (accessed on 29 September 2017).
- International Agency for Research on Cancer (IARC). Breast Cancer/Breast Self-Examination (BSE). 2008. Available online: http://screening.iarc.fr/breastselfexamination.php (accessed on 26 December 2016).
- Nuffield Health. Available online: https://www.nuffieldhealth.com/ (accessed on 23 December 2016).
- Wood, R.Y. Reliability and validity of a breast self-examination proficiency-rating instrument. Eval. Health Prof. 1994, 17, 418–435. [Google Scholar] [CrossRef]
- Parsa, P. Effects of Educational Interventions Pertaining to Knowledge, Beliefs, Practices on Breast Cancer Screening Behaviors among Teachers in Selangor. Ph.D. Thesis, University Putra Malaysia, Faculty of Medicine & Health Science, Selangor, Malaysia, 2008. [Google Scholar]
- McCance, K.L.; Mooney, K.H.; Smith, K.R.; Field, R. Validity and reliability of a breast cancer knowledge test. Am. J. Prev. Med. 1990, 6, 93–98. [Google Scholar] [CrossRef]
- Champion, V.L. Revised susceptibility, benefits, and barriers scale for mammography screening. Res. Nurs. Health 1999, 22, 341–348. [Google Scholar] [CrossRef]
- Lawshe, C.H. A quantitative approach to content validity. J. Pers. Psychol. 1975, 28, 563–575. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Process of Translation and Adaptaion of Instuments. Available online: www.who.int/substance_abuse/research_tools/translation/en/ (accessed on 18 September 2016).
- Lee-Lin, F.; Nguyen, T.; Pedhiwala, N.; Dieckmann, N.; Menon, U. A breast health educational program for Chinese-American women: 3-to 12-month postintervention effect. Am. J. Health Promot. 2015, 29, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.-W.; Tetzla, J.M.; Gøtzsche, P.C.; Altman, D.G.; Mann, H.; Berlin, J.A.; Dickersin, K.; Hróbjartsson, A.; Schulz, K.F.; Parulekar, W.R.; et al. SPIRIT 2013 explanation and elaboration: Guidance for protocols of clinical trials. BMJ 2013, 346, e7586. [Google Scholar] [CrossRef] [PubMed]
- Campbell, M.K.; Piaggio, G.; Elbourne, D.R.; Altman, D.G. Consort 2010 statement: Extension to cluster randomised trials. BMJ 2012, 345, e5661. [Google Scholar] [CrossRef]
- Sealed Envelope Ltd. Create a Randomization List. Available online: https://www.sealedenvelope.com/simple-randomiser/v1/lists (accessed on 2 November 2016).
| Sessions | Topics | HBM Constructs | Area of Target | Intervention |
|---|---|---|---|---|
| The normal breast |
|
|
|
|
| Knowledge of breast cancer |
|
|
|
|
| Breast cancer screening |
|
|
|
|
| Breast health awareness |
|
|
|
|
| Practice |
|
|
|
|
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noman, S.; Shahar, H.K.; Abdul Rahman, H.; Ismail, S. Effectiveness of An Educational Intervention of Breast Cancer Screening Practices Uptake, Knowledge, and Beliefs among Yemeni Female School Teachers in Klang Valley, Malaysia: A Study Protocol for a Cluster-Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 1167. https://doi.org/10.3390/ijerph17041167
Noman S, Shahar HK, Abdul Rahman H, Ismail S. Effectiveness of An Educational Intervention of Breast Cancer Screening Practices Uptake, Knowledge, and Beliefs among Yemeni Female School Teachers in Klang Valley, Malaysia: A Study Protocol for a Cluster-Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2020; 17(4):1167. https://doi.org/10.3390/ijerph17041167
Chicago/Turabian StyleNoman, Sarah, Hayati Kadir Shahar, Hejar Abdul Rahman, and Suriani Ismail. 2020. "Effectiveness of An Educational Intervention of Breast Cancer Screening Practices Uptake, Knowledge, and Beliefs among Yemeni Female School Teachers in Klang Valley, Malaysia: A Study Protocol for a Cluster-Randomized Controlled Trial" International Journal of Environmental Research and Public Health 17, no. 4: 1167. https://doi.org/10.3390/ijerph17041167
APA StyleNoman, S., Shahar, H. K., Abdul Rahman, H., & Ismail, S. (2020). Effectiveness of An Educational Intervention of Breast Cancer Screening Practices Uptake, Knowledge, and Beliefs among Yemeni Female School Teachers in Klang Valley, Malaysia: A Study Protocol for a Cluster-Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 17(4), 1167. https://doi.org/10.3390/ijerph17041167




