Malay Version of Exercise Self-Efficacy: A Confirmatory Analysis among Malaysians with Type 2 Diabetes Mellitus
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Inclusion and Exclusion Criteria of Participants
2.3. Sample Size Determination
2.4. Instrument
2.5. Ethical Consideration
2.6. Data Analysis
3. Results
3.1. Demographic Characteristics
3.2. Confirmatory Factor Analysis
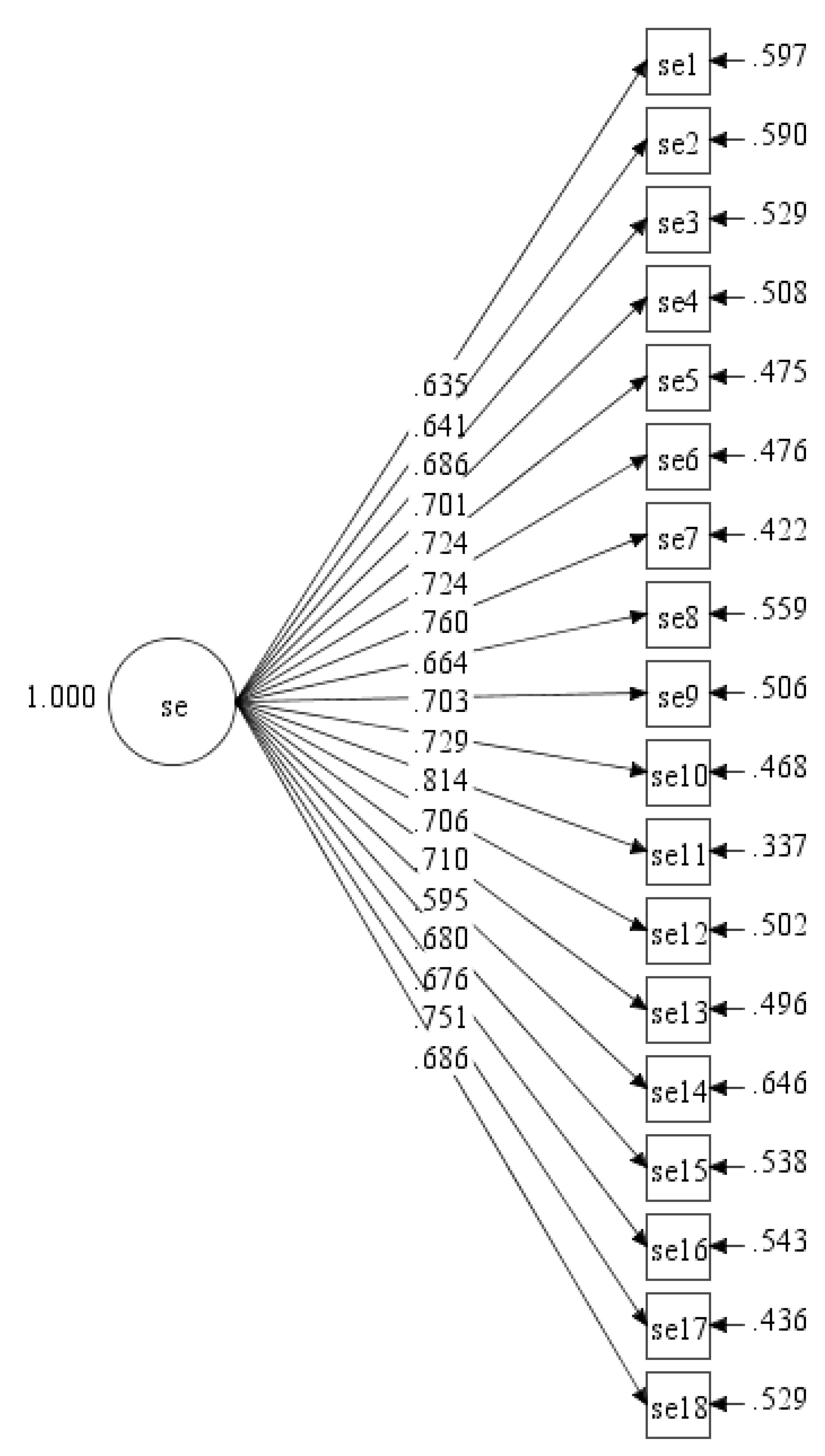
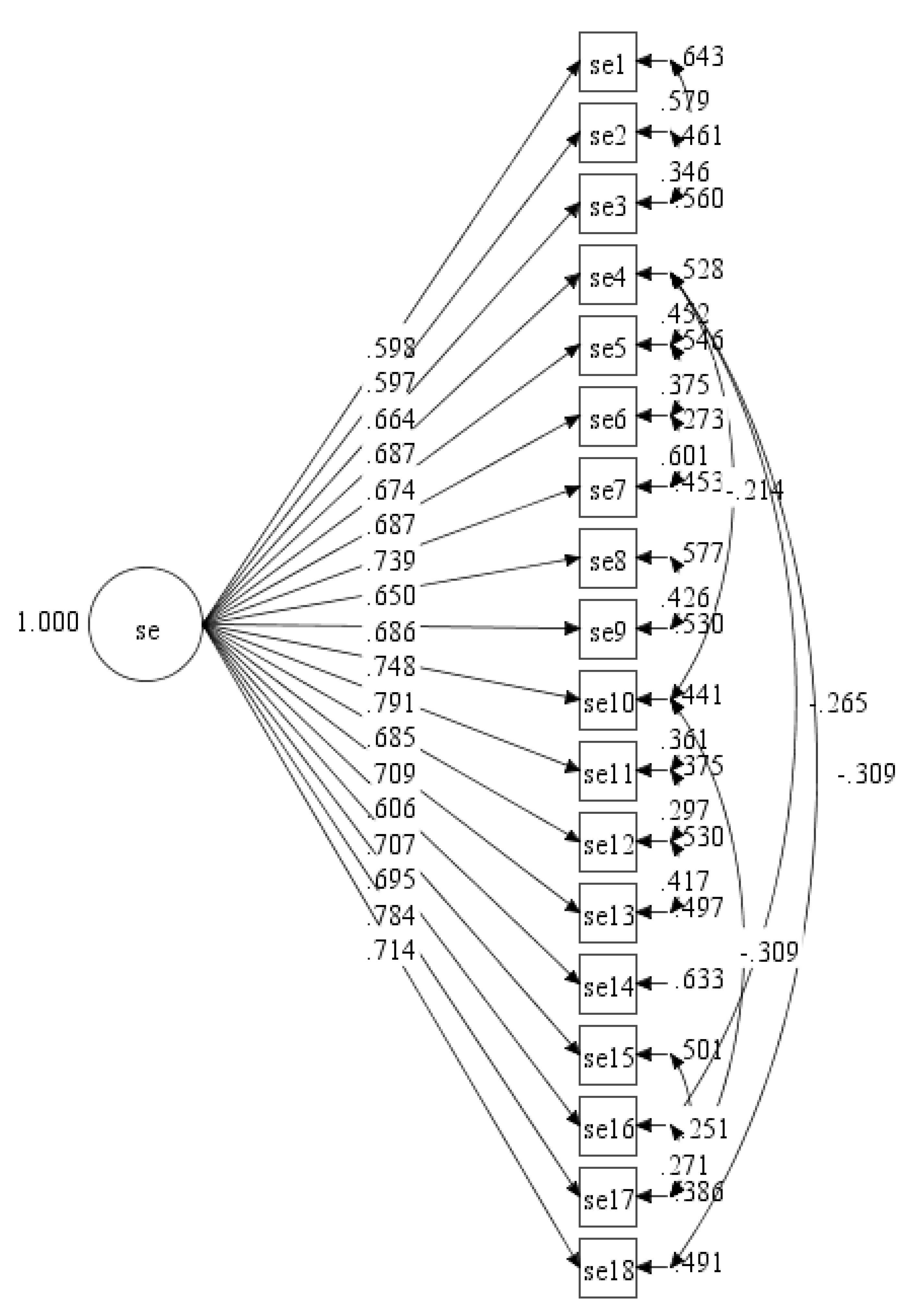
3.2.1. ESE-M with Single Factor
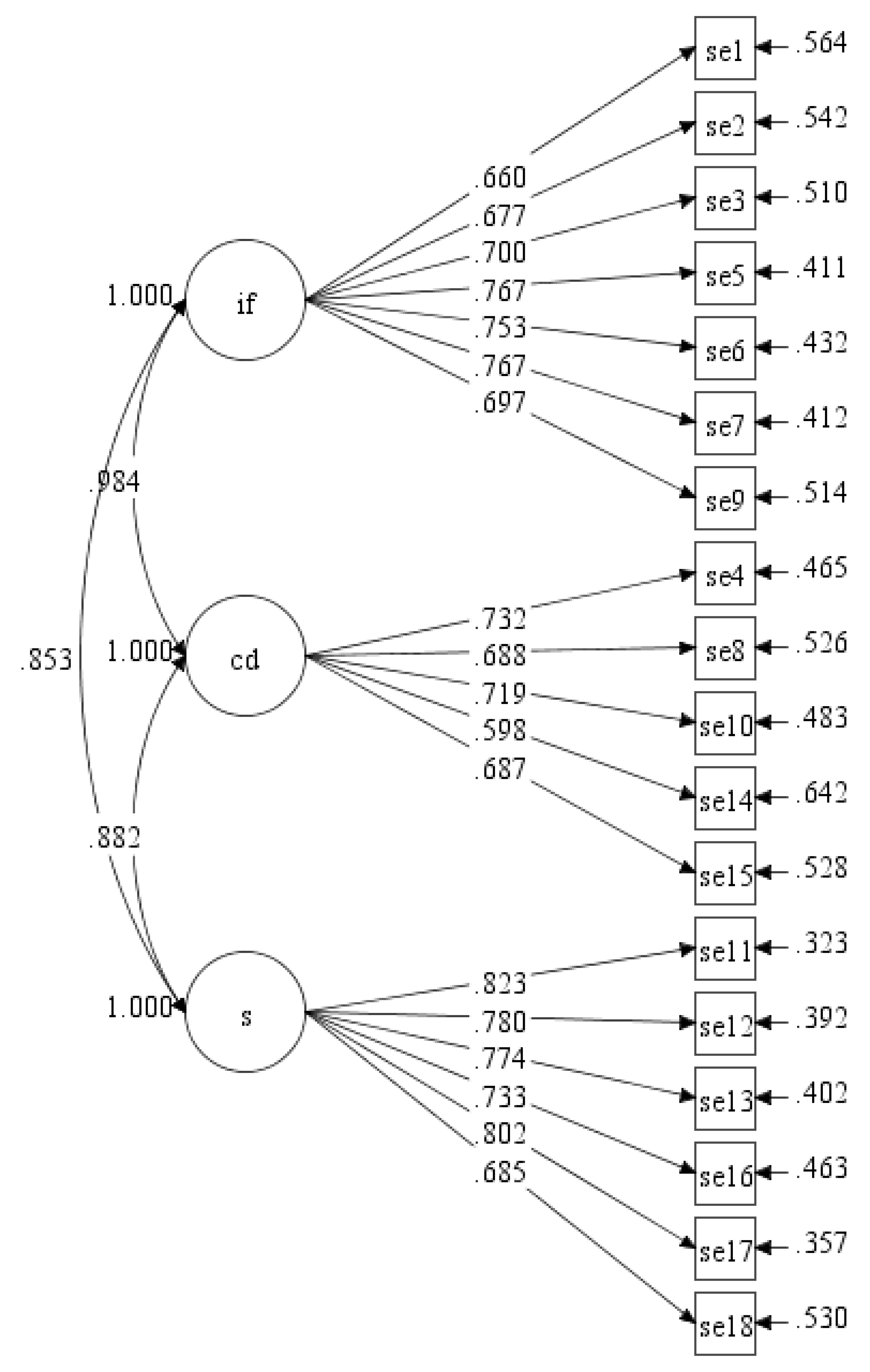
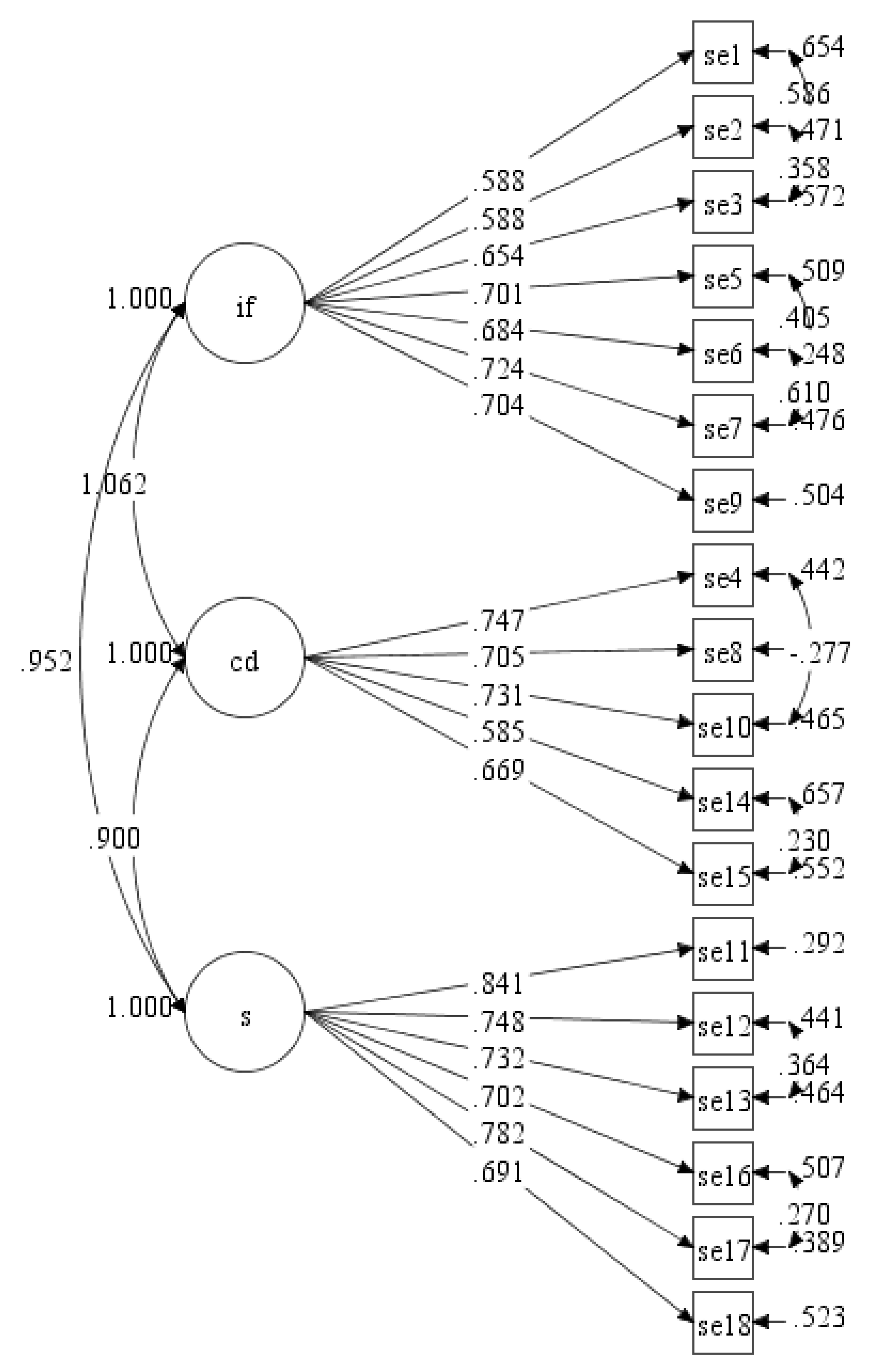
3.2.2. ESE-M with Three Factors
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Physical Activity. Available online: https://www.who.int/dietphysicalactivity/pa/en/ (accessed on 24 October 2019).
- Anderson, L.; Oldridge, N.; Thompson, D.R.; Zwisler, A.D.; Rees, K.; Martin, N.; Taylor, R.S. Exercise-based cardiac rehabilitation for coronary heart disease: Cochrane systematic review and meta-analysis. J. Am. Coll. Cardiol. 2016, 67, 1–12. [Google Scholar] [CrossRef]
- Institute for Public Health. National Health and Morbidity Survey 2015: Non-Communicable Diseases, Risk Factors & Other Health Problems; Ministry of Health Malaysia: Kuala Lumpur, Malaysia, 2015; Volume II, NMRR-14-1064-21877.
- Hussein, Z.; Taher, S.W.; Singh, H.K.G.; Swee, W.C.S. Diabetes care in Malaysia: Problems, new models, and solutions. Ann. Glob. Health 2015, 81, 851–862. [Google Scholar] [CrossRef]
- Tan, M.Y.; Magarey, J. Self-care practices of Malaysian adults with diabetes and sub-optimal glycaemic control. Patient Educ. Couns. 2008, 72, 252–267. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-Efficacy: The Exercise of Control; W. H. Freeman: New York, NY, USA, 1997. [Google Scholar]
- Bandura, A. Self-efficacy. In Encyclopedia of Human Behavior; Ramachaudran, V.S., Ed.; Academic Press: New York, NY, USA, 1994; Volume 4, pp. 71–81. [Google Scholar]
- Zelle, D.M.; Corpeleijn, E.; Klaassen, G.; Schutte, E.; Navis, G.; Bakker, S.J. Fear of movement and low self-efficacy are important barriers in physical activity after renal transplantation. PLoS ONE 2016, 11, e0147609. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Social Foundations of Thought and Action; Prentice Hall: Englewood Cliffs, NJ, USA, 1986. [Google Scholar]
- Resnick, B.; Jenkins, L.S. Testing the reliability and validity of the self-efficacy for exercise scale. Nurs. Res. 2000, 49, 154–159. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.; Jang, H.; Pender, N.J. Psychometric evaluation of the exercise self-efficacy scale among Korean adults with chronic diseases. Res. Nurs. Health 2001, 24, 68–76. [Google Scholar] [CrossRef]
- Lee, L.L.; Perng, S.J.; Ho, C.C.; Hsu, H.M.; Lau, S.C.; Arthur, A. A preliminary reliability and validity study of the Chinese version of the self-efficacy for exercise scale for older adults. Int. J. Nurs. Stud. 2009, 46, 230–238. [Google Scholar] [CrossRef]
- Rydwik, E.; Hovmöller, F.; Boström, C. Aspects of reliability and validity of the Swedish version of the Self-Efficacy for Exercise Scale for older people. Physiother. Theory Pract. 2014, 30, 131–137. [Google Scholar] [CrossRef]
- Sabo, A.; Kueh, Y.C.; Kuan, G. Psychometric properties of the Malay version of the self-efficacy for exercise scale. PLoS ONE 2019, 14, e0215698. [Google Scholar] [CrossRef]
- Resnick, B.; Luisi, D.; Vogel, A.; Junaleepa, P. Reliability and validity of the self–efficacy for exercise and outcome expectations for exercise scales with minority older adults. J. Nurs. Meas. 2004, 12, 235–248. [Google Scholar] [CrossRef]
- Wu, S.F.V.; Courtney, M.; Edwards, H.; McDowell, J.; Shortridge-Baggett, L.M.; Chang, P.J. Development and validation of the Chinese version of the Diabetes Management Self-efficacy Scale. Int. J. Nurs. Stud. 2008, 45, 534–542. [Google Scholar]
- Löve, J.; Moore, C.D.; Hensing, G. Validation of the Swedish translation of the general self-efficacy scale. Qual. Life Res. 2012, 21, 1249–1253. [Google Scholar] [CrossRef] [PubMed]
- Kline, R.B. Principles and Practice of Structural Equation Modeling; Guilford Publications: New York, NY, USA, 2015. [Google Scholar]
- Shah, R.; Goldstein, S.M. Use of structural equation modelling in operations management research: Looking back and forward. J. Oper. Manag. 2006, 24, 148–169. [Google Scholar] [CrossRef]
- Kim, Y.H. Application of the transtheoretical model to identify psychological constructs influencing exercise behavior: A questionnaire survey. Int. J. Nurs. Stud. 2007, 44, 936–944. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Kosma, M. Psychosocial and environmental correlates of physical activity among Korean older adults. Res. Aging 2013, 35, 750–767. [Google Scholar] [CrossRef]
- Brislin, R.W. Back-translation for cross-cultural research. J. Cross Cult. Psychol. 1970, 1, 185–216. [Google Scholar] [CrossRef]
- Muthén, L.K.; Muthén, B.O. Mplus User’s Guide, 8th ed.; Muthén & Muthén: Los Angeles, CA, USA, 1998. [Google Scholar]
- Wang, J.; Wang, X. Structural Equation Modeling: Applications Using Mplus; John Wiley & Sons Ltd.: Chichester, UK, 2019. [Google Scholar]
- Yuan, K.H.; Bentler, P.M. 5. Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociol. Methodol. 2000, 30, 165–200. [Google Scholar] [CrossRef]
- Cabrera-Nguyen, P. Author guidelines for reporting scale development and validation results in the Journal of the Society for Social Work and Research. J. Soc. Soc. Work Res. 2010, 1, 99–103. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2013. [Google Scholar]
- DeVon, H.A.; Block, M.E.; Moyle-Wright, P.; Ernst, D.M.; Hayden, S.J.; Lazzara, D.J.; Savoy, S.M.; Kostas-Polston, E. A psychometric toolbox for testing validity and reliability. J. Nurs. Scholarsh. 2007, 39, 155–164. [Google Scholar] [CrossRef]
- Ford, J.K.; MacCallum, R.C.; Tait, M. The application of exploratory factor analysis in applied psychology: A critical review and analysis. Pers. Psychol. 1986, 39, 291–314. [Google Scholar] [CrossRef]
- Raykov, T.; Marcoulides, G.A. Scale Reliability Evaluation Under Multiple Assumption Violations. Struct. Equ. Modeling Multidiscip. J. 2016, 23, 302–313. [Google Scholar] [CrossRef]
- Tseng, W.T.; Dörnyei, Z.; Schmitt, N. A new approach to assessing strategic learning: The case of self-regulation in vocabulary acquisition. Appl. Linguist. 2006, 27, 78–102. [Google Scholar] [CrossRef]
- Kueh, Y.C.; Morris, T.; Borkoles, E.; Shee, H. Modelling of diabetes knowledge, attitudes, self-management, and quality of life: A cross-sectional study with an Australian sample. Health Qual. Life Outcomes 2015, 13, 129. [Google Scholar] [CrossRef] [PubMed]
- Dutton, G.R.; Tan, F.; Provost, B.C.; Sorenson, J.L.; Allen, B.; Smith, D. Relationship between self-efficacy and physical activity among patients with type 2 diabetes. J. Behav. Med. 2009, 32, 270–277. [Google Scholar] [CrossRef]
- Qiu, S.; Sun, Z.; Cai, X.; Liu, L.; Yang, B. Improving patients’ adherence to physical activity in diabetes mellitus: A review. Diabetes Metab. J. 2012, 36, 1–5. [Google Scholar] [CrossRef]
- Kueh, Y.C.; Sabo, A.; Kuan, G. BASES Conference 2019—Programme and Abstracts: Structural relationship of social support, decisional balance, self-efficacy and satisfaction in exercise among undergraduate university students. J. Sports Sci. 2019, 37, 22. [Google Scholar]
- Rizal, H.; Hajar, M.S.; Muhamad, A.S.; Kueh, Y.C.; Kuan, G. The Effect of Brain Breaks on Physical Activity Behaviour among Primary School Children: A Transtheoretical Perspective. Int. J. Environ. Res. Public Health 2019, 16, 4283. [Google Scholar] [CrossRef]
- Liu, T.K.; Kuan, G.; Arifin, W.N.; Kueh, Y.C. Psychometric Properties of the Self-Efficacy Scale among Undergraduate Students in Malaysia. MJMS 2019, 26, 119–128. [Google Scholar]
- Van der Heijden, M.; Pouwer, F.; Pop, V. Psychometric properties of the exercise self-efficacy scale in Dutch primary care patients with type 2 diabetes mellitus. Int. J. Behav. Med. 2014, 21, 394–401. [Google Scholar] [CrossRef]
- Noroozi, A.; Ghofranipour, F.; Heydarnia, A.R.; Nabipour, I.; Tahmasebi, R.; Tavafian, S.S. The Iranian version of the exercise self-efficacy scale (ESES) Factor structure, internal consistency and construct validity. Health Educ. J. 2011, 70, 21–31. [Google Scholar] [CrossRef]
| Characteristics | Frequencies | Percentage | Mean (SD) |
|---|---|---|---|
| Gender | |||
| Male | 172 | 52.0% | |
| Female | 159 | 48.0% | |
| Age | 62.64 (0.56) | ||
| Ethnicity | |||
| Malay | 296 | 89.4% | |
| Chinese | 25 | 7.6% | |
| Indian | 6 | 1.8% | |
| Others | 4 | 1.2% | |
| Education background | |||
| Primary | 87 | 26.3% | |
| Secondary | 158 | 47.7% | |
| Diploma | 60 | 18.1% | |
| Bachelor degree | 26 | 7.9% | |
| Occupation | |||
| Working/Business | 92 | 27.9% | |
| Pensioners | 139 | 42.0% | |
| Not working/Housewife | 100 | 30.1% | |
| Diabetic period | |||
| Less than 5 years | 38 | 11.5% | |
| 5 years or longer | 32 | 9.7% | |
| 10 years or longer | 83 | 25.1% | |
| 20 years or longer | 178 | 53.8% | |
| HbA1c (mmol/mol) | 76.90 (1.33) | ||
| BMI (kg/m2) | 27.28 (0.28) |
| Model | CFI | TLI | SRMR | RMSEA (90% CI) | RMSEA (p-Value) |
|---|---|---|---|---|---|
| Initial model | 0.760 | 0.728 | 0.071 | 0.114 (0.106, 0.122) | <0.001 |
| Final model a | 0.952 | 0.938 | 0.044 | 0.054 (0.044, 0.065) | 0.228 |
| Model | CFI | TLI | SRMR | RMSEA (90% CI) | RMSEA (p-Value) |
|---|---|---|---|---|---|
| Initial model | 0.790 | 0.756 | 0.066 | 0.108 (0.100, 0.116) | <0.001 |
| Final model a | 0.891 | 0.863 | 0.049 | 0.081 (0.072, 0.090) | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hidrus, A.; Kueh, Y.C.; Norsa’adah, B.; Kuan, G. Malay Version of Exercise Self-Efficacy: A Confirmatory Analysis among Malaysians with Type 2 Diabetes Mellitus. Int. J. Environ. Res. Public Health 2020, 17, 922. https://doi.org/10.3390/ijerph17030922
Hidrus A, Kueh YC, Norsa’adah B, Kuan G. Malay Version of Exercise Self-Efficacy: A Confirmatory Analysis among Malaysians with Type 2 Diabetes Mellitus. International Journal of Environmental Research and Public Health. 2020; 17(3):922. https://doi.org/10.3390/ijerph17030922
Chicago/Turabian StyleHidrus, Aizuddin, Yee Cheng Kueh, Bachok Norsa’adah, and Garry Kuan. 2020. "Malay Version of Exercise Self-Efficacy: A Confirmatory Analysis among Malaysians with Type 2 Diabetes Mellitus" International Journal of Environmental Research and Public Health 17, no. 3: 922. https://doi.org/10.3390/ijerph17030922
APA StyleHidrus, A., Kueh, Y. C., Norsa’adah, B., & Kuan, G. (2020). Malay Version of Exercise Self-Efficacy: A Confirmatory Analysis among Malaysians with Type 2 Diabetes Mellitus. International Journal of Environmental Research and Public Health, 17(3), 922. https://doi.org/10.3390/ijerph17030922






