Salaried Workers’ Self-Perceived Health and Psychosocial Risk in Guayaquil, Ecuador
Abstract
1. Introduction
2. Materials and Methods
2.1. Design, Data, and Population
2.2. Analytical Variables
- (i)
- Q.33 “Do you feel supported by your team?”
- (ii)
- Q.34 “Do you feel supported by your superiors in your current work?”
- (iii)
- Q.35 “Are you afraid of losing your current job?”
- (iv)
- Q.32 “Are you exposed to negative feelings, emotions or treatment from others in the course of your work?”
- (v)
- Q.30 “Do you have to make a mental effort to do your job?”
- (vi)
- Q.31 “Do you have the time required to perform the tasks your job demands?”
2.3. Statistical Analysis
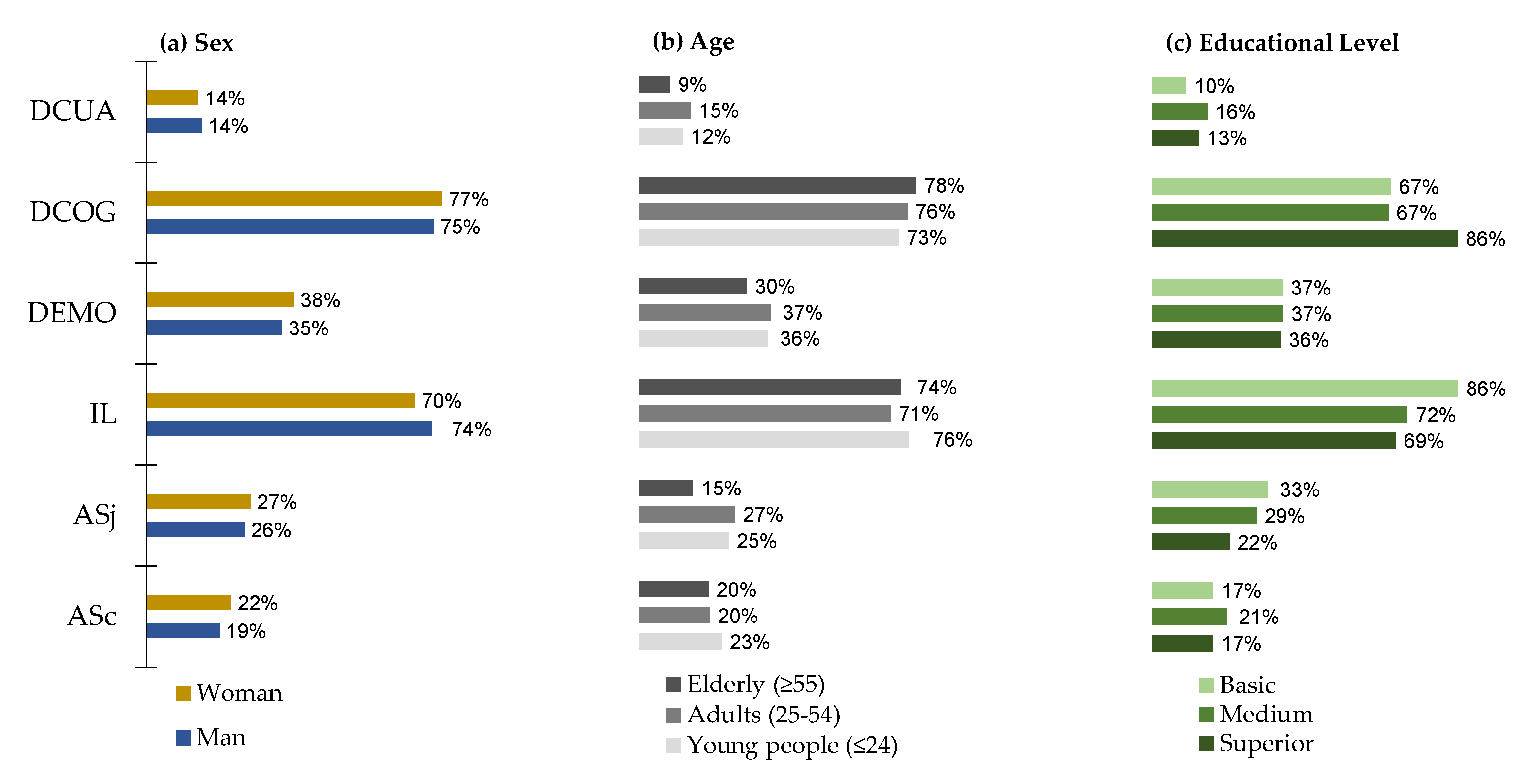
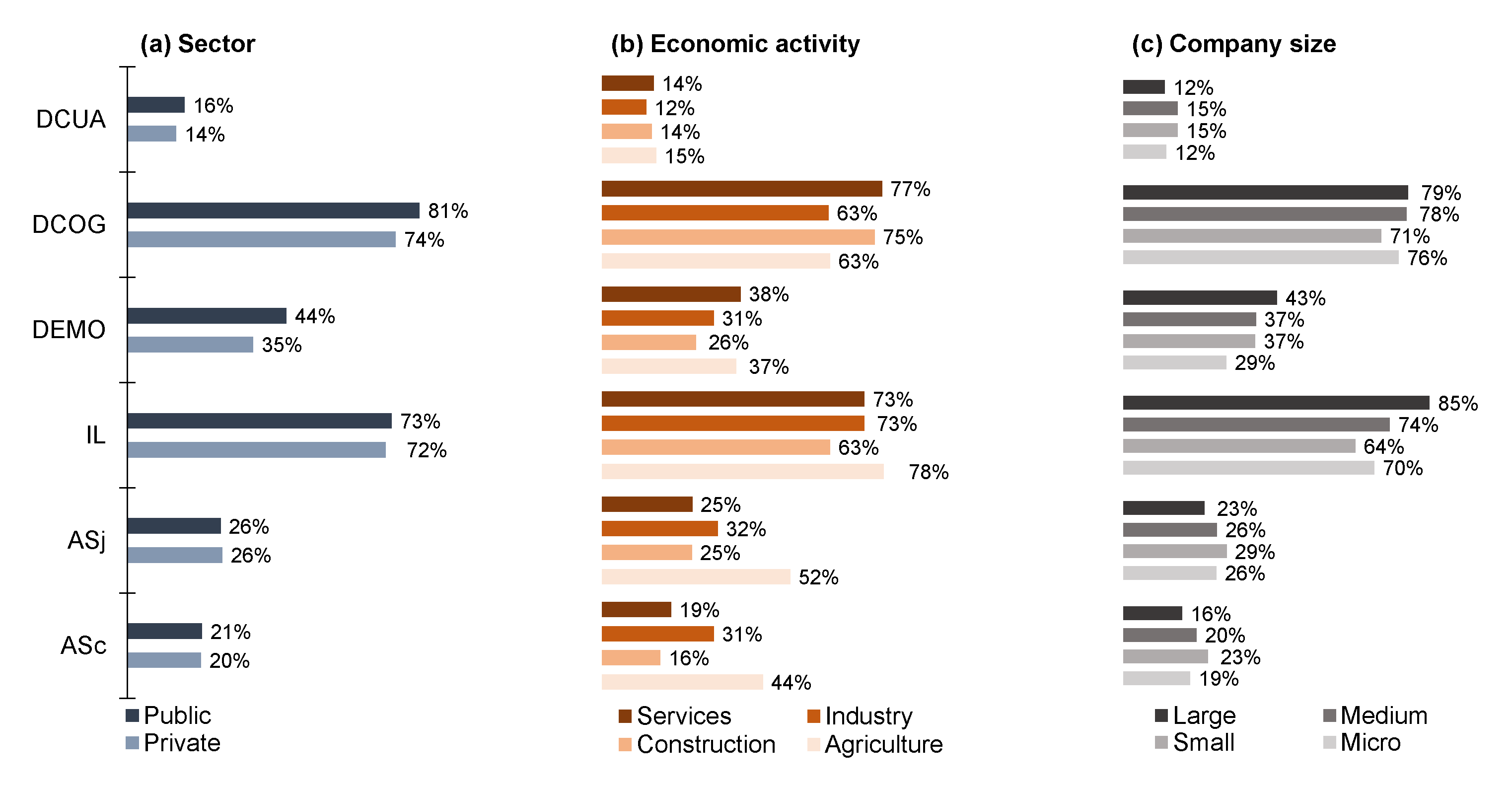
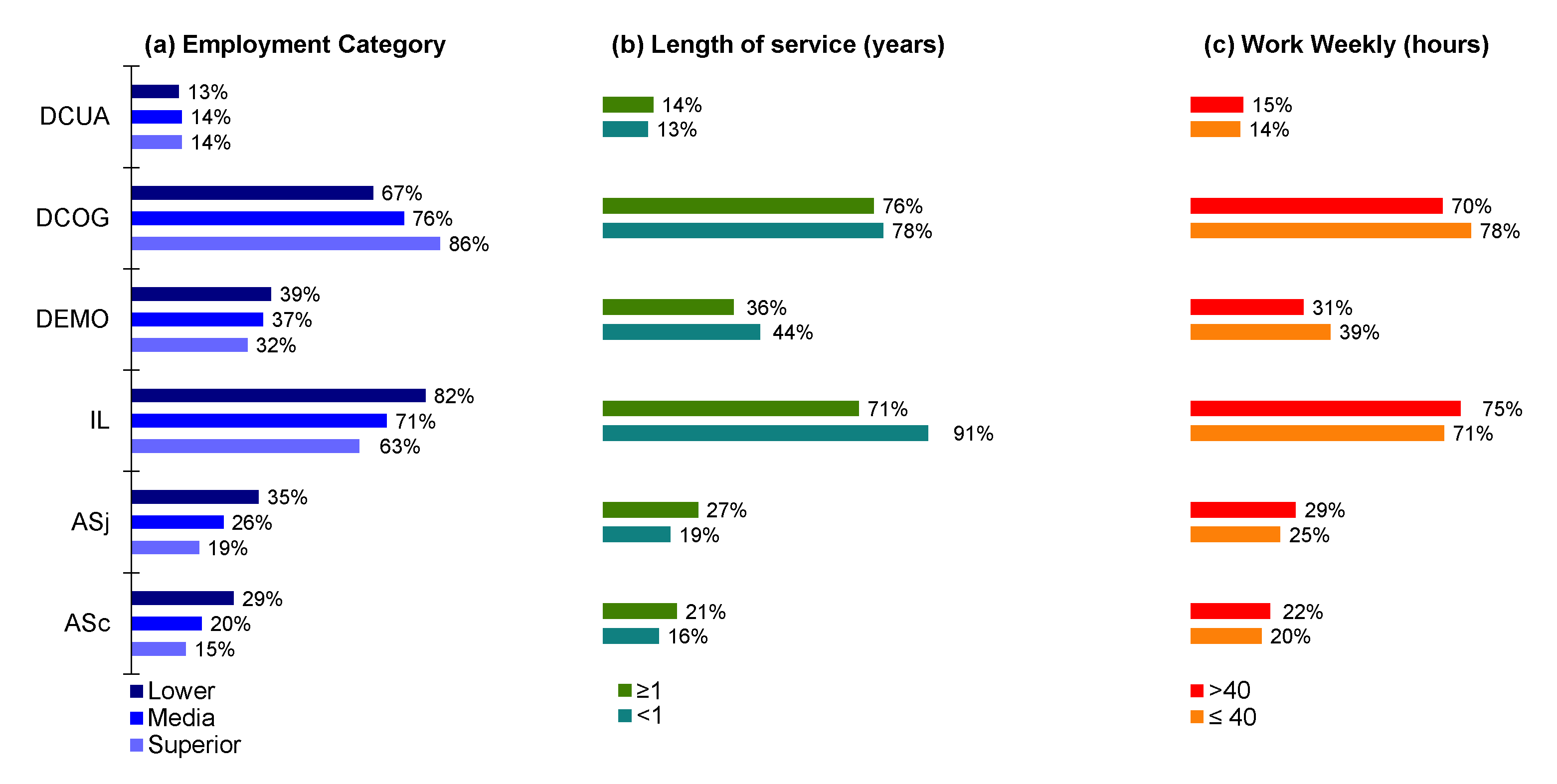
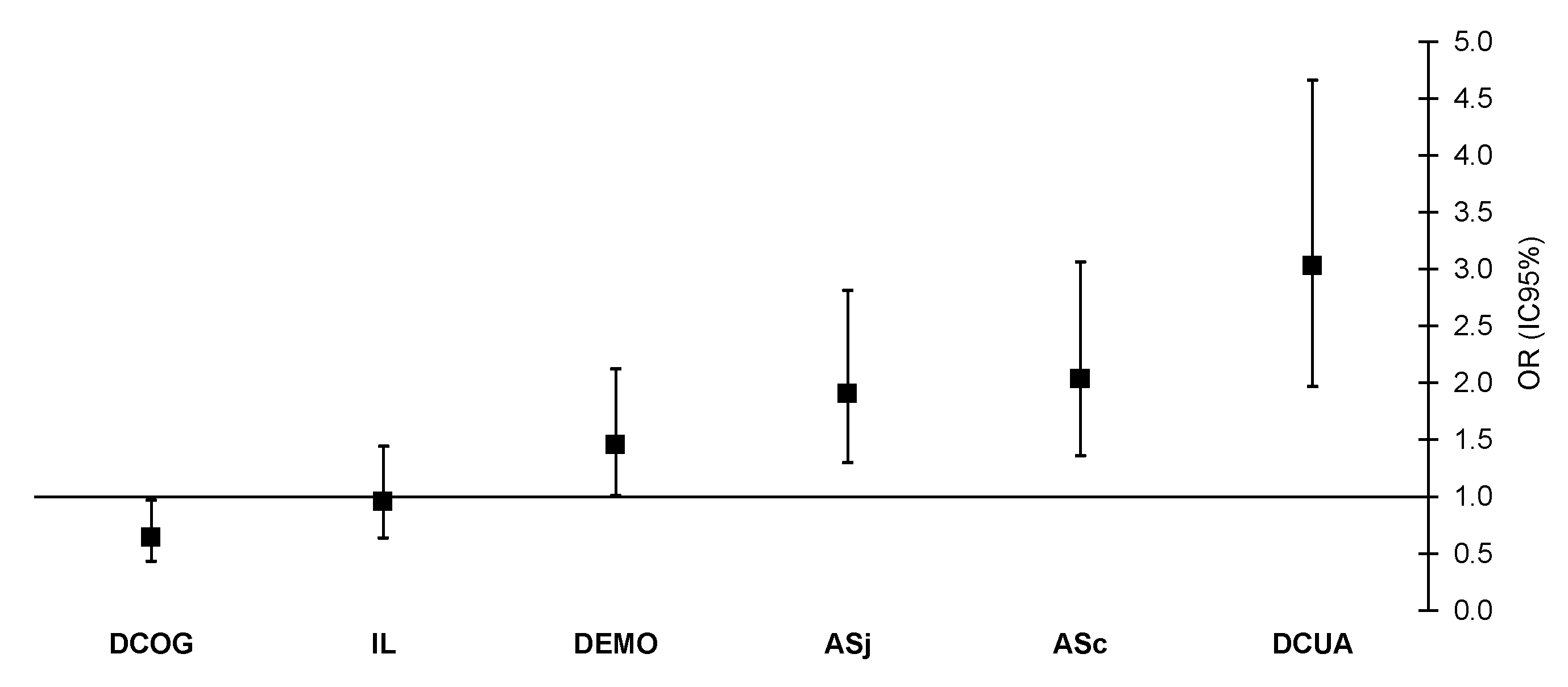
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Holmgren, K.; Dahlin-Ivanoff, S.; Björkelund, C.; Hensing, G. The prevalence of work-related stress, and its association with self-perceived health and sick-leave, in a population of employed Swedish women. BMC Public Health 2009, 9, 73. [Google Scholar] [CrossRef]
- Merino-Salazar, P.; Cornelio, C.; Lopez-Ruiz, M.; Benavides, F.G. Red Experta en Encuestas de Condiciones de Trabajo, Empleo y Salud. Propuesta de indicadores para la vigilancia de la salud ocupacional en América Latina y el Caribe. Revista Panamericana de Salud Pública 2018, 42, e125. [Google Scholar] [CrossRef] [PubMed]
- Cash-Gibson, L.; Rojas-Gualdrón, D.F.; Pericàs, J.M.; Benach, J. Inequalities in global health inequalities research: A 50-year bibliometric analysis (1966–2015). PLoS ONE 2018, 13, e0191901. [Google Scholar] [CrossRef] [PubMed]
- Leka, S.; Jain, A.; World Health Organization. Health Impact of Psychosocial Hazards at Work: An Overview; World Health Organization: Geneva, Switzerland, 2010; Available online: https://apps.who.int/iris/handle/10665/44428 (accessed on 10 August 2020).
- Benach, J.; Vives, A.; Amable, M.; Vanroelen, C.; Tarafa, G.; Muntaner, C. Precarious Employment: Understanding an Emerging Social Determinant of Health. Annu. Rev. Public Health 2014, 35, 229–253. [Google Scholar] [CrossRef] [PubMed]
- De Rovira, J.B.; Muntaner, C.; Solar, O.; Santana, V.S.; Quinlan, M. Introduction to the WHO Commission on Social Determinants of Health Employment Conditions Network (EMCONET) study, with a glossary on employment relations. Int. J. Health Serv. 2010, 40, 195–207. [Google Scholar] [CrossRef]
- Fonseca, S.; Guimaraes, V.; Gomes, M.; Nahas, M. Self-Perceived Health and Associated Factors in Industrial Workers from Santa Catarina State, Brasil. Cad. Saúde Pública 2008, 24, 567–576. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ghezzi, V.; Probst, T.M.; Petitta, L.; Ciampa, V.; Ronchetti, M.; Di Tecco, C.; Iavicoli, S.; Barbaranelli, C. The Interplay among Age and Employment Status on the Perceptions of Psychosocial Risk Factors at Work. Int. J. Environ. Res. Public Health 2020, 17, 3611. [Google Scholar] [CrossRef]
- López-Casasnovas, G.; Saez, M. Saved by Wealth? Income, Wealth, and Self-Perceived Health in Spain during the Financial Crisis. Int. J. Environ. Res. Public Health 2020, 17, 7018. [Google Scholar] [CrossRef]
- Cohidon, C.; Morisseau, P.; Derriennic, F.; Goldberg, M.; Imbernon, E. Psychosocial factors at work and perceived health among agricultural meat industry workers in France. Int. Arch. Occup. Environ. Health 2009, 82, 807–818. [Google Scholar] [CrossRef]
- Cox, T.; Griffiths, A.; Leka, S. Work Organization and Work-Related Stress. In Occupational Hygiene, 3rd ed.; Gardiner, K., Harrington, J.M., Eds.; Blackwell Publishing: Oxford, UK, 2005. [Google Scholar]
- De Raeve, L.; Jansen, N.W.H.; Brandt, P.A.V.D.; Vasse, R.; Kant, I.J. Interpersonal conflicts at work as a predictor of self-reported health outcomes and occupational mobility. Occup. Environ. Med. 2009, 66, 16–22. [Google Scholar] [CrossRef]
- De Witte, H. On the scarring effects of job insecurity (and how they can be explained). Scand. J. Work. Environ. Health 2016, 42, 99–102. [Google Scholar] [CrossRef] [PubMed]
- Lübke, C. How self-perceived job insecurity affects health: Evidence from an age-differentiated mediation analysis. Econ. Ind. Democr. 2019, 17, 1–18. [Google Scholar] [CrossRef]
- Vieco Gómez, G.F.; Abello Llanos, R. Factores psicosociales de origen laboral, estrés y morbilidad en el mundo. Psicología Desde el Caribe 2014, 31, 354–385. [Google Scholar]
- Rongen, A.; Robroek, S.J.; Schaufeli, W.; Burdorf, A. The Contribution of Work Engagement to Self-Perceived Health, Work Ability, and Sickness Absence Beyond Health Behaviors and Work-Related Factors. J. Occup. Environ. Med. 2014, 56, 892–897. [Google Scholar] [CrossRef]
- Niedhammer, I.; Chastang, J.-F.; David, S. Importance of psychosocial work factors on general health outcomes in the national French SUMER survey. Occup. Med. 2008, 58, 15–24. [Google Scholar] [CrossRef]
- Jung, J.; Kim, G.; Kim, K.; Paek, D.; Cho, S.-I. Association between working time quality and self-perceived health: Analysis of the 3rd Korean working conditions survey (2011). Ann. Occup. Environ. Med. 2017, 29, 55. [Google Scholar] [CrossRef]
- Frone, M.R. Work–family conflict and employee psychiatric disorders: The national comorbidity survey. J. Appl. Psychol. 2000, 85, 888–895. [Google Scholar] [CrossRef]
- Ravallion, M. Income inequality in the developing world. Science 2014, 344, 851–855. [Google Scholar] [CrossRef]
- Merino-Salazar, P.; Artazcoz, L.; Cornelio, C.; Iñiguez, M.J.I.; Rojas, M.; Martínez-Iñigo, D.; Vives, A.; Funcasta, L.; Benavides, F.G. Work and health in Latin America: Results from the working conditions surveys of Colombia, Argentina, Chile, Central America and Uruguay. Occup. Environ. Med. 2017, 74, 432–439. [Google Scholar] [CrossRef]
- Iñiguez, M.J.I.; Agudelosuarez, A.A.; Campos-Serna, J.; Cornelio, C.I.; Benavides, F.G. Encuestas de condiciones de trabajo y salud: Su utilización en la investigación en salud laboral. Med. Segur. Trab. 2012, 58, 205–215. [Google Scholar] [CrossRef][Green Version]
- Gómez García, A.R. I Encuesta sobre Seguridad y Salud en el Trabajo para Ecuador: I-ESST. CienciAmérica 2017, 6, 67–75. [Google Scholar]
- Merino-Salazar, P.; Gómez-García, A.R.; Silva-Peñaherrera, G.M.; Suasnavas-Bermudez, P.R.; Rojas, M. The Impact of Ergonomic Exposures on the Occurrence of Back Pain or Discomfort: Results from the First Working Conditions Survey in Quito-Ecuador. In Advances in Social & Occupational Ergonomics. AHFE 2017. Advances in Intelligent Systems and Computing; Springer: Cham, Switzerland, 2018; p. 605. [Google Scholar] [CrossRef]
- Gómez-García, A.R.; Salazar, P.M.; Samaniego, C.E.E.; Vasco, P.E.C. I Encuesta sobre Seguridad y Salud en el Trabajo en Quito: Siniestralidad laboral. Podium 2018, 33, 25–34. [Google Scholar] [CrossRef]
- Artázcoz, L.; Borrell, C.; Rohlfs, I.; Beni, C.; Moncada, A.; Benach, J. Trabajo doméstico, género y salud en población ocupada. Gac. Sanit. 2001, 15, 150–153. [Google Scholar] [CrossRef]
- Bartoll, X.; Ramos, R. Worked hours, job satisfaction and self-perceived health. J. Econ. Stud. 2020. [Google Scholar] [CrossRef]
- Liu, C.E.; Yu, S.; Chen, Y.; He, W. Supervision Incivility and Employee PsychologicalSafety in the Workplace. Int. J. Environ. Res. Public Health 2020, 17, 840. [Google Scholar] [CrossRef]
- Jarrín, P.V.; Di Gravia, A.R.; Campos, Y.Y. Working conditions related to self-perceived health in flower farmers [Condiciones de trabajo relacionada con salud autopercibida en floricultores]. Espacios 2019, 40, 5. [Google Scholar]
- Silva-Peñaherrera, M.; Lopez-Ruiz, M.; Merino-Salazar, P.; Gómez-García, A.R.; Benavides, F.G. Health inequity in workers of Latin America and the Caribbean. Int. J. Equity Health 2020, 19, 1–9. [Google Scholar] [CrossRef]
- González-Galarzo, M.C.; Ronda-Pérez, E.; García Benavides, F.; García García, A.M. Factores sociodemográficos y laborales relacionados con la exposición laboral a riesgos psicosociales por ocupación en España. Proyecto MatEmESp. Arch. Prevención Riesgos Labor. 2019, 22, 121–128. [Google Scholar] [CrossRef]
- Mikkelsen, E.G.; Einarsen, S. Relationships between exposure to bullying at work and psychological and psychosomatic health complaints: The role of state negative affectivity and generalized self-efficacy. Scand. J. Psychol. 2002, 43, 397–405. [Google Scholar] [CrossRef]
- Song, J.-T.; Lee, G.; Kwon, J.; Park, J.-W.; Choi, H.R.; Lim, S. The Association between Long Working Hours and Self-Rated Health. Ann. Occup. Environ. Med. 2014, 26, 2. [Google Scholar] [CrossRef]
- Artazcoz, L.; Cortès, I.; Escribà-Agüir, V.; Cascant, L.; Villegas, R. Understanding the relationship of long working hours with health status and health-related behaviours. J. Epidemiol. Community Health 2009, 63, 521–527. [Google Scholar] [CrossRef] [PubMed]
| Variables | n | %n | SHS | p-Value | |
|---|---|---|---|---|---|
| Good | Poor | ||||
| Socio-Demographics | |||||
| Sex | |||||
| Women | 519 | 49.5 | 88.2 | 11.8 | 0.660 |
| Men | 530 | 50.5 | 87.4 | 12.6 | |
| Age (years) | |||||
| Young people (≤24) | 146 | 13.9 | 93.2 | 6.8 | 0.002 |
| Adults (25–54) | 857 | 81.7 | 87.6 | 12.4 | |
| Elderly (≥55) | 46 | 4.4 | 73.9 | 26.1 | |
| Educational Level | |||||
| Superior | 477 | 45.5 | 89.9 | 10.1 | 0.001 |
| Medium | 477 | 45.5 | 88.1 | 11.9 | |
| Basic | 95 | 9.1 | 75.8 | 24.2 | |
| Labor | |||||
| Sector | |||||
| Private | 840 | 80.1 | 89.3 | 10.7 | 0.003 |
| Public | 209 | 19.9 | 81.8 | 18.2 | |
| Economic Activity | |||||
| Agriculture | 27 | 2.6 | 88.9 | 11.1 | 0.511 |
| Construction | 81 | 7.7 | 82.7 | 17.3 | |
| Industry | 91 | 8.7 | 86.8 | 13.2 | |
| Services | 850 | 81 | 88.4 | 11.6 | |
| Company Size | |||||
| Micro | 151 | 14.4 | 85.4 | 14.6 | 0.402 |
| Small | 384 | 36.6 | 87.8 | 12.2 | |
| Medium | 305 | 29.1 | 90.2 | 9.8 | |
| Large | 209 | 19.9 | 86.1 | 13.9 | |
| Employment | |||||
| Employment Category | |||||
| Superior | 93 | 8.9 | 84.9 | 15.1 | 0.000 |
| Medium | 812 | 77.4 | 90.0 | 10.0 | |
| Lower | 144 | 13.7 | 77.1 | 22.9 | |
| Tenure (years) | |||||
| <1 | 32 | 3.1 | 96.9 | 3.1 | 0.111 |
| ≥1 | 1017 | 96.9 | 87.5 | 12.5 | |
| Weekly Work (hours) | |||||
| ≤40 | 731 | 69.7 | 89.2 | 10.8 | 0.036 |
| >40 | 318 | 30.3 | 84.6 | 15.4 | |
| Variables | ASc | ASj | IL | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | Test a | OR (95% CI) | Test a | OR (95% CI) | Test a | |
| Socio-Demographics | ||||||
| Sex | ||||||
| Women | 2.06 (1.16–3.66) ** | s1 | 2.24 (1.29–3.89) ** | s1 | 1.14 (0.63–2.06) | s4 |
| Men | 2.04 (1.15–3.62) ** | 1.64 (0.95–2.83) | 0.80 (0.46–1.41) | |||
| Age (years) | ||||||
| Young people (≤24) | 1.45 (0.35–5.95) | s1 | 0.72 (0.15–3.56) | s1 | 1.28 (0.26–6.34) | s4 |
| Adults (25–54) | 2.23 (1.43–3.48) *** | 2.24 (1.47–3.41) *** | 0.98 (0.63–1.54) | |||
| Elderly (≥55) | 1.56 (0.32–7.52) | 1.16 (0.19–6.95) | 0.62 (0.15–2.59) | |||
| Educational Level | ||||||
| Superior | 1.94 (0.98–3.85) * | s3 | 1.55 (0.80–3.01) | s3 | 0.81 (0.43–1.52) | s4 |
| Medium | 1.56 (0.84–2.92) | 2.07 (1.18–3.65) ** | 1.09 (0.59–2.05) | |||
| Basic | 2.84 (1.08–7.46) * | 1.87 (0.71–4.92) | 0.45 (0.13–1.55) | |||
| Labor | ||||||
| Sector | ||||||
| Private | 2.04 (1.26–3.28) ** | s1 | 2.39 (1.52–3.74) *** | s1 | 1.18 (0.72–1.94) | s4 |
| Public | 2.08 (0.95–4.58) | 1.03 (0.46–2.29) | 0.56 (0.27–1.18) | |||
| Economic Activity | ||||||
| Agriculture | 2.80 (0.22–35.29) | s1 | 1.27 (0.97–1.67) | s1 | - | s4 |
| Construction | 1.56 (0.37–6.58) | 2.84 (0.85–9.53) | 1.07 (0.32–3.56) | |||
| Industry | 1.74 (0.50–6.05) | 2.44 (0.71–8.34) | 0.48 (0.14–1.66) | |||
| Services | 2.18 (1.37–3.47) *** | 1.68 (1.08–2.64) ** | 1.02 (0.63–1.62) | |||
| Company Size | ||||||
| Micro | 2.40 (0.87–6.60) | s1 | 1.81 (0.69–4.71) | s1 | 0.73 (0.28–1.89) | s4 |
| Small | 2.05 (1.07–3.92) * | 1.83 (0.98–3.45) | 0.88 (0.47–1.65) | |||
| Medium | 1.80 (0.78–4.14) | 2.83 (1.31–6.10) ** | 1.47 (0.58–3.75) | |||
| Large | 2.26 (0.90–5.63) | 1.38 (0.57–3.35) | 0.85 (0.30–2.41) | |||
| Employment | ||||||
| Employment Category | ||||||
| Superior | 1.69 (0.41–7.02) | s1 | 0.33 (0.04–2.71) | s3 | 1.04 (0.32–3.42) | s4 |
| Medium | 1.86 (1.11–3.10) ** | 1.72 (1.06–2.79) * | 0.90 (0.55–1.49) | |||
| Lower | 2.29 (1.01–5.18) * | 3.35 (1.50–7.48) ** | 0.77 (0.29–2.02) | |||
| Tenure (years) | ||||||
| <1 | 0.96 (0.89–1.04) | s1 | - | s2 | 1.04 (0.97–1.11) | s4 |
| ≥1 | 2.05 (1.36–3.08) *** | 1.91 (1.30–2.82) *** | 0.98 (0.65–1.47) | |||
| Weekly Work (hours) | ||||||
| ≤40 | 1.56 (0.91–2.66) | s1 | 1.67 (1.01–2.74) * | s2 | 1.37 (0.80–2.35) | s4 |
| >40 | 3.02 (1.58–5.77) *** | 2.27 (1.22–4.24) ** | 0.51 (0.26–0.97) | |||
| Socio-Demographics | ||||||
| Sex | ||||||
| Women | 1.49 (0.88–2.50) | s4 | 0.69 (0.38–1.25) | s4 | 3.98 (2.16–7.33) *** | s1 |
| Men | 1.44 (0.84–2.46) | 0.61 (0.35–1.06) | 2.33 (1.26–4.30) ** | |||
| Age (years) | ||||||
| Young people (≤24) | 1.83 (0.51–6.65) | s4 | 0.84 (0.21–3.42) | s4 | 1.88 (0.37–9.62) | s1 |
| Adults (25–54) | 1.42 (0.94–2.14) | 0.60 (0.39–0.94) * | 3.47 (2.18–5.51) *** | |||
| Elderly (≥55) | 1.98 (0.50–7.87) | 0.78 (0.17–3.66) | 0.94 (0.09–10.00) | |||
| Educational Level | ||||||
| Superior | 1.88 (1.03–3.42) * | s4 | 0.66 (0.31–1.44) | s4 | 5.73 (2.97–11.06) *** | s1 |
| Medium | 1.09 (0.62–1.92) | 0.71 (0.40–1.25) | 2.19 (1.14–4.19) ** | |||
| Basic | 1.83 (0.71–4.76) | 0.68 (0.26–1.82) | 1.65 (0.38–7.20) | |||
| Labor | ||||||
| Sector | ||||||
| Private | 1.43 (0.92–2.23) | s4 | 0.66 (0.41–1.05) | s4 | 2.70 (1.61–4.53) *** | s1 |
| Public | 1.34 (0.66–2.72) | 0.50 (0.22–1.12) | 3.93 (1.74–8.88) *** | |||
| Economic Activity | ||||||
| Agriculture | 4.00 (0.31–51.03) | s4 | 0.25 (0.02–3.19) | s4 | 3.50 (0.24–51.46) | s1 |
| Construction | 2.60 (0.78–8.67) | 0.52 (0.15–1.79) | 2.01 (0.46–8.79) | |||
| Industry | 1.15 (0.32–4.17) | 1.22 (0.34–4.42) | 8.69 (2.11–35.87) *** | |||
| Services | 1.40 (0.92–2.14) | 0.63 (0.40–1.01) | 2.83 (1.73–4.61) *** | |||
| Company Size | ||||||
| Micro | 0.93 (0.34–2.57) | s4 | 0.30 (0.12–0.78) * | s4 | 2.62 (0.83–8.29) | s1 |
| Small | 1.21 (0.65–2.26) | 0.84 (0.43–1.62) | 3.63 (1.83–7.19) *** | |||
| Medium | 2.13 (1.00–4.55) | 0.61 (0.27–1.40) | 4.73 (2.09–10.66) *** | |||
| Large | 2.13 (1.00–4.55) | 0.81 (0.32–2.05) | 1.28 (0.40–4.06) | |||
| Employment | ||||||
| Employment Category | ||||||
| Superior | 3.46 (1.08–11.10) * | s4 | 0.97 (0.19–4.94) | s4 | 3.11 (0.81–12.02) | s1 |
| Medium | 1.35 (0.85–2.16) | 0.57 (0.35–0.92) * | 3.70 (2.22–6.18) *** | |||
| Lower | 1.21 (0.55–2.67) | 0.96 (0.42–2.19) | 1.68 (0.58–4.82) | |||
| Tenure (years) | ||||||
| <1 | 0.94 (0.84–1.06) | s4 | - | s4 | 1.33 (0.76–2.35) ** | s1 |
| ≥1 | 1.50 (1.03–2.19) * | 0.67 (0.45–1.00) * | 2.93 (1.89–4.53) *** | |||
| Weekly Work (hours) | ||||||
| ≤40 | 1.72 (1.07–2.74) * | s4 | 0.70 (0.42–1.19) | s4 | 3.31 (1.94–5.65) *** | s1 |
| >40 | 1.19 (0.63–2.26) | 0.62 (0.33–1.17) | 2.58 (1.24–5.37) ** | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gómez-García, A.R.; Portalanza-Chavarría, C.A.; Arias-Ulloa, C.A.; Espinoza-Samaniego, C.E. Salaried Workers’ Self-Perceived Health and Psychosocial Risk in Guayaquil, Ecuador. Int. J. Environ. Res. Public Health 2020, 17, 9099. https://doi.org/10.3390/ijerph17239099
Gómez-García AR, Portalanza-Chavarría CA, Arias-Ulloa CA, Espinoza-Samaniego CE. Salaried Workers’ Self-Perceived Health and Psychosocial Risk in Guayaquil, Ecuador. International Journal of Environmental Research and Public Health. 2020; 17(23):9099. https://doi.org/10.3390/ijerph17239099
Chicago/Turabian StyleGómez-García, Antonio Ramón, Cecilia Alexandra Portalanza-Chavarría, Christian Arturo Arias-Ulloa, and César Eduardo Espinoza-Samaniego. 2020. "Salaried Workers’ Self-Perceived Health and Psychosocial Risk in Guayaquil, Ecuador" International Journal of Environmental Research and Public Health 17, no. 23: 9099. https://doi.org/10.3390/ijerph17239099
APA StyleGómez-García, A. R., Portalanza-Chavarría, C. A., Arias-Ulloa, C. A., & Espinoza-Samaniego, C. E. (2020). Salaried Workers’ Self-Perceived Health and Psychosocial Risk in Guayaquil, Ecuador. International Journal of Environmental Research and Public Health, 17(23), 9099. https://doi.org/10.3390/ijerph17239099






