A Multimodal Stress-Prevention Program Supplemented by Telephone-Coaching Sessions to Reduce Perceived Stress among German Farmers: Results from a Randomized Controlled Trial
Abstract
1. Introduction
- (1)
- participation in SGS would reduce perceived stress and improve further stress-related outcomes in the short and medium term;
- (2)
- participants receiving SGS followed by telephone-coaching would have better outcomes compared to controls receiving SGS without subsequent telephone-coaching.
2. Methods
- (1)
- SMI: (10 × 2 h) (Table 1), each of the 10 sessions consists of a theoretical part and practical exercises;
- (2)
- Relaxation: autogenic training (2 × 1 h), progressive muscle relaxation according to Jacobson (2 × 1 h), mindfulness-based stress reduction (4 × 1 h), massage (4 × 30 min);
- (3)
- Physical exercise: back schooling (2 × 1 h), aqua fitness (4 × 1 h), endurance sports activities (4 × 1 h);
- (4)
- Balneotherapy: 4 × peat or sulfur baths (20 min) followed by a resting period (20 min).
2.1. Telephone-Coaching
2.2. Outcomes and Measures
2.3. Data Analysis
2.4. Compliance with Ethical Standards and Registration
3. Results
3.1. Participant Flow
3.2. Participant Characteristics at Baseline
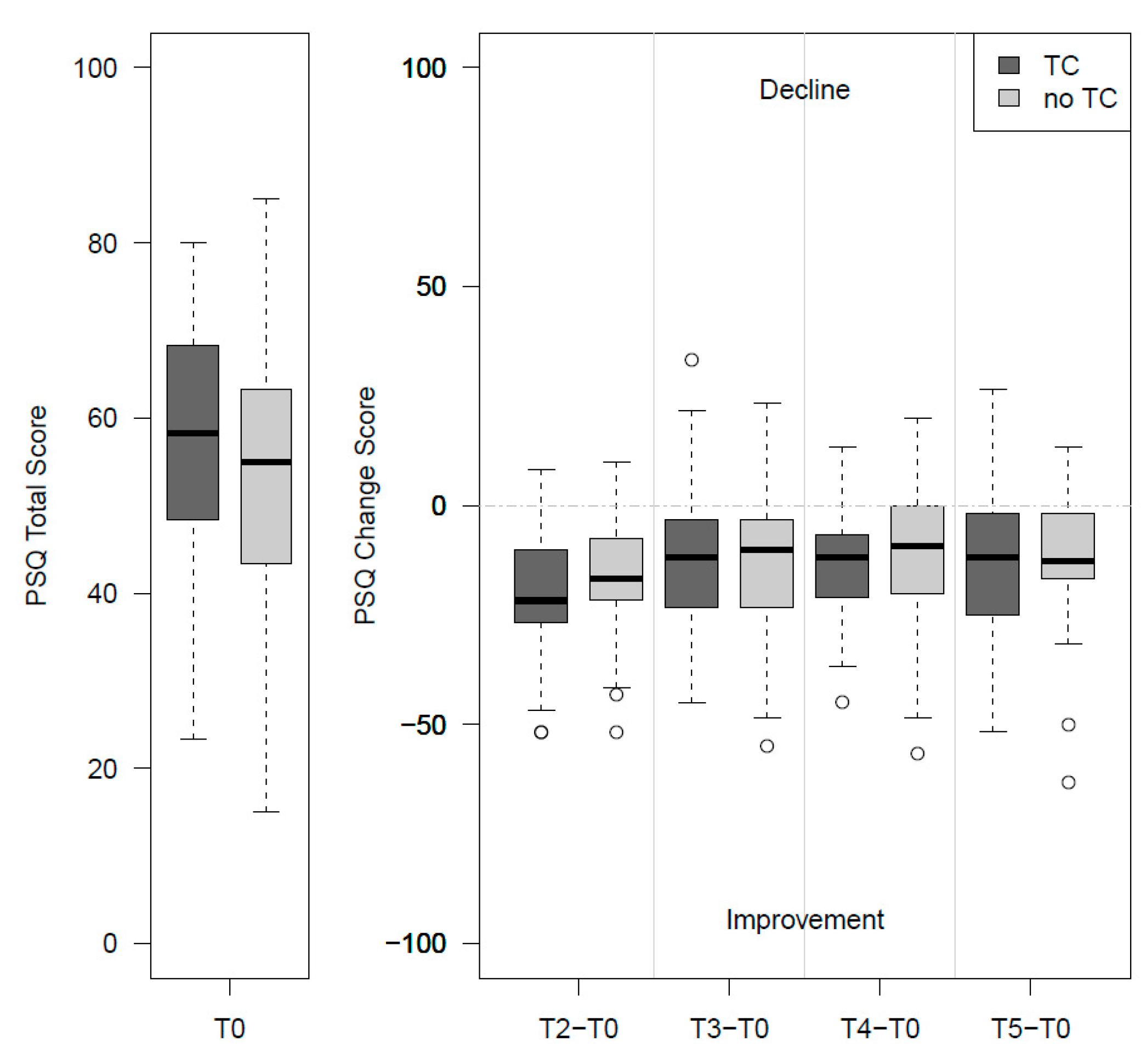
3.3. Change in PSQ-Total and Secondary Outcomes
3.4. Within-Group Changes
3.5. Participant Satisfaction
4. Discussion
Limitations and Strengths
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Stier-Jarmer, M.; Frisch, D.; Oberhauser, C.; Berberich, G.; Schuh, A. The Effectiveness of a Stress Reduction and Burnout Prevention Program. Dtsch. Arztebl. Int. 2016, 113, 781–788. [Google Scholar] [CrossRef] [PubMed]
- Truchot, D.; Andela, M. Burnout and hopelessness among farmers: The Farmers Stressors Inventory. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 859–867. [Google Scholar] [CrossRef] [PubMed]
- Hounsome, B.; Edwards, R.T.; Hounsome, N.; Edwards-Jones, G. Psychological morbidity of farmers and non-farming population: Results from a UK survey. Community Ment. Health J. 2012, 48, 503–510. [Google Scholar] [CrossRef] [PubMed]
- Fraser, C.E.; Smith, K.B.; Judd, F.; Humphreys, J.S.; Fragar, L.J.; Henderson, A. Farming and mental health problems and mental illness. Int. J. Soc. Psychiatry 2005, 51, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Jones-Bitton, A.; Best, C.; MacTavish, J.; Fleming, S.; Hoy, S. Stress, anxiety, depression, and resilience in Canadian farmers. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 55, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Rudolphi, J.M.; Berg, R.L.; Parsaik, A. Depression, Anxiety and Stress Among Young Farmers and Ranchers: A Pilot Study. Community Ment. Health J. 2020, 56, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Schirmer, J.; Peel, D.; Mylek, M. The 2014 Regional Wellbeing Survey-Farmers and Agriculture Canberra: University of Canberra. 2015. Available online: https://www.canberra.edu.au/research/institutes/health-research-institute/files/regional-wellbeing-survey/reports/2015-reports/Barriers-to-farm-development_26Oct2016.pdf (accessed on 29 January 2010).
- Daghagh Yazd, S.; Wheeler, S.A.; Zuo, A. Key Risk Factors Affecting Farmers’ Mental Health: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 4849. [Google Scholar] [CrossRef]
- Gevaert, J.; Moortel, D.; Wilkens, M.; Vanroelen, C. What’s up with the self-employed? A cross-national perspective on the self-employed’s work-related mental well-being. SSM Popul. Health 2018, 4, 317–326. [Google Scholar] [CrossRef]
- Saarni, S.I.; Saarni, E.S.; Saarni, H. Quality of life, work ability, and self employment: A population survey of entrepreneurs, farmers, and salary earners. Occup. Environ. Med. 2008, 65, 98–103. [Google Scholar] [CrossRef]
- Vayro, C.; Brownlow, C.; Ireland, M.; March, S. ‘Farming is not Just an Occupation [but] a Whole Lifestyle’: A Qualitative Examination of Lifestyle and Cultural Factors Affecting Mental Health Help-Seeking in Australian Farmers. Sociol. Rural. 2020, 60, 151–173. [Google Scholar] [CrossRef]
- Härter, M.; Dirmaier, J.; Dwinger, S.; Kriston, L.; Herbarth, L.; Siegmund-Schultze, E.; Bermejo, I.; Matschinger, H.; Heider, D.; König, H.-H. Effectiveness of Telephone-Based Health Coaching for Patients with Chronic Conditions: A Randomised Controlled Trial. PLoS ONE 2016, 11, e0161269. [Google Scholar] [CrossRef] [PubMed]
- Inglis, S.C.; Clark, R.A.; Dierckx, R.; Prieto-Merino, D.; Cleland, J.G. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Cochrane Database Syst. Rev. 2015, 10, CD007228. [Google Scholar] [CrossRef] [PubMed]
- Dennis, S.M.; Harris, M.; Lloyd, J.; Powell Davies, G.; Faruqi, N.; Zwar, N. Do people with existing chronic conditions benefit from telephone-coaching? A rapid review. Aust. Health Rev. 2013, 37, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, A.J.; Breckon, J.D. A review of telephone-coaching services for people with long-term conditions. J. Telemed. Telecare 2011, 17, 451–458. [Google Scholar] [CrossRef] [PubMed]
- Levenstein, S.; Prantera, C.; Varvo, V.; Scribano, M.; Berto, E.; Luzi, C.; Andreoli, A. Development of the perceived stress questionnaire: A new tool for psychosomatic research. J. Psychosom. Res. 1993, 37, 19–32. [Google Scholar] [CrossRef]
- Fliege, H.; Rose, M.; Arck, P.; Levenstein, S.; Klapp, B.F. Validierung des “Perceived Stress Questionnaire“ (PSQ) an einer deutschen Stichprobe. Diagnostica 2001, 47, 142–152. [Google Scholar] [CrossRef]
- Fliege, H.; Rose, M.; Arck, P.; Walter, O.B.; Kocalevent, R.-D.; Weber, C.; Klapp, B.F. The Perceived Stress Questionnaire (PSQ) Reconsidered: Validation and Reference Values From Different Clinical and Healthy Adult Samples. Psychosom. Med. 2005, 67, 78–88. [Google Scholar] [CrossRef]
- Büssing, A.; Glaser, J. Managerial Stress und Burnout, A Collaborative International Study (CISMS), Die Deutsche Untersuchung; Technische Universität, Lehrstuhl für Psychologie: München, Germany, 1998. [Google Scholar]
- Bech, P. Measuring the Dimension of Psychological General Well-Being by the WHO-5. Qual. Life Newsl. 2004, 32, 15–16. [Google Scholar]
- Bech, P.; Olsen, L.R.; Kjoller, M.; Rasmussen, N.K. Measuring well-being rather than the absence of distress symptoms: A comparison of the SF-36 Mental Health subscale and the WHO-Five well-being scale. Int. J. Methods Psychiatr. Res. 2003, 12, 85–91. [Google Scholar] [CrossRef]
- Rabin, R.; de Charro, F. EQ-5D: A measure of health status from the EuroQol Group. Ann. Med. 2001, 33, 337–343. [Google Scholar] [CrossRef]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; E Parkin, D.; Bonsel, G.J.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef]
- Gerber, M.; Lang, C.; Lemola, S.; Colledge, F.; Kalak, N.; Holsboer-Trachsler, E.; Pühse, U.; Brand, S. Validation of the German version of the insomnia severity index in adolescents, young adults and adult workers: Results from three cross-sectional studies. BMC Psychiatry 2016, 16, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Beierlein, C.; Kemper, C.J.; Kovaleva, A.; Rammstedt, B. Kurzskala zur Erfassung allgemeiner Selbstwirksamkeitserwartungen (ASKU). Methoden Daten Anal. 2013, 7, 251–278. [Google Scholar]
- Lowe, B.; Kroenke, K.; Grafe, K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J. Psychosom. Res. 2005, 58, 163–171. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.; Monahan, P.O.; Lowe, B. Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Ann. Intern. Med. 2007, 146, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Hasselhorn, H.M.; Freude, G. Der Work Ability Index-Ein Leitfaden; Schriftenreihe der Bundesanstalt für Arbeitsschutz und Arbeitsmedizin—Sonderschrift—S 87; Bundesanstalt für Arbeitsschutz und Arbeitsmedizin: Dortmund/Berlin/Dresden, Germany, 2007. [Google Scholar]
- R-Core-Team. A language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria, 2019. Available online: https://www.R-project.org/ (accessed on 11 May 2020).
- Kocalevent, R.D.; Hinz, A.; Brahler, E.; Klapp, B.F. Regional and individual factors of stress experience in Germany: Results of a representative survey with the perceived stress questionnaire (PSQ). Gesundheitswesen 2011, 73, 829–834. [Google Scholar] [CrossRef] [PubMed]
- Morin, C.M.; Belleville, G.; Belanger, L.; Ivers, H. The Insomnia Severity Index: Psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011, 34, 601–608. [Google Scholar] [CrossRef]
- Dieck, A.; Morin, C.M.; Backhaus, J. A German version of the Insomnia Severity Index. Validation and identification of a cut-off to detect insomnia. Somnologie 2018, 22, 27–35. [Google Scholar] [CrossRef]
- Alkhawaldeh, J.M.A.; Soh, K.L.; Mukhtar, F.B.M.; Ooi, C.P. Effectiveness of stress management interventional programme on occupational stress for nurses: A systematic review. J. Nurs. Manag. 2020, 28, 209–220. [Google Scholar] [CrossRef]
- Seo, E.; Kim, S. Effect of Autogenic Training for Stress Response: A Systematic Review and Meta-Analysis. J. Korean Acad. Nurs. 2019, 49, 361–374. [Google Scholar] [CrossRef]
- Isa, M.R.; Moy, F.M.; Razack, A.H.A.; Zainuddin, Z.; Zainal, N.Z. Impact of Applied Progressive Deep Muscle Relaxation Training on the Level of Depression, Anxiety and Stress among Prostate Cancer Patients: A Quasi-Experimental Study. Asian Pac. J. Cancer Prev. 2013, 14, 2237–2242. [Google Scholar] [CrossRef] [PubMed]
- Morton, M.L.; Helminen, E.C.; Felver, J.C. A Systematic Review of Mindfulness Interventions on Psychophysiological Responses to Acute Stress. Mindfulness 2020, 11, 2039–2054. [Google Scholar] [CrossRef]
- Kriakous, S.A.; Elliott, K.A.; Lamers, C.; Owen, R. The Effectiveness of Mindfulness-Based Stress Reduction on the Psychological Functioning of Healthcare Professionals: A Systematic Review. Mindfulness 2020. [Google Scholar] [CrossRef] [PubMed]
- Schuch, F.B.; Vancampfort, D.; Richards, J.; Rosenbaum, S.; Ward, P.B.; Stubbs, B. Exercise as a treatment for depression: A meta-analysis adjusting for 24 publication bias. J. Psychiatr. Res. 2016, 77, 42–51. [Google Scholar] [CrossRef] [PubMed]
- Borys, C.; Nodop, S.; Tutzschke, R.; Anders, C.; Scholle, H.C.; Strauss, B. [Evaluation of the German new back school. Pain-related and psychological characteristics]. Schmerz 2013, 27, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Kettunen, O.; Vuorimaa, T.; Vasankari, T. A 12-month exercise intervention decreased stress symptoms and increased mental resources among working adults—Results perceived after a 12-month follow-up. Int. J. Occup. Med. Environ. Health 2015, 28, 157–168. [Google Scholar] [CrossRef]
- Van Rhenen, W.; Blonk, R.W.; van der Klink, J.J.; van Dijk, F.J.; Schaufeli, W.B. The effect of a cognitive and a physical stress-reducing programme on psychological complaints. Int. Arch. Occup. Environ. Health 2005, 78, 139–148. [Google Scholar] [CrossRef]
- Stier-Jarmer, M.; Frisch, D.; Oberhauser, C.; Immich, G.; Kirschneck, M.; Schuh, A. Effects of single moor baths on physiological stress response and psychological state: A pilot study. Int. J. Biometeorol. 2017, 61, 1957–1964. [Google Scholar] [CrossRef]
- Brähler, E.; Mühlan, H.; Albani, C.; Schmidt, S. Teststatistische Prüfung und Normierung der deutschen Versionen des EUROHIS-QOL Lebensqualität-Index und des WHO-5 Wohlbefindens-Index. Diagnostica 2007, 53, 83–96. [Google Scholar] [CrossRef]
- Hagen, B.N.M.; Albright, A.; Sargeant, J.; Winder, C.B.; Harper, S.L.; O’Sullivan, T.L.; Jones-Bitton, A. Research trends in farmers’ mental health: A scoping review of mental heath outcomes and interventions among farming populations worldwide. PLoS ONE 2019, 14, e0225661. [Google Scholar] [CrossRef]
- Richardson, K.M.; Rothstein, H.R. Effects of occupational stress management intervention programs: A meta-analysis. J. Occup. Health Psychol. 2008, 13, 69–93. [Google Scholar] [CrossRef] [PubMed]
- Palpacuer, C.; Gallet, L.; Drapier, D.; Reymann, J.M.; Falissard, B.; Naudet, F. Specific and non-specific effects of psychotherapeutic interventions for depression: Results from a meta-analysis of 84 studies. J. Psychiatr. Res. 2017, 87, 95–104. [Google Scholar] [CrossRef] [PubMed]
- Cook, C. Mode of administration bias. J. Man. Manip. Ther. 2010, 18, 61–63. [Google Scholar] [CrossRef] [PubMed]
- Walter, U.; Plaumann, M.; Krugmann, C. Burnout Interventions. In Burnout for Experts-Prevention in the Context of Living and Working; Bährer-Kohler, S., Ed.; Springer Science+Business Media: New York, NY, USA, 2013; pp. 223–246. [Google Scholar]

| (1) Of Good and Bad Stress |
| Introduction to the stress concept, eustress/distress, stress consequences, burnout. Mindfulness exercise. |
| (2) Detect Your Own Stress Signals |
| Warning signals for stress, development of individual stress symptoms, personal experiences, and previous coping options. Mindfulness exercises. |
| (3) Conditions and Behavior |
| External stressors (conditions) and inner drivers (basics of one’s own behavior). Mindfulness exercises. |
| (4) Body and Stress |
| Hormones and neurobiology, physical sequelae, physical protective mechanisms, sport, and stress. Mindful walk. |
| (5) Personality and Stress |
| Inner drivers and rational alternatives, own stumbling blocks, performance, perfectionism, and demarcation. Mindfulness exercise. |
| (6) Goals and Values |
| “Higher, faster, further … “, the cake of importance, personal goals. Mindfulness exercise. |
| (7) Stress Management 1 |
| Basics: Sleep, regeneration, pleasure, biorhythm. Pleasure training. |
| (8) Stress Management 2 |
| Setting limits, task management, delegating. Role-play. |
| (9) Stress Management 3 |
| Leadership behavior, empathy and demarcation, cooperation, and responsibility. Role-play. |
| (10) I will change something |
| Transfer into everyday life: concrete definition of goals, points of change, time structure. Mindfulness exercise |
| Demographic and Clinical Characteristics | TC | noTC | Total |
|---|---|---|---|
| (n = 53) | (n = 55) | (n = 108) | |
| Age (years), M (SD) | 54.4 (7.6) | 56.1 (5.5) | 55.3 (6.7) |
| Female, n (%) | 25 (47.2%) | 28 (50.9%) | 53 (49.1%) |
| Marital status, n (%) | |||
| married/cohabiting | 48 (90.6%) | 50 (90.9%) | 98 (90.7%) |
| divorced/widowed | 2 (3.8%) | 4 (7.3%) | 6 (5.6%) |
| single | 3 (5.7%) | 1 (1.8%) | 4 (3.7%) |
| Highest educational level, n (%) | |||
| general secondary school certificate | 17 (32.1%) | 18 (32.7%) | 35 (32.4%) |
| intermediate secondary school certificate | 19 (35.9%) | 23 (41.8%) | 42 (38.9%) |
| qualification for university/universities of applied sciences entrance | 7 (13.2%) | 5 (9.1%) | 12 (11.1%) |
| university degree/universities of applied sciences degree | 8 (15.1%) | 6 (10.9%) | 14 (13.0%) |
| other | 2 (3.8%) | 3 (5.5%) | 5 (4.6%) |
| No days of sick leave (last 6 months), n (%) | 21 (41.2%) | 21 (38.2%) | 42 (39.6%) |
| Number of days of sick leave (last 6 months), M (SD), MD | 14.4 (22.9), 4.5 | 18.7 (29.0), 10 | 16.6 (26.2), 6 |
| PSQ, M (SD) | |||
| Worries | 47.4 (19.2) | 43.1 (17.5) | 45.2 (18.4) |
| Tension | 61.3 (18.1) | 58.4 (18.9) | 59.8 (18.5) |
| Joy | 42.6 (14.3) | 47.3 (19.4) | 45.0 (17.1) |
| Demands | 61.8 (18.3) | 59.8 (19.9) | 60.8 (19.1) |
| Total | 57.1 (13.3) | 53.5 (15.7) | 55.3 (14.6) |
| PSQ, n (%) | |||
| Stress level normal (≤45) | 10 (18.9%) | 18 (32.7%) | 28 (25.9%) |
| Stress level increased (46–59) | 20 (37.7%) | 15 (27.3%) | 35 (32.4%) |
| Stress level high (≥60) | 23 (43.4%) | 22 (40.0%) | 45 (41.7%) |
| ISI, M (SD) | |||
| Total | 12.1 (5.0) | 12.3 (6.0) | 12.2 (5.5) |
| ISI, n (%) | |||
| Absence of insomnia (<8 points) | 10 (18.9%) | 13 (23.6%) | 23 (21.3%) |
| Sub-threshold insomnia (8–14 points) | 25 (47.2%) | 25 (45.5%) | 50 (46.3%) |
| Moderate insomnia (15–21 points) | 18 (34.0%) | 12 (21.8%) | 30 (27.8%) |
| Severe insomnia (>21 points) | 0 (0.00%) | 5 (9.1%) | 5 (4.6%) |
| WHO-5, M (SD) | |||
| Total | 45.4 (18.7) | 44.6 (19.6) | 45.0 (19.1) |
| EQ-5D, M (SD) | |||
| Health Status | 67.1 (16.8) | 67.1 (15.6) | 67.1 (16.1) |
| EQ-5D, n (%) | |||
| Mobility. no problems | 35 (66.0%) | 34 (61.8%) | 69 (63.9%) |
| Self-care. no problems | 49 (92.5%) | 54 (98.2%) | 103 (95.4%) |
| Usual activities. no problems | 27 (50.9%) | 31 (57.4%) | 58 (54.2%) |
| Pain/discomfort. no problems | 3 (5.7%) | 5 (9.1%) | 8 (7.4%) |
| Anxiety/depression. no problems | 10 (18.9%) | 22 (40.0%) | 32 (29.6%) |
| MBI-EE, M (SD) | |||
| Emotional Exhaustion | 4.1 (0.8) | 4.1 (1.0) | 4.1 (0.9) |
| MBI-EE, n (%) | |||
| No burnout (<3.6 points) | 18 (34.0%) | 12 (21.8%) | 30 (27.8%) |
| Risk of burnout (3.6–5.0 points) | 29 (54.7%) | 33 (60.0%) | 62 (57.4%) |
| Symptoms of burnout (>5.0 points) | 6 (11.3%) | 10 (18.2%) | 16 (14.8%) |
| ASKU, M (SD) | |||
| Total | 3.6 (0.6) | 3.8 (0.6) | 3.7 (0.6) |
| PHQ-2, M (SD) | |||
| Total | 2.0 (1.3) | 2.0 (1.0) | 2.0 (1.1) |
| GAD-2, M (SD) | |||
| Total | 2.7 (1.6) | 2.3 (1.3) | 2.5 (1.5) |
| Pain frequency, n (%) | |||
| none/now and then | 19 (38.0%) | 16 (32.0%) | 35 (35.0%) |
| periodically/often/very often or permanently | 31 (62.0%) | 34 (68.0%) | 65 (65.0%) |
| Pain intensity, M (SD), MD | 3.5 (1.9), 3 | 4.3 (2.2), 4 | 3.9 (2.1), 4 |
| Pain-related limitations in everyday life, n (%) | |||
| Not at all | 4 (7.7%) | 6 (11.1%) | 10 (9.4%) |
| Somewhat | 18 (34.6%) | 14 (25.9%) | 32 (29.6%) |
| Moderate | 19 (36.5%) | 20 (37.0%) | 39 (36.8%) |
| Considerable | 10 (19.2%) | 12 (22.2%) | 22 (20.8%) |
| Severe | 1 (1.9%) | 2 (3.7%) | 3 (2.8%) |
| WAI, M (SD) | |||
| Total | 32.3 (5.9) | 31.5 (5.0) | 31.9 (5.5) |
| WAI current work ability, n (%) | |||
| Very good (>43 points) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Good (37–43 points) | 12 (24.0%) | 8 (15.4%) | 20 (19.6%) |
| Moderate (28–36 points) | 29 (58.0%) | 33 (63.5%) | 62 (60.8%) |
| Critical (<28 points) | 9 (18.0%) | 11 (21.2%) | 20 (19.6%) |
| Intervention Group (TC) | Control Group (noTC) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Change from Baseline | Change from Baseline | Change from Baseline—Difference between Groups | Effect Size | Between-Group ANCOVA d | ||||||
| N | M | SD | N | M | SD | M [95% CI] | Pooled SD | Cohen’s d | Parameter Estimate for Group [95% CI] | |
| PSQ-total (PP) | ||||||||||
| 1 month a | 49 | −19.06 | 14.32 | 51 | −16.06 | 12.62 | −3.00 [−8.36; 2.37] | 13.48 | −0.22 | −2.03 [−7.10; 3.03] |
| 6 months b | 48 | −13.27 | 12.19 | 50 | −11.57 | 15.85 | −1.70 [−7.37; 3.95] | 14.18 | −0.12 | −0.98 [−6.50; 4.55] |
| 9 months b | 49 | −13.38 | 14.98 | 50 | −11.09 | 14.15 | −2.29 [−8.10; 3.53] | 14.57 | −0.16 | −1.58 [−7.29; 4.13] |
| PSQ-total (ITT) | ||||||||||
| 1 month | 53 | −18.56 | 14.44 | 55 | −14.81 | 12.99 | −3.75 [−9.00; 1.50] | 13.72 | −0.27 | −3.00 [−7.99; 1.99] |
| 6 months | 53 | −12.54 | 11.91 | 55 | −10.55 | 15.53 | −1.99 [−7.26; 3.28] | 13.87 | −0.14 | −1.09 [−6.47; 4.29] |
| 9 months | 53 | −13.63 | 15.04 | 55 | −10.33 | 13.74 | −3.30 [−8.80; 2.21] | 14.39 | −0.23 | −2.43 [−8.01; 3.15] |
| ISI (PP) | ||||||||||
| 1 month a | 51 | −5.41 | 4.56 | 53 | −4.20 | 4.78 | −1.21 [−3.03; 0.60] | 4.67 | −0.26 | −1.38 [−2.94; 0.18] |
| 6 months b | 50 | −3.81 | 5.27 | 52 | −4.53 | 5.24 | 0.72 [−1.34; 2.79] | 5.25 | 0.14 | 0.49 [−1.32; 2.30] |
| 9 months b | 51 | −2.97 | 4.84 | 52 | −4.05 | 5.15 | 1.08 [−0.87; 3.04] | 5.00 | 0.22 | 0.88 [−0.88; 2.64] |
| WHO-5 (PP) | ||||||||||
| 1 month a | 51 | 20.00 | 21.67 | 53 | 18.94 | 18.63 | 1.06 [−6.82; 8.93] | 20.18 | 0.05 | 1.44 [−5.35; 8.23] |
| 6 months b | 51 | 11.45 | 18.63 | 52 | 15.77 | 19.97 | −4.32 [−11.86; 3.23] | 19.32 | −0.22 | −3.75 [−10.41; 2.91] |
| 9 months b | 51 | 11.69 | 17.74 | 52 | 12.77 | 18.98 | −1.08 [−8.26; 6.10] | 18.38 | −0.06 | −0.74 [−7.61; 6.14] |
| EQ5D Health Status (PP) | ||||||||||
| 1 month a | 51 | 10.76 | 16.52 | 51 | 11.88 | 14.24 | −1.12 [−7.18; 4.94] | 15.42 | −0.07 | −1.30 [−6.48; 3.88] |
| 6 months b | 51 | 11.24 | 14.95 | 51 | 9.37 | 14.82 | 1.87 [−3.99; 7.71] | 14.89 | 0.13 | 2.13 [−2.80; 7.05] |
| 9 months b | 51 | 7.90 | 15.25 | 51 | 9.04 | 15.25 | −1.14 [−7.13; 4.86] | 15.25 | −0.07 | −0.86 [−5.90; 4.17] |
| MBI-EE (PP) | ||||||||||
| 1 month a | 51 | −0.64 | 0.80 | 53 | −0.69 | 0.89 | 0.05 [−0.29; 0.37] | 0.85 | 0.06 | 0.03 [−0.27; 0.34] |
| 6 months b | 51 | −0.56 | 0.84 | 51 | −0.49 | 1.00 | −0.07 [−0.43; 0.29] | 0.92 | −0.08 | −0.08 [−0.42; 0.26] |
| 9 months b | 51 | −0.51 | 0.80 | 52 | −0.57 | 0.84 | 0.06 [−0.26; 0.38] | 0.82 | 0.07 | 0.06 [−0.25; 0.37] |
| ASKU (PP) | ||||||||||
| 1 month a | 50 | 0.17 | 0.61 | 53 | 0.26 | 0.56 | −0.09 [−0.31; 0.14] | 0.58 | −0.16 | −0.22 [−0.41; −0.03] |
| 6 months b | 50 | 0.27 | 0.57 | 51 | 0.24 | 0.55 | 0.03 [−0.19; 0.25] | 0.56 | 0.05 | −0.07 [−0.26; 0.12] |
| 9 months b | 50 | 0.23 | 0.66 | 52 | 0.22 | 0.50 | 0.01 [−0.22; 0.24] | 0.58 | 0.02 | −0.08 [−0.28; 0.13] |
| PHQ-2 (PP) | ||||||||||
| 1 month a | 51 | −0.67 | 1.18 | 53 | −0.70 | 0.99 | 0.03 [−0.39; 0.46] | 1.09 | 0.03 | 0.05 [−0.33; 0.42] |
| 6 months b | 51 | −0.29 | 1.17 | 52 | −0.40 | 1.27 | 0.11 [−0.37; 0.59] | 1.22 | 0.09 | 0.09 [−0.33; 0.50] |
| 9 months b | 51 | −0.41 | 1.06 | 52 | −0.48 | 1.16 | 0.07 [−0.37; 0.50] | 1.11 | 0.06 | 0.05 [−0.34; 0.44] |
| GAD-2 (PP) | ||||||||||
| 1 month a | 51 | −1.08 | 1.43 | 52 | −0.94 | 1.38 | −0.14 [−0.68; 0.41] | 1.40 | −0.10 | 0.08 [−0.38; 0.55] |
| 6 months b | 51 | −0.84 | 1.51 | 51 | −0.84 | 1.41 | 0.00 [−0.57; 0.57] | 1.46 | 0.00 | 0.22 [−0.25; 0.68] |
| 9 months b | 50 | −1.02 | 1.45 | 51 | −0.80 | 1.34 | −0.22 [−0.77; 0.34] | 1.40 | −0.16 | −0.00 [−0.44; 0.42] |
| WAI (PP) c | ||||||||||
| 9 months b | 48 | 2.66 | 4.17 | 50 | 3.29 | 4.50 | −0.63 [−2.37; 1.11] | 4.34 | −0.15 | −0.45 [−2.19; 1.28] |
| Group | Change from Baseline | Paired t-Test | Effect Size | ||||
|---|---|---|---|---|---|---|---|
| N | M | SD | [95% CI] | p-Value | Cohen’s d | ||
| PSQ-Total | Total | 99 | −12.22 | 14.54 | [−5.71; −3.88] | <0.0001 | 0.84 |
| TC | 49 | −13.38 | 14.98 | [−17.68; −9.07] | <0.0001 | 0.89 | |
| noTC | 50 | −11.09 | 14.15 | [−15.11; −7.07] | <0.0001 | 0.78 | |
| ISI | Total | 103 | −3.52 | 5.00 | [−4.50; −2.54] | <0.0001 | 0.70 |
| TC | 51 | −2.97 | 4.84 | [−4.33; −1.61] | 0.0001 | 0.61 | |
| noTC | 52 | −4.05 | 5.15 | [−5.49; −2.62] | <0.0001 | 0.79 | |
| WHO-5 | Total | 103 | 12.23 | 18.29 | [8.66; 15.81] | <0.0001 | 0.67 |
| TC | 51 | 11.69 | 17.74 | [6.70; 16.68] | <0.0001 | 0.66 | |
| noTC | 52 | 12.77 | 18.98 | [7.49; 18.05] | <0.0001 | 0.67 | |
| EQ5D Health Status | Total | 102 | 8.47 | 15.19 | [5.49; 11.45] | 0.0005 | 0.56 |
| TC | 51 | 7.90 | 15.25 | [3.61; 12.19] | <0.0010 | 0.52 | |
| noTC | 51 | 9.04 | 15.25 | [4.75; 13.33] | 0.0001 | 0.59 | |
| MBI-EE | Total | 103 | −0.54 | 0.82 | [−0.70; −0.38] | <0.0001 | 0.66 |
| TC | 51 | −0.51 | 0.80 | [−0.74; −0.29] | <0.0001 | 0.64 | |
| noTC | 52 | −0.57 | 0.84 | [−0.81; −0.34] | <0.0001 | 0.68 | |
| ASKU | Total | 102 | 0.23 | 0.58 | [0.11; 0.34] | 0.0001 | 0.40 |
| TC | 50 | 0.23 | 0.66 | [0.04; 0.42] | 0.0164 | 0.35 | |
| noTC | 52 | 0.22 | 0.50 | [0.09; 0.36] | 0.0020 | 0.44 | |
| PHQ-2 | Total | 103 | −0.45 | 1.11 | [−0.66; −0.23] | 0.0001 | 0.41 |
| TC | 51 | −0.41 | 1.06 | [−0.71; −0.11] | 0.0078 | 0.39 | |
| noTC | 52 | −0.48 | 1.16 | [−0.80; −0.16] | 0.0044 | 0.41 | |
| GAD-2 | Total | 101 | −0.91 | 1.39 | [−1.19; −0.64] | <0.0001 | 0.66 |
| TC | 50 | −1.02 | 1.45 | [−1.43; −0.61] | <0.0001 | 0.70 | |
| noTC | 51 | −0.80 | 1.34 | [−1.18; −0.43] | 0.0001 | 0.60 | |
| WAI | Total | 98 | 2.98 | 4.33 | [2.11; 3.85] | <0.0001 | 0.69 |
| TC | 48 | 2.66 | 4.17 | [1.44; 3.87] | 0.0001 | 0.64 | |
| noTC | 50 | 3.29 | 4.50 | [2.01; 4.57] | <0.0001 | 0.73 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stier-Jarmer, M.; Oberhauser, C.; Frisch, D.; Berberich, G.; Loew, T.; Schels-Klemens, C.; Braun, B.; Schuh, A. A Multimodal Stress-Prevention Program Supplemented by Telephone-Coaching Sessions to Reduce Perceived Stress among German Farmers: Results from a Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 9227. https://doi.org/10.3390/ijerph17249227
Stier-Jarmer M, Oberhauser C, Frisch D, Berberich G, Loew T, Schels-Klemens C, Braun B, Schuh A. A Multimodal Stress-Prevention Program Supplemented by Telephone-Coaching Sessions to Reduce Perceived Stress among German Farmers: Results from a Randomized Controlled Trial. International Journal of Environmental Research and Public Health. 2020; 17(24):9227. https://doi.org/10.3390/ijerph17249227
Chicago/Turabian StyleStier-Jarmer, Marita, Cornelia Oberhauser, Dieter Frisch, Götz Berberich, Thomas Loew, Carina Schels-Klemens, Birgit Braun, and Angela Schuh. 2020. "A Multimodal Stress-Prevention Program Supplemented by Telephone-Coaching Sessions to Reduce Perceived Stress among German Farmers: Results from a Randomized Controlled Trial" International Journal of Environmental Research and Public Health 17, no. 24: 9227. https://doi.org/10.3390/ijerph17249227
APA StyleStier-Jarmer, M., Oberhauser, C., Frisch, D., Berberich, G., Loew, T., Schels-Klemens, C., Braun, B., & Schuh, A. (2020). A Multimodal Stress-Prevention Program Supplemented by Telephone-Coaching Sessions to Reduce Perceived Stress among German Farmers: Results from a Randomized Controlled Trial. International Journal of Environmental Research and Public Health, 17(24), 9227. https://doi.org/10.3390/ijerph17249227




