Quality of Life and Mental Health in Mothers and Fathers Caring for Children and Adolescents with Rare Diseases Requiring Long-Term Mechanical Ventilation
Abstract
1. Introduction
- Are there differences in the distribution of QoL and mental health between mothers and fathers caring for children and adolescents with rare diseases requiring mechanical ventilation?
- Is there a significant association between coping and supportive factors and the psychosocial outcomes of QoL and mental health of affected parents?
2. Materials and Methods
2.1. Study Design
2.2. Variables and Instruments
2.3. Sample
2.4. Statistics
3. Results
3.1. Differences between Mothers and Fathers in Quality of Life
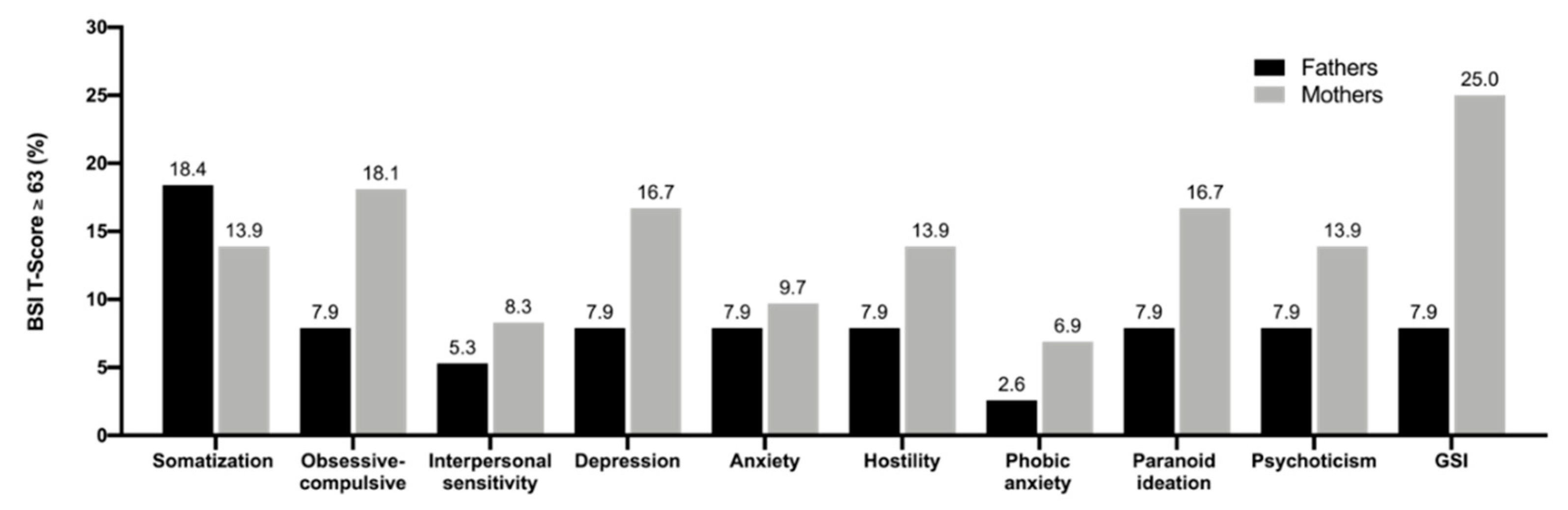
3.2. Mental Health
3.3. Differences between Mothers and Fathers in Coping and Supportive Factors
3.4. Predictors of QoL and Mental Health
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- European Commission Rare Diseases. European Commission, European Union. Available online: http://europa.eu.int/comm/health/ph_threats/non_com/rare_diseases_en.htm (accessed on 20 January 2020).
- EURORDIS Rare Diseases: Understanding this Public Health Priority. Available online: http://beta.eurordis.org/IMG/pdf/princeps_document-EN.pdf (accessed on 8 October 2019).
- Pelentsov, L.J.; Fielder, A.L.; Laws, T.A.; Esterman, A.J. The supportive care needs of parents with a child with a rare disease: Results of an online survey. BMC Fam. Pract. 2016, 17, 88. [Google Scholar] [CrossRef]
- Nguengang Wakap, S.; Lambert, D.M.; Olry, A.; Rodwell, C.; Gueydan, C.; Lanneau, V.; Murphy, D.; Le Cam, Y.; Rath, A. Estimating cumulative point prevalence of rare diseases: Analysis of the Orphanet database. Eur. J. Hum. Genet. 2020, 28, 165–173. [Google Scholar] [CrossRef]
- Anderson, M.; Elliott, E.; Zurynski, Y. Australian families living with rare disease: Experiences of diagnosis, health services use and needs for psychosocial support. Orphanet J. Rare Dis. 2013, 8, 22. [Google Scholar] [CrossRef] [PubMed]
- Zurynski, Y.; Deverell, M.; Dalkeith, T.; Johnson, S.; Christodoulou, J.; Leonard, H.; Elliott, E. Australian children living with rare diseases: Experiences of diagnosis and perceived consequences of diagnostic delays. Orphanet J. Rare Dis. 2017, 12, 68. [Google Scholar] [CrossRef] [PubMed]
- Swallow, V.; Macfadyen, A.; Santacroce, S.J.; Lambert, H. Fathers’ contributions to the management of their child’s long-term medical condition: A narrative review of the literature. Health Expect. 2012, 15, 157–175. [Google Scholar] [CrossRef]
- Pelentsov, L.J.; Laws, T.A.; Esterman, A.J. The supportive care needs of parents caring for a child with a rare disease: A scoping review. Disabil. Health J. 2015, 8, 475–491. [Google Scholar] [CrossRef]
- Raina, P.; O’Donnell, M.; Schwellnus, H.; Rosenbaum, P.; King, G.; Brehaut, J.; Russell, D.; Swinton, M.; King, S.; Wong, M.; et al. Caregiving process and caregiver burden: Conceptual models to guide research and practice. BMC Pediatrics 2004, 4, 1. [Google Scholar] [CrossRef]
- Pearlin, L.I.; Mullan, J.T.; Semple, S.J.; Skaff, M.M. Caregiving and the Stress Process: An Overview of Concepts and Their Measures 1. Gerontologist 1990, 30, 583–594. [Google Scholar] [CrossRef]
- King, G.; King, S.; Rosenbaum, P.; Goffin, R. Family-Centered Caregiving and Well-Beingof Parents of Children With Disabilities:Linking Process With Outcome. J. Pediatrics Psychol. 1999, 24, 41–53. [Google Scholar] [CrossRef]
- Wallander, J.L.; Varni, J.W.; Babani, L.; Dehaan, C.B.; Wilcox, K.T.; Banis, H.T. The Social Environment and the Adaptation of Mothers of Physically Handicapped Children 1. J. Pediatrics Psychol. 1989, 14, 371–387. [Google Scholar] [CrossRef]
- The World Health Organization Quality of Life Group The World Health Organization quality of life assessment (WHOQOL): Position paper from the World Health Organization. Soc. Sci. Med. 1995, 41, 1403–1409. [CrossRef]
- Galderisi, S.; Heinz, A.; Kastrup, M.; Beezhold, J.; Sartorius, N. Toward a new definition of mental health. World Psychiatry 2015, 14, 231–233. [Google Scholar] [CrossRef]
- Raina, P.; Rosenbaum, P.; Brehaut, J.; Walter, S.D.; Russell, D.; Swinton, M.; Zhu, B.; Wood, E. The Health and Well-Being of Caregivers of Children With Cerebral Palsy. Pediatrics 2005, 115, e626–e636. [Google Scholar] [CrossRef]
- Waldboth, V.; Patch, C.; Mahrer-Imhof, R.; Metcalfe, A. Living a normal life in an extraordinary way: A systematic review investigating experiences of families of young people’s transition into adulthood when affected by a genetic and chronic childhood condition. Int. J. Nurs. Stud. 2016, 62, 44–59. [Google Scholar] [CrossRef]
- Mesman, G.R.; Kuo, D.Z.; Carroll, J.L.; Ward, W.L. The Impact of Technology Dependence on Children and Their Families. J. Pediatrics Health Care 2013, 27, 451–459. [Google Scholar] [CrossRef]
- Carnevale, F.A.; Alexander, E.; Davis, M.; Rennick, J.; Troini, R. Daily living with distress and enrichment: The moral experience of families with ventilator-assisted children at home. Pediatrics 2006, 117, e48–e60. [Google Scholar] [CrossRef]
- Lee, J.; Lynn, F. Mental health and well-being of parents caring for a ventilator-dependent child. Nurs. Child. Young People 2017, 29, 33–40. [Google Scholar] [CrossRef]
- Chan, Y.H.; Lim, C.Z.-R.; Bautista, D.; Malhotra, R.; Østbye, T. The Health and Well-Being of Caregivers of Technologically Dependent Children. Glob. Pediatr. Health 2019, 6. [Google Scholar] [CrossRef]
- Kuster, P.A.; Badr, L.K. Mental health of mothers caring for ventilator-assisted children at home. Issues Ment. Health Nurs. 2006, 27, 817–835. [Google Scholar] [CrossRef]
- Toly, V.B.; Bolton, F.P.; Musil, C.M.; Carl, J.C. Families With Children Who Are Technology Dependent: Normalization and Family Functioning. West. J. Nurs. Res. 2012, 34, 52–71. [Google Scholar] [CrossRef]
- Toly, V.B.; Musil, C.M.; Carl, J.C. A longitudinal study of families with technology-dependent children. Res. Nurs. Health 2012, 35, 40–54. [Google Scholar] [CrossRef]
- Johannsen, J.; Fuhrmann, L.; Grolle, B.; Morgenstern, L.; Wiegand-Grefe, S.; Denecke, J. The impact of long-term ventilator-use on health-related quality of life and the mental health of children with neuromuscular diseases and their families: Need for a revised perspective? Health Qual. Life Outcomes 2020, 18, 1–11. [Google Scholar] [CrossRef]
- Goldbeck, L.; Storck, M. Das Ulmer Lebensqualitäts-Inventar für Eltern chronisch kranker Kinder (ULQIE). Z. Klin. Psychol. Psychother. 2002, 31, 31–39. [Google Scholar] [CrossRef]
- Derogatis, L.R.; Melisaratos, N. The Brief Symptom Inventory: An Introductory Report. Psychol. Med. 1983, 13, 595–605. [Google Scholar] [CrossRef]
- Franke, H. Brief Symptom Inventory von L.R. Derogatis (Kurzform der SCL-90-R). Deutsche Version. Manual; Beltz Test Gesellschaft: Göttingen, Germany, 2000. [Google Scholar]
- Geisheim, C.; Hahlweg, K.; Fiegenbaum, W.; Frank, M. Das Brief Symptom Inventory (BSI) als Instrument zur Qualitätssicherung in der Psychotherapie. Diagnostica 2002, 48, 28–36. [Google Scholar] [CrossRef]
- McCubbin, H.I.; McCubbin, M.A.; Cauble, E.; Goldbeck, L. Fragebogen zur elterlichen krankheitsbewältigung: Coping health inventory for parents (CHIP)-deutsche version. Kindh. Entwickl. 2001, 10, 28–35. [Google Scholar] [CrossRef]
- Meltzer, H. Development of a Common Instrument for Mental health; Nosikov, A., Gudex, C., Eds.; EUROHIS: Developing Common Instruments for Health Surveys; IOS Press: Amsterdam, The Netherlands, 2003. [Google Scholar]
- Kocalevent, R.D.; Berg, L.; Beutel, M.E.; Hinz, A.; Zenger, M.; Härter, M.; Nater, U.; Brähler, E. Social support in the general population: Standardization of the Oslo social support scale (OSSS-3). BMC Psychol. 2018, 6, 31. [Google Scholar] [CrossRef]
- Cierpka, M.; Frevert, G. Die Familienbögen: Ein Inventar zur Einschätzung von Familienfunktionen; Hogrefe: Goettingen, Germany, 1994. [Google Scholar]
- Windisch, W.; Dreher, M.; Geiseler, J.; Siemon, K.; Brambring, J.; Dellweg, D.; Grolle, B.; Hirschfeld, S.; Köhnlein, T.; Mellies, U.; et al. Guidelines for non-invasive and invasive home mechanical ventilation for treatment of chronic respiratory failure-update 2017. Pneumologie 2017, 71, 722–795. [Google Scholar]
- Winkler, J.; Stolzenberg, H. Adjustierung des Sozialen-Schicht-Index für die Anwendung im Kinder- und Jugendgesundheitssurvey (KiGGS); Wismarer Diskussionspapiere: Wismar, Germany, 2009. [Google Scholar]
- Baumbusch, J.; Mayer, S.; Sloan-Yip, I. Alone in a Crowd? Parents of Children with Rare Diseases’ Experiences of Navigating the Healthcare System. J. Genet. Couns. 2019, 28, 80–90. [Google Scholar] [CrossRef]
- Wiedebusch, S.; Konrad, M.; Foppe, H.; Reichwald-Klugger, E.; Schaefer, F.; Schreiber, V.; Muthny, F.A. Health-related quality of life, psychosocial strains, and coping in parents of children with chronic renal failure. Pediatr. Nephrol. 2010, 25, 1477–1485. [Google Scholar] [CrossRef]
- Rensen, N.; Steur, L.M.H.; Schepers, S.A.; Merks, J.H.M.; Moll, A.C.; Kaspers, G.J.L.; Van Litsenburg, R.R.L.; Grootenhuis, M.A. Determinants of health-related quality of life proxy rating disagreement between caregivers of children with cancer. Qual. Life Res. 2020, 29, 901–912. [Google Scholar] [CrossRef]
- Witvliet, M.; Sleeboom, C.; De Jong, J.; Van Dijk, A.; Zwaveling, S.; Van Der Steeg, A. Anxiety and quality of life of parents with children diagnosed with an anorectal malformation or hirschsprung disease. Eur. J. Pediatrics Surg. 2014, 24, 70–74. [Google Scholar] [CrossRef]
- Jones, B.L.; Pelletier, W.; Decker, C.; Barczyk, A.; Dungan, S.S. Fathers of children with cancer: A descriptive synthesis of the literature. Soc. Work Health Care 2010, 49, 458–493. [Google Scholar] [CrossRef]
- van Oers, H.A.; Haverman, L.; Limperg, P.F.; van Dijk-Lokkart, E.M.; Maurice-Stam, H.; Grootenhuis, M.A. Anxiety and depression in mothers and fathers of a chronically ill child. Matern. Child Health J. 2014, 18, 1993–2002. [Google Scholar] [CrossRef]
- Malm-Buatsi, E.; Aston, C.E.; Ryan, J.; Tao, Y.; Palmer, B.W.; Kropp, B.P.; Klein, J.; Wisniewski, A.B.; Frimberger, D. Mental health and parenting characteristics of caregivers of children with spina bifida. J. Pediatrics Urol. 2015, 11, 65.e1–65.e7. [Google Scholar] [CrossRef]
| Characteristics | n | % |
|---|---|---|
| Children’s gender | ||
| Female | 26 | 34.7 |
| Male | 49 | 65.3 |
| Marital status | ||
| Single Parent | 8 | 10.5 |
| Married | 53 | 71.0 |
| Divorced | 14 | 18.4 |
| Socioeconomic status of the families | ||
| Low (n; %) | 10 | 13.3 |
| Moderate (n; %) | 33 | 44.0 |
| High (n; %) | 32 | 42.7 |
| Family structure | ||
| One-child family | 54 | 75.0 |
| Two-child family | 14 | 19.4 |
| Three-child family | 7 | 9.7 |
| Child’s dysfunction | ||
| Isolated pathology | 6 | 7.9 |
| Multiple disabilities without progression | 23 | 30.3 |
| Multiple disabilities with progression | 4 | 5.3 |
| Neuromuscular diseases | 43 | 56.6 |
| Ventilation | ||
| No Mask | 25 | 33.3 |
| Mask | 25 | 33.3 |
| Tracheostoma | 25 | 33.3 |
| Mothers | Fathers | p | d | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | |||
| Physical and daily functioning | 2.6 | 0.75 | 2.8 | 0.68 | 0.087 | −0.27 |
| Satisfaction with family | 3.1 | 0.68 | 3.2 | 0.67 | 0.749 | −0.05 |
| Emotional stability | 2.2 | 0.79 | 2.4 | 0.76 | 0.080 | −0.25 |
| Self-development | 1.8 | 0.83 | 1.8 | 0.77 | 0.973 | 0.01 |
| Well-being | 2.6 | 0.66 | 3.1 | 0.63 | 0.001 *** | −0.58 |
| Total score | 2.5 | 0.54 | 2.7 | 0.52 | 0.014 * | −0.37 |
| Mothers | Fathers | p | d | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | |||
| Somatization | 2.5 | 3.54 | 1.4 | 2.31 | 0.093 | 0.340 |
| Obsessive-compulsive | 3.5 | 3.41 | 2.4 | 2.83 | 0.077 | 0.326 |
| Interpersonal sensitivity | 1.9 | 2.11 | 0.8 | 1.89 | 0.003 ** | 0.510 |
| Depression | 2.1 | 2.14 | 1.3 | 2.36 | 0.066 | 0.356 |
| Anxiety | 2.2 | 2.23 | 1.0 | 1.42 | 0.003 ** | 0.588 |
| Hostility | 2.2 | 2.07 | 1.3 | 1.78 | 0.020 * | 0.456 |
| Phobic anxiety | 0.6 | 1.14 | 0.4 | 0.71 | 0.157 | 0.266 |
| Paranoid ideation | 2.3 | 2.74 | 1.6 | 2.38 | 0.169 | 0.263 |
| Psychoticism | 0.9 | 1.26 | 0.6 | 1.34 | 0.257 | 0.202 |
| Global severity index | 19.9 | 16.48 | 11.9 | 13.77 | 0.006 ** | 0.446 |
| Mothers | Fathers | p | d | |||
|---|---|---|---|---|---|---|
| M | SD | M | SD | |||
| CHIP-FAM | 40.7 | 8.35 | 38.0 | 8.01 | 0.067 | 0.328 |
| CHIP-SUP | 38.6 | 6.87 | 37.1 | 7.31 | 0.180 | 0.218 |
| CHIP-MED | 15.7 | 4.29 | 14.1 | 4.05 | 0.033 * | 0.378 |
| CHIP-Total | 95.0 | 17.67 | 89.2 | 17.58 | 0.056 | 0.329 |
| OSSS | 9.7 | 2.76 | 9.7 | 2.39 | 0.839 | 0.022 |
| FAM | 23.9 | 7.02 | 24.9 | 7.29 | 0.407 | 0.141 |
| Quality of Life | Mental Health | |||
|---|---|---|---|---|
| Mothers | Fathers | Mothers | Fathers | |
| CHIP-FAM | 0.12 | −0.01 | −0.12 | −0.02 |
| CHIP-SUP | 0.34 ** | 0.08 | −0.30 * | −0.17 |
| CHIP-MED | 0.25 * | 0.07 | −0.25 * | −0.16 |
| CHIP-Total | 0.25 * | 0.05 | −0.23 * | −0.12 |
| OSSS | 0.37 ** | 0.21 | −0.47 ** | −0.07 |
| FAM | −0.46 ** | −0.34 ** | 0.44 ** | 0.30 * |
| Predictors of Quality of Life | ||||||||
| Mothers | Fathers | |||||||
| b | SE | p | b | SE | p | |||
| Intercept | 1.840 | 0.574 | 0.001 ** | 3.274 | 0.780 | 0.001 *** | ||
| Age of child | 0.024 | 0.011 | 0.030 * | 0.001 | 0.015 | 0.937 | ||
| Ventilation | 0.013 | 0.122 | 0.914 | −0.158 | 0.161 | 0.327 | ||
| CHIP-Total | 0.005 | 0.003 | 0.114 | 0.001 | 0.005 | 0.995 | ||
| OSSS | 0.045 | 0.027 | 0.102 | 0.038 | 0.035 | 0.278 | ||
| FAM | −0.022 | 0.010 | 0.038 * | −0.033 | 0.013 | 0.009 ** | ||
| F | df | p | R2adj | F | df | p | R2adj | |
| 8.12 | 5.69 | 0.001 | 0.319 | 3.09 | 5.69 | 0.039 | 0.121 | |
| Predictors of Mental Health | ||||||||
| Mothers | Fathers | |||||||
| b | SE | p | b | SE | p | |||
| Intercept | 40.589 | 15.186 | 0.008 ** | 0.595 | 13.819 | 0.966 | ||
| Age of child | −0.388 | 0.308 | 0.208 | −0.222 | 0.218 | 0.307 | ||
| Ventilation | 2.008 | 3.415 | 0.557 | 6.138 | 2.502 | 0.014 * | ||
| CHIP-Total | −0.132 | 0.094 | 0.163 | −0.074 | 0.090 | 0.411 | ||
| OSSS | −1.949 | 0.690 | 0.005 ** | 0.032 | 0.591 | 0.956 | ||
| FAM | 0.541 | 0.277 | 0.051 | 0.632 | 0.225 | 0.005 ** | ||
| F | df | p | R2adj | F | df | p | R2adj | |
| 7.97 | 5.69 | 0.001 | 0.316 | 3.19 | 5.69 | 0.015 | 0.128 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Boettcher, J.; Denecke, J.; Barkmann, C.; Wiegand-Grefe, S. Quality of Life and Mental Health in Mothers and Fathers Caring for Children and Adolescents with Rare Diseases Requiring Long-Term Mechanical Ventilation. Int. J. Environ. Res. Public Health 2020, 17, 8975. https://doi.org/10.3390/ijerph17238975
Boettcher J, Denecke J, Barkmann C, Wiegand-Grefe S. Quality of Life and Mental Health in Mothers and Fathers Caring for Children and Adolescents with Rare Diseases Requiring Long-Term Mechanical Ventilation. International Journal of Environmental Research and Public Health. 2020; 17(23):8975. https://doi.org/10.3390/ijerph17238975
Chicago/Turabian StyleBoettcher, Johannes, Jonas Denecke, Claus Barkmann, and Silke Wiegand-Grefe. 2020. "Quality of Life and Mental Health in Mothers and Fathers Caring for Children and Adolescents with Rare Diseases Requiring Long-Term Mechanical Ventilation" International Journal of Environmental Research and Public Health 17, no. 23: 8975. https://doi.org/10.3390/ijerph17238975
APA StyleBoettcher, J., Denecke, J., Barkmann, C., & Wiegand-Grefe, S. (2020). Quality of Life and Mental Health in Mothers and Fathers Caring for Children and Adolescents with Rare Diseases Requiring Long-Term Mechanical Ventilation. International Journal of Environmental Research and Public Health, 17(23), 8975. https://doi.org/10.3390/ijerph17238975






