Impact of a Postoperative Intervention Educational Program on the Quality of Life of Patients with Hip Fracture: A Randomized, Open-Label Controlled Trial
Abstract
1. Introduction
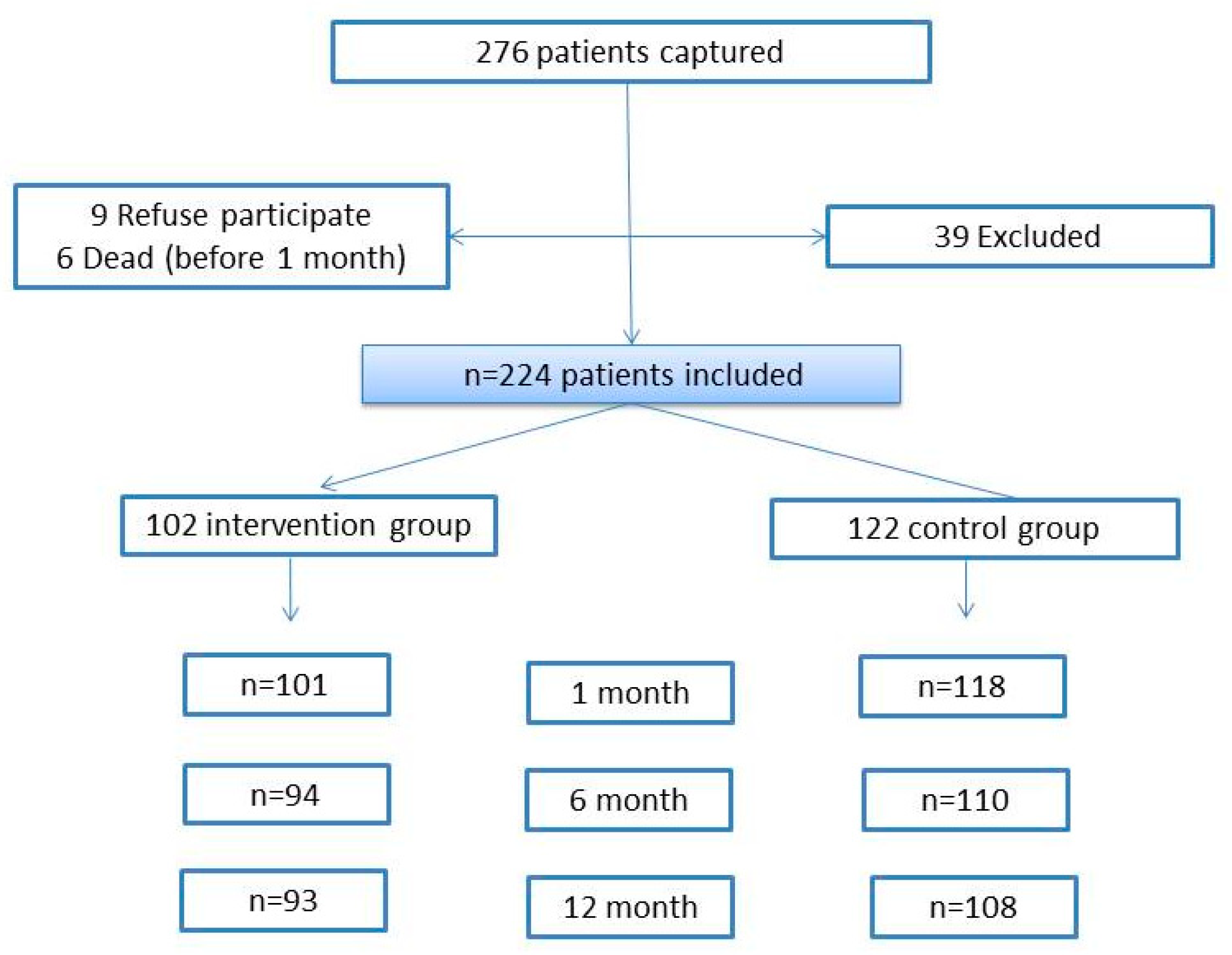
2. Methods
2.1. Study Design
2.2. Intervention
2.3. Variables
2.4. Statistical Analysis
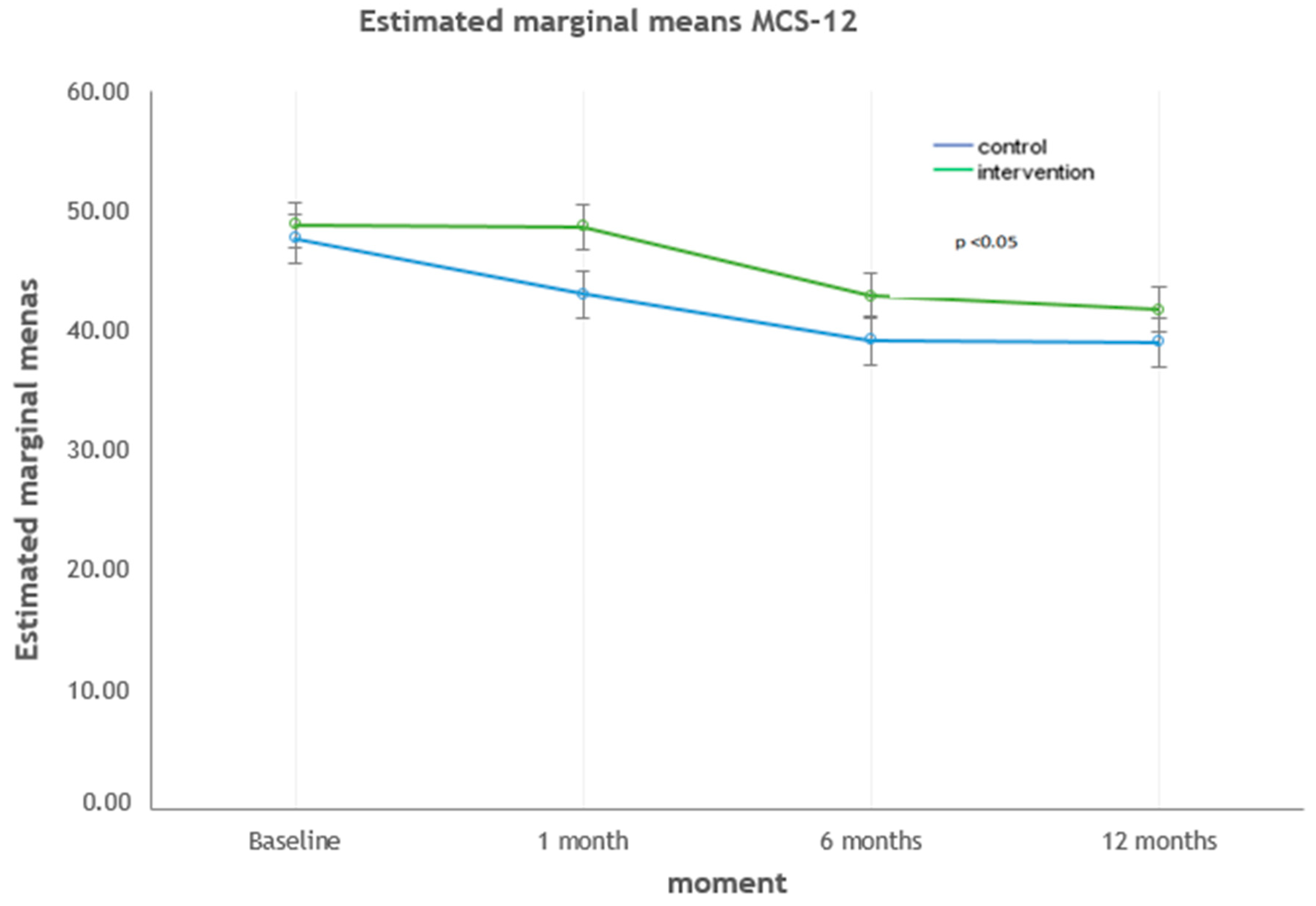
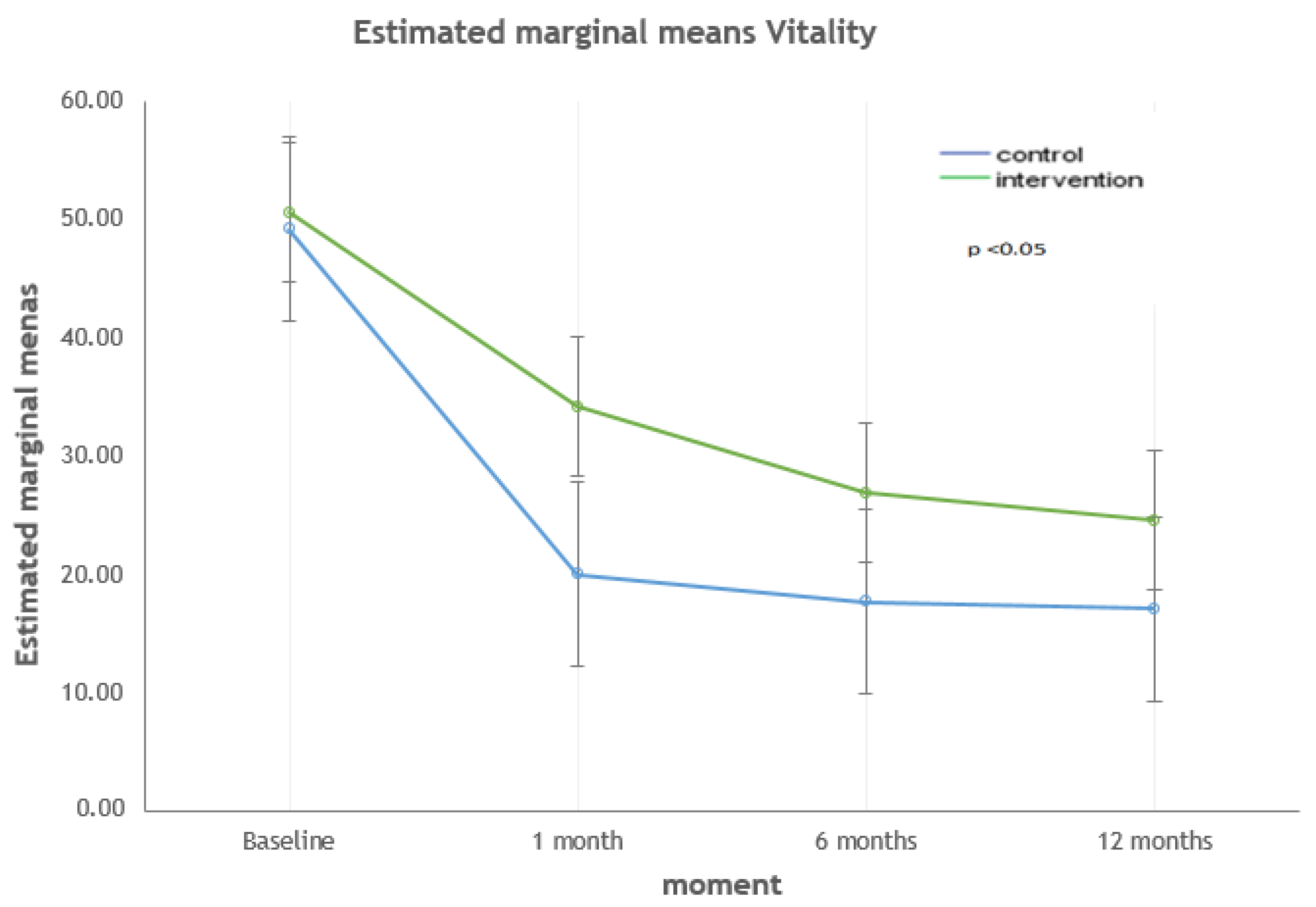
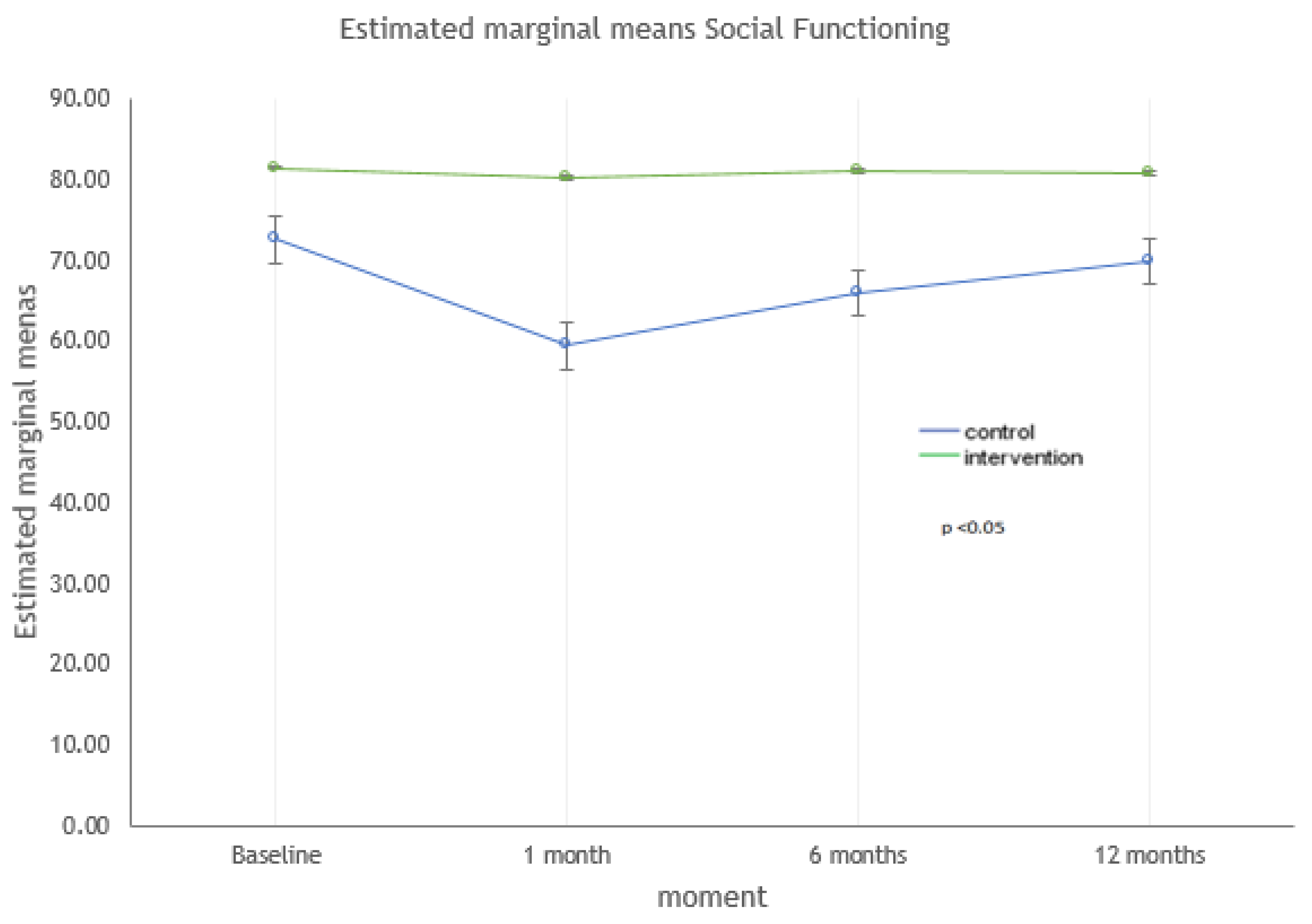
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ASA | American Society of Anesthesiologists |
| BI | Barthel index |
| CCI | Charlson comorbidity index |
| HRQoL | Health-related quality of life |
| FAC | Functional Ambulation Classification |
| MCS-12 | Mental summary dimension |
| PCS-12 | Physical summary dimension |
| SF-12 | SF-12 Health Survey |
| SD | Standard deviation |
References
- Prieto-Alhambra, D.; Reyes, C.; Sainz, M.S.; González-Macías, J.; Delgado, L.G.; Bouzón, C.A.; Gañan, S.M.; Miedes, D.M.; Vaquero-Cervino, E.; Bardaji, M.F.B.; et al. In-hospital care, complications, and 4-month mortality following a hip or proximal femur fracture: The Spanish registry of osteoporotic femur fractures prospective cohort study. Arch. Osteoporos. 2018, 13, 96. [Google Scholar] [CrossRef] [PubMed]
- López, P.S.; Montalvo, J.I.G.; Thies, C.O.; Campelo, P.G. Registro Nacional de Fracturas de Cadera. Informe Anual 2018; RNFC. IdiPAZ: Madrid, Spain, 2018. [Google Scholar]
- Moon, A.; Gray, A.; Deehan, D. Neck of Femur Fractures in Patient’s Aged More than 85 Years—Are They a Unique Subset? Geriatr. Orthop. Surg. Rehabil. 2011, 2, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Emmerson, B.; Varacallo, M.; Inman, D. Hip Fracture Overview. StatPearls 2020. Available online: https://www.ncbi.nlm.nih.gov/books/NBK557514/#article-22890.s11 (accessed on 5 October 2020).
- Dhanwal, D.K.; Dennison, E.M.; Harvey, N.C.; Cooper, C. Epidemiology of hip fracture: Worldwide geographic variation. Indian J. Orthop. 2011, 45, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Shumway-Cook, A.; Ciol, M.; Gruber, W.; Robinson, C. Incidence of and Risk Factors for Falls Following Hip Fracture in Community-dwelling Older Adults. Phys. Ther. 2005, 85, 648–655. [Google Scholar] [CrossRef]
- Portegijs, E.; Edgren, J.; Salpakoski, A.; Kallinen, M.; Rantanen, T.; Alén, M.; Kiviranta, I.; Sihvonen, S.; Sipilä, S. Balance Confidence Was Associated with Mobility and Balance Performance in Older People with Fall-Related Hip Fracture: A Cross-Sectional Study. Arch. Phys. Med. Rehabil. 2012, 93, 2340–2346. [Google Scholar] [CrossRef]
- Tang, V.L.; Sudore, R.; Cenzer, I.S.; Boscardin, W.J.; Smith, A.; Ritchie, C.; Wallhagen, M.; Finlayson, E.; Petrillo, L.; Covinsky, K. Rates of Recovery to Pre-Fracture Function in Older Persons with Hip Fracture: An Observational Study. J. Gen. Intern. Med. 2016, 32, 153–158. [Google Scholar] [CrossRef]
- Martinez-Laguna, D.; Nogués, X.; Abrahamsen, B.; Reyes, C.; Carbonell-Abella, C.; Diez-Perez, A.; Prieto-Alhambra, D. Excess of all-cause mortality after a fracture in type 2 diabetic patients: A population-based cohort study. Osteoporos. Int. 2017, 28, 2573–2581. [Google Scholar] [CrossRef]
- Gonzalez-Zabaleta, J.L.; Pita-Fernández, S.; Seoane-Pillado, T.; López-Calviño, B. Dependence for basic and instrumental activities of daily living after hip fractures. Arch. Gerontol. Geriatr. 2015, 60, 66–70. [Google Scholar] [CrossRef]
- Peeters, C.M.; Visser, E.; Van De Ree, C.L.; Gosens, T.; Oudsten, B.L.D.; De Vries, J. Quality of life after hip fracture in the elderly: A systematic literature review. Injury 2016, 47, 1369–1382. [Google Scholar] [CrossRef]
- Boonen, S.; Autier, P.; Barette, M.; Vanderschueren, D.; Lips, P.; Haentjens, P. Functional outcome and quality of life followinghip fracture in elderly women: A prospective controlled study. Osteoporos. Int. 2004, 15, 87–94. [Google Scholar]
- Dyer, S.M.; for the Fragility Fracture Network (FFN) Rehabilitation Research Special Interest Group; Crotty, M.; Fairhall, N.; Magaziner, J.; Beaupre, L.A.; Cameron, I.D.; Sherrington, C. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr. 2016, 16, 158. [Google Scholar] [CrossRef] [PubMed]
- Hallberg, I.; Rosenqvist, A.M.; Kartous, L.; Toss, G. Health-related quality of life after osteoporotic fractures. Osteoporos. Int. 2004, 15, 834–841. [Google Scholar] [CrossRef] [PubMed]
- Dinamarca, J. Fracturas de cadera y calidad de vida: La Ortogeriatría en el ojo del huracán. Bol. Hosp. Vina Mar. 2017, 73, 124–131. [Google Scholar]
- Alexiou, K.; Roushias, A.; Varitimidis, S.E.; Malizos, K.N. Quality of life and psychological consequences in elderly patients after a hip fracture: A review. Clin. Interv. Aging 2018, 13, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Sanclemente-Boli, T.; Ponce-Ruiz, S.; Álvarez-Lorenzo, C.; Zuriguel-Pérez, E.; Tapia-Melenchon, R.; Ramentol-Sintas, M.; Villar-Casares, M.D.M.; Teixidor-Serra, J.; Molero-García, V.; Sánchez-Raya, J.; et al. Effectiveness of a multidisciplinary educational intervention in patients with hip fracture: SWEET HOME study. Med. Clin. 2019, 153, 446–453. [Google Scholar] [CrossRef]
- Cinnella, G.; Gambatesa, M.; D’Antini, D.; Mirabella, L.; De Capraris, A.; Iuso, S.; Bellomo, A.; MacChiarola, A.; Dambrosio, M.; D’Ambrosio, A. Counseling, quality of life, and acute postoperative pain in elderly patients with hip fracture. J. Multidiscip. Healthc. 2013, 6, 335–346. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioural Science. In Statistical Power Anaylsis for the Behavioural Science, 2nd ed.; Lawrence Erlbaum Associates: New York, NY, USA, 1988; ISBN 0805802835. [Google Scholar]
- Consensus development conference: Diagnosis, prophylaxis, and treatment of osteoporosis. Am. J. Med. 1993, 94, 646–650. [CrossRef]
- Gandhi, S.; Salmon, J.; Zhao, S.; Lambert, B.L.; Gore, P.R.; Conrad, K. Psychometric evaluation of the 12-item short-form health survey (SF-12) in osteoarthritis and rheumatoid arthritis clinical trials. Clin. Ther. 2001, 23, 1080–1098. [Google Scholar] [CrossRef]
- Vilagut, G.; Ferrer, M.; Rajmil, L.; Rebollo, P.; Permanyer-Miralda, G.; Quintana, J.M.; Santed, R.; Valderas, J.M.; Ribera, A.; Domingo-Salvany, A.; et al. El Cuestionario de Salud SF-36 español: Una década de experiencia y nuevos desarrollos. Gac. Sanit. 2005, 19, 135–150. [Google Scholar] [CrossRef]
- Mahoney, F.; Barthel, D.W. Functional Evaluation: The Barthel Index. Md. State Med. J. 1965, 14, 61–65. [Google Scholar]
- Shah, S.; Vanclay, F.; Cooper, B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J. Clin. Epidemiol. 1989, 42, 703–709. [Google Scholar] [CrossRef]
- Lawton, M.; Brody, E. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Holden, M.; Gill, K.; Magliozzi, M. Gait assessment for neurologically impaired patients. Standards for outcome assessment. Phys. Ther. 1986, 66, 1530–1539. [Google Scholar] [CrossRef] [PubMed]
- Yesavage, J.; Brink, T.; Rose, T.; Lum, O.; Huang, V.; Adey, M.; Leirer, V.O. Development and validation of a geriatric depression screening scale: A preliminaryreport. J. Psychiatr. Res. 1983, 17, 37–49. [Google Scholar] [CrossRef]
- Martí, D.; Miralles, R.; Llorach, I. Depressive dissorders in a convalescence unit: Experience and validation of a Spanish versión of the 15-item Geriatric Depression Scale. Rev. Esp. Geriatr. Gerontol. 2000, 35, 7–14. [Google Scholar]
- Díaz, M.; Domínguez, O.; Toyos, G. Results of the application of a scale of social-familiar situation in primare care. Trab. Soc. Salud 1993, 16, 137–156. [Google Scholar]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chronic Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Lima, C.A.; Sherrington, C.; Guaraldo, A.; De Moraes, S.A.; Varanda, R.D.R.; Melo, J.D.A.; Kojima, K.E.; Perracini, M. Effectiveness of a physical exercise intervention program in improving functional mobility in older adults after hip fracture in later stage rehabilitation: Protocol of a randomized clinical trial (REATIVE Study). BMC Geriatr. 2016, 16, 1–6. [Google Scholar] [CrossRef]
- Hoekstra, J.C.; Goosen, J.H.M.; De Wolf, G.S.; Verheyen, K.C.P.M. Effectiveness of multidisciplinary nutritional care on nutritional intake, nutritional status and quality of life in patients with hip fractures: A controlled prospective cohort study. Clin. Nutr. 2011, 30, 455–461. [Google Scholar] [CrossRef]
- Romeo, R.; Knapp, M.; Banerjee, S.; Morris, J.; Baldwin, R.; Tarrier, N.; Pendleton, N.; Horan, M.; Burns, A. Treatment and prevention of depression after surgery for hip fracture in older people: Cost-effectiveness analysis. J. Affect. Disord. 2011, 128, 211–219. [Google Scholar] [CrossRef]
- Moerman, S.; Vochteloo, A.J.H.; Tuinebreijer, W.E.; Maier, A.B.; Mathijssen, N.M.C.; Nelissen, R.G.H.H. Factors associated with the course of health-related quality of life after a hip fracture. Arch. Orthop. Trauma Surg. 2016, 136, 935–943. [Google Scholar] [CrossRef] [PubMed]
- Allegrante, J.P.; Peterson, M.G.E.; Cornell, C.N.; MacKenzie, C.R.; Robbins, L.; Horton, R.; Ganz, S.B.; Ruchlin, H.S.; Russo, P.W.; Paget, S.A.; et al. Methodological Challenges of Multiple-Component Intervention: Lessons Learned from a Randomized Controlled Trial of Functional Recovery After Hip Fracture. HSS J. 2006, 3, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Zidén, L.; Frandin, K.; Kreuter, M. Home rehabilitation after hip fracture.A randomized controlled study on balance confidence, physical function and everyday activities. Clin. Rehabil. 2008, 22, 1019–1033. [Google Scholar] [CrossRef] [PubMed]
- Zidén, L.; Kreuter, M.; Frändin, K. Long-term effects of home rehabilitation after hip fracture—1-year follow-up of functioning, balance confidence, and health-related quality of life in elderly people. Disabil. Rehabil. 2010, 32, 18–32. [Google Scholar] [CrossRef] [PubMed]
- Beaupre, L.; Cinats, J.G.; Senthilselvan, A.; Scharfenberger, A.; Johnston, D.W.; Saunders, L.D. Does standardized rehabilitation and discharge planning improve functional recovery in elderly patients with hip fracture? Arch. Phys. Med. Rehabil. 2005, 86, 2231–2239. [Google Scholar] [CrossRef] [PubMed]
- Shyu, Y.-I.L.; Liang, J.; Wu, C.-C.; Cheng, H.-S.; Chen, M.-C. An interdisciplinary intervention for older Taiwanese patients after surgery for hip fracture improves health-related quality of life. BMC Musculoskelet. Disord. 2010, 11, 225. [Google Scholar] [CrossRef]
- Zapata, M.M.; Sales, M.J.; Roig, X.A.; Canovas, E.; Cuchí, G.U. Estudio prospectivo multicéntrico de una cohorte para evaluar la calidad de vidade pacientes intervenidos de fractura subcapital de fémur. Trauma Fund MAPFRE 2014, 25, 188–195. [Google Scholar]
- Úbeda Tomás, A.; Martínez Martínez, M.I.; Alfonso Sánchez, J.L.; Brú Pomer, A.; Espí Escrivá, F.; Ribes Iborra, J. Estudio de calidad de vida de pacientes con coxartrosis. Rev. Española Cirugía Osteoartic. 2015, 50, 93–98. [Google Scholar]
- Ramírez-Pérez, E.; Clark, P.; Carlos, F.; Camacho, A.; Franco-Marina, F. Seguimiento de la calidad de vida relacionada con la salud después de una cirugía de fractura de cadera: Estudio multicéntrico en población mexicana. Medwave 2014, 14, 5972. [Google Scholar] [CrossRef]
- Milte, R.; Crotty, M.; Miller, M.; Whitehead, C.; Ratcliffe, J. Quality of life in older adults following a hip fracture: An empirical comparison of the ICECAP-O and the EQ-5D-3 L instruments. Health Qual. Life Outcomes 2018, 16, 173. [Google Scholar] [CrossRef]
- Parsons, N.; Griffin, X.L.; Achten, J.; Chesser, T.J.; Lamb, S.E.; Costa, M.L. Modelling and estimation of health-related quality of life after hip fracture. Bone Jt. Res. 2018, 7, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Peterson, M.G.E.; Allegrante, J.P.; Cornell, C.N.; MacKenzie, C.R.; Robbins, L.; Horton, R.; Ganz, S.B.; Augurt, A. Measuring Recovery after a Hip Fracture Using the SF-36 and Cummings Scales. Osteoporos. Int. 2002, 13, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Sylliaas, H.; Thingstad, P.; Wyller, T.B.; Helbostad, J.L.; Sletvold, O.; Bergland, A. Prognostic factors for self-rated function and perceived health in patient living at home three months after a hip fracture. Disabil. Rehabil. 2012, 34, 1225–1231. [Google Scholar] [CrossRef] [PubMed]
- Prieto-Alhambra, D.; Moral-Cuesta, D.; Palmer, A.; Aguado-Maestro, I.; Bardaji, M.F.B.; Brañas, F.; Bueno, G.A.; Caeiro-Rey, J.R.; Cano, I.A.; Barres-Carsi, M.; et al. The impact of hip fracture on health-related quality of life and activities of daily living: The SPARE-HIP prospective cohort study. Arch. Osteoporos. 2019, 14, 56. [Google Scholar] [CrossRef]
- Brouwer, B.; Walker, C.; Rydahl, S.; Culham, E. Reducingfear of falling in seniors through education and activityprograms: A randomized trial. J. Am. Geriatr. Soc. 2003, 51, 829–834. [Google Scholar] [CrossRef]
- Scholten, A.C.; Haagsma, J.A.; Steyerberg, E.W.; Van Beeck, E.F.; Polinder, S. Assessment of pre-injury health-related quality of life: A systematic review. Popul. Health Metrics 2017, 15, 10. [Google Scholar] [CrossRef]
- Polinder, S.; Haagsma, J.; Belt, E.; Lyons, R.A.; Erasmus, V.; Lund, J.; van Beeck, E.F. A systematic review of studies measuring health-related quality of life of general injury populations. BMC Public Health 2010, 10, 783. [Google Scholar] [CrossRef]
| Intervention Group (n = 102, 45.5%) | Control Group (n = 122, 54.5%) | p-Value * | |
|---|---|---|---|
| Gender, n (%) | |||
| Female | 80 (78.4) | 91 (74.6) | 0.501 |
| Male | 22 (21.6) | 31 (25.4) | |
| Age, mean (SD) $ | 84.4 (5.5) | 84.8 (6.6) | 0.320 |
| Groups, n (%) | 0.070 | ||
| <85 years | 55 (53.9) | 51 (41.8) | |
| ≥85 years | 47 (46.1) | 71 (58.2) | |
| Study level, n (%) | 0.254 | ||
| No studies | 45 (44.1) | 40 (32.8) | |
| Primary | 52 (51.0) | 78 (63.9) | |
| Secondary | 3 (2.9) | 3 (2.5) | |
| University | 2 (2.0) | 1 (0.8) | |
| Living status, n (%) | 0.552 | ||
| Living alone | 24 (23.5) | 33 (27.0) | |
| Living in couple | 26 (25.5) | 35 (28.7) | |
| Living with relatives | 34 (33.3) | 28 (23.0) | |
| Supervised flat | 3 (2.9) | 4 (3.3) | |
| Residency | 15 (14.7) | 22 (18.0) | |
| Clinical history, n (%) | |||
| Prior diagnosis of Osteoporosis | 7 (6.9) | 14 (11.5) | 0.238 |
| Previous hip fracture, n (%) | 11 (10.8) | 7 (5.7) | 0.166 |
| Polymedication, n (%) | 78 (76.5) | 78 (63.9) | 0.154 |
| Charlson comorbidity index, mean (SD) | 5.2 (1.0) | 5.4 (1.3) | 0.421 |
| Type of fracture, n (%) | 0.079 | ||
| Neck | 36 (35.3) | 44 (36.1) | |
| Trochanter | 66 (64.7) | 78 (63.9) | |
| Type of surgical intervention, n (%) | 0.749 | ||
| Intramedullary nail | 68 (67.3) | 79 (65.3) | |
| Hip replacement | 33 (32.7) | 42 (34.7) | |
| ASA PS for peri-operative risk, n (%) | 0.075 | ||
| I | 1 (1.0) | 0 (0.0) | |
| II | 21 (20.6) | 49 (40.2) | |
| III | 70 (68.6) | 66 (54.1) | |
| IV | 10 (9.8) | 7 (5.7) | |
| Destination after surgery, n (%) | 0.392 | ||
| Home | 49 (48.0) | 49 (40.2) | |
| Institution | 33 (31.4) | 52 (42.6) | |
| With relatives | 20 (19.6) | 20 (16.4) | |
| Barthel index, mean (SD) | 88.18 (16.22) | 87.09 (17.47) | 0.974 |
| Lawton and Brody scale, mean (SD) | 5.20 (2.59) | 4.93 (2.75) | 0.604 |
| Functional Ambulation Classification (FAC): Does not walk independently, n (%) | 33 (32.7%) | 62 (51.2%) | 0.060 |
| Baseline | 1 Month | 6 Months | 12 Months | Within (Intra) | Between (Inter) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | p-Value # | p-Value # | |||||
| Control | Intervention | Control | Intervention | Control | Intervention | Control | Intervention | |||
| 62 | 73 | 62 | 73 | 62 | 73 | 62 | 73 | |||
| MCS-12 | 47.7 (10.8) | 48.9 (11,1) | 43 (13.2) | 48.7 (12.2) | 39.3 (11.8) | 42.9 (11.7) | 39.1 (12.1) | 41.8 (11.4) | 0.177 | 0.043 |
| PCS-12 | 39.9 (10.9) | 39.4 (11.4) | 29.0 (5.4) | 28.5 (4.5) | 32.5 (6.4) | 31.4 (4.8) | 32.8 (5.9) | 32.4 (5.7) | 0.092 | 0.460 |
| Physical function | 50.3 (39.4) | 51.9 (41.5) | 4.5 (17.1) | 3.7 (13.2) | 13.7 (24.4) | 11.2 (23.8) | 13.4 (24.1) | 13.3 (28.4) | 0.741 | 0.880 |
| Physical role | 51.3 (24.6) | 49.8 (24.9) | 25.5 (5.1) | 25.5 (3.4) | 28.4 (11.9) | 28.3 (12.4) | 26.1 (6.2) | 30.1 (15.3) | 0.228 | 0.645 |
| Bodily pain | 68.9 (28.4) | 64.2 (32.8) | 55.5 (22.8) | 59.1 (24.1) | 66.6 (20.5) | 67.3 (24.1) | 68.4 (22.5) | 69.2 (23.4) | 0.253 | 0.973 |
| General health | 46.3 (21.6) | 50.7 (21.3) | 32.1 (16.2) | 32.7 (16.9) | 28.4 (14.4) | 29.4 (17.4) | 27.9 (15.4) | 26.9 (17.7) | 0.195 | 0.530 |
| Vitality | 49.1 (33.3) | 50.5 (30.8) | 20.0 (24.9) | 34.1 (28.6) | 17.6 (20.3) | 26.8 (25.4) | 17.1 (21.9) | 24.5 (25.9) | 0.036 | 0.010 |
| Social functioning | 72.6 (24.7) | 81,5 (24.8) | 59.5 (28.1) | 80.4 (26.2) | 66.1 (22.7) | 81.1 (23.3) | 70.0 (21.1) | 80.8 (20.2) | 0.006 | <0.001 |
| Emotional role | 64.7 (19.5) | 61.9 (21.8) | 52.4 (24.7) | 57.0 (23.9) | 46.1 (24.5) | 47.4 (24.9) | 44.7 (24.4) | 45.6 (24.7) | 0.217 | 0.694 |
| Mental health | 65.4 (23.7) | 64.5 (24.2) | 49.3 (22.2) | 58.2 (22.6) | 44.7 (19.7) | 48.6 (20.8) | 42.4 (20.7) | 44.4 (20.2) | 0.056 | 0.224 |
| Physical Component Summary (PCS-12) 12 Months | Mental Component Summary (MCS-12) 12 Months | |||
| Mean (SD) | p-Value $ | Mean (SD) | p-Value $ | |
| Gender | 31.6 (6.2) | 0.094 | 46.7 (13) | 0.006 |
| Polymedication | 38 (33.8) | 0.135 | 38 (42.9) | 0.372 |
| Living status | 68 (33.3) | 0.023 | 68 (41.4) | 0.575 |
| Functional Ambulation Classification (FAC) | 77 (32.3) | 0.626 | 77 (39) | 0.050 |
| Rho | p-Value & | Rho | p-Value & | |
| Age | 0.026 | 0.727 | −0.216 | 0.003 |
| Charlson comorbidity index | 0.049 | 0.502 | −0.119 | 0.105 |
| Barthel index 12 months | 0.265 | <0.001 | 0.304 | <0.001 |
| Gijon scale 12 months | −0.143 | 0.050 | −0.194 | 0.008 |
| Yesavage depression scale 12 months | −0.075 | 0.305 | −0.562 | <0.001 |
| Lawton and Brody scale 12 months | 0.290 | <0.001 | 0.211 | 0.004 |
| MODEL | ||||||||
|---|---|---|---|---|---|---|---|---|
| B | IC 95% to B | Sig. | R2 | R2c | p-Value | |||
| Physical Component Summary (PCS-12) | Lawton and Brody scale | 1.058 | 0.353 | 1.764 | 0.003 | 0.203 | 0.176 | <0.001 |
| Mental Component Summary (MCS-12) | Age | −0.456 | −0.784 | −0.128 | 0.007 | 0.357 | 0.314 | <0.001 |
| Yesavage depression scale | −1.738 | −2.486 | −0.989 | <0.001 | ||||
| Physical function | Barthel index | 0.286 | 0.035 | 0.536 | 0.026 | 0.412 | 0.378 | <0.001 |
| Lawton and Brody scale | 4.301 | 1.607 | 6.994 | 0.002 | ||||
| Physical role | Intervention | 4.796 | 1.907 | 7.685 | 0.001 | 0.304 | 0.268 | <0.001 |
| Lawton and Brody scale | 2.369 | 1.049 | 3.689 | 0.001 | ||||
| Bodily pain | Charlson comorbidity index | 2.850 | 0.155 | 5.545 | 0.038 | |||
| Yesavage depression scale | −2.412 | −3.556 | −1.267 | <0.001 | ||||
| General health | Barthel index | 0.223 | 0.071 | 0.376 | 0.004 | |||
| Yesavage depression scale | −0.969 | −1.651 | −0.286 | 0.006 | ||||
| Vitality | Intervention | 10.171 | 4.505 | 15.837 | 0.001 | 0.413 | 0.379 | <0.001 |
| Yesavage geriatric depression scale | −1.105 | −2.194 | −0.016 | 0.047 | ||||
| Lawton and Brody scale | 4.825 | 2.213 | 7.438 | 0.000 | ||||
| Social functioning | Intervention | 10.155 | 4.895 | 15.415 | <0.001 | 0.267 | 0.249 | <0.001 |
| Yesavage depression scale | −1.531 | −2.457 | −0.605 | 0.001 | ||||
| Emotional role | Age | −0.659 | −1.248 | −0.070 | 0.029 | 0.330 | 0.294 | <0.001 |
| Yesavage depression scale | −3.741 | −5.016 | −2.466 | <0.001 | ||||
| Mental health | Yesavage depression scale | −2.616 | −3.806 | −1.427 | <0.001 | 0.323 | 0.281 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amarilla-Donoso, F.J.; Roncero-Martín, R.; Lavado-García, J.; Canal-Macías, M.d.l.L.; Pedrera-Canal, M.; Chimpén-López, C.; Toribio-Felipe, R.; Rico-Martin, S.; Barrios-Fernández, S.; López-Espuela, F. Impact of a Postoperative Intervention Educational Program on the Quality of Life of Patients with Hip Fracture: A Randomized, Open-Label Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 9327. https://doi.org/10.3390/ijerph17249327
Amarilla-Donoso FJ, Roncero-Martín R, Lavado-García J, Canal-Macías MdlL, Pedrera-Canal M, Chimpén-López C, Toribio-Felipe R, Rico-Martin S, Barrios-Fernández S, López-Espuela F. Impact of a Postoperative Intervention Educational Program on the Quality of Life of Patients with Hip Fracture: A Randomized, Open-Label Controlled Trial. International Journal of Environmental Research and Public Health. 2020; 17(24):9327. https://doi.org/10.3390/ijerph17249327
Chicago/Turabian StyleAmarilla-Donoso, Francisco Javier, Raúl Roncero-Martín, Jesus Lavado-García, María de la Luz Canal-Macías, María Pedrera-Canal, Carlos Chimpén-López, Rosaura Toribio-Felipe, Sergio Rico-Martin, Sabina Barrios-Fernández, and Fidel López-Espuela. 2020. "Impact of a Postoperative Intervention Educational Program on the Quality of Life of Patients with Hip Fracture: A Randomized, Open-Label Controlled Trial" International Journal of Environmental Research and Public Health 17, no. 24: 9327. https://doi.org/10.3390/ijerph17249327
APA StyleAmarilla-Donoso, F. J., Roncero-Martín, R., Lavado-García, J., Canal-Macías, M. d. l. L., Pedrera-Canal, M., Chimpén-López, C., Toribio-Felipe, R., Rico-Martin, S., Barrios-Fernández, S., & López-Espuela, F. (2020). Impact of a Postoperative Intervention Educational Program on the Quality of Life of Patients with Hip Fracture: A Randomized, Open-Label Controlled Trial. International Journal of Environmental Research and Public Health, 17(24), 9327. https://doi.org/10.3390/ijerph17249327






