Non-Exercise Based Estimation of Cardiorespiratory Fitness Mediates Associations between Comorbidities and Health-Related Quality of Life in Older Korean Adults with Diabetes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Study Variables
2.2.1. Assessment of HRQoL (Dependent Variable, Y)
2.2.2. Assessment of Comorbidities (Independent Variable, X)
2.2.3. Estimation of Cardiorespiratory Fitness (Mediator, M)
2.2.4. Covariates
2.3. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Saito, I.; Inami, F.; Ikebe, T.; Moriwaki, C.; Tsubakimoto, A.; Yonemasu, K.; Ozawa, H. Impact of diabetes on health-related quality of life in a population study in Japan. Diabetes Res. Clin. Pract. 2006, 73, 51–57. [Google Scholar] [CrossRef]
- Eisele, M.; Kaduszkiewicz, H.; König, H.H.; Lange, C.; Wiese, B.; Prokein, J.; Weyerer, S.; Werle, J.; Riedel-Heller, S.G.; Luppa, M.; et al. AgeCoDe Study Group. Determinants of health-related quality of life in older primary care patients: Results of the longitudinal observational AgeCoDe study. Br. J. Gen. Pract. 2015, 65, e716–e723. [Google Scholar] [CrossRef]
- Yancik, R.; Ershler, W.; Satariano, W.; Hazzard, W.; Cohen, H.J.; Ferrucci, L. Report of the national institute on aging task force on comorbidity. J. Gerontol. Biol. Sci. Med. Sci. 2007, 62, 275–280. [Google Scholar] [CrossRef] [PubMed]
- Tran, J.; Norton, R.; Conrad, N.; Rahimian, F.; Canoy, D.; Nazarzadeh, M.; Rahimi, K. Patterns and temporal trends of comorbidity among adult patients with incident cardiovascular disease in the UK between 2000 and 2014: A population-based cohort study. PLoS Med. 2018, 15, e1002513. [Google Scholar] [CrossRef] [PubMed]
- Mata-Cases, M.; Franch-Nadal, J.; Real, J.; Cedenilla, M.; Mauricio, D. Prevalence and coprevalence of chronic comorbid conditions in patients with type 2 diabetes in Catalonia: A population-based cross-sectional study. BMJ Open 2019, 9, e031281. [Google Scholar] [CrossRef] [PubMed]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, S.; Zhang, J.; Zhang, Y.; Ernstsen, L.; Lavie, C.J.; Hooker, S.P.; Chen, Y.; Sui, X. Nonexercise estimated cardiorespiratory fitness and all-cancer mortality: The NHANES III Study. Mayo Clin. Proc. 2018, 93, 848–856. [Google Scholar] [CrossRef]
- Ekblom-Bak, E.; Ekblom, B.; Söderling, J.; Börjesson, M.; Blom, V.; Kallings, L.V.; Hemmingsson, E.; Andersson, G.; Wallin, P.; Ekblom, Ö. Sex-and age-specific associations between cardiorespiratory fitness, CVD morbidity and all-cause mortality in 266.109 adults. Prev. Med. 2019, 127, 105799. [Google Scholar] [CrossRef]
- Xu, H.; Tang, L.; Hu, Z.; Gao, F.; Yang, Y.; Qin, L.; Luo, B.A. Association between physical activity and health-related quality of life in elderly individuals with pre-diabetes in rural Hunan Province, China: A cross-sectional study. BMJ Open 2018, 8, e019836. [Google Scholar] [CrossRef]
- Subramaniam, M.; Zhang, Y.; Lau, J.H.; Vaingankar, J.A.; Abdin, E.; Chong, S.A.; Lee, E.S. Patterns of physical activity and health-related quality of life amongst patients with multimorbidity in a multi-ethnic Asian population. BMC Public Health 2019, 19, 1612. [Google Scholar] [CrossRef]
- Clennin, M.N.; Payne, J.P.; Rienzi, E.G.; Lavie, C.J.; Blair, S.N.; Pate, R.R.; Sui, X. Association between cardiorespiratory fitness and health-related quality of life among patients at risk for cardiovascular disease in Uruguay. PLoS ONE 2015, 10, e0123989. [Google Scholar] [CrossRef] [PubMed]
- Stamatakis, E.; Hamer, M.; O’Donovan, G.; Batty, G.D.; Kivimaki, M. A non-exercise testing method for estimating cardiorespiratory fitness: Associations with all-cause and cardiovascular mortality in a pooled analysis of eight population-based cohorts. Eur. Heart J. 2013, 34, 750–758. [Google Scholar] [CrossRef]
- Jurca, R.; Jackson, A.S.; LaMonte, M.J.; Morrow, J.R., Jr.; Blair, S.N.; Wareham, N.J.; Haskell, W.L.; van Mechelen, W.; Church, T.S.; Jakicic, J.M.; et al. Assessing cardiorespiratory fitness without performing exercise testing. Am. J. Prev. Med. 2005, 29, 185–193. [Google Scholar] [CrossRef]
- Song, M.; Lee, I.; Kang, H. Cardiorespiratory Fitness without Exercise Testing Can Predict All-Cause Mortality Risk in a Representative Sample of Korean Older Adults. Int. J. Environ. Res. Public Health 2019, 16, 1633. [Google Scholar] [CrossRef] [PubMed]
- Won, J.C.; Lee, J.H.; Kim, J.H.; Kang, E.S.; Won, K.C.; Kim, D.J.; Lee, M.K. Diabetes fact sheet in Korea, 2016: An appraisal of current status. Diabetes Metab. J. 2018, 42, 415–424. [Google Scholar] [CrossRef]
- Kweon, A.; Kim, Y.; Jang, M.-J.; Kim, Y.; Kim, K.; Choi, S.; Chun, C.; Khang, Y.-H.; Oh, K. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 2014, 43, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.J.; Lee, M.S.; An, S.Y.; Kim, T.H.; Han, S.J.; Kim, H.J.; Chung, Y.S.; Lee, K.W.; Kim, D.J. The relationship between diabetes mellitus and health-related quality of life in Korean adults: The fourth Korea National Health and Nutrition Examination Survey (2007–2009). Diabetes Metab. J. 2011, 35, 587–594. [Google Scholar] [CrossRef] [PubMed]
- The EuroQol Group. EuroQol—A new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef]
- Brooks, R. EuroQol: The current state of play. Health Policy 1996, 37, 53–72. [Google Scholar] [CrossRef]
- Baron, R.M.; Kenny, D.A. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986, 51, 1173–1182. [Google Scholar] [CrossRef]
- Wexler, D.J.; Grant, R.W.; Wittenberg, E.; Bosch, J.L.; Cagliero, E.; Delahanty, L.; Blais, M.A.; Meigs, J.B. Correlates of health-related quality of life in Type 2 diabetes. Diabetologia 2006, 49, 1489–1497. [Google Scholar] [CrossRef] [PubMed]
- Larkin, M.E.; Walders-Abramson, N.; Hirst, K.; Keady, J.; Ievers-Landis, C.E.; Venditti, E.M.; Yasuda, P.M. Effects of comorbid conditions on health-related quality of life in youth with Type 2 diabetes: The TODAY clinical trial. Diabetes Manag. 2015, 5, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, A.F.; Graco, M.; Rasekaba, T.M.; Parikh, S.; Berlowitz, D.J.; Lim, W.K. Relationship between health-related quality of life, comorbidities and acute health care utilization in adults with chronic conditions. Health Qual. Life Outcomes 2015, 13, 39. [Google Scholar] [CrossRef] [PubMed]
- Nelis, S.M.; Wu, Y.T.; Matthews, F.E.; Martyr, A.; Quinn, C.; Rippon, I.; Rusted, J.; Thom, J.M.; Kopelman, M.D.; Hindle, J.V.; et al. The impact of co-morbidity on the quality of life of people with dementia: Findings from the IDEAL study. Age Aging 2019, 48, 361–367. [Google Scholar] [CrossRef]
- Bavière, W.; Deprez, X.; Houvenagel, E.; Philippe, P.; Deken, V.; Flipo, R.M.; Paccou, J. Association between Comorbidities and Quality of Life in Psoriatic Arthritis: Results from a Multicentric Cross-sectional Study (PSAQUAL study). J. Rheumatol. 2019. [Google Scholar] [CrossRef]
- Lim, J.W. The impact of comorbidity on the relationship between life stress and health-related quality of life for Chinese- and Korean-American breast cancer survivors. Ethn. Health 2018, 23, 16–32. [Google Scholar] [CrossRef]
- Wang, J.W.; Sun, L.; Ding, N.; Li, J.; Gong, X.H.; Chen, X.F.; Yu, D.H.; Luo, Z.N.; Yuan, Z.P.; Yu, J.M. The association between comorbidities and the quality of life among colorectal cancer survivors in the People’s Republic of China. Patient Prefer. Adher. 2016, 10, 1071–1077. [Google Scholar] [CrossRef]
- Bennett, W.L.; Ouyang, P.; Wu, A.W.; Barone, B.B.; Stewart, K.J. Fatness and fitness: How do they influence health-related quality of life in type 2 diabetes mellitus? Health Qual. Life Outcomes 2008, 6, 110. [Google Scholar] [CrossRef]
- Lukács, A.; Varga, B.; Kiss-Tóth, E.; Soós, A.; Barkai, L. Factors influencing the diabetes-specific health-related quality of life in children and adolescents with type 1 diabetes mellitus. J. Child Health Care 2014, 18, 253–260. [Google Scholar] [CrossRef]
- Engberg, E.; Tikkanen, H.O.; Koponen, A.; Hägglund, H.; Kukkonen-Harjula, K.; Tiitinen, A.; Peltonen, J.E.; Pöyhönen-Alho, M. Cardiorespiratory fitness and health-related quality of life in women at risk for gestational diabetes. Scand. J. Med. Sci. Sports 2018, 28, 203–211. [Google Scholar] [CrossRef] [PubMed]
- Lukács, A.; Mayer, K.; Török, A.; Kiss-Tóth, E.; Barkai, L. Better cardiorespiratory fitness associated with favorable metabolic control and health-related quality of life in youths with type 1 diabetes. Acta Physiol. Hung. 2013, 100, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Wanderley, F.A.C.; Silva, G.; Marques, E.; Oliveira, J.; Mota, J.; Carvalho, J. Associations between objectively assessed physical activity levels and fitness and self-reported health-related quality of life in community-dwelling older adults. Qual. Life Res. 2011, 20, 1371–1378. [Google Scholar] [CrossRef] [PubMed]
- Strijk, J.E.; Proper, K.I.; Klaver, L.; van der Beek, A.J.; van Mechelen, W. Associations between VO2max and vitality in older workers: A cross-sectional study. BMC Public Health 2010, 1, 684. [Google Scholar] [CrossRef]
- Mugui´a-Izquierdo, D.; Santalla, A.; Lucia, A. Cardiorespiratory Fitness, Physical Activity, and Quality of Life in Patients with McArdle Disease. Med. Sci. Sports Exerc. 2015, 47, 799–808. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Perez-Cruzado, D.; Cuesta-Vargas, A.I.; Vera-Garcia, E.; Mayoral-Cleries, F. The relationship between quality of life and physical fitness in people with severe mental illness. Health Qual. Life Outcomes 2018, 16, 82. [Google Scholar] [CrossRef] [PubMed]
- Buffart, L.M.; De Backer, I.C.; Schep, G.; Vreugdenhil, A.; Brug, J.; Chinapaw, M.J. Fatigue mediates the relationship between physical fitness and quality of life in cancer survivors. J. Sci. Med. Sport 2013, 16, 99–104. [Google Scholar] [CrossRef]
- Juraschek, S.P.; Blaha, M.J.; Al-Mallah, M.H. Response to comment on Juraschek et al. cardiorespiratory fitness and incident diabetes: The FIT (Henry Ford ExercIse Testing) project. Diabetes Care 2015, 38, e194–e195. [Google Scholar] [CrossRef][Green Version]
- Juraschek, S.P.; Blaha, M.J.; Blumenthal, R.S.; Brawner, C.; Qureshi, W.; Keteyian, S.J.; Schairer, J.; Ehrman, J.K.; Al-Mallah, M.H. Cardiorespiratory fitness and incident diabetes: The FIT (Henry Ford ExercIse Testing) project. Diabetes Care 2015, 38, 1075–1081. [Google Scholar] [CrossRef]
| Variables | All (n = 1371) | Men (n = 604) | Women (n = 767) | p-Value |
|---|---|---|---|---|
| Demographics | ||||
| Age (years) | 69.1 ± 6.1 | 68.3 ± 5.9 | 69.8 ± 6.2 | <0.001 |
| Marital status, n (%) | 0.606 | |||
| Yes | 1360 (99.2) | 600 (99.3) | 760 (99.1) | |
| No | 11 (0.8) | 4 (0.7) | 7 (0.9) | |
| Living condition, n (%) | <0.001 | |||
| Live someone | 1176 (85.8) | 564 (93.4) | 612 (79.8) | |
| Alone | 195 (14.2) | 40 (6.6) | 155 (20.2) | |
| Socioeconomic Status | ||||
| Income (10,000 won/month) | 228.1 ± 113.0 | 217.1 ± 319.9 | 236.8 ± 148.6 | 0.752 |
| Education, n (%) | <0.001 | |||
| Lower than elementary school | 558 (40.7) | 122 (20.2) | 436 (56.8) | |
| Middle/high school | 597 (43.5) | 304 (50.3) | 293 (38.2) | |
| Over than college | 216 (15.8) | 178 (29.5) | 38 (5.0) | |
| Health Behavior Factors | <0.001 | |||
| Smoking, n (%) | ||||
| Never | 769 (56.1) | 87 (14.4) | 682 (88.9) | |
| Past/current | 602 (43.9) | 517 (85.6) | 85 (11.1) | |
| Weekly alcohol intake, n (%) | <0.001 | |||
| <2 | 1137 (82.9) | 394 (65.2) | 743 (96.9) | |
| ≥2 | 234 (17.1) | 210 (34.8) | 24 (3.1) | |
| Regular exercise, n (%) | <0.001 | |||
| Yes | 430 (31.4) | 243 (40.2) | 187 (24.4) | |
| No | 941 (68.6) | 361 (59.8) | 580 (75.6) | |
| Number of Comorbidity, n (%) | <0.001 | |||
| 0 | 220 (16.0) | 133 (22.0) | 87 (11.3) | |
| 1 | 567 (41.4) | 286 (47.4) | 281 (36.6) | |
| ≥2 | 584 (42.6) | 185 (30.6) | 399 (52.1) | |
| eCRF Variables | ||||
| eCRF (METs) | 7.1 ± 2.3 | 9.1 ± 1.6 | 5.6 ± 1.5 | <0.001 |
| BMI (kg/m2) | 24.7 ± 3.3 | 24.0 ± 3.0 | 25.3 ± 3.5 | <0.001 |
| RHR (beats/min) | 73.0 ± 10.2 | 72.3 ± 10.5 | 73.5 ± 9.8 | 0.023 |
| Physical activity score, n (%) | <0.001 | |||
| Level 1 | 224 (16.3) | 66 (10.9) | 158 (20.6) | |
| Level 2 | 642 (46.9) | 283 (46.9) | 359 (46.8) | |
| Level 3 | 23 (1.7) | 8 (1.3) | 15 (2.0) | |
| Level 4 | 95 (6.9) | 40 (6.6) | 55 (7.2) | |
| Level 5 | 387 (28.2) | 207 (34.3) | 180 (23.4) | |
| Health-Related Quality of Life | ||||
| EQ-5D problems | ||||
| Mobility, n (%) | 621 (45.3) | 189 (31.3) | 432 (56.3) | <0.001 |
| Self-care, n (%) | 205 (15.0) | 55 (9.1) | 150 (19.6) | <0.001 |
| Usual activities, n (%) | 409 (29.8) | 121 (20.0) | 288 (37.5) | <0.001 |
| Pain/discomfort, n (%) | 585 (42.7) | 189 (31.3) | 396 (51.6) | <0.001 |
| Anxiety/depression, n (%) | 260 (19.0) | 79 (13.1) | 181 (23.6) | <0.001 |
| EQ-5D index | 0.85 ± 0.18 | 0.90 ± 0.15 | 0.81 ± 0.19 | <0.001 |
| EQ-VAS score | 67.0 ± 22.1 | 70.1 ± 19.0 | 64.6 ± 24.0 | <0.001 |
| Variables | Number of Comorbidity | p for Linear Trend | ||
|---|---|---|---|---|
| 0 (n = 220) | 1 (n = 567) | ≥2 (n = 584) | ||
| Socio-Demographic Status | ||||
| Age (years) | 67.6 ± 6.0 | 69.3 ± 6.3 | 69.6 ± 5.9 | <0.001 |
| Marital status, n (%) | 0.194 | |||
| Yes | 219 (99.5) | 564 (99.5) | 577 (98.8) | |
| No | 1 (0.5) | 3 (0.5) | 7 (1.2) | |
| Living condition, n (%) | 0.022 | |||
| Live someone | 197 (89.5) | 491 (86.6) | 488 (83.6) | |
| Alone | 23 (10.5) | 76 (13.4) | 96 (16.4) | |
| Socio-Economic Status | ||||
| Income (10,000 won/month) | 236.5 ± 386.3 | 268.0 ± 172.2 | 186.8 ± 289.2 | 0.583 |
| Education, n (%) | 0.001 | |||
| Lower than elementary school | 71 (32.3) | 234 (41.3) | 253 (43.3) | |
| Middle/high school | 106 (48.2) | 234 (41.3) | 257 (44.0) | |
| Over than college | 43 (19.5) | 99 (17.4) | 74 (12.7) | |
| Health Behavior Factor | ||||
| Smoking, n (%) | <0.001 | |||
| Never | 102 (46.4) | 285 (50.3) | 382 (65.4) | |
| Past/current | 118 (53.6) | 282 (49.7) | 202 (34.6) | |
| Weekly alcohol intake, n (%) | 0.004 | |||
| <2 | 181 (82.3) | 444 (78.3) | 512 (87.7) | |
| ≥2 | 39 (17.7) | 123 (21.7) | 72 (12.3) | |
| Regular exercise, n (%) | 0.251 | |||
| Yes | 79 (35.9) | 172 (30.3) | 179 (30.7) | |
| No | 141 (64.1) | 395 (69.7) | 405 (69.3) | |
| HRQoL | ||||
| EQ-5D problems | ||||
| Mobility, n (%) | 69 (31.4) | 221 (39.0) | 331 (56.7) | <0.001 |
| Self-care, n (%) | 24 (10.9) | 58 (10.2) | 123 (21.1) | <0.001 |
| Usual activities, n (%) | 41 (18.6) | 136 (24.0) | 232 (39.7) | <0.001 |
| Pain/discomfort, n (%) | 73 (33.2) | 209 (36.9) | 303 (51.9) | <0.001 |
| Anxiety/depression, n (%) | 33 (15.0) | 93 (16.4) | 134 (22.9) | <0.001 |
| EQ-5D index | 0.90 ± 0.14 | 0.87 ± 0.16 | 0.81 ± 0.20 | <0.001 |
| EQ-VAS score | 69.2 ± 22.7 | 69.4 ± 20.9 | 63.9 ± 22.5 | 0.002 |
| Variables | eCRF Categories | p for Linear Trend | ||
|---|---|---|---|---|
| Low (n = 342) | Middle (n = 686) | High (n = 343) | ||
| eCRF (METs) | 5.3 ± 1.8 | 7.0 ± 1.9 | 9.3 ± 1.8 | <0.001 |
| Demographics | ||||
| Age (years) | 74.3 ± 5.5 | 67.9 ± 5.3 | 66.5 ± 5.2 | <0.001 |
| Marital status, n (%) | 0.198 | |||
| Yes | 339 (99.1) | 678 (98.8) | 343 (100.0) | |
| No | 3 (0.9) | 8 (1.2) | 0 (0.0) | |
| Living condition, n (%) | 0.003 | |||
| Live someone | 274 (80.1) | 600 (87.5) | 302 (88.0) | |
| Alone | 68 (19.9) | 86 (12.5) | 41 (12.0) | |
| Socioeconomic Status | ||||
| Income (10,000 won/month) | 291.4 ± 220.3 | 191.7 ± 253.6 | 238.0 ± 418.4 | 0.547 |
| Education, n (%) | 0.002 | |||
| Lower than elementary school | 155 (45.3) | 288 (42.0) | 115 (33.5) | |
| Middle/high school | 144 (42.1) | 284 (41.4) | 169 (49.3) | |
| Over than college | 43 (12.6) | 114 (16.6) | 59 (17.2) | |
| Health Behavior Factors | ||||
| Smoking, n (%) | 0.676 | |||
| Never | 186 (54.4) | 391 (57.0) | 192 (56.0) | |
| Past/current | 156 (45.6) | 295 (43.0) | 151 (44.0) | |
| Weekly alcohol intake, n (%) | 0.034 | |||
| <2 | 301 (88.0) | 555 (80.9) | 1.9) | |
| ≥2 | 41 (12.0) | 131 (19.1) | 62 (18.1) | |
| Regular exercise, n (%) | <0.001 | |||
| Yes | 83 (24.3) | 216 (31.5) | 131 (38.2) | |
| No | 259 (75.7) | 470 (68.5) | 212 (61.8) | |
| Number of Comorbidity, n (%) | 0.008 | |||
| 0 | 36 (10.5) | 115 (16.8) | 69 (20.1) | |
| 1 | 156 (45.6) | 270 (39.4) | 1.1) | |
| ≥2 | 150 (43.9) | 301 (43.8) | 133 (38.8) | |
| Health-Related Quality of Life | ||||
| EQ-5D problems | ||||
| Mobility, n (%) | 206 (60.2) | 288 (42.0) | (37.0) 127 | <0.001 |
| Self-care, n (%) | 85 (24.9) | 85 (12.4) | 35 (10.2) | <0.001 |
| Usual activities, n (%) | 141 (41.2) | 178 (25.9) | 90 (26.2) | <0.001 |
| Pain/discomfort, n (%) | 170 (49.7) | 271 (39.5) | 144 (42.0) | 0.041 |
| Anxiety/depression, n (%) | 64 (18.7) | 140 (20.4) | 56 (16.3) | 0.425 |
| EQ-5D index | 0.80 ± 0.22 | 0.87 ± 0.16 | 0.87 ± 0.16 | <0.001 |
| EQ-VAS score | 62.9 ± 24.9 | 67.3 ± 20.9 | 70.6 ± 20.7 | <0.001 |
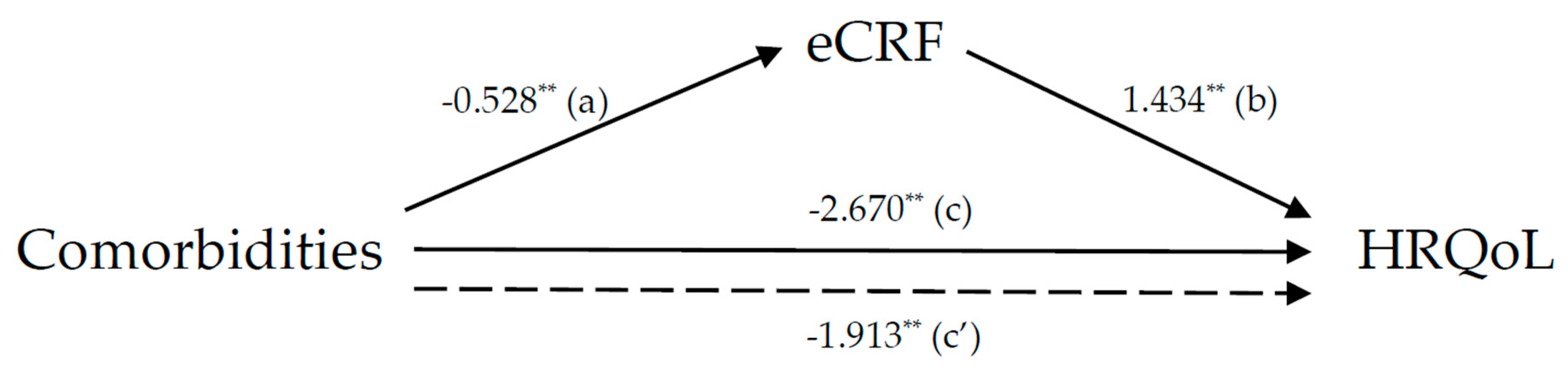
| Path | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| β (SE) | 95% CI | β (SE) | 95% CI | β (SE) | 95% CI | |
| Comorbidity → eCRF, a | −0.528 (0.063) ** | −0.652 to −0.404 | −0.388 (0.055) ** | −0.495 to −0.281 | −0.244 (0.046) ** | −0.335 to −0.154 |
| eCRF → Quality of life, b | 1.434 (0.258) ** | 0.928 to 1.940 | 0.996 (0.300) ** | 0.407 to 1.586 | 1.153 (0.358) * | 0.452 to 1.855 |
| Total effect, c | −2.670 (0.611) ** | −3.868 to −1.472 | −2.327 (0.609) ** | −3.522 to −1.133 | −2.321 (0.613) ** | −3.522 to −1.119 |
| Direct effect, c′ | −1.913 (0.619) * | −3.128 to −0.698 | −1.941 (0.618) * | −3.153 to −0.729 | −2.039 (0.617) * | −3.249 to −0.829 |
| Indirect effect, ab | −0.757 (0.168) | −1.104 to −0.453 | −0.387 (0.135) | −0.672 to −0.145 | −0.282 (0.107) | −0.517 to −0.095 |
| Ratio of indirect to total effect mediated (%) | 28.4 | 16.1 | 12.1 | |||
| Sobel test | −4.632 ** | −3.004 ** | −2.753 ** | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, I.; Kim, S.; Kang, H. Non-Exercise Based Estimation of Cardiorespiratory Fitness Mediates Associations between Comorbidities and Health-Related Quality of Life in Older Korean Adults with Diabetes. Int. J. Environ. Res. Public Health 2020, 17, 1164. https://doi.org/10.3390/ijerph17041164
Lee I, Kim S, Kang H. Non-Exercise Based Estimation of Cardiorespiratory Fitness Mediates Associations between Comorbidities and Health-Related Quality of Life in Older Korean Adults with Diabetes. International Journal of Environmental Research and Public Health. 2020; 17(4):1164. https://doi.org/10.3390/ijerph17041164
Chicago/Turabian StyleLee, Inhwan, Shinuk Kim, and Hyunsik Kang. 2020. "Non-Exercise Based Estimation of Cardiorespiratory Fitness Mediates Associations between Comorbidities and Health-Related Quality of Life in Older Korean Adults with Diabetes" International Journal of Environmental Research and Public Health 17, no. 4: 1164. https://doi.org/10.3390/ijerph17041164
APA StyleLee, I., Kim, S., & Kang, H. (2020). Non-Exercise Based Estimation of Cardiorespiratory Fitness Mediates Associations between Comorbidities and Health-Related Quality of Life in Older Korean Adults with Diabetes. International Journal of Environmental Research and Public Health, 17(4), 1164. https://doi.org/10.3390/ijerph17041164






