Factorial Validity and Variance of the Maslach Burnout Inventory between Demographic and Workload Groups among Dentists of Lithuania
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Size Calculation
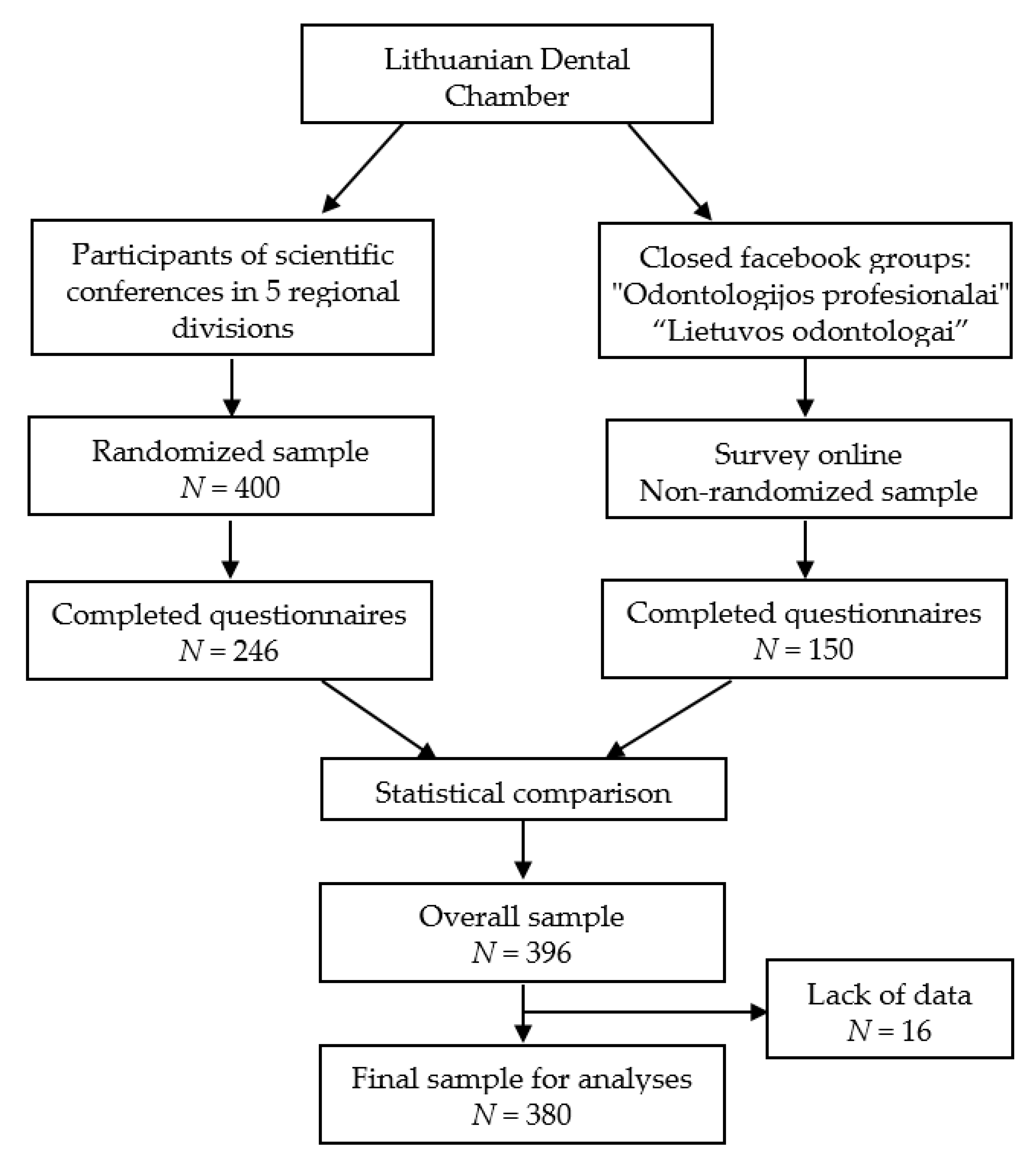
2.2. Study Design, Participants and Data Collection
2.3. Burnout Measure
2.4. Statistical Analysis
2.5. Ethical Statement
3. Results
3.1. Sample Characteristics
3.2. Descriptive Characteristics of the Maslach Burnout Inventory
3.3. Psychometric Characteristics
3.4. Exploratory Factor Analysis
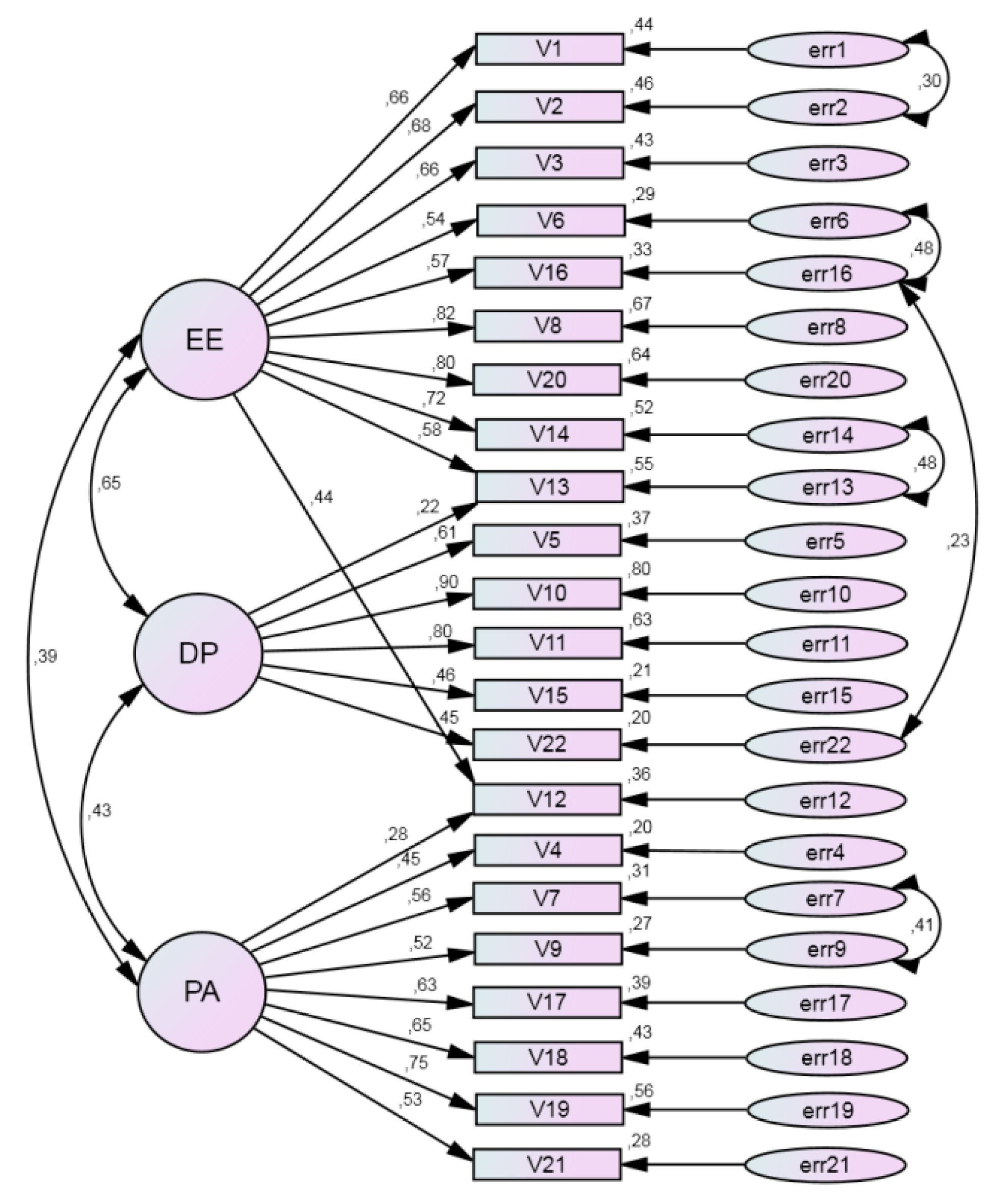
3.5. Confirmatory Factor Analysis
3.6. Multiple-Group Analysis of Invariance
3.7. Multiple-Group Analysis of Factor Means
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CFA | Confirmatory factor analysis |
| CFI | Comparative fit index |
| CI | Confidence interval |
| DP | Depersonalization |
| EE | Emotional exhaustion |
| EFA | Exploratory factor analysis |
| IFI | Bollen’s incremental fit index |
| KMO | Kaiser-Meyer-Olkin measure |
| MBI | Maslach Burnout Inventory |
| PA | Personal accomplishment |
| RMSEA | Root mean square error of approximation |
| SD | Standard deviation |
| TLI | Tucker–Lewis index |
References
- Maslach, C.; Leiter, M.P. Understanding the burnout experience: Recent research and its implications for psychiatry. World Psychiatry 2016, 15, 103–111. [Google Scholar] [CrossRef] [PubMed]
- West, C.P.; Dyrbye, L.N.; Shanafelt, T.D. Physician burnout: Contributors, consequences and solutions. J. Intern. Med. 2018, 283, 516–529. [Google Scholar] [CrossRef] [PubMed]
- Roland-Lévy, C.; Lemoine, J.; Jeoffrion, C. Health and well-being at work: The hospital context. Eur. Rev. Appl. Psychol. 2014, 64, 53–62. [Google Scholar] [CrossRef][Green Version]
- Maslach, C.; Schaufeli, W.B.; Leiter, M.P. Job burnout. Annu. Rev. Psychol. 2001, 52, 397–422. [Google Scholar] [CrossRef]
- Schaufeli, W.B.; Leiter, M.P.; Maslach, C. Burnout: 35 years of research and practice. Career Dev. Int. 2009, 14, 204–220. [Google Scholar] [CrossRef]
- Leiter, M.P.; Maslach, C. Latent burnout profiles: A new approach to understanding the burnout experience. Burn. Res. 2016, 3, 89–100. [Google Scholar] [CrossRef]
- Stewart, M.T.; Reed, S.; Reese, J.; Galligan, M.M.; Mahan, J.D. Conceptual models for understanding physician burnout, professional fulfillment, and well-being. Curr. Probl. Pediatr. Adolesc. Health Care 2019, 49, 100658. [Google Scholar] [CrossRef]
- Zhang, X.J.; Song, Y.; Jiang, T.; Ding, N.; Shi, T.Y. Interventions to reduce burnout of physicians and nurses: An overview of systematic reviews and meta-analyses. Med. Baltim. 2020, 26, e20992. [Google Scholar] [CrossRef]
- Grow, H.M.; McPhillips, H.A.; Batra, M. Understanding physician burnout. Curr. Probl. Pediatr. Adolesc. Health Care 2019, 49, 100656. [Google Scholar] [CrossRef]
- Reith, T.P. Burnout in United States Healthcare Professionals: A Narrative Review. Cureus 2018, 10, e3681. [Google Scholar] [CrossRef]
- Rotenstein, L.S.; Torre, M.; Ramos, M.A.; Rosales, R.C.; Guille, C.; Sen, S.; Mata, D.A. Prevalence of burnout among physicians: A systematic review. JAMA 2018, 320, 1131–1150. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E. The measurement of experienced burnout. J. Occup. Behav. 1981, 2, 99–113. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.; Leiter, M. The Maslach Burnout Inventory Manual, 4th ed.; Ming Garden, Inc.: Menio Park, CA, USA, 2016. [Google Scholar]
- Žutautienė, R.; Radišauskas, R.; Kalinienė, G.; Ustinavičienė, R. The prevalence of burnout and its associations with psychosocial work environment among Kaunas region (Lithuania) hospitals’ physicians. Int. J. Environ. Res. Public Health 2020, 17, 3739. [Google Scholar] [CrossRef] [PubMed]
- Skorobogatova, N.; Žemaitienė, N.; Šmigelskas, K.; Tamelienė, R. Professional burnout and concurrent health complaints in neonatal nursing. Open Med. 2017, 12, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Mikalauskas, A.; Benetis, R.; Širvinskas, E.; Andrejaitienė, J.; Kinduris, Š.; Macas, A.; Padaiga, Ž. Burnout among anesthetists and intensive care physicians. Open Med. 2018, 13, 105–112. [Google Scholar] [CrossRef]
- Eriksonas, L. Lithuania socialbriefing: Lithuania tightens the regulation of dentists through the legislation changes on state-controlled licensing. China-CEE Inst. 2020, 26, 1–5. Available online: https://china-cee.eu/wp-content/uploads/2020/04/2020s02Lithuania.pdf (accessed on 20 October 2020).
- Deshmukh, S.V. Burnout in dentistry: A myth or reality. J. Int. Clin. Dent. Res. Organ. 2019, 11, 1–2. [Google Scholar] [CrossRef]
- Puriene, A.; Janulyte, V.; Musteikyte, M.; Bendinskaite, R. General health of dentists. Lit. Rev. Stomatol. 2007, 9, 10–20. [Google Scholar]
- Toon, M.; Collin, V.; Whitehead, P.; Reynold, L. An analysis of stress and burnout. Br. Dent. J. 2019, 226, 125–130. [Google Scholar] [CrossRef]
- Singh, P.; Aulak, D.S.; Mangat, S.S.; Aulak, M.S. Systematic review: Factors contributing to burnout in dentistry. Occup. Med. Lond. 2016, 66, 27–31. [Google Scholar] [CrossRef]
- Zini, A.; Zaken, Y.; Ovadia-Gonen, H.; Mann, J.; Vered, Y. Burnout Level among General and Specialist Dentists: A Global Manpower Concern. Occup. Med. Health Aff. 2013, 1, 5. [Google Scholar]
- Vered, Y.; Zaken, Y.; Ovadia-Gonen, H.; Mann, J.; Zini, A. Professional burnout: Its relevance and implications for the general dental community. Quintessence Int. 2014, 45, 87–90. [Google Scholar] [PubMed]
- Gorter, R.C. Burnout among Dentists: Identification and Prevention. Doctorial Thesis, University of Amsterdam, Amsterdam, The Netherlands, 2000. [Google Scholar]
- Hallberg, U.E.; Sverke, M. Construct validity of the Maslach Burnout Inventory: Two Swedish health care samples. Eur. J. Psychol. Assess. 2004, 20, 320–338. [Google Scholar] [CrossRef]
- Poghosyan, L.; Aiken, L.H.; Sloane, D.M. Factor structure of the Maslach burnout inventory: An analysis of data from large scale cross-sectional surveys of nurses from eight countries. Int. J. Nurs. Stud. 2009, 46, 894–902. [Google Scholar] [CrossRef] [PubMed]
- Jin, M.U.; Jeong, S.H.; Kim, E.K.; Choi, Y.H.; Song, K.B. Burnout and its related factors in Korean dentists. Int. Dent. J. 2015, 65, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Kalliath, T.J.; O’Driscoll, M.P.; Gillespie, D.F.; Bluedorn, A.C. A test of the Maslach Burnout Inventory in three samples of healthcare professionals. Work Stress 2000, 14, 35–50. [Google Scholar] [CrossRef]
- De Beer, L.T.; Bianchi, R. Confirmatory factor analysis of the Maslach. burnout Inventory. Eur. J. Psychol. Assess. 2019, 35, 217–224. [Google Scholar] [CrossRef]
- Dwivedi, A.; Purohit, B.M.; Bhambal, A. Is Dentistry Turning into Weary Profession? Dimensionality of Experienced Professional Burnout among Dentists in Central India. J. Dent. Oral Surg. 2016, 1, 1–4. [Google Scholar] [CrossRef]
- Densten, I.L. Re-thinking burnout. J. Organ. Behav. 2001, 22, 833–847. [Google Scholar] [CrossRef]
- Sakakibara, K.; Shimazu, A.; Toyama, H.; Schaufeli, W.B. Validation of the Japanese Version of the Burnout Assessment Tool. Front. Psychol. 2020, 11, 1819. [Google Scholar] [CrossRef]
- Croucher, R.; Osborne, D.; Marcenes, W.; Sheiham, A. Burnout and issues of the work environment reported by general dental practitioners in the United Kingdom. Community Dent. Health 1998, 15, 40–43. [Google Scholar] [PubMed]
- Bria, M.; Spânua, F.; Băbana, A.; Dumitraşcu, D.L. Maslach Burnout Inventory–General Survey: Factorial validity and invariance among Romanian healthcare professionals. Burn. Res. 2014, 1, 103–111. [Google Scholar] [CrossRef]
- Pakalniškienė, V. Tyrimo ir Įvertinimo Priemonių Patikimumo ir Validumo Nustatymas. Metodinė Priemonė. (Evaluation of Reliability and Validity of Research Instruments); Vilniaus Universiteto Leidykla: Vilnius, Lithuania, 2012. [Google Scholar]
- COSMIN. Find the COSMIN Tool to Help You Select the Best Outcome Measure. Website of Amsterdam Public Health. Available online: https://www.cosmin.nl/cosmin-tools/ (accessed on 28 November 2020).
- Gil-Monte, P.R. Factorial validity of the Maslach Burnout Inventory (MBI-HSS) among Spanish professionals. Rev. Saúde Pública 2005, 39, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Tsang, S.; Royse, C.F.; Terkawi, A.S. Guidelines for developing, translating, and validating a questionnaire in perioperative and pain medicine. Saudi. J. Anaesth. 2017, 11, S80–S89. [Google Scholar] [CrossRef]
- Arbuckle, J.L. IBM SPSS AMOS 21 User’s Guide; Amos Development Corporation: Chicago, IL, USA, 2012. [Google Scholar]
- Hair, J.F.J.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis, 7th ed.; Pearson Prentice Hall: Upper Saddle River, NJ, USA, 2009. [Google Scholar]
- Albright, J.J.; Park, H.M. Confirmatory Factor Analysis Using AMOS, LISREL, Mplus, SAS/STAT CALIS; Indiana University: Bloomington, Indiana, 2006–2009; Available online: https://fliphtml5.com/wjxe/uqzh/basic (accessed on 20 October 2020).
- Byrne, B.M. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming, 2nd ed.; Routledge: New York, NY, USA, 2010. [Google Scholar]
- Schmitt, T.A. Current methodological considerations in exploratory and confirmatory factor analysis. J. Psychoeduc. Ass. 2011, 29, 304–321. [Google Scholar] [CrossRef]
- Peters, G.-J.Y. The alpha and the omega of scale reliability and validity. Why and how to abandon Cronbach’s alpha and the route towards more comprehensive assessment of scale quality. Eur. Health Psychol. 2014, 16, 56–69. [Google Scholar]
- Vanheule, S.; Rosseel, Y.; Vlerick, P. The factorial validity and measurement invariance of the Maslach Burnout Inventory for human services. Stress Health 2007, 23, 87–91. [Google Scholar] [CrossRef]
- Gorter, R.C.; Albrecht, G.; Hoogstraten, J.; Eijkman, M.A.J. Factorial validity of the Maslach Burnout Inventory–Dutch version (MBI-NL) among dentists. J. Organ. Behav. 1999, 20, 209–217. [Google Scholar] [CrossRef]
- Alves da Silva, R.A.D.; Macedo Teixeira, A.K.; Arcanjo Frota, M.M.; Cavalcante Maciel, J.A.; Ramalho de Farias, M. Job satisfaction and burnout among oral healthcare providers within the Unified Health System in Sobral, Ceará, Brazil. Rev. Bras. Med. Trab. 2020, 17, 313–324. [Google Scholar]
- Choy, H.B.; Wong, M.C. Occupational stress and burnout among Hong Kong dentists. Hong Kong Med. J. 2017, 23, 480–488. [Google Scholar] [CrossRef]
- Kravitz, A.S.; Bullock, A.; Cowpe, J.C.; Barnes, E. EU Manual of Dental Practice 2015 Lithuania, 5th ed.; Cardiff University and the Council of European Dentists: Wales, UK, 2015; Available online: https://cedentists.eu/library/eu-manual.html (accessed on 28 November 2020).
- Jugale, P.V.; Mallaiah, P.; Krishnamurthy, A.; Sangha, R. Burnout and work engagement among dental practitioners in Bangalore city: A cross-sectional study. J. Clin. Diagn. Res. 2016, 10, ZC63–ZC67. [Google Scholar] [CrossRef] [PubMed]
- Puriene, A.; Aleksejuniene, J.; Petrauskiene, J.; Balciuniene, I.; Janulyte, V. Self-perceived mental health and job satisfaction among Lithuanian dentists. Ind. Health 2008, 46, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Te Brake, H.J.H.M. Burnout and Job Engagement in Dentistry. Ph.D. Thesis, University of Amsterdam, Amsterdam, The Netherlands, 2005. [Google Scholar]
- Gorter, R.C.; Freeman, R. Burnout and engagement in relation with job demands and resources among dental staff in Northern Ireland. Community Dent. Oral Epidemiol. 2011, 39, 87–95. [Google Scholar] [CrossRef] [PubMed]
- Humphris, G.; Lilley, J.; Kaney, S.; Broomfield, D. Burnout and stress-related factors among junior staff of three dental hospital specialties. Br. Dent. J. 1997, 183, 15–21. [Google Scholar] [CrossRef]
- Collin, V.; Toon, M.; O’Selmo, E.; Reynolds, L.; Whitehead, P. A survey of stress, burnout and well-being in UK dentists. Br. Dent. J. 2019, 226, 40–49. [Google Scholar] [CrossRef]
- Alqahtani, N.D.; Aljajji, S.; Alshalan, N.; Aljabaa, A.; Aldosari, M.; Albarakati, S. Occupational Stress among Orthodontists in Saudi Arabia. J. Int. Soc. Prev. Community Dent. 2020, 10, 350–358. [Google Scholar] [CrossRef]
- Gorter, R.C.; Te Brake, H.J.; Hoogstraten, J.; Eijkman, M.A. Positive engagement and job resources in dental practice. Community Dent. Oral Epidemiol. 2008, 36, 47–54. [Google Scholar] [CrossRef]
- Gorter, R.C.; Eijkman, M.A.; Hoogstraten, J. A career counselling program for dentists: Effects on burnout. Patient Educ. Couns. 2001, 43, 23–30. [Google Scholar] [CrossRef]
| Characteristics | Number (n)/Mean | Percentage (%)/Standard Deviation |
|---|---|---|
| Gender: | ||
| Male | 58 | 15.3 |
| Female | 322 | 84.7 |
| Age (years): | ||
| Mean and standard deviation | 37.3 | 12.9 |
| Up to 30 | 151 | 39.7 |
| 30 or more | 229 | 60.3 |
| Work practice experience (years): | ||
| Mean and standard deviation | 12.8 | 12.3 |
| Up to 10 years | 204 | 53.7 |
| 10 or more years | 176 | 46.3 |
| Staffing: | ||
| Half-time | 263 | 69.3 |
| Full-time | 117 | 30.7 |
| Working in several places: | ||
| In one clinic only | 187 | 49.2 |
| In two or more clinics | 193 | 50.8 |
| Specialty: | ||
| Dentists in general practice | 278 | 73.3 |
| Oral surgeons | 19 | 5.1 |
| Prosthodontists | 13 | 3.4 |
| Orthodontists | 13 | 3.4 |
| Poedodontists | 20 | 5.3 |
| Endodontists | 23 | 6.1 |
| Periodontists | 13 | 3.4 |
| Item | Percentage Distribution On Seven-Point Likert Scale | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Never | A Few Times a Year | Once Time a Month | A Few Times a Month | Once Time a Week | A Few Times a Week | Every Day | |||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | ||
| V1 | I feel emotionally drained from my work | 9 | 2.4 | 43 | 11.3 | 51 | 13.4 | 73 | 19.2 | 58 | 15.3 | 109 | 28.7 | 37 | 9.7 |
| V2 | I feel used up at the end of the workday | 4 | 1.1 | 22 | 5.8 | 56 | 14.7 | 50 | 13.2 | 72 | 18.9 | 120 | 31.6 | 56 | 14.7 |
| V3 | I feel fatigued when I get up in the morning and have to face another day on the job | 44 | 11.6 | 63 | 16.6 | 59 | 15.5 | 65 | 17.1 | 53 | 13.9 | 67 | 17.6 | 29 | 7.6 |
| V4 ^ | I can easily understand how my patients feel about things | 4 | 1.1 | 4 | 1.1 | 10 | 2.6 | 19 | 5.0 | 35 | 9.2 | 87 | 22.9 | 221 | 58.2 |
| V5 | I feel I treat some patients as if they were impersonal objects | 198 | 52.1 | 53 | 13.9 | 40 | 10.5 | 31 | 8.2 | 31 | 8.2 | 22 | 5.8 | 5 | 1.3 |
| V6 | Working with people all say is really a strain for me | 26 | 6.8 | 53 | 13.9 | 57 | 15.0 | 60 | 15.8 | 51 | 13.4 | 71 | 18.7 | 62 | 16.3 |
| V7 ^ | I deal very effectively with the problems of my patients | 3 | 0.8 | 4 | 1.1 | 17 | 4.5 | 34 | 8.9 | 47 | 12.4 | 130 | 34.2 | 145 | 38.2 |
| V8 | I feel burned out from my work | 56 | 14.7 | 78 | 20.5 | 57 | 15.0 | 66 | 17.4 | 53 | 13.9 | 43 | 11.3 | 27 | 7.1 |
| V9 ^ | I feel I’m positively influencing other people’s lives though my work | 6 | 1.6 | 6 | 1.6 | 14 | 3.7 | 19 | 5.0 | 39 | 10.3 | 101 | 26.6 | 195 | 51.3 |
| V10 | I’ve become more callous toward people since I took this job | 165 | 43.4 | 70 | 18.4 | 37 | 9.7 | 40 | 10.5 | 31 | 8.2 | 21 | 5.5 | 16 | 4.2 |
| V11 | I worry that this job is hardening me emotionally | 93 | 24.5 | 77 | 20.3 | 64 | 16.8 | 56 | 14.7 | 32 | 8.4 | 33 | 8.7 | 25 | 6.6 |
| V12 ^ | I feel very energetic | 24 | 6.3 | 33 | 8.7 | 60 | 15.8 | 77 | 20.3 | 53 | 13.9 | 81 | 21.3 | 52 | 13.7 |
| V13 | I feel frustrated by my job | 115 | 30.3 | 98 | 25.8 | 61 | 16.1 | 56 | 14.7 | 22 | 5.8 | 17 | 4.5 | 11 | 2.9 |
| V14 | I feel I’m working too hard on my job | 118 | 31.1 | 116 | 30.5 | 57 | 15.0 | 45 | 11.8 | 19 | 5.0 | 14 | 3.7 | 11 | 2.9 |
| V15 | I don’t really care what happens to some patients | 253 | 66.6 | 61 | 16.1 | 17 | 4.5 | 13 | 3.4 | 17 | 4.5 | 6 | 1.6 | 13 | 3.4 |
| V16 | Working with people directly puts too much stress on me | 39 | 10.3 | 78 | 20.5 | 80 | 21.1 | 51 | 13.4 | 46 | 12.1 | 48 | 12.6 | 38 | 10.0 |
| V17 ^ | I can easily create a relax atmosphere with my patients | 9 | 2.4 | 3 | 0.8 | 17 | 4.5 | 33 | 8.7 | 45 | 11.8 | 101 | 26.6 | 172 | 45.3 |
| V18 ^ | I feel exhilarated after working closely with my patients | 10 | 2.6 | 15 | 3.9 | 48 | 12.6 | 67 | 17.6 | 75 | 19.7 | 106 | 27.9 | 59 | 15.5 |
| V19 ^ | I have accomplished many worthwhile things in this job | 7 | 1.8 | 14 | 3.7 | 31 | 8.2 | 44 | 11.6 | 41 | 10.8 | 100 | 26.3 | 143 | 37.6 |
| V20 | I feel that this job is hardening me emotionally | 85 | 22.4 | 110 | 28.9 | 49 | 12.9 | 53 | 13.9 | 44 | 11.6 | 25 | 6.6 | 14 | 3.7 |
| V21 ^ | In my work I deal with emotional problems very calmly | 18 | 4.7 | 41 | 10.8 | 51 | 13.4 | 70 | 18.4 | 57 | 15.0 | 71 | 18.7 | 72 | 18.9 |
| V22 | I feel patients blame me for some of their problems | 57 | 15.0 | 130 | 34.2 | 71 | 18.7 | 55 | 14.5 | 33 | 8.7 | 21 | 5.5 | 13 | 3.4 |
| Subscale in the Original Version [12] | Item b | Four-Factor Model c | Three-Factor Model c | ||||||
|---|---|---|---|---|---|---|---|---|---|
| F1 | F2 | F3 | F4 | F1 | F2 | F3 | |||
| Standardized factor loadings | |||||||||
| EE | V20 | I feel that this job is hardening me emotionally | 0.786 | 0.797 | |||||
| EE | V2 | I feel used up at the end of the workday | 0.780 | 0.805 | |||||
| EE | V1 | I feel emotionally drained from my work | 0.771 | 0.782 | |||||
| EE | V8 | I feel burned out from my work | 0.759 | 0.772 | |||||
| EE | V6 | Working with people all say is really a strain for me | 0.747 | 0.740 | |||||
| EE | V16 | Working with people directly puts too much stress on me | 0.745 | 0.720 | |||||
| EE | V3 | I feel fatigued when I get up in the morning and have to face another day on the job | 0.737 | 0.753 | |||||
| EE | V14 | I feel I’m working too hard on my job | 0.663 | 0.513 | 0.642 | ||||
| EE | V13 | I feel frustrated by my job | 0.662 | 0.552 | 0.654 | 0.604 | |||
| PA | V12 | I feel very energetic | 0.608 | 0.520 | 0.590 | 0.529 | |||
| PA | V7 | I deal very effectively with the problems of my patients | 0.717 | 0.710 | |||||
| PA | V19 | I have accomplished many worthwhile things in this job | 0.713 | 0.720 | |||||
| PA | V9 | I feel I’m positively influencing other people’s lives though my work | 0.683 | 0.682 | |||||
| PA | V17 | I can easily create a relax atmosphere with my patients | 0.672 | 0.682 | |||||
| PA | V4 | I can easily understand how my patients feel about things | 0.624 | 0.626 | |||||
| PA | V18 | I feel exhilarated after working closely with my patients | 0.605 | 0.602 | |||||
| PA | V21 | In my work I deal with emotional problems very calmly | 0.511 | 0.504 | |||||
| DP | V10 | I’ve become more callous toward people since I took this job | 0.783 | 0.520 | 0.684 | ||||
| DP | V5 | I feel I treat some patients as if they were impersonal objects | 0.696 | 0.568 | |||||
| DP | V11 | I worry that this job is hardening me emotionally | 0.684 | 0.535 | 0.526 | ||||
| DP | V22 | I feel patients blame me for some of their problems | 0.715 | 0.581 | |||||
| DP | V15 | I don’t really care what happens to some patients | 0.671 | 0.601 | |||||
| Percentage of variances explained | 31.10 | 13.84 | 6.06 | 5.44 | 31.10 | 13.84 | 6.06 | ||
| Cronbach’s α | 0.905 | 0.775 | 0.784 | 0.373 | 0.905 | 0.775 | 0.653 | ||
| Model That Directly Replicated the EFA Results | Revised (Final) Model | |||
|---|---|---|---|---|
| Estimate | p | Estimate | p | |
| Standardized Regression Weights (Factor Loadings): | ||||
| V1 ← EE | 0.68 | <0.001 | 0.66 | <0.001 |
| V2 ← EE | 0.69 | <0.001 | 0.68 | <0.001 |
| V3 ← EE | 0.65 | <0.001 | 0.66 | <0.001 |
| V6 ← EE | 0.58 | <0.001 | 0.54 | <0.001 |
| V8 ← EE | 0.80 | <0.001 | 0.82 | <0.001 |
| V14 ← EE | 0.75 | <0.001 | 0.72 | <0.001 |
| V16 ← EE | 0.63 | <0.001 | 0.57 | <0.001 |
| V20 ← EE | 0.77 | <0.001 | 0.80 | <0.001 |
| V4 ← PA | 0.47 | <0.001 | 0.45 | <0.001 |
| V7 ← PA | 0.64 | <0.001 | 0.56 | <0.001 |
| V9 ← PA | 0.60 | <0.001 | 0.52 | <0.001 |
| V17 ← PA | 0.65 | <0.001 | 0.63 | <0.001 |
| V18 ← PA | 0.62 | <0.001 | 0.66 | <0.001 |
| V21 ← PA | 0.50 | <0.001 | 0.53 | <0.001 |
| V19 ← PA | 0.71 | <0.001 | 0.75 | <0.001 |
| V5 ← DP | 0.59 | <0.001 | 0.61 | <0.001 |
| V15 ← DP | 0.46 | <0.001 | 0.46 | <0.001 |
| V22 ← DP | 0.47 | <0.001 | 0.45 | <0.001 |
| V12 ← EE | 0.45 | <0.001 | 0.44 | <0.001 |
| V12 ← PA | 0.25 | 0.001 | 0.28 | <0.001 |
| V13 ← EE | 0.57 | <0.001 | 0.58 | <0.001 |
| V13 ← DP | 0.27 | 0.002 | 0.22 | 0.001 |
| V10 ← EE | 0.21 | 0.161 | - | |
| V10 ← DP | 0.98 | <0.001 | 0.90 | <0.001 |
| V11 ← EE | −0.05 | 0.679 | - | |
| V11 ← DP | 0.82 | <0.001 | 0.80 | <0.001 |
| Model fit estimates: | ||||
| Chi-squared/df | 2.36 | <0.001 | 1.67 | <0.001 |
| CFI | 0.85 | 0.93 | ||
| TLI | 0.82 | 0.92 | ||
| IFI | 0.85 | 0.93 | ||
| RMSEA (90% CI) | 0.085 (0.075–0.095) | 0.059 (0.048–0.070) | ||
| Correlations: | ||||
| DP ←→ PA | 0.41 | <0.001 | 0.43 | <0.001 |
| PA ←→ EE | 0.38 | <0.001 | 0.39 | <0.001 |
| DP ←→ EE | 0.72 | <0.001 | 0.65 | <0.001 |
| Compared Study Groups | Constraints | χ2 | df | χ2/df | CFI | TLI | IFI | RMSEA (90% CI) |
|---|---|---|---|---|---|---|---|---|
| Subsamples: 1 vs. 2 | Identical path diagrams | 659.3 | 398 | 1.66 | 0.92 | 0.91 | 0.92 | 0.042 (0.036–0.047) |
| Constant factor loadings | 682.5 | 419 | 1.63 | 0.92 | 0.91 | 0.92 | 0.041 (0.035–0.046) | |
| Constant factor variances and covariances | 695.8 | 425 | 1.64 | 0.92 | 0.91 | 0.92 | 0.041 (0.035–0.046) | |
| Gender: males vs. females | Identical path diagrams | 693.4 | 398 | 1.74 | 0.92 | 0.90 | 0.92 | 0.044 (0.039–0.050) |
| Constant factor loadings | 720.9 | 419 | 1.72 | 0.91 | 0.90 | 0.92 | 0.044 (0.038–0.049) | |
| Constant factor variances and covariances | 730.6 | 425 | 1.72 | 0.91 | 0.91 | 0.91 | 0.044 (0.038–0.048) | |
| Age (years): Up to 30 vs. 30 or more | Identical path diagrams | 743.6 | 398 | 1.87 | 0.90 | 0.89 | 0.91 | 0.048 (0.043–0.054) |
| Constant factor loadings | 794.0 | 419 | 1.90 | 0.90 | 0.89 | 0.90 | 0.049 (0.044–0.054) | |
| Constant factor variances and covariances | 803.3 | 425 | 1.89 | 0.90 | 0.89 | 0.90 | 0.049 (0.044–0.054) | |
| Staffing: half-time vs. full-time | Identical path diagrams | 712.9 | 398 | 1.79 | 0.91 | 0.89 | 0.91 | 0.046 (0.041–0.052) |
| Constant factor loadings | 738.5 | 419 | 1.76 | 0.91 | 0.90 | 0.91 | 0.045 (0.040–0.051) | |
| Constant factor variances and covariances | 745.8 | 425 | 1.76 | 0.91 | 0.90 | 0.91 | 0.045 (0.040–0.051) |
| Compared Study Groups | Difference in Means Between Group 2 And Group 1 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Group 1 | Group 2 | EE | DP | PA | ||||||
| Estimate | SE | p | Estimate | SE | p | Estimate | SE | p | |||
| Gender | Male | Female | 0.386 | 0.159 | 0.015 | 0.157 | 0.141 | 0.265 | 0.003 | 0.145 | 0.983 |
| Age | Up to 30 years | 30 or more years | −0.381 | 0.127 | 0.003 | −0.422 | 0.124 | <0.001 | −0.073 | 0.027 | 0.796 |
| Work practice experience | Up to 10 years | 10 or more years | −0.395 | 0.130 | 0.002 | −0.463 | 0.118 | <0.001 | −0.140 | 0.106 | 0.186 |
| Staffing | Half-time | Full-time | 0.515 | 0.134 | <0.001 | 0.420 | 0.131 | 0.001 | 0.026 | 0.112 | 0.819 |
| Working in several places | In one clinic only | In two or more clinics | 0.166 | 0.124 | 0.182 | 0.082 | 0.119 | 0.490 | −0.067 | 0.106 | 0.528 |
| Specialization of dentists | Dentists in general practice | Oral surgeons | −0.776 | 0.254 | 0.002 | −0.445 | 0.219 | 0.002 | −0.226 | 0.235 | 0.336 |
| Prosthodontists | −0.565 | 0.328 | 0.085 | −0.693 | 0.183 | <0.001 | −0.491 | 0.246 | 0.046 | ||
| Orthodontists | −0.583 | 0.204 | 0.004 | −0.804 | 0.145 | <0.001 | −0.012 | 0.307 | 0.968 | ||
| Poedodontists | −0.319 | 0.284 | 0.262 | −0.440 | 0.227 | 0.053 | −0.429 | 0.227 | 0.059 | ||
| Endodontists | −0.864 | 0.216 | <0.001 | −0.635 | 0.188 | <0.001 | −0.240 | 0.219 | 0.273 | ||
| Periodontists | 0.152 | 0.298 | 0.610 | 0.216 | 0.433 | 0.617 | 0.060 | 0.288 | 0.834 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Slabšinskienė, E.; Gorelik, A.; Vasiliauskienė, I.; Kavaliauskienė, A.; Zaborskis, A. Factorial Validity and Variance of the Maslach Burnout Inventory between Demographic and Workload Groups among Dentists of Lithuania. Int. J. Environ. Res. Public Health 2020, 17, 9154. https://doi.org/10.3390/ijerph17249154
Slabšinskienė E, Gorelik A, Vasiliauskienė I, Kavaliauskienė A, Zaborskis A. Factorial Validity and Variance of the Maslach Burnout Inventory between Demographic and Workload Groups among Dentists of Lithuania. International Journal of Environmental Research and Public Health. 2020; 17(24):9154. https://doi.org/10.3390/ijerph17249154
Chicago/Turabian StyleSlabšinskienė, Eglė, Andrej Gorelik, Ingrida Vasiliauskienė, Aistė Kavaliauskienė, and Apolinaras Zaborskis. 2020. "Factorial Validity and Variance of the Maslach Burnout Inventory between Demographic and Workload Groups among Dentists of Lithuania" International Journal of Environmental Research and Public Health 17, no. 24: 9154. https://doi.org/10.3390/ijerph17249154
APA StyleSlabšinskienė, E., Gorelik, A., Vasiliauskienė, I., Kavaliauskienė, A., & Zaborskis, A. (2020). Factorial Validity and Variance of the Maslach Burnout Inventory between Demographic and Workload Groups among Dentists of Lithuania. International Journal of Environmental Research and Public Health, 17(24), 9154. https://doi.org/10.3390/ijerph17249154






