Buccal Bone Changes Around First Permanent Molars and Second Primary Molars after Maxillary Expansion with a Low Compliance Ni–Ti Leaf Spring Expander
Abstract
1. Introduction
2. Materials and Methods
2.1. Cone-Beam Computerized Tomography (CBCT) Examination and Data Processing
- -
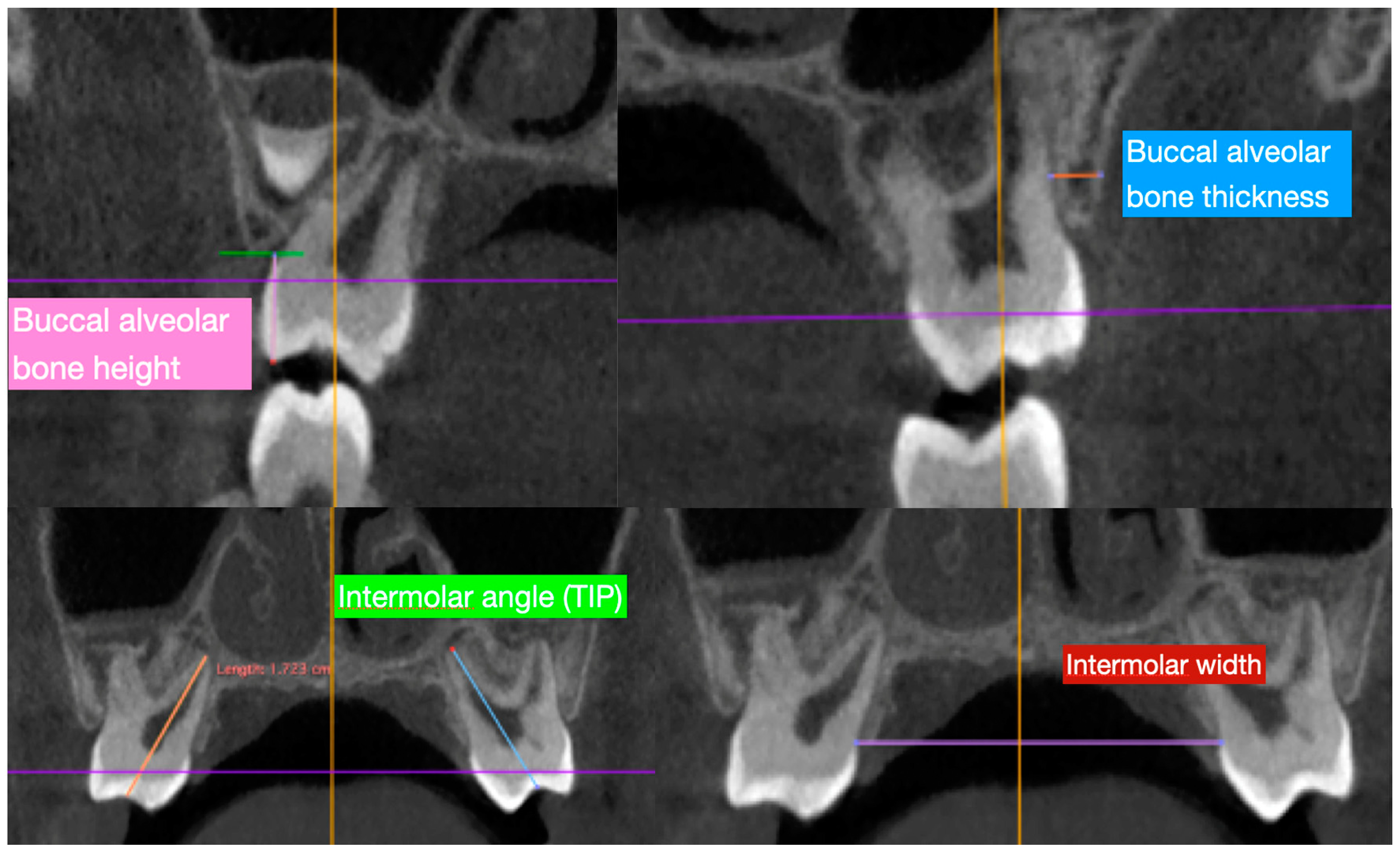
- Buccal alveolar bone thickness (BT), defined as the distance between the buccal root surface and the outer border of the alveolar bone, along a horizontal line passing through the furcation;
- -
- Buccal alveolar bone height (BH), defined as the distance between the buccal or mesio-buccal cusp tip and the buccal alveolar bone crest;
- -
- Inter-dental angle (TIP), represented by the angle between the right and left axes of the upper molars (6-6) and deciduous molars (E-E), determined by connecting the central fossa and the apex of the palatal root; and
- -
- Inter-molar width (IW), defined as the upper inter-molar (6-6) and deciduous molar (E-E) distance between the mesio-buccal cusp tips.
2.2. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Gungor, K.; Taner, L.; Kaygisiz, E. Prevalence of Posterior Crossbite for Orthodontic Treatment Timing. J. Clin. Pediatr. Dent. 2016, 40, 422–424. [Google Scholar] [CrossRef] [PubMed]
- Abate, A.; Cavagnetto, D.; Fama, A.; Matarese, M.; Lucarelli, D.; Assandri, F. Short term effects of rapid maxillary expansion on breathing function assessed with spirometry: A case-control study. Saudi Dent. J. 2020. [Google Scholar] [CrossRef]
- Iodice, G.; Danzi, G.; Cimino, R.; Paduano, S.; Michelotti, A. Association between posterior crossbite, skeletal, and muscle asymmetry: A systematic review. Eur. J. Orthod. 2016, 38, 638–651. [Google Scholar] [CrossRef] [PubMed]
- Maspero, C.; Cavagnetto, D.; Abate, A.; Cressoni, P.; Farronato, M. Effects on the Facial Growth of Rapid Palatal Expansion in Growing Patients Affected by Juvenile Idiopathic Arthritis with Monolateral Involvement of the Temporomandibular Joints: A Case-Control Study on Posteroanterior and Lateral Cephalograms. J. Clin. Med. 2020, 9, 1159. [Google Scholar] [CrossRef]
- Lagravere, M.O.; Major, P.W.; Flores-Mir, C. Long-term dental arch changes after rapid maxillary expansion treatment: A systematic review. Angle Orthod. 2005, 75, 155–161. [Google Scholar] [CrossRef]
- Pereira, J.D.S.; Jacob, H.B.; Locks, A.; Brunetto, M.; Ribeiro, G.L.U. Evaluation of the rapid and slow maxillary expansion using cone-beam computed tomography: A randomized clinical trial. Dental Press J. Orthod. 2017, 22, 61–68. [Google Scholar] [CrossRef]
- McNamara, J.A.; Lione, R.; Franchi, L.; Angelieri, F.; Cevidanes, L.H.S.; Darendeliler, M.A.; Cozza, P. The role of rapid maxillary expansion in the promotion of oral and general health. Prog. Orthod. 2015, 16, 33. [Google Scholar] [CrossRef]
- Maspero, C.; Farronato, M.; Bellincioni, F.; Annibale, A.; Machetti, J.; Abate, A.; Cavagnetto, D. Three-Dimensional Evaluation of Maxillary Sinus Changes in Growing Subjects: A Retrospective Cross-Sectional Study. Materials 2020, 13, 1007. [Google Scholar] [CrossRef]
- Lagravère, M.O.; Heo, G.; Major, P.W.; Flores-Mir, C. Meta-analysis of immediate changes with rapid maxillary expansion treatment. J. Am. Dent. Assoc. 2006, 137, 44–53. [Google Scholar] [CrossRef]
- Priyadarshini, J.; Mahesh, C.M.; Chandrashekar, B.S.; Sundara, A.; Arun, A.V.; Reddy, V.P. Stress and displacement patterns in the craniofacial skeleton with rapid maxillary expansion-a finite element method study. Prog. Orthod. 2017, 18, 17. [Google Scholar] [CrossRef]
- Farronato, G.; Giannini, L.; Galbiati, G.; Maspero, C. Comparison of the dental and skeletal effects of two different rapid palatal expansion appliances for the correction of the maxillary asymmetric transverse discrepancies. Minerva Stomatol. 2012, 61, 45–55. [Google Scholar] [PubMed]
- Maspero, C.; Abate, A.; Cavagnetto, D.; Morsi, M.; Fama, A.; Farronato, M. Available Technologies, Applications and Benefits of Teleorthodontics. A Literature Review and Possible Applications during the COVID-19 Pandemic. J. Clin. Med. 2020, 9, 1891. [Google Scholar] [CrossRef] [PubMed]
- Maspero, C.; Farronato, M.; Bellincioni, F.; Cavagnetto, D.; Abate, A. Assessing mandibular body changes in growing subjects: A comparison of CBCT and reconstructed lateral cephalogram measurements. Sci. Rep. 2020. [Google Scholar] [CrossRef] [PubMed]
- Zimring, J.F.; Isaacson, R.J. Forces produced by rapid maxillary expansion. 3. Forces present during retention. Angle Orthod. 1965, 35, 178–186. [Google Scholar] [CrossRef]
- Fama, A.; Cavagnetto, D.; Abate, A.; Mainardi, E.; De Filippis, A.; Esposito, L. Treatment of dental dilacerations. Dent. Cadmos 2020, in press. [Google Scholar]
- Maspero, C.; Fama, A.; Cavagnetto, D.; Abate, A.; Farronato, M. Treatment of dental dilacerations. J. Biol. Regul. Homeost. Agents 2019, 33, 1623–1627. [Google Scholar]
- Bishara, S.E.; Staley, R.N. Maxillary expansion: Clinical implications. Am. J. Orthod. Dentofac. Orthop. 1987, 91, 3–14. [Google Scholar] [CrossRef]
- Huynh, T.; Kennedy, D.B.; Joondeph, D.R.; Bollen, A.-M. Treatment response and stability of slow maxillary expansion using Haas, hyrax, and quad-helix appliances: A retrospective study. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 331–339. [Google Scholar] [CrossRef]
- Greenbaum, K.R.; Zachrisson, B.U. The effect of palatal expansion therapy on the periodontal supporting tissues. Am. J. Orthod. 1982, 81, 12–21. [Google Scholar] [CrossRef]
- Van Vlijmen, O.J.C.; Maal, T.J.J.; Bergé, S.J.; Bronkhorst, E.M.; Katsaros, C.; Kuijpers-Jagtman, A.M. A comparison between two-dimensional and three-dimensional cephalometry on frontal radiographs and on cone beam computed tomography scans of human skulls. Eur. J. Oral Sci. 2009, 117, 300–305. [Google Scholar] [CrossRef]
- Janson, G.; Bombonatti, R.; Brandão, A.G.; Henriques, J.F.C.; de Freitas, M.R. Comparative radiographic evaluation of the alveolar bone crest after orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2003, 124, 157–164. [Google Scholar] [CrossRef]
- Farronato, G.; Maspero, C.; Esposito, L.; Briguglio, E.; Farronato, D.; Giannini, L. Rapid maxillary expansion in growing patients. Hyrax versus transverse sagittal maxillary expander: A cephalometric investigation. Eur. J. Orthod. 2011, 33, 185–189. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Maspero, C.; Abate, A.; Bellincioni, F.; Cavagnetto, D.; Lanteri, V.; Costa, A.; Farronato, M. Comparison of a tridimensional cephalometric analysis performed on 3T-MRI compared with CBCT: A pilot study in adults. Prog. Orthod. 2019, 20, 40. [Google Scholar] [CrossRef] [PubMed]
- Brunetto, M.; Andriani, J.D.S.P.; Ribeiro, G.L.U.; Locks, A.; Correa, M.; Correa, L.R. Three-dimensional assessment of buccal alveolar bone after rapid and slow maxillary expansion: A clinical trial study. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 633–644. [Google Scholar] [CrossRef] [PubMed]
- Lanteri, C.; Beretta, M.; Lanteri, V.; Gianolio, A.; Cherchi, C.; Franchi, L. The Leaf Expander for Non-Compliance Treatment in the Mixed Dentition. J. Clin. Orthod. 2016, 50, 552–560. [Google Scholar]
- Lanteri, V.; Cossellu, G.; Gianolio, A.; Beretta, M.; Lanteri, C.; Cherchi, C.; Farronato, G. Comparison between RME, SME and Leaf Expander in growing patients: A retrospective postero-anterior cephalometric study. Eur. J. Paediatr. Dent. 2018. [Google Scholar] [CrossRef]
- Beretta, M.; Lanteri, C.; Lanteri, V.; Cherchi, C.; Franchi, L.; Gianolio, A. Evolution of the Leaf Expander: A Maxillary Self Expander. J. Clin. Orthod. 2019, 53, 260–266. [Google Scholar]
- Lanteri, V.; Gianolio, A.; Gualandi, G.; Beretta, M. Maxillary tridimensional changes after slow expansion with leaf expander in a sample of growing patients: A pilot study. Eur. J. Paediatr. Dent. 2018. [Google Scholar] [CrossRef]
- Lanteri, V.; Farronato, M.; Ugolini, A.; Cossellu, G.; Gaffuri, F.; Parisi, F.M.R.; Cavagnetto, D.; Abate, A.; Maspero, C. Volumetric Changes in the Upper Airways after Rapid and Slow Maxillary Expansion in Growing Patients: A Case-Control Study. Materials 2020, 13, 2239. [Google Scholar] [CrossRef]
- Mutinelli, S.; Cozzani, M. Rapid maxillary expansion in early-mixed dentition: Effectiveness of increasing arch dimension with anchorage on deciduous teeth. Eur. J. Paediatr. Dent. 2015, 16, 115–122. [Google Scholar]
- Castro, L.O.; Castro, I.O.; de Alencar, A.H.G.; Valladares-Neto, J.; Estrela, C. Cone beam computed tomography evaluation of distance from cementoenamel junction to alveolar crest before and after nonextraction orthodontic treatment. Angle Orthod. 2016, 86, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Cotton, L.A. Slow maxillary expansion: Skeletal versus dental response to low magnitude force in Macaca mulatta. Am. J. Orthod. 1978, 73, 1–23. [Google Scholar] [CrossRef]
- Isaacson, R.J.; Ingram, A.H. Forces Produced By Rapid Maxillary Expansion. Angle Orthod. 1964, 31, 201. [Google Scholar]
- Proffit, W.R.; Fields, H.W., Jr.; Sarver, D.M. Contemporary Orthodontics; Mosby; Elsevier: St. Louis, MO, USA, 2007. [Google Scholar]
- Ballanti, F.; Lione, R.; Fanucci, E.; Franchi, L.; Baccetti, T.; Cozza, P. Immediate and post-retention effects of rapid maxillary expansion investigated by computed tomography in growing patients. Angle Orthod. 2009, 79, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Lagravère, M.O.; Carey, J.; Heo, G.; Toogood, R.W.; Major, P.W. Transverse, vertical, and anteroposterior changes from bone-anchored maxillary expansion vs traditional rapid maxillary expansion: A randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 304. [Google Scholar] [CrossRef]
- Rungcharassaeng, K.; Caruso, J.M.; Kan, J.Y.K.; Kim, J.; Taylor, G. Factors affecting buccal bone changes of maxillary posterior teeth after rapid maxillary expansion. Am. J. Orthod. Dentofac. Orthop. 2007, 132, 428.e1–428.e8. [Google Scholar] [CrossRef] [PubMed]
- Adkins, M.D.; Nanda, R.S.; Currier, G.F. Arch perimeter changes on rapid palatal expansion. Am. J. Orthod. Dentofac. Orthop. 1990, 97, 194–199. [Google Scholar] [CrossRef]
- Garib, D.G.; Henriques, J.F.C.; Janson, G.; de Freitas, M.R.; Fernandes, A.Y. Periodontal effects of rapid maxillary expansion with tooth-tissue-borne and tooth-borne expanders: A computed tomography evaluation. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 749–758. [Google Scholar] [CrossRef]
- Weissheimer, A.; de Menezes, L.M.; Mezomo, M.; Dias, D.M.; de Lima, E.M.S.; Rizzatto, S.M.D. Immediate effects of rapid maxillary expansion with Haas-type and hyrax-type expanders: A randomized clinical trial. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 366–376. [Google Scholar] [CrossRef]
- Wong, C.A.; Sinclair, P.M.; Keim, R.G.; Kennedy, D.B. Arch dimension changes from successful slow maxillary expansion of unilateral posterior crossbite. Angle Orthod. 2011, 81, 616–623. [Google Scholar] [CrossRef]
- Digregorio, M.V.; Fastuca, R.; Zecca, P.A.; Caprioglio, A.; Lagravère, M.O. Buccal bone plate thickness after rapid maxillary expansion in mixed and permanent dentitions. Am. J. Orthod. Dentofac. Orthop. 2019, 155, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Baccetti, T.; Franchi, L.; Cameron, C.G.; McNamara, J.A. Treatment Timing for Rapid Maxillary Expansion. Angle Orthod. 2001, 71, 343–350. [Google Scholar] [PubMed]
- Cerruto, C.; Ugolini, A.; Di Vece, L.; Doldo, T.; Caprioglio, A.; Silvestrini-Biavati, A. Cephalometric and dental arch changes to Haas-type rapid maxillary expander anchored to deciduous vs permanent molars: A multicenter, randomized controlled trial. J. Orofac. Orthop. 2017, 78, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Maspero, C.; Abate, A.; Cavagnetto, D.; Fama, A.; Stabilini, A.; Farronato, G.; Farronato, M. Operculectomy and spontaneous eruption of impacted second molars: A retrospective study. J. Biol. Regul. Homeost. Agents 2019, 33, 1909–1912. [Google Scholar]
- Abate, A.; Cavagnetto, D.; Fama, A.; Bellincioni, F.; Assandri, F. Efficacy of Operculectomy in the Treatment of 145 Cases with Unerupted Second Molars: A Retrospective Case–Control Study. Dent. J. 2020, 8, 65. [Google Scholar] [CrossRef]
- Farronato, M.; Cavagnetto, D.; Abate, A.; Cressoni, P.; Fama, A.; Maspero, C. Assessment of condylar volume and ramus height in JIA patients with unilateral and bilateral TMJ involvement: Retrospective case-control study. Clin. Oral. Investig. 2020, 24, 2635–2643. [Google Scholar] [CrossRef]
- Abate, A.; Cavagnetto, D.; Fama, A.; Maspero, C.; Farronato, G. Relationship between Breastfeeding and Malocclusion: A Systematic Review of the Literature. Nutrients 2020, 12, 3688. [Google Scholar] [CrossRef]


| Variable | Timing | Mean ± SD | Confidence Interval | I–III Interquartile | Shapiro Wilk | Pairwise Comparison * |
|---|---|---|---|---|---|---|
| BT-E-r (mm) | 1 | 1.31 ± 0.47 | (1.06–1.56) | (0.78–1.80) | 0.056 | <0.001 * |
| BT-E-r (mm) | 2 | 0.77 ± 0.36 | (0.58–0.97) | (0.56–0.98) | 0.008 | |
| BT-E-l (mm) | 1 | 1.35 ± 0.43 | (1.12–1.59) | (1.08–1.74) | 0.366 | 0.001 * |
| BT-E-l (mm) | 2 | 0.88 ± 0.36 | (0.69–1.07) | (0.60–1.02) | 0.095 | |
| BT-6-r (mm) | 1 | 2.41 ± 0.39 | (2.20–2.62) | (2.10–2.80) | 0.193 | 0.107 |
| BT-6-r (mm) | 2 | 2.18 ± 0.38 | (2.25–2.66) | (1.97–2.49) | 0.682 | |
| BT-6-l (mm) | 1 | 2.14 ± 0.45 | (1.90–2.38) | (2.13–2.84) | 0.665 | 0.074 |
| BT-6-l (mm) | 2 | 2.07 ± 0.38 | (1.87–2.28) | (1.84–2.50) | 0.391 | |
| BH-E-r (mm) | 1 | 7.00 ± 0.65 | (6.65–7.35) | (6.42–7.42) | 0.109 | 0.008 * |
| BH-E-r (mm) | 2 | 7.72 ± 0.80 | (7.30–8.14) | (6.99–8.53) | 0.113 | |
| BH-E-l (mm) | 1 | 6.80 ± 0.58 | (6.49–7.10) | (6.38–7.19) | 0.562 | 0.020 * |
| BH-E-l (mm) | 2 | 7.13 ± 1.70 | (6.22–8.04) | (6.92–7.92) | 0.000 | |
| BH-6-r (mm) | 1 | 7.55 ± 0.71 | (7.17–7.93) | (7.11–8.10) | 0.568 | 0.181 |
| BH-6-r (mm) | 2 | 8.17 ± 0.78 | (7.76–8.58) | (7.48–8.87) | 0.422 | |
| BH-6-l (mm) | 1 | 7.60 ± 0.65 | (7,25-7,95) | (7.14-7,94) | 0.401 | 0.118 |
| BH-6-l (mm) | 2 | 8.06 ± 0.91 | (7.56–8.74) | (7.10–8.73) | 0.193 | |
| TIP E (°) | 1 | 52.78 ± 10.11 | (47.39–58.16) | (44.75–61.53) | 0.176 | 0.067 |
| TIP E (°) | 2 | 60.20 ± 11.36 | (54.14–66.24) | (50.16–66.11) | 0.364 | |
| TIP-6 (°) | 1 | 57.17 ± 7.03 | (53.42–60.91) | (50.42–62.60) | 0.501 | 0.539 |
| TIP-6 (°) | 2 | 55.72 ± 7.87 | (51.53–59.91) | (48.76–60.37) | 0.796 | |
| IW-E (mm) | 1 | 29.5 ± 0.26 | (2.81–3.09) | (2.78–3.079) | 0.657 | <0.01 * |
| IW-E (mm) | 2 | 34.3 ± 0.23 | (3.31–3.56) | (3.27–3.619) | 0.930 | |
| IW-6 (mm) | 1 | 30.5 ± 0.32 | (2.88–3.22) | (2.85–3.24) | 0.099 | 0.002 * |
| IW-6 (mm) | 2 | 33.2 ± 0.27 | (3.17–3.46) | (3.06–3.46) | 0.637 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lanteri, V.; Cavagnetto, D.; Abate, A.; Mainardi, E.; Gaffuri, F.; Ugolini, A.; Maspero, C. Buccal Bone Changes Around First Permanent Molars and Second Primary Molars after Maxillary Expansion with a Low Compliance Ni–Ti Leaf Spring Expander. Int. J. Environ. Res. Public Health 2020, 17, 9104. https://doi.org/10.3390/ijerph17239104
Lanteri V, Cavagnetto D, Abate A, Mainardi E, Gaffuri F, Ugolini A, Maspero C. Buccal Bone Changes Around First Permanent Molars and Second Primary Molars after Maxillary Expansion with a Low Compliance Ni–Ti Leaf Spring Expander. International Journal of Environmental Research and Public Health. 2020; 17(23):9104. https://doi.org/10.3390/ijerph17239104
Chicago/Turabian StyleLanteri, Valentina, Davide Cavagnetto, Andrea Abate, Eleonora Mainardi, Francesca Gaffuri, Alessandro Ugolini, and Cinzia Maspero. 2020. "Buccal Bone Changes Around First Permanent Molars and Second Primary Molars after Maxillary Expansion with a Low Compliance Ni–Ti Leaf Spring Expander" International Journal of Environmental Research and Public Health 17, no. 23: 9104. https://doi.org/10.3390/ijerph17239104
APA StyleLanteri, V., Cavagnetto, D., Abate, A., Mainardi, E., Gaffuri, F., Ugolini, A., & Maspero, C. (2020). Buccal Bone Changes Around First Permanent Molars and Second Primary Molars after Maxillary Expansion with a Low Compliance Ni–Ti Leaf Spring Expander. International Journal of Environmental Research and Public Health, 17(23), 9104. https://doi.org/10.3390/ijerph17239104










