Prevalence and Determinants of Bad Sleep Perception among Italian Children and Adolescents
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Procedure
2.2. Instruments
- (a)
- Sleep habits, composed of six open questions assessing habitual bedtime, rise time, and sleep duration, in hours and minutes, on both schooldays and weekends;
- (b)
- Sleep features, including one question on habitual sleep latency, consisting of a single forced-choice item with six response categories (“0 to 5 min”, “6 to 15 min”, “16 to 30 min”, “31 to 45 min”, “46 to 60 min”, and “more than one hour”); a forced question examining whether sleep duration is considered sufficient (“How often do you think you sleep enough?”), with five choices (“always”, “often”, “sometimes”, “seldom”, and “never”); a forced question investigating the frequency of nocturnal awakenings (“Never”, “Once”, “2 or 3 times”, “More than 3 times”, and “I have no idea”); a forced question evaluating daytime napping (“Some people take naps in the daytime every day, others never do. When do you nap?”), with four choices (“I never nap”; “I sometimes nap on school days”; “I sometimes nap on weekends”; “I never nap unless I am sick”);
- (c)
- Daytime behavior and sleep disturbances (DBSD), which includes three scales: a sleepiness scale (SLS), a depressed mood scale (DMS) and a sleep–wake problems behavior scale (SWP). The SLS is composed of nine items assessing the ease of staying awake in different situations (“talking vis a vis with someone else”, “travelling on public transports”, “watching a show”, “watching television or listening to music”, “reading or studying”, “during a school test”, “sitting in class”, “working at the computer”, and “playing a videogame”): respondents had to choose among four ordinal alternatives, ranging from “no difficulty staying awake” to “struggling to stay awake but falling asleep”. A global vigilance score, ranging from 9 to 36, was then obtained by summing up scores at all of the nine items, with higher scores reflecting higher sleepiness levels. The DMS consists of 5 multiple choice items assessing the presence of depressed mood over the last two weeks. Participants have to choose among three alternatives (“not at all”; “somewhat”; “much”). A global index of depressed mood, ranging from 10 to 30, is obtained by averaging scores and multiplying them by ten, with higher scores indicating more depressed mood. Finally, the SWP is made up of 10 items, assessing how often the subjects have experienced some sleep/wake-related perceptions and problems over the last two weeks (“being late at school for having slept too long”, “falling asleep in a morning class”, “falling asleep in an evening class”, “going to bed late in the evening”, “staying awake all night long”, “sleeping until noon”, “having difficulties waking up in the morning”, “having problems falling asleep at bedtime”, “having nightmares”, and “going to bed too early because of excessive sleepiness”). The answers are graded on a five-point scale, ranging from “never” to “always”. The total score, ranging from 10 to 50, is computed by summing the answers to all items, with higher scores reflecting more sleep-related problems;
- (d)
- Circadian preference, assessed by means of a Morningness–Eveningness Questionnaire (MEQ), composed of ten items. The global score, ranging from 43 (extreme morningness) to 10 (extreme eveningness), allows to identify subjects as morning types (M-types), intermediate types (I-types), and evening types (E-types);
- (e)
- Sleep quality: an item about sleep quality perception (“Do you consider yourself as a good or a bad sleeper?”) was added to the original Italian version of the questionnaire [16]. Subjects had to choose among two response alternatives (“a good sleeper”, “a bad sleeper”);
- (f)
- Dreaming: two questions about dreams were also added to the original questionnaire [16]: one regarding dream recall frequency (“How often you remember having dreamed?”), with four ordinal alternatives ranging from “always” to “never”, and one regarding dream pleasantness (“How are your dreams usually?”), with five forced-choice alternatives ranging from “wonderful and exciting” to “horrible and frightening”.
2.3. Procedure
2.4. Data Analysis
- sleep habits, that is, sleep duration in minutes, bedtime and rise time—all variables reported for schooldays and weekends—plus the differences (Δ) between schooldays (SD) and weekends (WE) in bedtime (reported as “Δ-SD/WE bedtime”), rise time (indicated as “Δ-SD/WE rise time”), and sleep duration (reported as “Δ-SD/WE sleep duration”);
- habitual sleep latency;
- sufficiency of sleep;
- night awakenings frequency;
- daytime napping frequency;
- sleepiness global score, obtained from the sleepiness scale;
- depressive mood index, calculated from the depressed mood scale;
- sleep–wake behavioral problems global score, obtained from sleep–wake problems behavior scale;
- circadian preference, assessed through the morningness–eveningness questionnaire;
- dream frequency and dream pleasantness.
3. Results
3.1. Response Rate
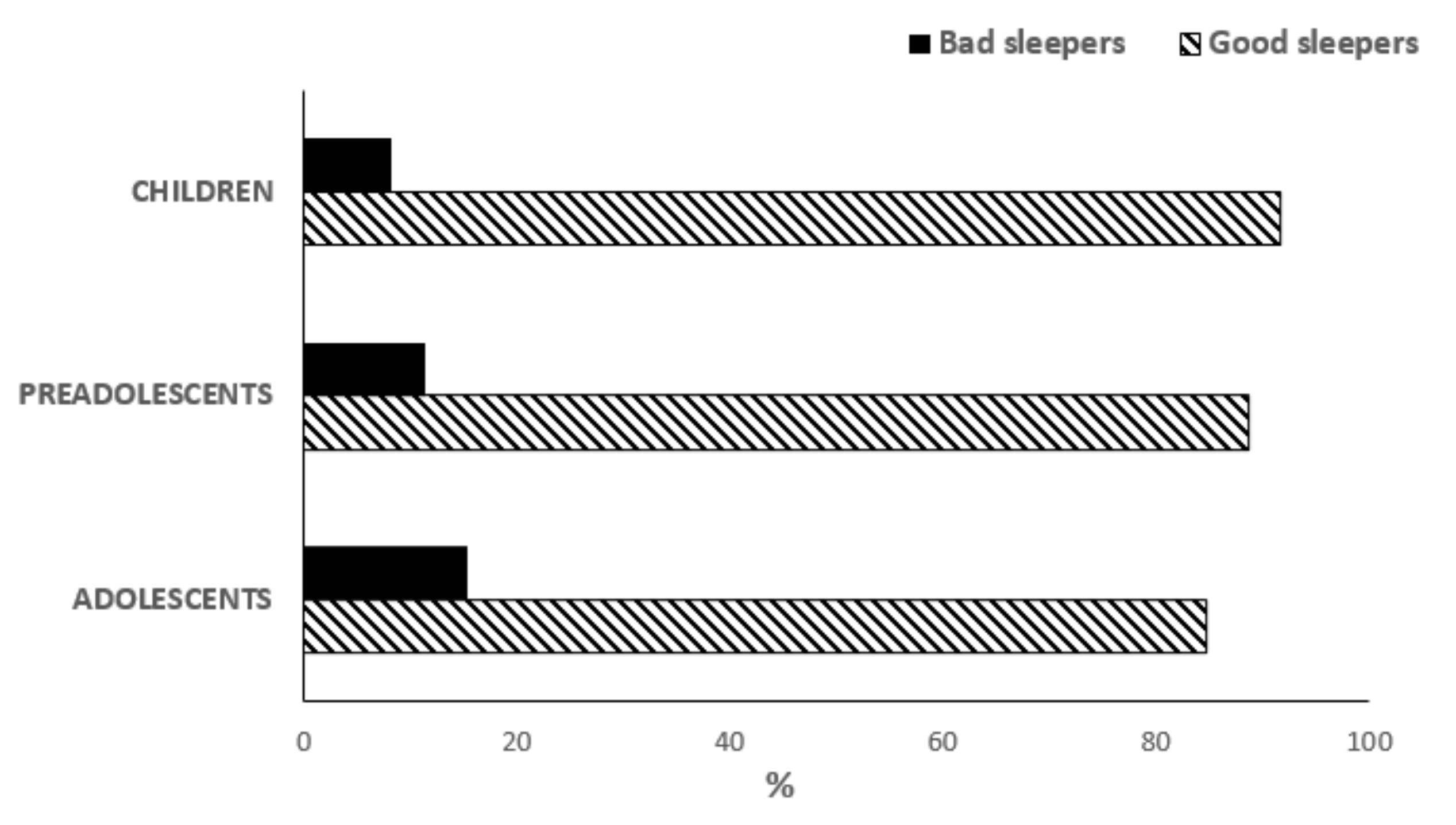
3.2. Overall Sleep Quality
3.3. Sleep Habits
3.4. Sleep Features
3.5. Daytime Behaviour and Sleep Disturbances
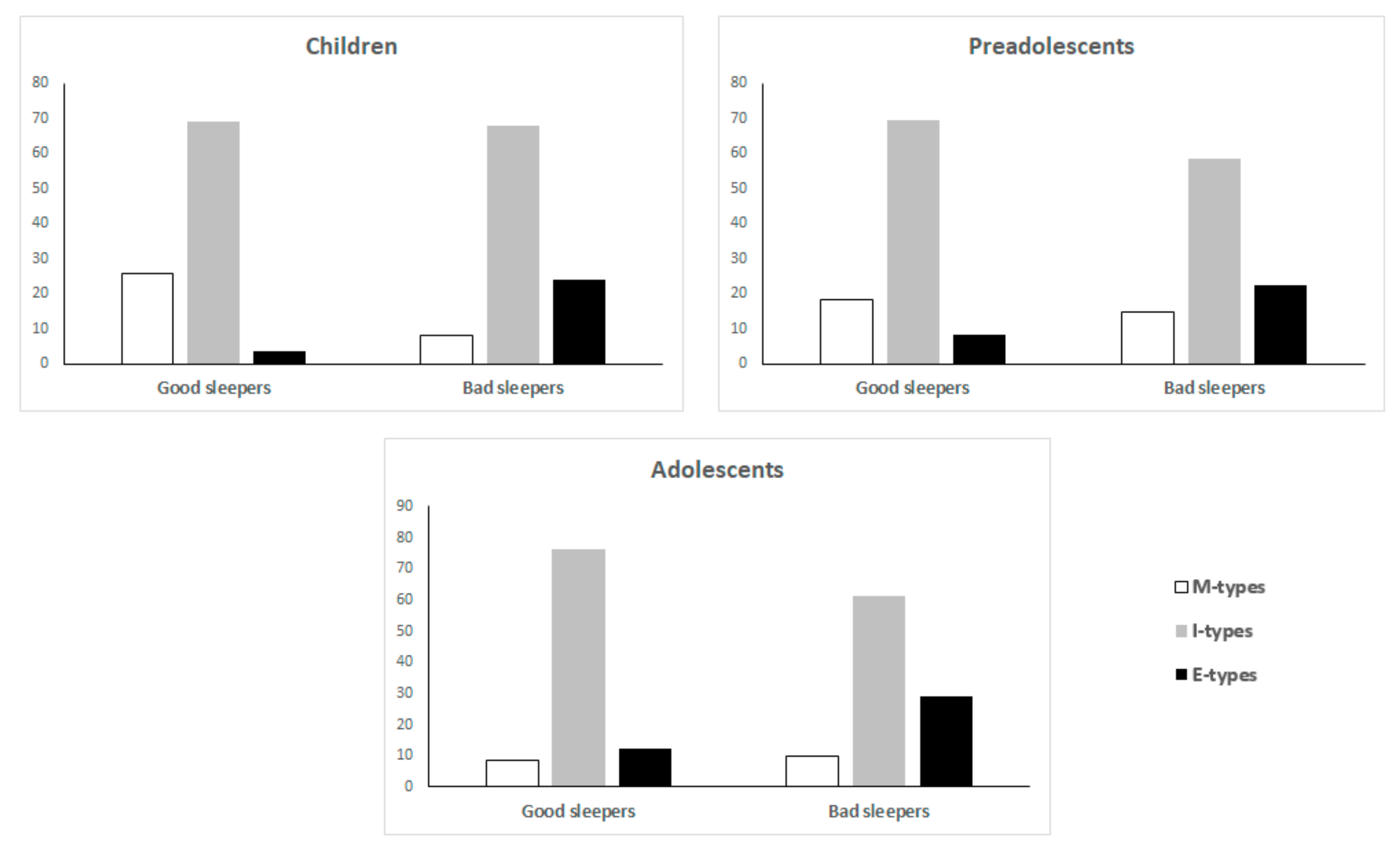
3.6. Circadian Preference
3.7. Dreaming
3.8. Subjective Sleep Quality Determinants
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ohayon, M.M.; Carskadon, M.A.; Guilleminault, C.; Vitiello, M.V. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: Developing normative sleep values across the human lifespan. Sleep 2004, 27, 1255–1273. [Google Scholar] [CrossRef] [PubMed]
- Jenni, O.; Carskadon, M. Sleep Behavior and Sleep Regulation from Infancy through Adolescence. Sleep Med. Clin. 2007, 2, 321–329. [Google Scholar] [CrossRef]
- Iglowstein, I.; Jenni, O.G.; Molinari, L.; Largo, R.H. Sleep duration from infancy to adolescence: Reference values and generational trends. Pediatrics 2003, 111, 302–307. [Google Scholar] [CrossRef] [PubMed]
- Garbarino, S. Sleep Disorders across the Lifespan: A Different Perspective. Int. J. Environ. Res. Public Health 2020, 17, 9025. [Google Scholar] [CrossRef] [PubMed]
- Fricke-Oerkermann, L.; Plück, J.; Schredl, M.; Heinz, K.; Mitschke, A.; Wiater, A.; Lehmkuhl, G. Prevalence and course of sleep problems in childhood. Sleep 2007, 30, 1371–1377. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Ren, J.; Shi, L.; Jin, X.; Yan, C.; Jiang, F.; Shen, X.; Li, S. Frequent nocturnal awakening in children: Prevalence, risk factors, and associations with subjective sleep perception and daytime sleepiness. BMC Psychiatry 2014, 14, 204. [Google Scholar] [CrossRef]
- Wiater, A.H.; Mitschke, A.R.; Widdern, S.V.; Fricke, L.; Breuer, U.; Lehmkuhl, G. Sleep disorders and behavioural problems among 8- to 11-year-old children. Somnologie 2005, 9, 210–214. [Google Scholar] [CrossRef]
- Shreeram, S.; He, J.P.; Kalaydjian, A.; Brothers, S.; Merikangas, K.R. Prevalence of enuresis and its association with attention-deficit/hyperactivity disorder among U.S. children: Results from a nationally representative study. J. Am. Acad. Child Adolesc. Psychiatry 2009, 48, 35–41. [Google Scholar] [CrossRef]
- Ma, Y.; Shen, Y.; Liu, X. Association between enuresis and obesity in children with primary monosymptomatic nocturnal enuresis. Int. Braz. J. Urol. 2019, 45, 790–797. [Google Scholar] [CrossRef]
- Mindell, J.A.; Meltzer, L.J.; Carskadon, M.A.; Chervin, R.D. Developmental aspects of sleep hygiene: Findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep Med. 2009, 10, 771–779. [Google Scholar] [CrossRef]
- Mindell, J.A.; Meltzer, L.J. Behavioural sleep disorders in children and adolescents. Ann. Acad. Med. Singap. 2008, 37, 722–728. [Google Scholar] [PubMed]
- Chaput, J.P.; Janssen, I. Sleep duration estimates of Canadian children and adolescents. J. Sleep Res. 2016, 25, 541–548. [Google Scholar] [CrossRef] [PubMed]
- Dewald, J.F.; Meijer, A.M.; Oort, F.J.; Kerkhof, G.A.; Bögels, S.M. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: A meta-analytic review. Sleep Med. Rev. 2010, 14, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Meijer, A.M.; Habekothé, H.T.; van den Wittenboer, G.L. Time in bed, quality of sleep and school functioning of children. J. Sleep Res. 2000, 9, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Giannotti, F.; Cortesi, F.; Sebastiani, T.; Ottaviano, S. Circadian preference, sleep and daytime behaviour in adolescence. J. Sleep Res. 2002, 11, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Russo, P.M.; Bruni, O.; Lucidi, F.; Ferri, R.; Violani, C. Sleep habits and circadian preference in Italian children and adolescents. J. Sleep Res. 2007, 16, 163–169. [Google Scholar] [CrossRef]
- Giannotti, F.; Cortesi, F. Sleep patterns and daytime function in adolescence: An epidemiological survey of an Italian high school student sample. In Adolescent Sleep Patterns: Biological, Social and Psychological Influences; Carskadon, M.A., Ed.; Cambridge University Press: Cambridge, UK, 2002; pp. 132–147. [Google Scholar]
- Giannotti, F.; Cortesi, F.; Sebastiani, T.; Vagnoni, C. Sleeping habits in Italian children and adolescents. Sleep Biol. Rhythm. 2005, 3, 15–21. [Google Scholar] [CrossRef]
- Bruni, O.; Sette, S.; Angriman, M.; Baumgartner, E.; Selvaggini, L.; Belli, C.; Ferri, R. Clinically Oriented Subtyping of Chronic Insomnia of Childhood. J. Pediatr. 2018, 196, 194–200. [Google Scholar] [CrossRef]
- Castronovo, V.; Zucconi, M.; Nosetti, L.; Marazzini, C.; Hensley, M.; Veglia, F.; Nespoli, L.; Ferini-Strambi, L. Prevalence of habitual snoring and sleep-disordered breathing in preschool-aged children in an Italian community. J. Pediatr. 2003, 142, 377–382. [Google Scholar] [CrossRef]
- Brunetti, L.; Rana, S.; Lospalluti, M.L.; Pietrafesa, A.; Francavilla, R.; Fanelli, M.; Armenio, L. Prevalence of obstructive sleep apnea syndrome in a cohort of 1,207 children of southern Italy. Chest 2001, 120, 1930–1935. [Google Scholar] [CrossRef]
- Manni, R.; Ratti, M.T.; Marchioni, E.; Castelnovo, G.; Murelli, R.; Sartori, I.; Galimberti, C.A.; Tartara, A. Poor sleep in adolescents: A study of 869 17-year-old Italian secondary school students. J. Sleep Res. 1997, 6, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Chen, N.; Fong, D.Y.T.; Li, S.; Wong, J.Y.H. Association between Non-Restorative Sleep and Quality of Life in Chinese Adolescents. Int. J. Environ. Res. Public Health 2020, 17, 7249. [Google Scholar] [CrossRef] [PubMed]
- Jean-Louis, G.; Kripke, D.F.; Ancoli-Israel, S. Sleep and quality of well-being. Sleep 2000, 23, 1115–1121. [Google Scholar] [CrossRef] [PubMed]
- Lemola, S.; Ledermann, T.; Friedman, E.M. Variability of sleep duration is related to subjective sleep quality and subjective well-being: An actigraphy study. PLoS ONE 2013, 8, e71292. [Google Scholar] [CrossRef]
- Taylor, D.J.; Lichstein, K.L.; Durrence, H.H. Insomnia as a Health Risk Factor. Behav. Sleep Med. 2003, 1, 227–247. [Google Scholar] [CrossRef]
- Buysse, D.J. Sleep health: Can we define it? Does it matter? Sleep 2014, 37, 9–17. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Publishing: Arlinghton, VA, USA; Washington, DC, USA, 2013. [Google Scholar]
- Martínez, M.P.; Miró, E.; Sánchez, A.I.; Díaz-Piedra, C.; Cáliz, R.; Vlaeyen, J.W.; Buela-Casal, G. Cognitive-behavioral therapy for insomnia and sleep hygiene in fibromyalgia: A randomized controlled trial. J. Behav. Med. 2014, 37, 683–697. [Google Scholar] [CrossRef]
- Wells, G.; Li, T.; Maxwell, L.; Maclean, R.; Tugwell, P. Responsiveness of patient reported outcomes including fatigue, sleep quality, activity limitation and quality of life following treatment with abatacept for rheumatoid arthritis. Ann. Rheum. Dis. 2008, 67, 260–265. [Google Scholar] [CrossRef]
- Short, M.A.; Gradisar, M.; Gill, J.; Camfferman, D. Identifying Adolescent Sleep Problems. PLoS ONE 2013, 8, e75301. [Google Scholar] [CrossRef]
- Åkerstedt, T.; Hume, K.; Minors, D.; Waterhouse, J. Good sleep—Its timing and physiological sleep characteristics. J. Sleep Res. 1997, 6, 221–229. [Google Scholar] [CrossRef]
- Kecklund, G.; Åkerstedt, T. Objective components of individual differences in subjective sleep quality. J. Sleep Res. 1997, 6, 217–220. [Google Scholar] [CrossRef] [PubMed]
- Argyropoulos, S.V.; Hicks, J.A.; Nash, J.R.; Bell, C.J.; Rich, A.S.; Nutt, D.J.; Wilson, S.J. Correlation of subjective and objective sleep measurements at different stages of the treatment of depression. Psychiatry Res. 2003, 120, 179–190. [Google Scholar] [CrossRef]
- O’Donnell, D.; Silva, E.J.; Münch, M.M.; Wang, W.; Duffy, J.F. Comparison of subjective and objective assessments of sleep in healthy older subjects without sleep complaints. J. Sleep Res. 2009, 18, 254–263. [Google Scholar] [CrossRef] [PubMed]
- Riedel, B.W.; Lichstein, K.L. Objective sleep measures and subjective sleep satisfaction: How do older adults with insomnia define a good night’s sleep? Psychol. Aging 1998, 13, 159–163. [Google Scholar] [CrossRef]
- Rosipal, R.; Lewandowski, A.; Dorffner, G. In search of objective components for sleep quality indexing in normal sleep. Biol. Psychol. 2013, 94, 210–220. [Google Scholar] [CrossRef]
- Westerlund, A.; Lagerros, Y.T.; Kecklund, G.; Axelsson, J.; Åkerstedt, T. Relationships between questionnaire ratings of sleep quality and polysomnography in healthy adults. Behav. Sleep Med. 2016, 14, 185–199. [Google Scholar] [CrossRef]
- Kryger, M.H.; Steljes, D.; Pouliot, Z.; Neufeld, H.; Odynski, T. Subjective versus objective evaluation of hypnotic efficacy: Experience with zolpidem. Sleep 1991, 14, 399–407. [Google Scholar] [CrossRef]
- Landis, C.A.; Frey, C.A.; Lentz, M.J.; Rothermel, J.; Buchwald, D.; Shaver, J.L. Self-reported sleep quality and fatigue correlates with actigraphy in midlife women with fibromyalgia. Nurs. Res. 2003, 52, 140–147. [Google Scholar] [CrossRef]
- Hoch, C.C.; Reynolds, C.F.; Kupfer, D.J.; Berman, S.R.; Houck, P.R.; Stack, J.A. Empirical note: Self-report vs. recorded sleep in healthy seniors. Psychophysiology 1987, 24, 293–299. [Google Scholar] [CrossRef]
- Åkerstedt, T.; Hume, K.; Minors, D.; Waterhouse, J. The subjective meaning of good sleep, an intraindividual approach using the Karolinska Sleep Diary. Percept. Mot. Skills 1994, 79, 287–296. [Google Scholar] [CrossRef]
- Baekcland, F.; Hoy, P. Reported vs. recorded sleep characteristics. Arch. Gen. Psychiatry 1971, 24, 548–551. [Google Scholar] [CrossRef]
- Della Monica, C.; Johnsen, S.; Atzori, G.; Groeger, J.A.; Dijk, D.J. Rapid Eye Movement Sleep, Sleep Continuity and Slow Wave Sleep as Predictors of Cognition, Mood, and Subjective Sleep Quality in Healthy Men and Women, Aged 20–84 Years. Front. Psychiatry 2018, 9, 255. [Google Scholar] [CrossRef]
- Conte, F.; Cerasuolo, M.; Fusco, G.; Giganti, F.; Inserra, I.; Malloggi, S.; di Iorio, I.; Ficca, G. Sleep continuity, stability and organization in good and bad sleepers. J. Health Psychol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Goelema, M.S.; Regis, M.; Haakma, R.; van den Heuvel, E.R.; Markopoulos, P.; Overeem, S. Determinants of perceived sleep quality in normal sleepers. Behav. Sleep Med. 2019, 4, 388–397. [Google Scholar] [CrossRef] [PubMed]
- Åkerstedt, T.; Orsini, N.; Petersen, H.; Axelsson, J.; Lekander, M.; Kecklund, G. Predicting sleep quality from stress and prior sleep—A study of day-to-day covariation across six weeks. Sleep Med. 2012, 13, 674–679. [Google Scholar] [CrossRef] [PubMed]
- Belmon, L.S.; Busch, V.; van Stralen, M.M.; Stijnman, D.P.M.; Hidding, L.M.; Harmsen, I.A.; Chinapaw, M.J.M. Child and Parents Perceived Determinants of Children’s Inadequate Sleep Health. A concept mapping Study. Int. J. Environ. Res. Public Health 2020, 17, 1583. [Google Scholar] [CrossRef] [PubMed]
- Zilli, I.; Ficca, G.; Salzarulo, P. Factors involved in sleep satisfaction in the elderly. Sleep Med. 2009, 10, 233–239. [Google Scholar] [CrossRef]
- Wolfson, A.R.; Carskadon, M.A.; Acebo, C.; Seifer, R.; Fallone, G.; Labyak, S.E.; Martin, J.L. Evidence for the validity of a sleep habits survey for adolescents. Sleep 2003, 26, 213–216. [Google Scholar] [CrossRef]
- Carskadon, M.A.; Feifer, R.; Acebo, C. Reliability of six scales in a sleep questionnaire for adolescents. Sleep Res. 1991, 20, 421. [Google Scholar]
- Meltzer, L.J.; Mindell, J.A. Sleep and sleep disorders in children and adolescents. Psychiatr. Clin. N. Am. 2006, 29, 1059. [Google Scholar] [CrossRef]
- Drollette, E.S.; Shishido, T.; Pontifex, M.B.; Hillman, C.H. Maintenance of cognitive control during and after walking in preadolescent children. MSSE 2012, 44, 2017–2024. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the false discovery rate: A practical and powerful approach to multiple testing. J. R. Stat. Soc. 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Lehmann, E.L. Nonparametrics: Statistical Methods Based on Ranks, 2nd ed.; Springer: New York, NY, USA, 1988. [Google Scholar]
- Cohen, J. Statistical Power Analysis, 2nd ed.; Erlbaum: Hillsdale, NJ, USA, 1988. [Google Scholar]
- BaHammam, A.; AlFaris, E.; Shaikh, S.; Bin Saeed, A. Prevalence of sleep problems and habits in a sample of Saudi primary school children. Ann. Saudi Med. 2006, 26, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Gradisar, M.; Gardner, G.; Dohnt, H. Recent worldwide sleep patterns and problems during adolescence: A review and meta-analysis of age, region, and sleep. Sleep Med. 2011, 12, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Hvolby, A.; Jørgensen, J.; Bilenberg, N. Sleep and sleep difficulties in Danish children aged 6–11 years. Ugeskr. Laeger 2008, 170, 448–451. [Google Scholar]
- Sadeh, A.; Dark, I.; Vohr, B.R. Newborns’ sleep-wake patterns: The role of maternal, delivery and infant factors. Early Hum. Dev. 1996, 44, 113–126. [Google Scholar] [CrossRef]
- Sadeh, A. Evaluating night wakings in sleep-disturbed infants: A methodological study of parental reports and actigraphy. Sleep 1996, 19, 757–762. [Google Scholar] [CrossRef]
- National Sleep Foundation. The NSF 2006 Sleep in America Poll; National Sleep Foundation: Washington, DC, USA, 2006. [Google Scholar]
- Simola, P.; Niskakangas, M.; Liukkonen, K.; Virkkula, P.; Pitkäranta, A.; Kirjavainen, T.; Aronen, E.T. Sleep problems and daytime tiredness in Finnish preschool-aged children-a community survey. Child Care Health Dev. 2010, 36, 805–811. [Google Scholar] [CrossRef]
- Gaina, A.; Sekine, M.; Hamanishi, S.; Chen, X.; Kagamimori, S. Gender and temporal differences in sleep-wake patterns in Japanese schoolchildren. Sleep 2005, 28, 337–342. [Google Scholar]
- Galland, B.C.; Gray, A.R.; Penno, J.; Smith, C.; Lobb, C.; Taylor, R.W. Gender differences in sleep hygiene practices and sleep quality in New Zealand adolescents aged 15 to 17 years. Sleep Health 2017, 3, 77–83. [Google Scholar] [CrossRef]
- Zhang, N.; Wing, Y.K. Sex differences in insomnia: A meta-analysis. Sleep 2006, 29, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Mallampalli, M.P.; Carter, C.L. Exploring sex and gender differences in sleep health: A Society for Women’s Health Research Report. J. Women’s Health 2014, 23, 553–562. [Google Scholar] [CrossRef] [PubMed]
- Madrid-Valero, J.J.; Martínez-Selva, J.M.; Ribeiro do Couto, B.; Sánchez-Romera, J.F.; Ordoñana, J.R. Age and gender effects on the prevalence of poor sleep quality in the adult population. Gac. Sanit. 2017, 31, 18–22. [Google Scholar] [CrossRef] [PubMed]
- Wolfson, A.R.; Carskadon, M.A. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998, 69, 875–887. [Google Scholar] [CrossRef]
- Anderson, B.; Storfer-Isser, A.; Taylor, H.G.; Rosen, C.L.; Redline, S. Associations of executive function with sleepiness and sleep duration in adolescents. Pediatrics 2009, 123, e701–e707. [Google Scholar] [CrossRef]
- Fallone, G.; Owens, J.A.; Deane, J. Sleepiness in children and adolescents: Clinical implications. Sleep Med. Rev. 2002, 6, 287–306. [Google Scholar] [CrossRef]
- Drake, C.; Nickel, C.; Burduvali, E.; Thomas Roth, B.A.; Jefferson, C.; Badia, P. The Pediatric Daytime Sleepiness Scale (PDSS): Sleep Habits and School Outcomes in Middle-school Children. Sleep 2003, 26, 455–458. [Google Scholar]
- Colrain, I.M.; Baker, F.C. Changes in sleep as a function of adolescent development. Neuropsychol. Rev. 2011, 21, 5–21. [Google Scholar] [CrossRef]
- Lovato, N.; Gradisar, M. A meta-analysis and model of the relationship between sleep and depression in adolescents: Recommendations for future research and clinical practice. Sleep Med. Rev. 2014, 18, 521–529. [Google Scholar] [CrossRef]
- Chiu, H.Y.; Lee, H.C.; Chen, P.Y.; Lai, Y.F.; Tu, Y.K. Associations between sleep duration and suicidality in adolescents: A systematic review and dose-response meta-analysis. Sleep Med. Rev. 2018, 42, 119–126. [Google Scholar] [CrossRef]
- Becker, S.P.; Sidol, C.A.; van Dyk, T.R.; Epstein, J.N.; Beebe, D.W. Intraindividual variability of sleep/wake patterns in relation to child and adolescent functioning: A systematic review. Sleep Med. Rev. 2017, 34, 94–121. [Google Scholar] [CrossRef] [PubMed]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social jetlag: Misalignment of biological and social time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef] [PubMed]
- Simor, P.; Pajkossy, P.; Horváth, K.; Bódizs, R. Impaired executive functions in subjects with frequent nightmares as reflected by performance in different neuropsychological tasks. Brain Cogn. 2012, 78, 274–283. [Google Scholar] [CrossRef] [PubMed]
- Smedje, H.; Broman, J.E.; Hetta, J. Short-term prospective study of sleep disturbances in 5–8-year-old children. Acta Pædiatrica 2001, 90, 1456–1463. [Google Scholar] [CrossRef] [PubMed]
- Gray, K.; Eagleston, J.R.; Gibson, E.; Thoresen, C.E. Sleep disturbance in adolescents: Sleep quality, sleep habits, beliefs about sleep, and daytime functioning. J. Youth Adolesc. 1984, 13, 375–384. [Google Scholar] [CrossRef] [PubMed]
- Harvey, A.G.; Stinson, K.; Whitaker, K.L.; Moscovitz, D.; Virk, H. The subjective meaning of sleep quality: A comparison of individuals with and without insomnia. Sleep 2008, 31, 383–393. [Google Scholar] [CrossRef] [PubMed]
- Libman, E.; Fichten, C.; Creti, L.; Conrod, K.; Tran, D.L.; Grad, R.; Jorgensen, M.; Amsel, R.; Rizzo, D.; Baltzan, M.; et al. Refreshing sleep and sleep continuity determine perceived sleep quality. Sleep Disord. 2016, 2016, 7170610. [Google Scholar] [CrossRef]
- Goelema, M.S.; de Bruijn, R.; Overeem, S.; Møst, E.; Hakma, R.; Markopoulos, P. Conceptions of sleep experience: A layman perspective. BMC Res. Notes 2018, 11, 494. [Google Scholar] [CrossRef]
- Jenni, O.G.; Carskadon, M.A. Sleep Behavior and Sleep Regulation from Infancy Through Adolescence: Normative Aspects. Sleep Med. Clin. 2012, 7, 529–538. [Google Scholar] [CrossRef]
- Fontanellaz-Castiglione, C.E.G.; Markovic, A.; Tarokh, L. Sleep and the adolescent brain. Curr. Opin. Physiol. 2020, 15, 167–171. [Google Scholar] [CrossRef]
- Garrison, W.; Felice, M.E. Adolescence. In Developmental-Behavioral Pediatrics, 4th ed.; Carey, W., Crocker, A., Elias, E., Coleman, W., Feldman, H., Eds.; WB Saunders: Philadelphia, PA, USA, 2009; pp. 62–73. [Google Scholar]
- Senín-Calderón, C.; Rodríguez-Testal, J.F.; Perona-Garcelán, S.; Perpiñá, C. Body image and adolescence: A behavioral impairment model. Psychiatry Res. 2017, 248, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Littleton, H.L.; Ollendick, T. Negative body image and disordered eating behavior in children and adolescents: What places youth at risk and how can these problems be prevented? Clin. Child Fam. Psychol. Rev. 2003, 6, 51–66. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, S.H.; Petrie, T.A.; Greenleaf, C.A.; Martin, S.B. Moderators of the internalization–body dissatisfaction relationship in middle school girls. Body Image 2012, 9, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Semler, C.N.; Harvey, A.G. Misperception of sleep can adversely affect daytime functioning in insomnia. Behav. Res. Ther. 2005, 43, 843–856. [Google Scholar] [CrossRef]
- Cain, N.; Gradisar, M. Electronic media use and sleep in school-aged children and adolescents: A review. Sleep Med. 2010, 11, 735–742. [Google Scholar] [CrossRef]
- Hale, L.; Guan, S. Screen time and sleep among school-aged children and adolescents: A systematic literature review. Sleep Med. Rev. 2015, 21, 50–58. [Google Scholar] [CrossRef]
| N | M | F | 6–8 | 9–11 | 12–14 | |
|---|---|---|---|---|---|---|
| Como | 736 | 377 | 359 | 153 | 362 | 221 |
| Sansepolcro | 534 | 268 | 266 | 130 | 218 | 185 |
| Cospaia | 47 | 33 | 14 | 12 | 35 | 0 |
| Lama | 6 | 1 | 5 | 2 | 4 | 0 |
| Selci | 34 | 18 | 16 | 1 | 33 | 0 |
| Sangiustino | 73 | 34 | 39 | 9 | 65 | 0 |
| Total sample | 1430 | 731 | 699 | 307 | 717 | 406 |
| Sleep Habits | Good Sleepers | Bad Sleepers | U | p |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| Children | ||||
| Bedtime schooldays | 21:24 ± 00:38 | 21:29 ± 00:33 | 3017 | 0.298 |
| Bedtime weekend | 22:30 ± 00:48 | 22:35 ± 00:55 | 3040 | 0.387 |
| Rise time schooldays | 07:04 ± 00:25 | 07:05 ± 00:27 | 3411 | 0.972 |
| Rise time weekend | 09:14 ± 01:13 | 09:00 ± 01:34 | 2980 | 0.303 |
| Sleep duration schooldays | 09:25 ± 00:53 | 09:01 ± 01:01 | 2645 | 0.046 |
| Sleep duration weekend | 10:32 ± 01:13 | 09:52 ± 01:19 | 2642 | 0.053 |
| Δ-SD/WE Bedtime | 01:09 ± 00:43 | 01:10 ± 00:38 | 3263 | 0.756 |
| Δ-SD/WE Rise time | 02:11 ± 00:14 | 01:54 ± 01:30 | 2971 | 0.308 |
| Δ-SD/WE Sleep duration | 01:23 ± 01:05 | 01:17 ± 00:57 | 3405 | 0.938 |
| Preadolescents | ||||
| Bedtime schooldays | 21:45 ± 00:42 | 21:49 ± 00:49 | 24784 | 0.917 |
| Bedtime weekend | 22:55 ± 01:14 | 22:59 ± 00:56 | 24029 | 0.766 |
| Rise time schooldays | 07:06 ± 00:22 | 07:03 ± 00:28 | 22852 | 0.205 |
| Rise time weekend | 09:22 ± 01:15 | 09:05 ± 01:10 | 21853 | 0.112 |
| Sleep duration schooldays | 09:15 ± 01:01 | 09:04 ± 01:09 | 22469 | 0.206 |
| Sleep duration weekend | 10:17 ± 01:19 | 09:51 ± 01:32 | 20961 | 0.047 |
| Δ-SD/WE Bedtime | 01:17 ± 01:10 | 01:15 ± 00:47 | 24305 | 0.912 |
| Δ-SD/WE Rise time | 02:15 ± 01:16 | 02:02 ± 01:10 | 22330 | 0.193 |
| Δ-SD/WE Sleep duration | 01:23 ± 01:40 | 01:24 ± 01:30 | 23984 | 0.852 |
| Adolescents | ||||
| Bedtime schooldays | 22:19 ± 00:59 | 22:25 ± 00:38 | 10051 | 0.487 |
| Bedtime weekend | 23:38 ± 00:53 | 23:51 ± 00:50 | 8869 | 0.060 |
| Rise time schooldays | 07:01 ± 00:19 | 06:57 ± 00:27 | 9758 | 0.285 |
| Rise time weekend | 09:43 ± 01:15 | 09:45 ± 01:33 | 10496 | 0.958 |
| Sleep duration schooldays | 08:30 ± 00:58 | 08:12 ± 00:56 | 8712 | 0.023 |
| Sleep duration weekend | 09:55 ± 01:21 | 09:52 ± 01:31 | 10328 | 0.772 |
| Δ-SD/WE Bedtime | 01:22 ± 01:27 | 01:26 ± 00:48 | 9290 | 0.158 |
| Δ-SD/WE Rise time | 02:41 ±01:15 | 02:47 ± 01:34 | 10424 | 0.890 |
| Δ-SD/WE Sleep duration | 01:37 ± 01:07 | 01:51 ± 01:10 | 9400 | 0.164 |
| Sleep Features | Good Sleepers | Bad Sleepers | U | p |
|---|---|---|---|---|
| Children | ||||
| Habitual sleep latency | 2 (2.1 ± 1.3) | 2 (2.8 ± 1.7) | 2612 | 0.042 |
| Sufficiency of sleep | 2 (2.1 ± 1.2) | 3 (2.7 ± 1.3) | 2497 | 0.016 |
| Nocturnal awakening frequency | 2 (1.9 ± 1.2) | 2 (2.6 ± 1.3) | 2354 | 0.004 |
| Nap frequency | 1 (1.9 ± 1.2) | 2 (2.1 ± 1.2) | 3060 | 0.308 |
| Preadolescents | ||||
| Habitual sleep latency | 2 (2.5 ± 1.4) | 3 (3.3 ± 1.7) | 16892 | <0.001 |
| Sufficiency of sleep | 2 (2.2 ± 1.0) | 3 (2.8 ± 1.1) | 15960 | <0.001 |
| Nocturnal awakening frequency | 2 (2.1 ± 1.2) | 3 (2.9 ± 1.4) | 15348 | <0.001 |
| Nap frequency | 1 (1.9 ± 1.2) | 2 (2.1 ± 1.3) | 22438 | 0.113 |
| Adolescents | ||||
| Habitual sleep latency | 2 (2.5 ± 1.3) | 3 (3.1 ± 1.7) | 7620 | <0.001 |
| Sufficiency of sleep | 2 (2.3 ± 0.9) | 3 (3.3 ± 0.9) | 4679 | <0.001 |
| Nocturnal awakening frequency | 2 (1.9 ± 1.1) | 3 (2.8 ± 1.1) | 5877 | <0.001 |
| Nap frequency | 1 (1.9 ± 1.2) | 2 (1.9 ± 1.1) | 10072 | 0.47 |
| Age Groups | DBSD | Good Sleepers | Bad Sleepers | U | p |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | ||||
| Children | SLS | 12.1 ± 2.5 | 15.4 ± 4.5 | 1817 | >0.001 |
| SWP | 19.1 ± 5.5 | 23.4 ± 5.4 | 1612 | 0.001 | |
| DMS | 14.8 ± 3.5 | 19.6 ± 3.5 | 1473 | >0.001 | |
| Preadolescents | SLS | 12.5 ± 2.9 | 13.9 ± 4.4 | 20527 | 0.014 |
| SWP | 20.3 ± 5.4 | 23 ± 5.7 | 16029 | >0.001 | |
| DMS | 15.3 ± 3.3 | 18.7 ± 3.7 | 12551 | >0.001 | |
| Adolescents | SLS | 12.3 ± 2.6 | 13.9 ± 3.3 | 7304 | >0.001 |
| SWP | 20.5 ± 5.6 | 25.0 ± 4.8 | 5151 | >0.001 | |
| DMS | 16.4 ± 3.6 | 19.6 ± 3.6 | 5584 | >0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malloggi, S.; Conte, F.; Gronchi, G.; Ficca, G.; Giganti, F. Prevalence and Determinants of Bad Sleep Perception among Italian Children and Adolescents. Int. J. Environ. Res. Public Health 2020, 17, 9363. https://doi.org/10.3390/ijerph17249363
Malloggi S, Conte F, Gronchi G, Ficca G, Giganti F. Prevalence and Determinants of Bad Sleep Perception among Italian Children and Adolescents. International Journal of Environmental Research and Public Health. 2020; 17(24):9363. https://doi.org/10.3390/ijerph17249363
Chicago/Turabian StyleMalloggi, Serena, Francesca Conte, Giorgio Gronchi, Gianluca Ficca, and Fiorenza Giganti. 2020. "Prevalence and Determinants of Bad Sleep Perception among Italian Children and Adolescents" International Journal of Environmental Research and Public Health 17, no. 24: 9363. https://doi.org/10.3390/ijerph17249363
APA StyleMalloggi, S., Conte, F., Gronchi, G., Ficca, G., & Giganti, F. (2020). Prevalence and Determinants of Bad Sleep Perception among Italian Children and Adolescents. International Journal of Environmental Research and Public Health, 17(24), 9363. https://doi.org/10.3390/ijerph17249363







