1. Background
Rural settings present numerous challenges around healthcare access for all patients, including long travel times, lack of specialized clinicians, lack of public transportation, and limited capacity for patient care [
1]. Transgender patients face particular disadvantages while attempting to access care in rural settings [
2]. Rural settings often lack specialty clinics and trained clinicians for transgender patients. Instead, care is provided by clinicians who are unfamiliar with transgender people and their specific healthcare needs [
3,
4,
5]. Transgender patients may avoid seeking medical care due to a history of traumatizing interactions with healthcare providers [
6] and the inability to locate affirming providers. Transgender people also report abuse and discrimination from healthcare workers in response to their nontraditional gender identities and sexual preferences [
6,
7,
8]. The development of healthcare systems serving transgender people is considered a “wicked problem”, i.e., one that is systematic, complex, and persistent [
9]. As such, multifaceted and complex interventions such as the one described in this study are needed to improve care for transgender people, particularly in rural settings [
9].
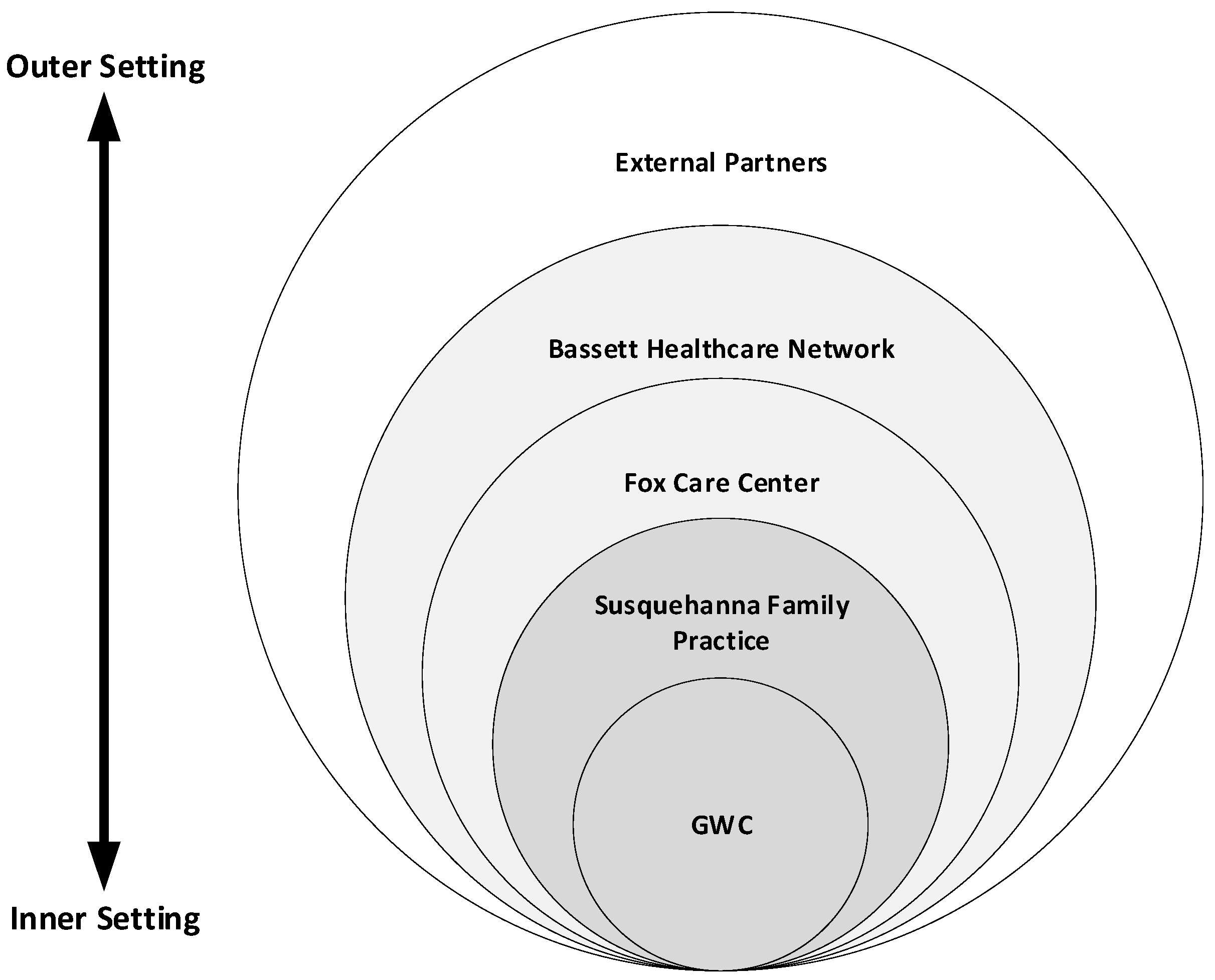
The Gender Wellness Center (GWC), located in rural upstate New York, was first established in 2015 and is a program of Susquehanna Family Practice. This primary care practice operates within a large multidisciplinary outpatient facility, the Fox Care Center, which is owned and operated by the eight-county Bassett Healthcare Network [
10]. These entities provide not-for-profit healthcare services for all patients. Activities within the GWC are led by a clinical director and mental health director and guided by input from a community advisory board. This setting is unique in that other centers for transgender health are typically found within a specialty care setting.
The establishment of the GWC was based on a growing community of transgender individuals seeking care from this practice, which is located nearly 200 miles northwest of New York City in a rural community that is devoid of other transgender-specific health services and where transgender service organizations are limited compared to large urban areas. One doctor provided care to one transgender patient in a family practice in 2007, an event that eventually led to the creation of the GWC as an embedded entity within that family practice. Over time, as additional patients presented asking for services, the clinician began to work with a local mental health provider to offer interdisciplinary care.
The clinicians became acutely aware of the unmet needs of this growing patient population, one with significant barriers to care and healthcare disparities. They recruited additional clinicians and searched for funding. In 2015, they were awarded a Robert Wood Johnson Foundation (RWJF) Clinical Scholars grant, with the goal of establishing a Center of Excellence (COE) in Transgender Health, the first of its kind in a rural area of the US [
11].
The goal of COEs is to develop specialized skills in an area of practice in order to improve outcomes for patients [
12]. To develop this COE, the GWC team first developed a mission and vision statement and identified six essential objectives, or prongs, for their center including the provision of trans-specific (1) medical care, (2) surgical care, (3) mental healthcare, (4) community-based research, (5) legal services, and (6) training and education. The team then participated in a three-part strategic planning retreat led by an external facilitator. The facilitator was a professional strategic planning consultant with a Master’s of Social Work degree. The strategic planning process included three 1–2-day, off-site retreats attended by three GWC medical providers, a case worker, three mental health providers, and the professional consultant. The initial session focused on brainstorming steps required for development and implementation of the Center of Excellence. Five strategic initiatives were agreed upon. Specific tasks related to these initiatives were identified and assigned to team members. Follow-up retreats, supplemented by monthly team meetings, were scheduled to monitor task completion.
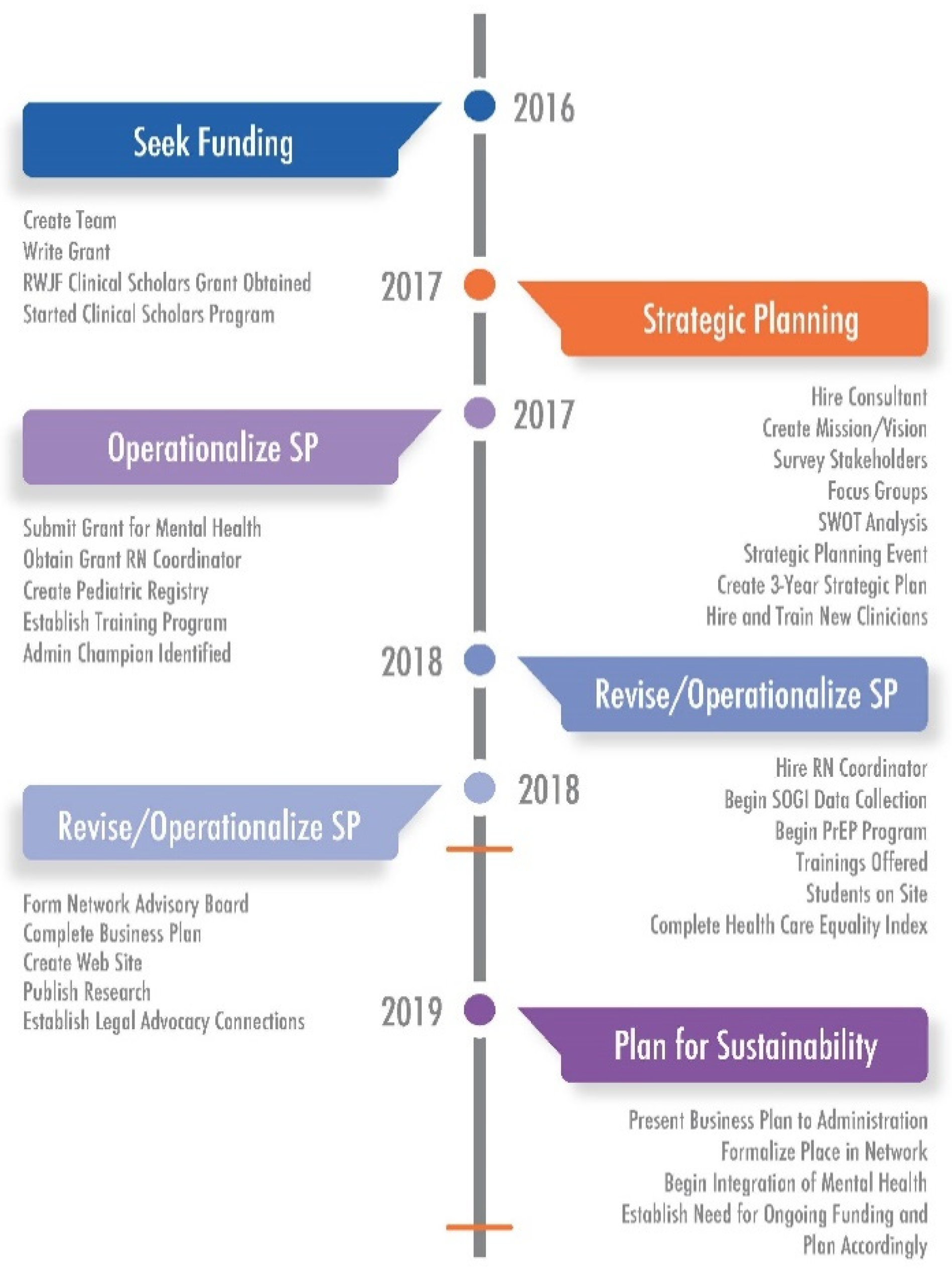
Figure 1 highlights the five arms of the strategic plan and key activities within each, while
Figure 2 shows the grant timeline, including two time points relevant to this study.
Efforts such as this one that address wicked socio-cultural problems with numerous moving parts are difficult to evaluate; however, in order to improve implementation efforts related to both the current effort as well as future initiatives, evaluation is necessary. The Consolidated Framework for Implementation Research (CFIR) evaluates implementation using several perspectives to explain what works, what does not work, and why in various settings [
13]. The CFIR is comprehensive in that it includes a range of implementation factors compiled from various other implementation frameworks and is, thus, suitable for the evaluation of complex initiatives such as the implementation of a COE in rural transgender care [
13]. Because of its comprehensive nature, the CFIR provides a framework to evaluate a multitude of potential barriers and facilitators (organized as constructs) to implementation efforts, including in healthcare settings [
14,
15]. CFIR has been described as “a powerful longitudinal evaluation tool that facilitated capture of thoughtful nuances and key voices throughout the implementation process [
16].”
Study Aims
The aims of this study were (1) to evaluate the implementation of the COE using the CFIR at two points in time during the grant cycle, i.e., at the midpoint and at the end of the grant (
Figure 2) and (2) to understand changes in barriers and facilitators to COE implementation over 18 months within the context of rural transgender healthcare.
3. Results
The results of this study are described in terms of each CFIR domain (intervention characteristics, process, characteristics of individuals, inner setting, and outer setting). These findings identified the constructs that act as both barriers and facilitators to implementation of this COE, as well as how these constructs changed from baseline to follow-up. Discussions of subconstructs were included under the main constructs under which they fell (i.e., engaging, implementation climate, and readiness for implementation).
3.1. Intervention Characteristics
Overall, there was little discussion of intervention characteristics in either the baseline or follow-up surveys. Four CFIR constructs did not have any text coded to them: design quality and packaging, intervention source, relative advantage, and trialability. Those constructs that were discussed saw a general trend of improved rating (from negative or neutral to positive rankings) over time, as well as an increase in specific positive examples at follow-up.
Evidence strength and quality: Over time, survey participants’ view of evidence supporting the COE changed in a positive way. At baseline, participants were largely aware of other COEs; however, they were unaware of the details or benefits of them and found it difficult to justify implementing their own COE. At follow-up, survey participants had more fully engaged in implementation of the COE and had seen firsthand evidence demonstrating the value of COEs, particularly in their own setting.
Complexity: Intervention complexity was a significant focus of participants during both the baseline and follow-up interviews. The tone in which participants discussed intervention complexity changed dramatically between the two surveys. At the time of the baseline survey, participants discussed the many moving parts of the COE (i.e., the five focus areas described in
Figure 1, with numerous action items to achieve each part) as barriers to implementing the COE. At follow-up, these complexities were reframed as challenges, and participants indicated their success in overcoming most of them.
Adaptability: Though complex with some rigidity built into the strategic plan and six-pronged approach to implementing the COE, survey participants felt that the COE model could be adequately adapted to the current setting at baseline and demonstrated this adaptability in the examples provided during follow-up. Specific adaptations included those embracing the rural setting compared to urban settings that are traditionally home to COEs.
Cost: Concerns over the cost of maintaining the COE and the GWC within the larger healthcare network were discussed at both the baseline and follow-up. At baseline, several participants expressed concern about costs and indicated that the team needed more evidence to demonstrate financial sustainability. In the follow-up survey, this concern persisted; however, participants had begun thinking about funding options for continuing the GWC and COE, particularly in terms of competitive grants to establish and maintain relevant services.
3.2. Process
Similar to intervention characteristics, there was limited discussion related to process measures, particularly in the baseline surveys. Those discussions that did take place were more positive at follow-up than at the baseline.
Engaging: The CFIR construct of engaging can relate to a number of individuals. In this study, the primary focus of discussions related to engaging clinical and administrative champions; specifically, those who could serve as a bridge between the GWC and larger healthcare network. At baseline and follow-up, the discussions primarily focused on the fact that such champions were needed in order to make progress and establish sustainability within the network. Despite success in garnering support from many members of the healthcare network, including local administrators, there was a consistent concern over the difficulty of engaging key administrators in the network executive leadership team to actively support the COE and GWC. Both at baseline and follow-up, participants also recognized the importance of engaging members of the transgender population. Participants described their development of a community advisory board comprised of transgender individuals to address this gap.
Planning: Survey participants primarily discussed the planning construct in the baseline survey, which took place soon after the strategic plan for implementing the COE was developed and initiated. In these discussions, participants described the benefits of including transgender patients in the planning process as well as the importance of developing a cohesive plan for project implementation. At follow-up, this discussion transitioned to appreciation of the strategic plan as a valuable tool for implementation and evaluation of progress toward achieving stated goals.
Executing: Discussion of how the COE implementation would be executed did not occur at baseline. However, at follow-up, several participants discussed both challenges and facilitators of execution. Participants described challenges around involving nonclinical staff with the COE, particularly those who were not engaged in the process early on or who did not share similar values. Additionally, participants discussed the development of a marketing plan for the GWC, with conflicting feedback regarding how well this strategy was carried out.
Reflecting and Evaluating: The benefits of strategic planning were demonstrated further at follow-up when participants reflected back on their planned processes and goals. Participants described a process of repeatedly evaluating progress toward implementation of goals and revising the strategic plan based on challenges or new opportunities. Reflection and evaluation took place in the form of gathering patient, community, and healthcare network feedback through GWC advisory boards as well as team discussions regarding progress.
3.3. Characteristics of Individuals
Particularly when discussing the GWC team, participants reported positive views of constructs within the characteristics of individuals’ domain, which remained largely unchanged from baseline to follow-up. Much of this discussion took place during the baseline survey, with relatively little discussion of the various characteristics of individuals at follow-up.
Individual identification with the organization: Participants largely indicated that they themselves had beliefs that closely aligned with the mission of the GWC. Participants also indicated that some nonclinical or supervisory staff did not share similar values or passion for the work. Those individuals were reportedly more likely to hold personal biases about the gender-affirming care conducted at the GWC, creating challenges in implementation of the COE.
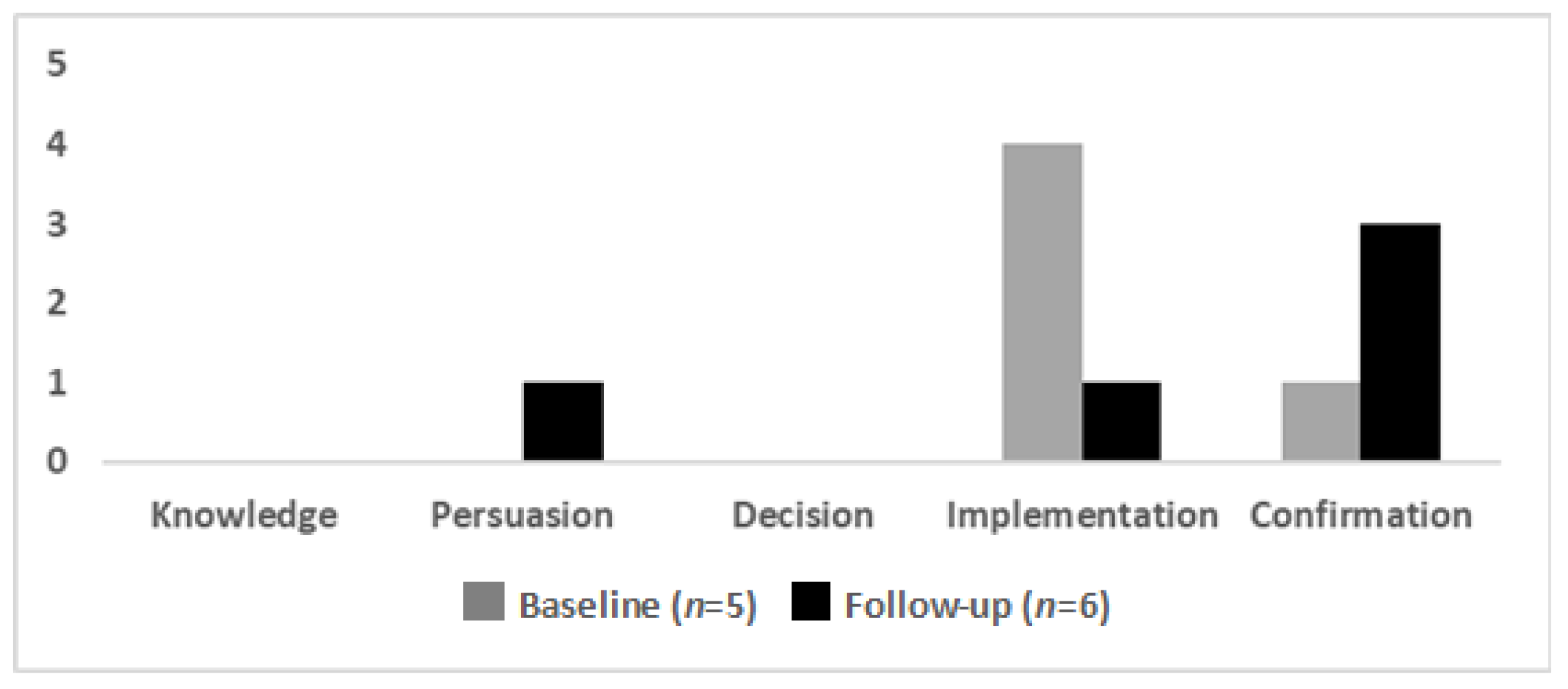
Individual stage of change: At baseline, four of the five participants reported being in the implementation stage, with one reporting being in the confirmation stage (
Figure 4). At follow-up, most participants (four of six) reported being in the confirmation stage, with one participant each in the implementation and persuasion stages (
Figure 4).
Knowledge and beliefs about the intervention: Similar to individual identification with the organization, most participants indicated (at baseline and follow-up) positive opinions about the COE and implementation within the GWC. In rare instances, participants indicated that they were unsure of the overall success of the COE but still believed in the importance of the overall mission. There was also discussion about external individuals and the groups who were critical of the COE and concern that these opinions could damage team efforts.
Self-efficacy: Discussions of self-efficacy were notably limited. At baseline, participants indicated that they believed in their abilities to implement the COE.
Other personal attributes: Similar to other constructs captured in the characteristics of individuals’ domain, the codes categorized within the other personal attributes’ construct related primarily to individual’s intrinsic desires to succeed with the COE implementation. These discussions did not change significantly from baseline to follow-up.
3.4. Inner Setting
Throughout this study, constructs considered under the inner setting domain were among the most highly discussed. The relative positivity of the constructs was fairly static from baseline to follow-up.
Culture: In terms of this implementation study, organizational culture needed to be examined on multiple levels: from within the GWC, as well as within the outer layers of the healthcare network. As survey participants described at both baseline and follow-up, the organizational culture within each layer of the healthcare network was complex with differences between and within each layer. As the layers of the healthcare network interacted around COE implementation, these complexities and differences became more apparent. Overall, this became one of the most heavily discussed constructs among participants, with two primary components of culture discussed: the GWC culture (and resulting interactions) and culture surrounding the acceptance of trans-identified people.
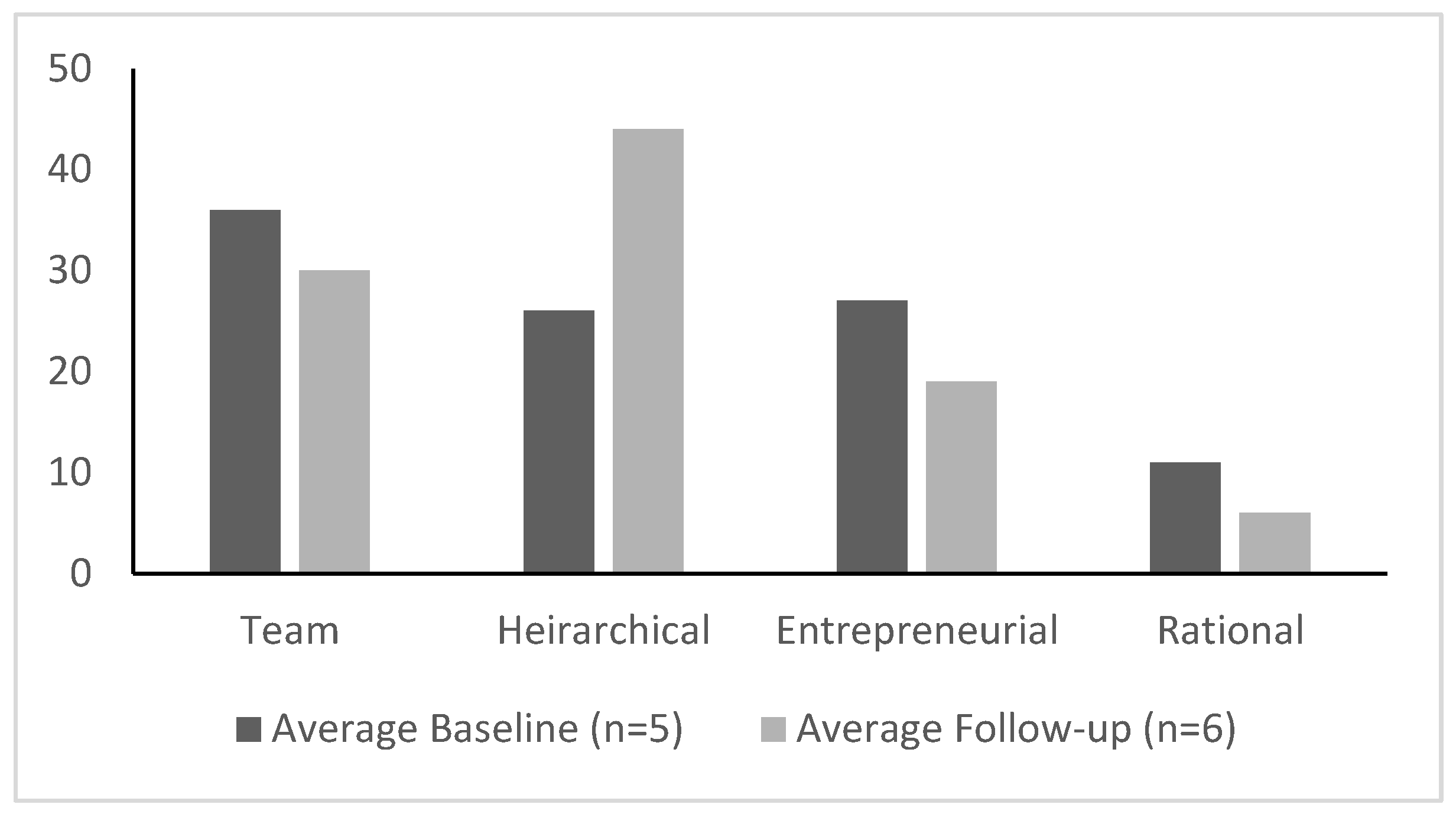
One of the most direct survey questions related to culture asked participants, “to what extent (%) would you characterize your culture as” each of four types, with the end result totaling 100%. These types included:
Team: A friendly workplace where leaders act like mentors, facilitators, and team builders. There is value placed on long-term development and doing things together.
Hierarchical: A structured and formalized workplace where leaders act like coordinators, monitors, and organizers. There is value placed on incremental change and doing things right.
Entrepreneurial: A dynamic workplace with leaders that stimulate COE. There is value placed on breakthroughs and doing things first.
Rational: A competitive workplace with leaders like hard drivers, producers, or competitors. There is value placed on short-term performance and doing things fast.
Within the GWC itself, measures of the type of workplace culture most actively present changed over time, with the primary culture shifting from a mixture of team and entrepreneurial at the baseline to hierarchical at follow-up (
Figure 5). In addition, at both baseline and follow-up, participants described relatively high amounts of conflict and negativity within the GWC but outside of the core implementation team. At baseline, there was a great deal of discussion about GWC and family practice staff feeling out of touch with the COE implementation and, therefore, without support. At follow-up, these concerns had improved.
In addition to these challenges, struggles related to support for the transgender population and the work of the GWC were present at both baseline and follow-up. At baseline, participants indicated that members of the GWC team were highly supportive of and provided affirming care to the transgender population. However, participants also indicated that outside of the GWC, individuals, including support staff in their own family practice, were sometimes less tolerant or supportive.
At follow-up, several participants indicated that as the GWC became better known and integrated into the larger healthcare network, there was a positive shift in network culture, with outside clinicians and nonclinical staff becoming more tolerant and affirming of the transgender population. Despite verbal support, a lack of follow-through with supportive actions often occurred, indicating that a full culture shift toward support of the GWC COE and transgender people had not yet been achieved.
Implementation climate: Much of the discussion on implementation climate focused on the inner-most implementation setting, the GWC itself. In this setting, participants generally were quite positive, describing an organizational incentive of improving patient care through the COE implementation. They described a positive learning climate with opportunities for education and the discussion and implementation of new ideas, as well as an appreciation for the strategic plan as a means of monitoring of goals and reviewing feedback.
Though most indicators of implementation climate were positive, there were mixed opinions of the compatibility of the COE with the existing environment at the time of the baseline survey. In addition, at both baseline and follow-up, participants described numerous competing priorities, particularly when it came to the responsibilities of the larger healthcare network. Finally, tension for change was shown to be variable in different parts of the healthcare network. The highest levels of tension for change were present in the immediate GWC; lower levels of tension for change existed in the more outer settings of the healthcare network.
Networks and communication: Communication issues, in particular, have been a challenge within the GWC over the course of the COE implementation. At both baseline and follow-up, participants indicated that communication within the GWC could be both tense and inconsistent. In terms of consistency, this related to both a lack of a standardized process for sharing new information, as well as challenges caused by the fact that several GWC mental health providers were not employed by the healthcare network and, therefore, unable to access patient records. At follow-up, participants expressed that communications about the GWC with other members of the larger healthcare network had improved over the course of the COE implementation.
Readiness for implementation: Due to the fact that the follow-up survey was conducted at the end of the grant cycle, much of the discussion related to readiness for implementation took place in the baseline survey. These constructs (leadership engagement, available resources, and access to knowledge and education) were described to a lesser extent in the follow-up survey.
Over the course of the study, participants indicated that network leadership engagement and support generally varied from person to person; however, at follow-up, participants indicated that there was overall more and better engagement by and support from leadership than at the baseline. At follow-up, several participants focused heavily on the resources that were lacking, specifically ancillary staff (mental health providers, administrative support, etc.), physical space, and time and energy of members of the GWC team. This lack of resources created barriers to smooth implementation of the COE. In addition, participants consistently described the educational opportunities that were available to them, noting, however, at baseline that individual’s ability to participate was somewhat limited due to time and funding constraints related to the consuming nature of project implementation.
Structural characteristics: From baseline to follow-up, responses did not change with regard to structural characteristics that could impact implementation. At both times, participants indicated that the relative newness of the GWC could be seen as a benefit to implementation, as there was ample opportunity to mold the GWC and COE to fit within the mission and vision of the larger healthcare network. While this was seen as a positive, COE implementation occurred during the restructuring of the healthcare network. Because this restructuring led to incorporation of the GWC into a new system, views were mixed with regard to the advantages and disadvantages of being included in a much larger network. This restructuring resulted in challenges adapting to a new organizational structure.
3.5. Outer Setting
Discussion of the outer setting constructs was limited in this analysis. Overall, the interactions between the GWC team, implementation of the COE, and the outer setting remained positive from the baseline through follow-up.
Cosmopolitanism: At both the baseline and follow-up surveys, participants discussed the benefits of collaborating with transgender healthcare providers outside of the healthcare network. Study participants indicated that making these connections through engagement in events and conferences was encouraged by GWC leadership.
External policy and incentives: Survey participants described the benefits of being the only organization in the region that provided interdisciplinary gender-affirming healthcare across the lifespan, with a commitment to the GWC’s six prongs for care (discussed previously). In addition, the implementation of the COE to improve these services was seen as positive compared to other regional services for transgender people.
Patient needs and resources: Throughout the study, survey participants consistently indicated that recognition of patient needs and the ability to meet those needs were a high priority for the GWC. At baseline, participants expressed concern that nonclinical GWC staff were less sensitive to the unique needs of transgender patients. This led to efforts to improve cultural competency through training and education. At follow-up, better patient transportation and health insurance were also identified as sources of gaps in care.
Peer pressure: At the baseline evaluations, participants described examples of peer pressure. This included the pressure to fit into the wider healthcare network, as well as the pressure to train other clinical departments within the healthcare network that also provide care for transgender patients. At follow-up, discussion around peer pressure focused on whether or not the GWC could continue to meet the healthcare network’s standards in terms of productivity and patient care metrics.
4. Discussion
This study highlights the implementation barriers and facilitators in the creation of a rural-based COE for transgender healthcare, which requires socio-cultural change in both the inner and outer settings of the health system. The multiple barriers to care and the stigma faced by transgender people require complex interventions, particularly in rural settings such as the one explored here. The results of this study are equally useful for GWC, aiming to improve implementation of the COE and sustain its efforts, as well as those outside of the GWC hoping to implement similar initiatives. These complexities can be seen in several individual constructs, as well as the interactions between them, as they have been described by participants in this study. Of particular interest in this study are the constructs within the inner and outer settings, which have created challenges to progress in assuring affirming care and fulfilling staffing needs, two arms of the COE strategy.
The constructs of organizational culture in the inner setting domain, engagement in the process domain, and individual stage of change and identification with the organization constructs in the characteristics of individuals’ domain were particularly important to implementation of the GWC’s COE. As previously described, while organizational culture is formally classified under the inner setting domain, this study considered the construct in terms of both the inner and outer settings. Similarly, engagement, which falls under the process domain, and the characteristics of individuals’ domain consider an array of inner and outer setting individuals. Prior studies have demonstrated that characteristics of individuals constructs are closely related to culture and engagement and together can influence implementation [
18,
19].
Comparing the baseline and follow-up surveys demonstrated a more positive outlook expressed during follow-up, despite ongoing challenges within the inner setting, including communication problems, lack of financial and physical space resources, tension over fitting into the network, and relative priority of the GWC compared to other initiatives within the healthcare network. Overall, the culture of the inner-most setting (GWC) was reported to be highly trans-affirming, while the outer settings, i.e., other parts of the healthcare network, were less affirming and less consistent in accepting and supporting people with diverse gender identities. It is likely that the differences in organizational cultures are closely connected to the characteristics of the individuals working in each setting. The relationship between individuals and their culture has the potential to affect constructs such as individual identification with the organization, individual stage of change, knowledge and beliefs about the intervention, and self-efficacy in both positive and negative ways.
Less trans-affirming attitudes and actions within healthcare networks is usually attributed to a lack of education and training regarding transgender people, their healthcare disparities, and their specific healthcare needs. Stigma and transphobia are well described and pervasive throughout healthcare cultures across the United States [
4]. Trainings in cultural competency and responsiveness are effective in increasing staff awareness and understanding of the transgender community and lead to decreased discrimination [
20,
21]. Though it was outside of the scope of this study to assess the other subcultures within the network, prior studies indicate that network training and education regarding cultural competency will be essential to wider network culture change.
The GWC’s individual and organizational cultural influences, and those of the larger healthcare network, as well as those outside of the network impact how individuals engage in COE activities [
22]. While study participants reported active support from many network administrators, staff, and clinicians, they also described a lack of meaningful engagement with some individuals in top leadership positions, including those most critical to champion efforts. Thus, at both baseline and follow-up, study participants described numerous competing priorities, particularly when it came to responsibilities set forth by the larger healthcare network. While it is possible that this lack of engagement stems from individual beliefs or organizational values regarding transgender healthcare, we did not assess the leadership’s level of engagement and, thus, we cannot comment further based on the results of this study. However, the complexity of engaging certain network-wide, shared services in all aspects of the network at all times is significant. In many cases, it may not be feasible for various specialty or primary care services to be as engaged in implementation as the GWC team would like. This is particularly true in a time of healthcare restructuring that ran parallel to the COE implementation.
Despite remaining challenges, the GWC team created a center with an excellent reputation and increased regional visibility. The GWC was successful in developing its infrastructure, expanding clinicians’ knowledge and skills in the area of transgender care, and advancing evidence-based practices–the remaining three arms of the COE strategy. Increasing numbers of patients sought care, often from areas outside the usual network catchment area. Despite increased patient volume, participants described financial successes and vulnerabilities. Several survey participants noted that the network was focused on financial viability whereas the GWC was focused on providing highly specialized care to a vulnerable minority, a setup for organizational conflict. Though these conflicts existed at both baseline and follow-up, there were improvements over the course of the COE implementation, likely due to the increased visibility of the GWC and movement toward the normalization of gender-affirming care. To further address concerns over the value of the GWC within the healthcare network, the GWC team developed a business plan to demonstrate its financial and cultural worth to the network. This included documentation of the GWC’s financial growth and sustainability, importance as a research and training institution, and plans to obtain additional grant funding for projects unrelated to direct patient care.
The GWC team developed a network of individuals within and outside the network who served as allies and change agents for project implementation, including administrative champions, patients, colleagues, and representative from other LGBT organizations across the state. These social networks allowed the GWC team to engage with people and programs with a similar interest in reducing healthcare disparities for at-risk populations.
Additional discussions focused on the complexity of the intervention, an issue related to self-efficacy of the GWC team, its knowledge of COEs, and beliefs about how implementation of a COE would affect its work. At baseline, complexity of the COE and implementation process was discussed as a barrier to implementation. At follow-up, complexity was seen as a challenge rather than a barrier. This suggests that firsthand experience in COE implementation led to a deeper understanding of the process, more positive knowledge and beliefs about providing gender-affirming care, and improved self-efficacy in the provision of care. The development and regular review of the COE strategic planning document helped to ease perceived complexities, creating a roadmap for implementation.
The constructs within the inner and outer setting domains were discussed in survey responses far more frequently, and with far more detail, than most others. This indicates the important influence, either positive or negative, that they had on implementing the COE compared to other constructs. Other constructs, such as networks and communications, presented challenges, while yet others (e.g., cosmopolitanism) provided additional support for implementation. Participant feedback did not suggest that any one of these factors was solely responsible for the overall success of the COE implementation.