Computerized Clinical Decision Support System for Prompting Brief Alcohol Interventions with Treatment Seeking Smokers: A Sex-Based Secondary Analysis of a Cluster Randomized Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Sample
2.2. Study Variables
2.2.1. Treatment Arms
2.2.2. Patients’ Sex
2.2.3. Outcomes
2.3. Statistical Analyses
2.4. Ethical Considerations
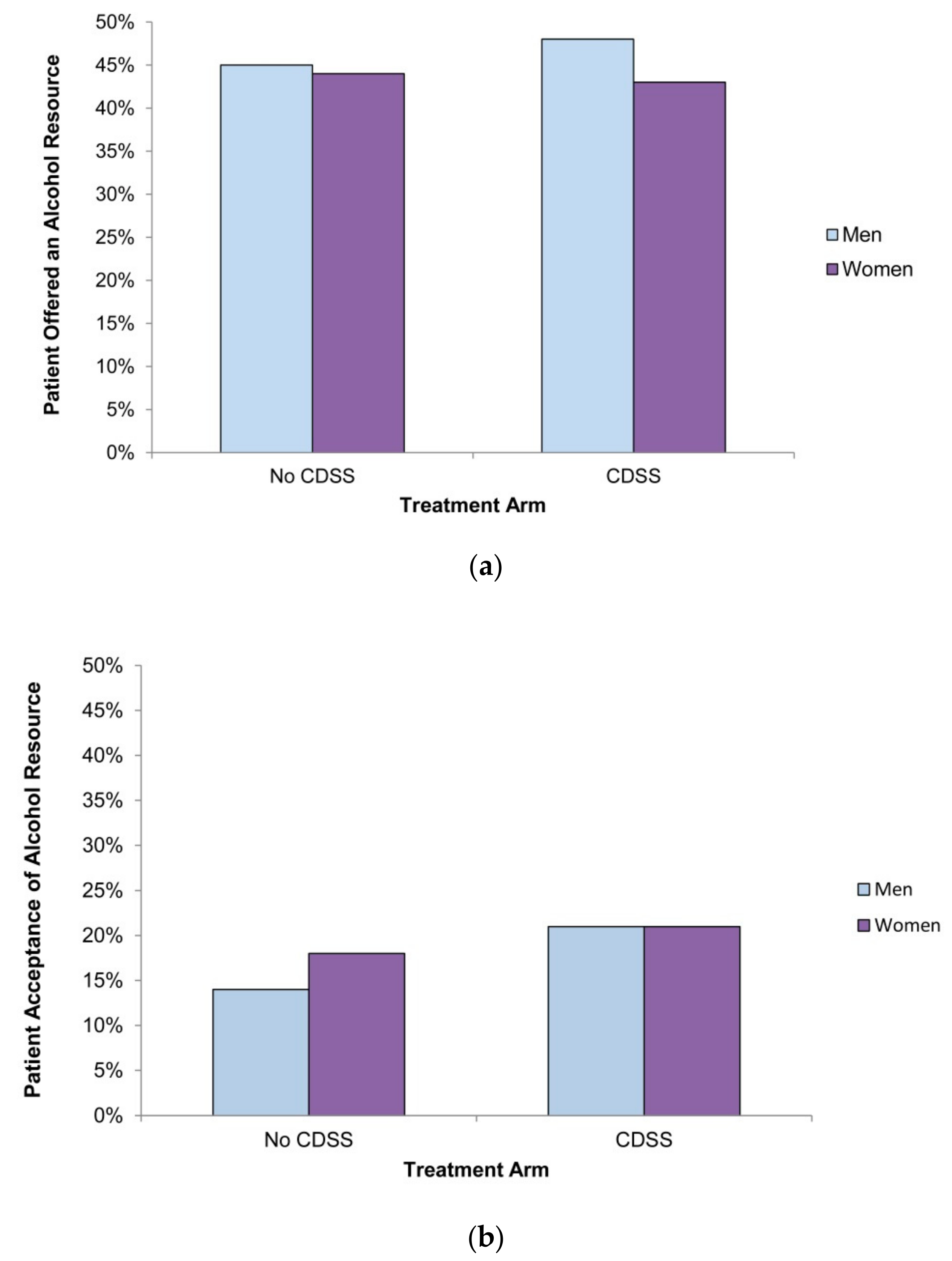
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Yasin, Y.J.; Banoub, J.A.M. GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018, 392, 1015–1035. [Google Scholar]
- Statistics Canada. Canadian Tobacco, Alcohol and Drugs Survey (CTADS): Summary of Results for 2017. Available online: https://www.canada.ca/en/health-canada/services/canadian-tobacco-alcohol-drugs-survey/2017-summary.html (accessed on 9 December 2019).
- Young, S.W.; Candido, E.; Klein-Geltink, J.; Giesbrecht, N. Preventing alcohol-related cancer: What if everyone drank within the guidelines? Can. J. Public Health 2018, 109, 70–78. [Google Scholar] [CrossRef]
- Pennings, E.J.; Leccese, A.P.; Wolff, F.A.D. Effects of concurrent use of alcohol and cocaine. Addiction 2002, 97, 773–783. [Google Scholar] [CrossRef] [PubMed]
- Chihuri, S.; Li, G.; Chen, Q. Interaction of marijuana and alcohol on fatal motor vehicle crash risk: A case–control study. Inj. Epidemiol. 2017, 4, 8. [Google Scholar] [CrossRef] [PubMed]
- Yurasek, A.M.; Aston, E.R.; Metrik, J. Co-use of alcohol and cannabis: A review. Curr. Addict. Rep. 2017, 4, 184–193. [Google Scholar] [CrossRef]
- Pennay, A.; Lubman, D.I.; Miller, P. Combining energy drinks and alcohol: A recipe for trouble? Aust. Fam. Physician 2011, 40, 104. [Google Scholar]
- Franceschi, S.; Talamini, R.; Barra, S.; Barón, A.E.; Negri, E.; Bidoli, E.; Serraino, D.; La Vecchia, C. Smoking and drinking in relation to cancers of the oral cavity, pharynx, larynx, and esophagus in northern Italy. Cancer Res. 1990, 50, 6502–6507. [Google Scholar]
- Pelucchi, C.; Gallus, S.; Garavello, W.; Bosetti, C.; La, C.V. Cancer risk associated with alcohol and tobacco use: Focus on upper aero-digestive tract and liver. Alcohol Res. Health 2006, 29, 193–198. [Google Scholar]
- Dawson, D.A. Drinking as a risk factor for sustained smoking. Drug Alcohol Depend. 2000, 59, 235–249. [Google Scholar] [CrossRef]
- Falk, D.E.; Yi, H.-Y.; Hiller-Sturmhöfel, S. An epidemiologic analysis of co-occurring alcohol and tobacco use and disorders: Findings from the National Epidemiologic Survey on Alcohol and Related Conditions. Alcohol Res. Health 2006, 29, 162. [Google Scholar]
- Kaner, E.F.; Beyer, F.R.; Muirhead, C.; Campbell, F.; Pienaar, E.D.; Bertholet, N.; Daeppen, J.B.; Saunders, J.B.; Burnand, B. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst. Rev. 2018. [Google Scholar] [CrossRef] [PubMed]
- Canadian Institute of Health Information (CIHI). How Canada Compares: Results From The Commonwealth Fund’s 2016 International Health Policy Survey of Adults in 11 Countries—Accessible Report 2017; Canadian Institute of Health Information: Ottawa, ON, Canada, 2017. [Google Scholar]
- Curry, S.J.; Krist, A.H.; Owens, D.K.; Barry, M.J.; Caughey, A.B.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Kemper, A.R.; Kubik, M. Screening and behavioral counseling interventions to reduce unhealthy alcohol use in adolescents and adults: US Preventive Services Task Force recommendation statement. JAMA 2018, 320, 1899–1909. [Google Scholar] [PubMed]
- RNAO. Engaging Clients Who Use Substances; Registered Nurses’ Association of Ontario: Toronto, ON, Canada, 2015. [Google Scholar]
- Kaner, E.; Heather, N.; Brodie, J.; Lock, C.A.; McAvoy, B.R. Patient and practitioner characteristics predict brief alcohol intervention in primary care. Br. J. Gen. Pract. 2001, 51, 822–827. [Google Scholar] [PubMed]
- McKnight-Eily, L.R.; Liu, Y.; Brewer, R.D.; Kanny, D.; Lu, H.; Denny, C.H.; Balluz, L.; Collins, J. Vital signs: Communication between health professionals and their patients about alcohol use—44 states and the District of Columbia, 2011. Mmwr. Morb. Mortal. Wkly. Rep. 2014, 63, 16. [Google Scholar] [PubMed]
- Bertakis, K.D.; Azari, R. Determinants of physician discussion regarding tobacco and alcohol abuse. J. Health Commun. 2007, 12, 513–525. [Google Scholar] [CrossRef] [PubMed]
- Volk, R.J.; Steinbauer, J.R.; Cantor, S.B. Patient factors influencing variation in the use of preventive interventions for alcohol abuse by primary care physicians. J. Stud. Alcohol 1996, 57, 203–209. [Google Scholar] [CrossRef]
- Denny, C.H.; Serdula, M.K.; Holtzman, D.; Nelson, D.E. Physician advice about smoking and drinking: Are US adults being informed? Am. J. Prev. Med. 2003, 24, 71–74. [Google Scholar] [CrossRef]
- Angus, C.; Brown, J.; Beard, E.; Gillespie, D.; Buykx, P.; Kaner, E.F.; Michie, S.; Meier, P. Socioeconomic inequalities in the delivery of brief interventions for smoking and excessive drinking: Findings from a cross-sectional household survey in England. BMJ Open 2019, 9, e023448. [Google Scholar] [CrossRef]
- Bachrach, R.L.; Blosnich, J.R.; Williams, E.C. Alcohol screening and brief intervention in a representative sample of veterans receiving primary care services. J. Subst. Abus. Treat. 2018, 95, 18–25. [Google Scholar] [CrossRef]
- Lock, C.A.; Kaner, E.F. Implementation of brief alcohol interventions by nurses in primary care: Do non-clinical factors influence practice? Fam. Pract. 2004, 21, 270–275. [Google Scholar] [CrossRef]
- Williams, E.C.; Lapham, G.T.; Rubinsky, A.D.; Chavez, L.J.; Berger, D.; Bradley, K.A. Influence of a targeted performance measure for brief intervention on gender differences in receipt of brief intervention among patients with unhealthy alcohol use in the Veterans Health Administration. J. Subst. Abus. Treat. 2017, 81, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Rapley, T.; May, C.; Kaner, E.F. Still a difficult business? Negotiating alcohol-related problems in general practice consultations. Soc. Sci. Med. 2006, 63, 2418–2428. [Google Scholar] [CrossRef] [PubMed]
- Tam, C.W.M.; Zwar, N.; Markham, R. Australian general practitioner perceptions of the detection and screening of at-risk drinking, and the role of the AUDIT-C: A qualitative study. Bmc Fam. Pract. 2013, 14, 121. [Google Scholar] [CrossRef] [PubMed]
- Capraro, R.L. Why college men drink: Alcohol, adventure, and the paradox of masculinity. J. Am. Coll. Health 2000, 48, 307–315. [Google Scholar] [CrossRef] [PubMed]
- Ricciardelli, L.A.; Connor, J.P.; Williams, R.J.; Young, R.M. Gender stereotypes and drinking cognitions as indicators of moderate and high risk drinking among young women and men. Drug Alcohol Depend. 2001, 61, 129–136. [Google Scholar] [CrossRef]
- Erol, A.; Karpyak, V.M. Sex and gender-related differences in alcohol use and its consequences: Contemporary knowledge and future research considerations. Drug Alcohol Depend. 2015, 156, 1–13. [Google Scholar] [CrossRef]
- National Institute on Alcohol Abuse and Alcoholism. Are Women More Vulnerable to Alcohol’s Effects? Available online: https://pubs.niaaa.nih.gov/publications/aa46.htm#:~:targetText=In%20general%2C%20women%20have%20less,the%20blood%20faster%20than%20men (accessed on 29 January 2020).
- Canadian Institute for Health Information. Alcohol Harm on the Rise for Canadian Women. Available online: https://www.cihi.ca/en/alcohol-harm-on-the-rise-for-canadian-women (accessed on 9 December 2019).
- Myran, D.T.; Hsu, A.T.; Smith, G.; Tanuseputro, P. Rates of emergency department visits attributable to alcohol use in Ontario from 2003 to 2016: A retrospective population-level study. CMAJ 2019, 191, E804–E810. [Google Scholar] [CrossRef]
- Lobach, D.F.; Hammond, W.E. Computerized decision support based on a clinical practice guideline improves compliance with care standards. Am. J. Med. 1997, 102, 89–98. [Google Scholar] [CrossRef]
- Coma, E.; Medina, M.; Méndez, L.; Hermosilla, E.; Iglesias, M.; Olmos, C.; Calero, S. Effectiveness of electronic point-of-care reminders versus monthly feedback to improve adherence to 10 clinical recommendations in primary care: A cluster randomized clinical trial. Bmc Med. Inform. Decis. Mak. 2019, 19, 245. [Google Scholar] [CrossRef]
- Kawamoto, K.; Houlihan, C.A.; Balas, E.A.; Lobach, D.F. Improving clinical practice using clinical decision support systems: A systematic review of trials to identify features critical to success. BMJ 2005, 330, 765. [Google Scholar] [CrossRef]
- Pearson, S.-A.; Moxey, A.; Robertson, J.; Hains, I.; Williamson, M.; Reeve, J.; Newby, D. Do computerised clinical decision support systems for prescribing change practice? A systematic review of the literature (1990–2007). Bmc Health Serv. Res. 2009, 9, 154. [Google Scholar] [CrossRef] [PubMed]
- Shojania, K.G.; Jennings, A.; Mayhew, A.; Ramsay, C.R.; Eccles, M.P.; Grimshaw, J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database Syst. Rev. 2009, 3, CD001096. [Google Scholar] [CrossRef] [PubMed]
- Bright, T.J.; Wong, A.; Dhurjati, R.; Bristow, E.; Bastian, L.; Coeytaux, R.R.; Samsa, G.; Hasselblad, V.; Williams, J.W.; Musty, M.D. Effect of clinical decision-support systems: A systematic review. Ann. Intern. Med. 2012, 157, 29–43. [Google Scholar] [CrossRef] [PubMed]
- Dexter, P.R.; Perkins, S.; Overhage, J.M.; Maharry, K.; Kohler, R.B.; McDonald, C.J. A computerized reminder system to increase the use of preventive care for hospitalized patients. N. Engl. J. Med. 2001, 345, 965–970. [Google Scholar] [CrossRef] [PubMed]
- Kastner, M.; Straus, S.E. Clinical decision support tools for osteoporosis disease management: A systematic review of randomized controlled trials. J. Gen. Intern. Med. 2008, 23, 2095–2105. [Google Scholar] [CrossRef]
- Groenhof, T.K.J.; Asselbergs, F.W.; Groenwold, R.H.; Grobbee, D.E.; Visseren, F.L.; Bots, M.L. The effect of computerized decision support systems on cardiovascular risk factors: A systematic review and meta-analysis. BMC Med. Inform. Decis. Mak. 2019, 19, 108. [Google Scholar] [CrossRef]
- Lapham, G.T.; Achtmeyer, C.E.; Williams, E.C.; Hawkins, E.J.; Kivlahan, D.R.; Bradley, K.A. Increased documented brief alcohol interventions with a performance measure and electronic decision support. Med. Care 2012, 50, 179–187. [Google Scholar] [CrossRef]
- Williams, E.C.; Achtmeyer, C.E.; Kivlahan, D.R.; Greenberg, D.; Merrill, J.O.; Wickizer, T.M.; Koepsell, T.D.; Heagerty, P.J.; Bradley, K.A. Evaluation of an electronic clinical reminder to facilitate brief alcohol-counseling interventions in primary care. J. Stud. Alcohol Drugs 2010, 71, 720–725. [Google Scholar] [CrossRef][Green Version]
- Minian, N.; Baliunas, D.; Noormohamed, A.; Zawertailo, L.; Giesbrecht, N.; Hendershot, C.S.; Le Foll, B.; Rehm, J.; Samokhvalov, A.V.; Selby, P.L. The effect of a clinical decision support system on prompting an intervention for risky alcohol use in a primary care smoking cessation program: A cluster randomized trial. Implement. Sci. 2019, 14, 85. [Google Scholar] [CrossRef]
- Canadian Cancer Society. The Truth About Alcohol. Available online: http://www.cancer.ca/en/about-us/news/on/2016/february/story4/?region=on (accessed on 23 December 2019).
- Pérez-Stable, E.J.; Jean-Francois, B.; Aklin, C.F. Leveraging Advances in Technology to Promote Health Equity. Med. Care 2019, 57, S101–S103. [Google Scholar] [CrossRef]
- US Department of Health and Human Services. National Healthcare Disparities Report 2011; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2012.
- Graham, G.N.; Spengler, R.F. Collaborating to end health disparities in our lifetime. Am. J. Public Health 2009, 99, 1930–1932. [Google Scholar] [CrossRef] [PubMed]
- Lee, J. The impact of health information technology on disparity of process of care. Int. J. Equity Health 2015, 14, 34. [Google Scholar] [CrossRef] [PubMed]
- Lau, B.D.; Haider, A.H.; Streiff, M.B.; Lehmann, C.U.; Kraus, P.S.; Hobson, D.B.; Kraenzlin, F.S.; Zeidan, A.M.; Pronovost, P.J.; Haut, E.R. Eliminating healthcare disparities via mandatory clinical decision support: The venous thromboembolism (VTE) example. Med. Care 2015, 53, 18. [Google Scholar] [CrossRef] [PubMed]
- Bachhuber, M.A.; O’Grady, M.A.; Chung, H.; Neighbors, C.J.; DeLuca, J.; D’Aloia, E.M.; Diaz, A.; Cunningham, C.O. Delivery of screening and brief intervention for unhealthy alcohol use in an urban academic Federally Qualified Health Center. Addict. Sci. Clin. Pract. 2017, 12, 33. [Google Scholar] [CrossRef] [PubMed]
- Bradley, K.A.; Boyd-Wickizer, J.; Powell, S.H.; Burman, M.L. Alcohol screening questionnaires in women: A critical review. JAMA 1998, 280, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Minian, N.; Baliunas, D.; Zawertailo, L.; Noormohamed, A.; Giesbrecht, N.; Hendershot, C.S.; Le Foll, B.; Rehm, J.; Samokhvalov, A.; Selby, P.L. Combining alcohol interventions with tobacco addictions treatment in primary care—The COMBAT study: A pragmatic cluster randomized trial. Implement. Sci. 2017, 12, 65. [Google Scholar] [CrossRef]
- Minian, N.; Noormohamed, A.; Zawertailo, L.; Baliunas, D.; Giesbrecht, N.; Le Foll, B.; Rehm, J.; Samokhvalov, A.; Selby, P.L. A method for co-creation of an evidence-based patient workbook to address alcohol use when quitting smoking in primary care: A case study. Res. Involv. Engagem. 2018, 4, 4. [Google Scholar] [CrossRef]
- Gomez, A.; Conde, A.; Santana, J.; Jorrin, A. Diagnostic usefulness of brief versions of Alcohol Use Disorders Identification Test (AUDIT) for detecting hazardous drinkers in primary care settings. J. Stud. Alcohol 2005, 66, 305–308. [Google Scholar] [CrossRef]
- Heatherton, T.F.; Kozlowski, L.T.; Frecker, R.C.; Rickert, W.; Robinson, J. Measuring the heaviness of smoking: Using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br. J. Addict. 1989, 84, 791–800. [Google Scholar] [CrossRef]
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef]
- StataCorp. Stata Statistical Software: Release 14; StataCorp LP: College Station, TX, USA, 2015. [Google Scholar]
- Gomel, M.K.; Wutzke, S.E.; Hardcastle, D.M.; Lapsley, H.; Reznik, R.B. Cost-effectiveness of strategies to market and train primary health care physicians in brief intervention techniques for hazardous alcohol use. Soc. Sci. Med. 1998, 47, 203–211. [Google Scholar] [CrossRef]
- Kaner, E.F.; Heather, N.; Mcavoy, B.R.; Lock, C.A.; Gilvarry, E. Intervention for excessive alcohol consumption in primary health care: Attitudes and practices of English general practitioners. Alcohol Alcohol. 1999, 34, 559–566. [Google Scholar] [CrossRef] [PubMed]
- Seale, J.P.; Shellenberger, S.; Tillery, W.K.; Boltri, J.; Barton, B.; McCauley, M.; Vogel, R. Implementing alcohol screening and intervention in a family medicine residency clinic. Subst. Abus. 2006, 26, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Weisner, C.; Schmidt, L. Gender disparities in treatment for alcohol problems. JAMA 1992, 268, 1872–1876. [Google Scholar] [CrossRef]
- Thom, B.; Téllez, C. A difficult business: Detecting and managing alcohol problems in general practice. Br. J. Addict. 1986, 81, 405–418. [Google Scholar] [CrossRef]
- Nygaard, P.; Aasland, O.G. Barriers to implementing screening and brief interventions in general practice: Findings from a qualitative study in Norway. Alcohol Alcohol. 2011, 46, 52–60. [Google Scholar] [CrossRef]
- Gomberg, E. Alcoholic women in treatment: The question of stigma and age. Alcohol Alcohol. 1988, 23, 507. [Google Scholar]
- Brawarsky, P.; Brooks, D.; Mucci, L.; Wood, P. Effect of physician recommendation and patient adherence on rates of colorectal cancer testing. Cancer Detect. Prev. 2004, 28, 260–268. [Google Scholar] [CrossRef]
- Sinclair, J.; Lawson, B.; Burge, F. Which patients receive on diet and exercise?: Do certain characteristics affect whether they receive such advice? Can. Fam. Physician 2008, 54, 404–412. [Google Scholar]
- Bulloch, A.G.; Williams, J.V.; Lavorato, D.H.; Patten, S.B. Trends in binge drinking in Canada from 1996 to 2013: A repeated cross-sectional analysis. CMAJ Open 2016, 4, E599. [Google Scholar] [CrossRef]
- Johnston, A.D. Drink: The Intimate Relationship Between Women and Alcohol; Harper Collins: New York, NY, USA, 2013. [Google Scholar]
- Stockwell, T.; Wettlaufer, A.; Vallance, K.; Chow, C.; Giesbrecht, N.; April, N.; Asbridge, M.; Callaghan, R.; Cukier, S.; Davis-MacNevin, P.; et al. Strategies to Reduce Alcohol-Related Harms and Costs in Canada: A Review of Provincial and Territorial Policies; Canadian Institute for Substance Use Research, University of Victoria: Victoria, BC, Canada, 2019. [Google Scholar]
- Brand, D.A.; Saisana, M.; Rynn, L.A.; Pennoni, F.; Lowenfels, A.B. Comparative analysis of alcohol control policies in 30 countries. PLos Med. 2007, 4, e151. [Google Scholar] [CrossRef] [PubMed]
- Madureira-Lima, J.; Galea, S. Alcohol control policies and alcohol consumption: An international comparison of 167 countries. J. Epidemiol. Community Health 2018, 72, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Patra, J.; Giesbrecht, N.; Rehm, J.; Bekmuradov, D.; Popova, S. Are alcohol prices and taxes an evidence-based approach to reducing alcohol-related harm and promoting public health and safety? A literature review. Contemp. Drug Probl. 2012, 39, 7–48. [Google Scholar] [CrossRef]
- Cook, P.J. Paying the Tab: The Costs and Benefits of Alcohol Control; Princeton University Press: Princeton, NJ, USA, 2007. [Google Scholar]
- Elder, R.W.; Lawrence, B.; Ferguson, A.; Naimi, T.S.; Brewer, R.D.; Chattopadhyay, S.K.; Toomey, T.L.; Fielding, J.E.; Services, T.F.o.C.P. The effectiveness of tax policy interventions for reducing excessive alcohol consumption and related harms. Am. J. Prev. Med. 2010, 38, 217–229. [Google Scholar] [CrossRef]
- Naimi, T.S.; Brewer, R.D.; Miller, J.W.; Okoro, C.; Mehrotra, C. What do binge drinkers drink?: Implications for alcohol control policy. Am. J. Prev. Med. 2007, 33, 188–193. [Google Scholar] [CrossRef]
- Sornpaisarn, B.; Shield, K.D.; Rehm, J. Alcohol taxation policy in Thailand: Implications for other low-to middle-income countries. Addiction 2012, 107, 1372–1384. [Google Scholar] [CrossRef]
- Anderson, P.; Chisholm, D.; Fuhr, D.C. Effectiveness and cost-effectiveness of policies and programmes to reduce the harm caused by alcohol. Lancet 2009, 373, 2234–2246. [Google Scholar] [CrossRef]
- Giesbrecht, N.; Wettlaufer, A.; April, N.; Asbridge, M.; Cukier, S.; Mann, R.; McAllister, J.; Murie, A.; Pauley, C.; Plamondon, L.; et al. Strategies to Reduce Alcohol-Related Harms and Costs in Canada: A Comparison of Provincial Policies; Centre for Addiction and Mental Health: Toronto, ON, Canada, 2013. [Google Scholar]
- Agardh, E.; Högberg, P.; Miller, T.; Norström, T.; Österberg, E.; Ramstedt, M.; Rossow, I.; Stockwell, T. Alcohol Monopoly and Public Health: Potential Effects of Privatization of the Swedish Alcohol Retail Monopoly; Statens Folkhälsoinstitut: Östersund, Sweden, 2008. [Google Scholar]
- Chikritzhs, T.; Catalano, P.; Pascal, R.; Henrickson, N. Predicting Alcohol-Related Harms from Licensed Outlet Density: A Feasibility Study; National Drug Law Enforcement Research Fund: Hobart, Austrilia, 2007. [Google Scholar]
- Vendetti, J.; Gmyrek, A.; Damon, D.; Singh, M.; McRee, B.; Del Boca, F. Screening, brief intervention and referral to treatment (SBIRT): Implementation barriers, facilitators and model migration. Addiction 2017, 112, 23–33. [Google Scholar] [CrossRef]
- Hargraves, D.; White, C.; Frederick, R.; Cinibulk, M.; Peters, M.; Young, A.; Elder, N. Implementing SBIRT (Screening, Brief Intervention and Referral to Treatment) in primary care: Lessons learned from a multi-practice evaluation portfolio. Public Health Rev. 2017, 38, 31. [Google Scholar] [CrossRef]
- Mertens, J.R.; Chi, F.W.; Weisner, C.M.; Satre, D.D.; Ross, T.B.; Allen, S.; Pating, D.; Campbell, C.I.; Lu, Y.W.; Sterling, S.A. Physician versus non-physician delivery of alcohol screening, brief intervention and referral to treatment in adult primary care: The ADVISe cluster randomized controlled implementation trial. Addict. Sci. Clin. Pract. 2015, 10, 26. [Google Scholar] [CrossRef]
- Muench, J.; Jarvis, K.; Vandersloot, D.; Hayes, M.; Nash, W.; Hardman, J.; Grover, P.; Winkle, J. Perceptions of clinical team members toward implementation of SBIRT processes. Alcohol. Treat. Q. 2015, 33, 143–160. [Google Scholar] [CrossRef]
- Greaves, L.; Poole, N. Victimized or validated? Responses to substance-using pregnant women. Can. Woman Stud. 2004, 24, 87–92. [Google Scholar]
- Jacobs, L. ‘Bad’ mothers have alcohol use disorder: Moral panic or brief intervention? Gend. Behav. 2014, 12, 5971–5979. [Google Scholar]
- Nathoo, T. Doorways to Conversation: Brief Intervention on Substance Use With Girls and Women; Centre of Excellence for Women’s Health: Vancouver, Austrilia, 2018. [Google Scholar]
- Wagner, E.; Babaei, M. Provincial Guideline for the Clinical Management of High-Risk Drinking and Alcohol Use Disorder; British Columbia Centre on Substance Use: Vancouver, BC, Canada, 2019. [Google Scholar]
- Tannenbaum, C.; Greaves, L.; Graham, I.D. Why sex and gender matter in implementation research. Bmc Med. Res. Methodol. 2016, 16, 145. [Google Scholar] [CrossRef] [PubMed]
| Variables | Control | Intervention | ||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| (n = 1547) | (n = 1246) | (n = 1597) | (n = 1312) | |
| Age in years (mean, SD) | 49.1 (13.5) | 46.9 (13.8) | 48.5 (13.6) | 46.8 (13.4) |
| Graduated high school | 1033 (67) | 977 (78) | 1071 (68) | 997 (76) |
| Household income above $40,000 | 532 (34) | 373 (30) | 495 (31) | 372 (28) |
| Currently employed | 827 (53) | 660 (53) | 829 (52) | 693 (53) |
| Daily smoking status | 1430 (92) | 1177 (94) | 1506 (94) | 1238 (94) |
| Heaviness of smoking index > 3 | 417 (29) | 229 (19) | 441 (29) | 273 (22) |
| Number of alcoholic drinks in past week (mean, SD) | 12.9 (14.3) | 7.6 (9.4) | 12.5 (14.7) | 8.2 (10.6) |
| Above AUDIT-C cut off | 1270 (82) | 1018 (82) | 1290 (81) | 1080 (82) |
| Above AUDIT-10 cut off | 67 (4) | 33 (3) | 97 (6) | 43 (3) |
| Past year attempts to quit smoking | 797 (52) | 631 (51) | 808 (51) | 685 (52) |
| Lifetime attempts to quit smoking ≥ 11 | 261 (17) | 180 (14) | 293 (18) | 185 (14) |
| Marijuana use in past 30 days | 546 (35) | 303 (24) | 599 (38) | 367 (28) |
| Opioid use in past 30 days | 244 (16) | 175 (14) | 244 (15) | 189 (14) |
| Number of comorbid conditions endorsed 1 (mean, SD) | 2.3 (2.0) | 2.4 (2.0) | 2.5 (2.1) | 2.4 (2.0) |
| CDSS as predictor of being OFFERED an appropriate alcohol resource n = 5702 | ||||||
| Original model | With sex as covariate | With interaction term | ||||
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| CDSS | 1.20 (0.88–1.64) | 0.25 | 1.20 (0.88–1.64) | 0.25 | 1.24 (0.90–1.72) | 0.19 |
| Female patient | - | - | 0.92 (0.82–1.03) | 0.13 | 0.95 (0.82–1.11) | 0.51 |
| CDSS × Sex interaction term | - | - | - | - | 0.93 (0.74–1.16) | 0.53 |
| CDSS as a predictor of ACCEPTANCE of offered alcohol resource n = 2615 | ||||||
| Original model | With sex as covariate | With interaction term | ||||
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| CDSS | 1.49 (1.01–2.18) | 0.04 | 1.48 (1.01–2.16) | 0.046 | 1.70 (1.12–2.57) | 0.01 |
| Female patient | - | - | 1.12 (0.93–1.37) | 0.24 | 1.33 (0.96–1.86) | 0.09 |
| CDSS × Sex interaction term | - | - | - | - | 0.74 (0.50–1.09) | 0.13 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Minian, N.; Ivanova, A.; Voci, S.; Veldhuizen, S.; Zawertailo, L.; Baliunas, D.; Noormohamed, A.; Giesbrecht, N.; Selby, P. Computerized Clinical Decision Support System for Prompting Brief Alcohol Interventions with Treatment Seeking Smokers: A Sex-Based Secondary Analysis of a Cluster Randomized Trial. Int. J. Environ. Res. Public Health 2020, 17, 1024. https://doi.org/10.3390/ijerph17031024
Minian N, Ivanova A, Voci S, Veldhuizen S, Zawertailo L, Baliunas D, Noormohamed A, Giesbrecht N, Selby P. Computerized Clinical Decision Support System for Prompting Brief Alcohol Interventions with Treatment Seeking Smokers: A Sex-Based Secondary Analysis of a Cluster Randomized Trial. International Journal of Environmental Research and Public Health. 2020; 17(3):1024. https://doi.org/10.3390/ijerph17031024
Chicago/Turabian StyleMinian, Nadia, Anna Ivanova, Sabrina Voci, Scott Veldhuizen, Laurie Zawertailo, Dolly Baliunas, Aliya Noormohamed, Norman Giesbrecht, and Peter Selby. 2020. "Computerized Clinical Decision Support System for Prompting Brief Alcohol Interventions with Treatment Seeking Smokers: A Sex-Based Secondary Analysis of a Cluster Randomized Trial" International Journal of Environmental Research and Public Health 17, no. 3: 1024. https://doi.org/10.3390/ijerph17031024
APA StyleMinian, N., Ivanova, A., Voci, S., Veldhuizen, S., Zawertailo, L., Baliunas, D., Noormohamed, A., Giesbrecht, N., & Selby, P. (2020). Computerized Clinical Decision Support System for Prompting Brief Alcohol Interventions with Treatment Seeking Smokers: A Sex-Based Secondary Analysis of a Cluster Randomized Trial. International Journal of Environmental Research and Public Health, 17(3), 1024. https://doi.org/10.3390/ijerph17031024




