Associations between Health-Related Physical Fitness and Cardiovascular Disease Risk Factors in Overweight and Obese University Staff
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Study Design
2.2. Study Variables
2.2.1. Health-Related Physical Fitness Measurement
2.2.2. Cardiovascular Disease Factors Measurement
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Zhou, M.; Wang, H.; Zhu, J.; Chen, W.; Wang, L.; Liu, S.; Li, Y.; Wang, L.; Liu, Y.; Yin, P.; et al. Cause-specific mortality for 240 causes in China during 1990-2013: A systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet 2016, 387, 251–272. [Google Scholar] [CrossRef]
- Liu, S.; Li, Y.; Zeng, X.; Wang, H.; Yin, P.; Wang, L.; Liu, Y.; Liu, J.; Qi, J.; Ran, S.; et al. Burden of Cardiovascular Diseases in China, 1990-2016: Findings From the 2016 Global Burden of Disease Study. JAMA Cardiol. 2019, 4, 342–352. [Google Scholar] [CrossRef]
- Yu, Q.; Wang, B.; Wang, Y.; Dai, C.L. Level and trend of cardiovascular disease mortality in China from 2002 to 2016. Zhonghua Xin Xue Guan Bing Za Zhi 2019, 47, 479–485. [Google Scholar] [PubMed]
- Shen, C.; Ge, J. Epidemic of Cardiovascular Disease in China: Current Perspective and Prospects for the Future. Circulation 2018, 138, 342–344. [Google Scholar] [CrossRef] [PubMed]
- Joseph, P.; Leong, D.; McKee, M.; Anand, S.S.; Schwalm, J.D.; Teo, K.; Mente, A.; Yusuf, S. Reducing the Global Burden of Cardiovascular Disease, Part 1: The Epidemiology and Risk Factors. Circ. Res. 2017, 121, 677–694. [Google Scholar] [CrossRef] [PubMed]
- Kleber, M.E.; Delgado, G.; Grammer, T.B.; Silbernagel, G.; Huang, J.; Kramer, B.K.; Ritz, E.; Marz, W. Uric Acid and Cardiovascular Events: A Mendelian Randomization Study. J. Am. Soc. Nephrol. 2015, 26, 2831–2838. [Google Scholar] [CrossRef] [PubMed]
- Chiang, K.M.; Tsay, Y.C.; Vincent, N.T.; Yang, H.C.; Huang, Y.T.; Chen, C.H.; Pan, W.H. Is Hyperuricemia, an Early-Onset Metabolic Disorder, Causally Associated with Cardiovascular Disease Events in Han Chinese? J. Clin. Med. 2019, 8, 1202. [Google Scholar] [CrossRef]
- Khan, S.S.; Ning, H.; Wilkins, J.T.; Allen, N.; Carnethon, M.; Berry, J.D.; Sweis, R.N.; Lloyd-Jones, D.M. Association of Body Mass Index With Lifetime Risk of Cardiovascular Disease and Compression of Morbidity. JAMA Cardiol. 2018, 3, 280–287. [Google Scholar] [CrossRef]
- Barry, V.W.; Caputo, J.L.; Kang, M. The Joint Association of Fitness and Fatness on Cardiovascular Disease Mortality: A Meta-Analysis. Prog. Cardiovasc. Dis. 2018, 61, 136–141. [Google Scholar] [CrossRef]
- Abdullah, A.; Wolfe, R.; Stoelwinder, J.U.; de Courten, M.; Stevenson, C.; Walls, H.L.; Peeters, A. The number of years lived with obesity and the risk of all-cause and cause-specific mortality. Int. J. Epidemiol. 2011, 40, 985–996. [Google Scholar] [CrossRef]
- Ortega, F.B.; Lavie, C.J.; Blair, S.N. Obesity and Cardiovascular Disease. Circ. Res. 2016, 118, 1752–1770. [Google Scholar] [CrossRef] [PubMed]
- Penha, J.; Gazolla, F.M.; Carvalho, C.; Madeira, I.R.; Rodrigues-Junior, F.; Machado, E.A.; Sicuro, F.L.; Farinatti, P.; Bouskela, E.; Collett-Solberg, P.F. Physical fitness and activity, metabolic profile, adipokines and endothelial function in children. J. Pediatr. 2019, 95, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Medrano, M.; Arenaza, L.; Migueles, J.H.; Rodriguez-Vigil, B.; Ruiz, J.R.; Labayen, I. Associations of physical activity and fitness with hepatic steatosis, liver enzymes, and insulin resistance in children with overweight/obesity. Pediatr. Diabetes. 2020, 21, 565–574. [Google Scholar] [CrossRef] [PubMed]
- Lima, T.R.; Martins, P.C.; Guerra, P.H.; Silva, D. Muscular strength and cardiovascular risk factors in adults: Systematic review. Phys. Sportsmed. 2020, 1, 1–13. [Google Scholar] [CrossRef]
- Chen, G.C.; Arthur, R.; Iyengar, N.M.; Kamensky, V.; Xue, X.; Wassertheil-Smoller, S.; Allison, M.A.; Shadyab, A.H.; Wild, R.A.; Sun, Y.; et al. Association between regional body fat and cardiovascular disease risk among postmenopausal women with normal body mass index. Eur. Heart J. 2019, 40, 2849–2855. [Google Scholar] [CrossRef]
- Barry, V.W.; Baruth, M.; Beets, M.W.; Durstine, J.L.; Liu, J.; Blair, S.N. Fitness vs. fatness on all-cause mortality: A meta-analysis. Prog. Cardiovasc. Dis. 2014, 56, 382–390. [Google Scholar] [CrossRef]
- Castro-Pinero, J.; Perez-Bey, A.; Segura-Jimenez, V.; Aparicio, V.A.; Gomez-Martinez, S.; Izquierdo-Gomez, R.; Marcos, A.; Ruiz, J.R. Cardiorespiratory Fitness Cutoff Points for Early Detection of Present and Future Cardiovascular Risk in Children: A 2-Year Follow-up Study. Mayo Clin. Proc. 2017, 92, 1753–1762. [Google Scholar] [CrossRef]
- Simons, S.O.; Elliott, A.; Sastry, M.; Hendriks, J.M.; Arzt, M.; Rienstra, M.; Kalman, J.M.; Heidbuchel, H.; Nattel, S.; Wesseling, G.; et al. Chronic obstructive pulmonary disease and atrial fibrillation: An interdisciplinary perspective. Eur. Heart J. 2020. [Google Scholar] [CrossRef]
- Lawman, H.G.; Troiano, R.P.; Perna, F.M.; Wang, C.Y.; Fryar, C.D.; Ogden, C.L. Associations of Relative Handgrip Strength and Cardiovascular Disease Biomarkers in U.S. Adults, 2011-2012. Am. J. Prev. Med. 2016, 50, 677–683. [Google Scholar] [CrossRef]
- Van der Palen, J.; Rea, T.D.; Manolio, T.A.; Lumley, T.; Newman, A.B.; Tracy, R.P.; Enright, P.L.; Psaty, B.M. Respiratory muscle strength and the risk of incident cardiovascular events. Thorax 2004, 59, 1063–1067. [Google Scholar] [CrossRef]
- Garcia-Esquinas, E.; Rodriguez-Artalejo, F. Association between serum uric acid concentrations and grip strength: Is there effect modification by age? Clin. Nutr. 2018, 37, 566–572. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.V.; Hung, C.Y.; Li, C.M.; Lin, Y.H.; Wang, T.G.; Tsai, K.S.; Han, D.S. Reduced flexibility associated with metabolic syndrome in community-dwelling elders. PLoS ONE 2015, 10, e117167. [Google Scholar] [CrossRef] [PubMed]
- Sita, C.; Sachita, S.; Mausumi, B.; Raghunath, M. A study on cardiovascular disease risk factors among faculty members of a tertiary care teaching institute of Kolkata. J. Community Health Manag. 2018, 5, 67–71. [Google Scholar] [CrossRef]
- Cheong, S.M.; Kandiah, M.; Chinna, K.; Chan, Y.M.; Saad, H.A. Prevalence of obesity and factors associated with it in a worksite setting in Malaysia. J. Community Health 2010, 35, 698–705. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.F. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults--study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed. Environ. Sci. 2002, 15, 83–96. [Google Scholar]
- Yeh, W.C.; Tsao, Y.C.; Li, W.C.; Tzeng, I.S.; Chen, L.S.; Chen, J.Y. Elevated triglyceride-to-HDL cholesterol ratio is an indicator for insulin resistance in middle-aged and elderly Taiwanese population: A cross-sectional study. Lipids Health Dis. 2019, 18, 176. [Google Scholar] [CrossRef]
- Tsushima, Y.; Nishizawa, H.; Tochino, Y.; Nakatsuji, H.; Sekimoto, R.; Nagao, H.; Shirakura, T.; Kato, K.; Imaizumi, K.; Takahashi, H.; et al. Uric acid secretion from adipose tissue and its increase in obesity. J. Biol. Chem. 2013, 288, 27138–27149. [Google Scholar] [CrossRef]
- Nagao, H.; Nishizawa, H.; Tanaka, Y.; Fukata, T.; Mizushima, T.; Furuno, M.; Bamba, T.; Tsushima, Y.; Fujishima, Y.; Kita, S.; et al. Hypoxanthine Secretion from Human Adipose Tissue and its Increase in Hypoxia. Obesity 2018, 26, 1168–1178. [Google Scholar] [CrossRef]
- Yamada, A.; Sato, K.K.; Kinuhata, S.; Uehara, S.; Endo, G.; Hikita, Y.; Fujimoto, W.Y.; Boyko, E.J.; Hayashi, T. Association of Visceral Fat and Liver Fat With Hyperuricemia. Arthritis Care Res. 2016, 68, 553–561. [Google Scholar] [CrossRef]
- Huang, X.; Jiang, X.; Wang, L.; Chen, L.; Wu, Y.; Gao, P.; Hua, F. Visceral adipose accumulation increased the risk of hyperuricemia among middle-aged and elderly adults: A population-based study. J. Transl. Med. 2019, 17, 341. [Google Scholar] [CrossRef]
- Kawamoto, R.; Ninomiya, D.; Kasai, Y.; Kusunoki, T.; Ohtsuka, N.; Kumagi, T.; Abe, M. Serum Uric Acid Is Positively Associated with Handgrip Strength among Japanese Community-Dwelling Elderly Women. PLoS ONE 2016, 11, e151044. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.R.; Zhang, Q.; Chen, L.F.; Xu, K.Y.; Xia, J.Y.; Li, S.M.; Yang, Y.M. Characteristics of hyperuricemia in older adults in China and possible associations with sarcopenia. Aging Med. 2018, 1, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zhang, D.; Pang, Z.; Jiang, W.; Wang, S.; Tan, Q. Association of serum uric acid level with muscle strength and cognitive function among Chinese aged 50-74 years. Geriatr. Gerontol. Int. 2013, 13, 672–677. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.W.; Tian, H.Y.; He, J.; Wang, C.; Qiu, R.; Chen, Y.M. Elevated Serum Uric Acid Is Associated with Greater Bone Mineral Density and Skeletal Muscle Mass in Middle-Aged and Older Adults. PLoS ONE 2016, 11, e154692. [Google Scholar] [CrossRef]
- Macchi, C.; Molino-Lova, R.; Polcaro, P.; Guarducci, L.; Lauretani, F.; Cecchi, F.; Bandinelli, S.; Guralnik, J.M.; Ferrucci, L. Higher circulating levels of uric acid are prospectively associated with better muscle function in older persons. Mech. Ageing Dev. 2008, 129, 522–527. [Google Scholar] [CrossRef]
- Lee, J.; Hong, Y.S.; Park, S.H.; Kang, K.Y. High serum uric acid level is associated with greater handgrip strength in the aged population. Arthritis Res. Ther. 2019, 21, 73. [Google Scholar] [CrossRef]
- Molino-Lova, R.; Sofi, F.; Pasquini, G.; Vannetti, F.; Del, R.S.; Vassalle, C.; Clerici, M.; Sorbi, S.; Macchi, C. Higher uric acid serum levels are associated with better muscle function in the oldest old: Results from the Mugello Study. Eur. J. Intern. Med. 2017, 41, 39–43. [Google Scholar] [CrossRef]
- Park, C.; Obi, Y.; Streja, E.; Rhee, C.M.; Catabay, C.J.; Vaziri, N.D.; Kovesdy, C.P.; Kalantar-Zadeh, K. Serum uric acid, protein intake and mortality in hemodialysis patients. Nephrol Dial. Transpl. 2017, 32, 1750–1757. [Google Scholar] [CrossRef]
- Alexandrov, N.V.; Eelderink, C.; Singh-Povel, C.M.; Navis, G.J.; Bakker, S.; Corpeleijn, E. Dietary Protein Sources and Muscle Mass over the Life Course: The Lifelines Cohort Study. Nutrients 2018, 10, 1471. [Google Scholar] [CrossRef]
- Aparicio, V.A.; Marin-Jimenez, N.; Coll-Risco, I.; de la Flor-Alemany, M.; Baena-Garcia, L.; Acosta-Manzano, P.; Aranda, P. Doctor, ask your perimenopausal patient about her physical fitness; association of self-reported physical fitness with cardiometabolic and mental health in perimenopausal women: The FLAMENCO project. Menopause 2019, 26, 1146–1153. [Google Scholar] [CrossRef]
- Won, H.Y.; Park, J.B.; Park, E.Y.; Riew, K.D. Effect of hyperglycemia on apoptosis of notochordal cells and intervertebral disc degeneration in diabetic rats. J. Neurosurg Spine 2009, 11, 741–748. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Markova, D.; Anderson, D.G.; Zheng, Z.; Shapiro, I.M.; Risbud, M.V. TNF-alpha and IL-1beta promote a disintegrin-like and metalloprotease with thrombospondin type I motif-5-mediated aggrecan degradation through syndecan-4 in intervertebral disc. J. Biol. Chem. 2011, 286, 39738–39749. [Google Scholar] [CrossRef] [PubMed]
- Dagistan, Y.; Cukur, S.; Dagistan, E.; Gezici, A.R. Importance of IL-6, MMP-1, IGF-1, and BAX Levels in Lumbar Herniated Disks and Posterior Longitudinal Ligament in Patients with Sciatic Pain. World Neurosurg. 2015, 84, 1739–1746. [Google Scholar] [CrossRef] [PubMed]
- Gregorio-Arenas, E.; Ruiz-Cabello, P.; Camiletti-Moiron, D.; Moratalla-Cecilia, N.; Aranda, P.; Lopez-Jurado, M.; Llopis, J.; Aparicio, V.A. The associations between physical fitness and cardiometabolic risk and body-size phenotypes in perimenopausal women. Maturitas 2016, 92, 162–167. [Google Scholar] [CrossRef]
- Supriya, R.; Yu, A.P.; Lee, P.H.; Lai, C.W.; Cheng, K.K.; Yau, S.Y.; Chan, L.W.; Yung, B.Y.; Siu, P.M. Yoga training modulates adipokines in adults with high-normal blood pressure and metabolic syndrome. Scand. J. Med. Sci Sports 2018, 28, 1130–1138. [Google Scholar] [CrossRef]
- Konieczna, J.; Abete, I.; Galmes, A.M.; Babio, N.; Colom, A.; Zulet, M.A.; Estruch, R.; Vidal, J.; Toledo, E.; Diaz-Lopez, A.; et al. Body adiposity indicators and cardiometabolic risk: Cross-sectional analysis in participants from the PREDIMED-Plus trial. Clin. Nutr. 2019, 38, 1883–1891. [Google Scholar] [CrossRef]
- Keswell, D.; Tootla, M.; Goedecke, J.H. Associations between body fat distribution, insulin resistance and dyslipidaemia in black and white South African women. Cardiovasc. J. Afr. 2016, 27, 177–183. [Google Scholar] [CrossRef]
- Ormazabal, V.; Nair, S.; Elfeky, O.; Aguayo, C.; Salomon, C.; Zuniga, F.A. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc. Diabetol. 2018, 17, 122. [Google Scholar] [CrossRef]
- Lee, W.J.; Peng, L.N.; Chiou, S.T.; Chen, L.K. Relative Handgrip Strength Is a Simple Indicator of Cardiometabolic Risk among Middle-Aged and Older People: A Nationwide Population-Based Study in Taiwan. PLoS ONE 2016, 11, e160876. [Google Scholar] [CrossRef]
- Lee, M.R.; Jung, S.M.; Kim, H.S.; Kim, Y.B. Association of muscle strength with cardiovascular risk in Korean adults: Findings from the Korea National Health and Nutrition Examination Survey (KNHANES) VI to VII (2014-2016). Medicine 2018, 97, e13240. [Google Scholar] [CrossRef]
- Giudice, J.; Taylor, J.M. Muscle as a paracrine and endocrine organ. Curr. Opin. Pharmacol. 2017, 34, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Bostrom, P.; Wu, J.; Jedrychowski, M.P.; Korde, A.; Ye, L.; Lo, J.C.; Rasbach, K.A.; Bostrom, E.A.; Choi, J.H.; Long, J.Z.; et al. A PGC1-alpha-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature 2012, 481, 463–468. [Google Scholar] [CrossRef] [PubMed]
- Seldin, M.M.; Peterson, J.M.; Byerly, M.S.; Wei, Z.; Wong, G.W. Myonectin (CTRP15), a novel myokine that links skeletal muscle to systemic lipid homeostasis. J. Biol. Chem. 2012, 287, 11968–11980. [Google Scholar] [CrossRef] [PubMed]
| Men | Women | All | |
|---|---|---|---|
| Sample size (n, %) | 231 (67.9%) | 109 (32.1%) | 340 (100%) |
| Age (n, %) | |||
| ≤30 years | 20 (8.7%) | 11 (10.1%) | 31 (9.1%) |
| 31–40 years | 80 (34.6%) | 41 (37.6%) | 121 (35.6%) |
| 41–50 years | 60 (26.0%) | 31 (28.4%) | 91 (26.8%) |
| 51–60 years | 71 (30.7%) | 26 (23.9%) | 97 (28.5%) |
| BMI (n, %) | |||
| 24–27.9 (overweight) | 192 (83.1%) | 92 (84.4%) | 284 (83.5%) |
| ≥ 28.0 (obese) | 39 (16.9%) | 17 (15.6%) | 56 (16.5%) |
| HPF indicators | |||
| Skeletal muscle mass (kg) a | 33.07 ± 2.86 | 24.40 ± 2.49 | 30.29 ± 4.86 |
| Skeletal muscle mass index (kg/m2) a | 11.00 ± 0.62 | 9.17 ± 0.68 | 10.43 ± 1.06 |
| Body fat mass (kg) b | 20.00 (5.80) | 24.10 (5.00) | 21.20 (6.40) |
| Body fat percentage (%)b | 25.00 (5.06) | 35.55 (4.34) | 27.48 (9.64) |
| Grip strength (kg) b | 36.50 (9.40) | 25.60 (5.20) | 33.60 (11.10) |
| Sit-and-reach (cm) b | 4.10 (11.50) | 9.15 (11.80) | 5.90 (11.00) |
| Vital capacity (mL) a | 3957.94 ± 844.10 | 2708.75 ± 624.92 | 3564.65 ± 979.17 |
| Vital capacity index (mL/kg) a | 50.66 ± 10.59 | 39.71 ± 9.54 | 47.40 ± 11.44 |
| CVD risk factors | |||
| UA (umol/L) b | 384.00 (72.00) | 301.50 (65.00) | 363.00 (97.00) |
| TG (mmol/L) b | 1.35 (0.79) | 1.10 (0.65) | 1.27 (0.79) |
| HDL-C (mmol/L) a | 1.32 ± 0.24 | 1.54 ± 0.25 | 1.38 ± 0.42 |
| LDL-C (mmol/L) b | 2.96 (0.74) | 2.65 (0.91) | 2.92 (0.86) |
| TG/HDL-C ratio b | 1.01 (0.70) | 0.70 (0.53) | 0.91 (0.72) |
| GLU (mmol/L) a | 5.03 ± 0.43 | 5.07 ± 0.42 | 5.05 ± 0.51 |
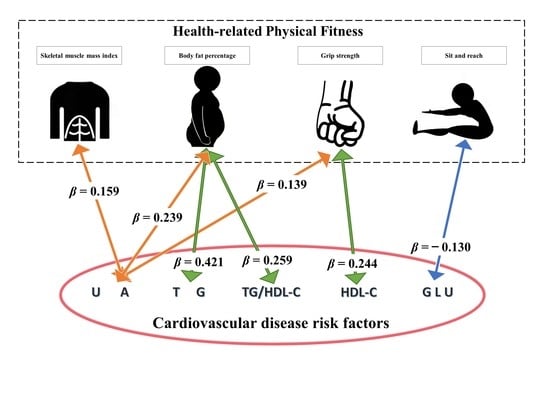
| Dependent Variables a | Independent Variables a | β | β (95%CI) | SE | p | R2 |
|---|---|---|---|---|---|---|
| SMI | 0.159 | (0.001, 0.318) | 0.081 | 0.049 * | ||
| BFP | 0.239 | (0.076, 0.402) | 0.083 | 0.004 * | ||
| UA | GS | 0.139 | (0.018, 0.259) | 0.061 | 0.024 * | 0.363 |
| SRT | 0.027 | (−0.068, 0.122) | 0.048 | 0.579 | ||
| VCI | 0.031 | (−0.086, 0.147) | 0.059 | 0.608 | ||
| SMI | 0.162 | (−0.030, 0.353) | 0.097 | 0.098 | ||
| BFP | 0.421 | (0.226, 0.617) | 0.099 | 0.000 * | ||
| TG | GS | 0.031 | (−0.113, 0.175) | 0.073 | 0.673 | 0.098 |
| SRT | −0.036 | (−0.149, 0.078) | 0.058 | 0.538 | ||
| VCI | 0.047 | (−0.092, 0.187) | 0.071 | 0.507 | ||
| SMI | −0.183 | (−0.370, 0.003) | 0.095 | 0.054 | ||
| BFP | 0.014 | (−0.177, 0.205) | 0.097 | 0.887 | ||
| HDL-C | GS | 0.244 | (0.103, 0.385) | 0.072 | 0.001 * | 0.128 |
| SRT | −0.009 | (−0.121, 0.103) | 0.057 | 0.871 | ||
| VCI | 0.066 | (−0.072, 0.203) | 0.070 | 0.349 | ||
| SMI | 0.045 | (−0.148, 0.238) | 0.054 | 0.646 | ||
| BFP | 0.131 | (−0.068, 0.330) | 0.010 | 0.197 | ||
| LDL-C | GS | −0.009 | (−0.155, 0.136) | 0.005 | 0.900 | 0.063 |
| SRT | 0.097 | (−0.019, 0.212) | 0.004 | 0.102 | ||
| VCI | 0.004 | (−0.138, 0.147) | 0.004 | 0.954 | ||
| SMI | 0.150 | (−0.043, 0.344) | 0.099 | 0.128 | ||
| BFP | 0.259 | (0.061, 0.457) | 0.101 | 0.011 * | ||
| TG/HDL-C | GS | −0.054 | (−0.201, 0.092) | 0.074 | 0.465 | 0.070 |
| SRT | −0.029 | (−0.145, 0.087) | 0.059 | 0.622 | ||
| VCI | −0.008 | (−0.151, 0.134) | 0.072 | 0.909 | ||
| SMI | 0.181 | (−0.007, 0.369) | 0.096 | 0.059 | ||
| BFP | 0.128 | (−0.065, 0.321) | 0.098 | 0.192 | ||
| GLU | GS | 0.035 | (−0.107, 0.177) | 0.072 | 0.630 | 0.083 |
| SRT | −0.130 | (−0.243, −0.017) | 0.057 | 0.024 * | ||
| VCI | −0.052 | (−0.190, 0.086) | 0.070 | 0.461 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, J.; Zhou, Y.; Pan, X.; Li, X.; Long, J.; Zhang, H.; Zhang, J. Associations between Health-Related Physical Fitness and Cardiovascular Disease Risk Factors in Overweight and Obese University Staff. Int. J. Environ. Res. Public Health 2020, 17, 9031. https://doi.org/10.3390/ijerph17239031
Chen J, Zhou Y, Pan X, Li X, Long J, Zhang H, Zhang J. Associations between Health-Related Physical Fitness and Cardiovascular Disease Risk Factors in Overweight and Obese University Staff. International Journal of Environmental Research and Public Health. 2020; 17(23):9031. https://doi.org/10.3390/ijerph17239031
Chicago/Turabian StyleChen, Jiangang, Yuan Zhou, Xinliang Pan, Xiaolong Li, Jiamin Long, Hui Zhang, and Jing Zhang. 2020. "Associations between Health-Related Physical Fitness and Cardiovascular Disease Risk Factors in Overweight and Obese University Staff" International Journal of Environmental Research and Public Health 17, no. 23: 9031. https://doi.org/10.3390/ijerph17239031
APA StyleChen, J., Zhou, Y., Pan, X., Li, X., Long, J., Zhang, H., & Zhang, J. (2020). Associations between Health-Related Physical Fitness and Cardiovascular Disease Risk Factors in Overweight and Obese University Staff. International Journal of Environmental Research and Public Health, 17(23), 9031. https://doi.org/10.3390/ijerph17239031