Cervical Cancer Screening and Human Papillomavirus Vaccination among Korean Sexual Minority Women by Sex of Their Sexual Partners
Abstract
1. Introduction
2. Materials and Methods
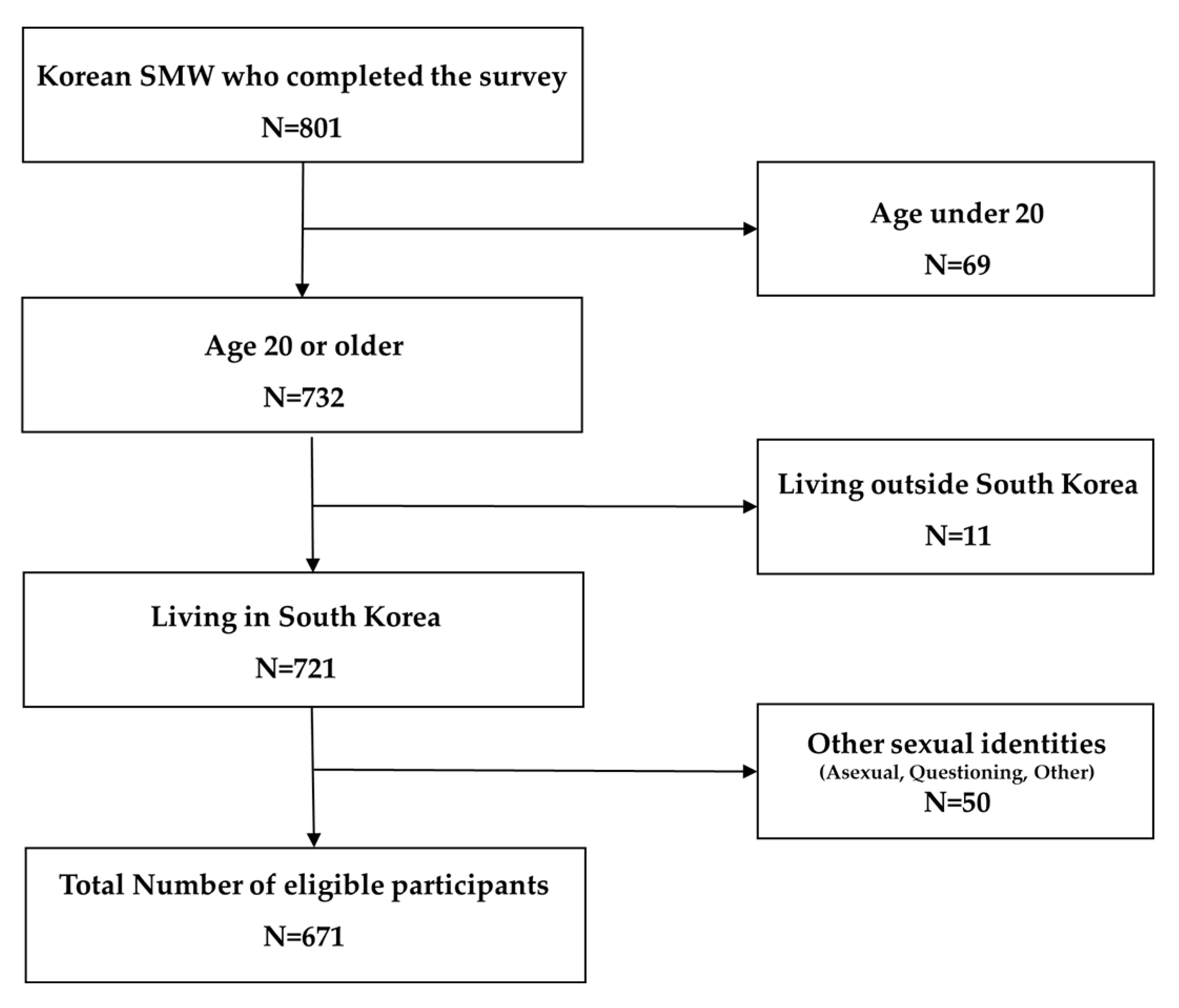
2.1. Study Design and Participants
2.2. Study Variables
2.2.1. Sexual Identity and Sex of Sexual Partners
2.2.2. Cervical Cancer Screening and HPV Vaccination Completion
2.2.3. Medical History
2.2.4. Reasons for Being Unscreened or Unvaccinated
2.2.5. Sociodemographic Variables
2.3. Statistical Analysis
2.4. Ethics Declarations
3. Results
3.1. Sociodemographic Characteristics by Sex of Sexual Partner
3.2. Logistic Regression Analysis of Cervical Cancer Screening
3.3. Logistic Regression Analysis of HPV Vaccination
3.4. Reasons for Being Unscreened for Cervical Cancer or Unvaccinated against HPV
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Small, W., Jr.; Bacon, M.A.; Bajaj, A.; Chuang, L.T.; Fisher, B.J.; Harkenrider, M.M.; Jhingran, A.; Kitchener, H.C.; Mileshkin, L.R.; Viswanathan, A.N. Cervical cancer: A global health crisis. Cancer 2017, 123, 2404–2412. [Google Scholar] [CrossRef]
- Curry, S.J.; Krist, A.H.; Owens, D.K.; Barry, M.J.; Caughey, A.B.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Kemper, A.R.; Kubik, M.J.J. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA 2018, 320, 674–686. [Google Scholar] [CrossRef]
- Meites, E.; Szilagyi, P.G.; Chesson, H.W.; Unger, E.R.; Romero, J.R.; Markowitz, L.E. Human papillomavirus vaccination for adults: Updated recommendations of the Advisory Committee on Immunization Practices. Am. J. Transplant. 2019, 19, 3202–3206. [Google Scholar] [CrossRef]
- Porsch, L.M.; Zhang, H.; Dayananda, I.; Dean, G. Comparing Receipt of Cervical Cancer Screening and Completion of Human Papillomavirus Vaccination Using a New Construct of Sexual Orientation: A Serial Cross-Sectional Study. Lgbt Health 2019, 6, 184–191. [Google Scholar] [CrossRef]
- Agénor, M.; Krieger, N.; Austin, S.B.; Haneuse, S.; Gottlieb, B.R. Sexual orientation disparities in Papanicolaou test use among US women: The role of sexual and reproductive health services. Am. J. Public Health 2014, 104, e68–e73. [Google Scholar] [CrossRef]
- Matthews, A.K.; Brandenburg, D.L.; Johnson, T.P.; Hughes, T.L. Correlates of underutilization of gynecological cancer screening among lesbian and heterosexual women. Prev. Med. 2004, 38, 105–113. [Google Scholar] [CrossRef]
- Tracy, J.K.; Schluterman, N.H.; Greenberg, D.R. Understanding cervical cancer screening among lesbians: A national survey. BMC Public Health 2013, 13, 442. [Google Scholar] [CrossRef]
- Charlton, B.M.; Corliss, H.L.; Missmer, S.A.; Frazier, A.L.; Rosario, M.; Kahn, J.A.; Austin, S.B. Influence of hormonal contraceptive use and health beliefs on sexual orientation disparities in Papanicolaou test use. Am. J. Public Health 2014, 104, 319–325. [Google Scholar] [CrossRef]
- Curmi, C.; Peters, K.; Salamonson, Y. Lesbians’ attitudes and practices of cervical cancer screening: A qualitative study. BMC Women’s Health 2014, 14, 2. [Google Scholar] [CrossRef]
- Marrazzo, J.M.; Stine, K.; Koutsky, L.A. Genital human papillomavirus infection in women who have sex with women: A review. Am. J. Obstet. Gynecol. 2000, 183, 770–774. [Google Scholar] [CrossRef]
- Anderson, T.A.; Schick, V.; Herbenick, D.; Dodge, B.; Fortenberry, J. A study of human papillomavirus on vaginally inserted sex toys, before and after cleaning, among women who have sex with women and men. Sex. Transm. Infect. 2014, 90, 529–531. [Google Scholar] [CrossRef] [PubMed]
- Agénor, M.; Krieger, N.; Austin, S.B.; Haneuse, S.; Gottlieb, B.R. At the intersection of sexual orientation, race/ethnicity, and cervical cancer screening: Assessing Pap test use disparities by sex of sexual partners among black, Latina, and white US women. Soc. Sci. Med. 2014, 116, 110–118. [Google Scholar] [CrossRef] [PubMed]
- Gates, G.; Badgett, M.L. Best Practices for Asking Questions about Sexual Orientation on Surveys. Available online: https://escholarship.org/uc/item/706057d5 (accessed on 1 November 2020).
- Moon, E.-K.; Oh, C.-M.; Won, Y.-J.; Lee, J.-K.; Jung, K.-W.; Cho, H.; Jun, J.K.; Lim, M.C.; Ki, M. Trends and age-period-cohort effects on the incidence and mortality rate of cervical cancer in Korea. Cancer Res. Treat. 2017, 49, 526. [Google Scholar] [CrossRef]
- Kim, J.; Lee, D.; Son, K.-B.; Bae, S. The Burden of Cervical Cancer in Korea: A Population-Based Study. Int. J. Environ. Res. Public Health 2020, 17, 6308. [Google Scholar] [CrossRef]
- Min, K.-J.; Lee, Y.J.; Suh, M.; Yoo, C.W.; Lim, M.C.; Choi, J.; Ki, M.; Kim, Y.-M.; Kim, J.-W.; Kim, J.-H.; et al. The Korean guideline for cervical cancer screening. J. Gynecol. Oncol. 2015, 26, 232–239. [Google Scholar] [CrossRef]
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef]
- Korea Centers for Disease Control & Prevention. Guidelines for Adult Immunization, 2nd ed.; Korea Centers for Disease Control & Prevention: Chungbuk, Korea, 2018.
- Yi, H.; Lee, H.; Park, J.; Choi, B.; Kim, S.-S. Health Disparities Between Lesbian, Gay, and Bisexual Adults and the General Population in South Korea: Rainbow Connection Project I. Epidemiol. Health 2017, 39, e2017046. [Google Scholar] [CrossRef]
- Na, T.; Kim, J.; Ryu, M.; Lee, S.; Chang, S.; Jeong, H. Key Results of the South Korean LGBTI Community Social Needs Assessment Survey; Korean Gay Men’s Human Rights Group Chingusai: Seoul, Korea, 2014. [Google Scholar]
- Lee, H.; Operario, D.; Yi, H.; Choo, S.; Kim, S.-S. Internalized Homophobia, Depressive Symptoms, and Suicidal Ideation Among Lesbian, Gay, and Bisexual Adults in South Korea: An Age-Stratified Analysis. Lgbt Health 2019, 6, 393–399. [Google Scholar] [CrossRef]
- Youatt, E.J.; Harris, L.H.; Harper, G.W.; Janz, N.K.; Bauermeister, J.A. Sexual health care services among young adult sexual minority women. Sex. Res. Soc. Policy 2017, 14, 345–357. [Google Scholar] [CrossRef]
- Statistics Korea. The Survey of Household Finances and Living Conditions (SFLC) in 2017. Available online: http://kostat.go.kr/portal/eng/pressReleases/6/3/index.board (accessed on 16 November 2020).
- Douglas, C.; Deacon, R.; Mooney-Somers, J. Pap smear rates among Australian community-attached lesbian and bisexual women: Some good news but disparities persist. Sex. Health 2015, 12, 249–256. [Google Scholar] [CrossRef]
- Solazzo, A.L.; Gorman, B.K.; Denney, J.T. Cancer screening utilization among US women: How mammogram and pap test use varies among heterosexual, lesbian, and bisexual women. Popul. Res. Policy Rev. 2017, 36, 357–377. [Google Scholar] [CrossRef]
- Organisation for Economic Co-operation and Development. Health Care Utilization Cervical Cancer Screening, Programme Data; OECD Statistics: Paris, France, 2020; Volume 2020. [Google Scholar]
- National Health Insuarance Service. National Health Screening Statistical Yearbook; National Health Insurance Service: Wonju City, Korea, 2018.
- Park, S.; Chang, S.; Chung, C. Context of barriers to Pap testing in Korean women. Appl. Nurs. Res. 2006, 19, 177–181. [Google Scholar] [CrossRef]
- Kang, K.-A.; Kim, S.-J.; Noriyo, K.; Cho, H.; Lim, Y.-S. A prediction of behavioral intention on Pap screening test in college women: A path model. J. Korean Public Health Nurs. 2017, 31, 135–148. [Google Scholar] [CrossRef][Green Version]
- Greene, M.Z.; Meghani, S.H.; Sommers, M.S.; Hughes, T.L. Health Care-Related Correlates of Cervical Cancer Screening among Sexual Minority Women: An Integrative Review. J. Midwifery Women’s Health 2018, 63, 550–577. [Google Scholar] [CrossRef]
- Kang, J.; Kim, K. Human papillomavirus vaccine predictors among US adults aged 18 to 45 by sexual orientation. West. J. Nurs. Res. 2019, 41, 1761–1789. [Google Scholar] [CrossRef]
- McRee, A.-L.; Katz, M.L.; Paskett, E.D.; Reiter, P.L. HPV vaccination among lesbian and bisexual women: Findings from a national survey of young adults. Vaccine 2014, 32, 4736–4742. [Google Scholar] [CrossRef]
- Kim, J. The relationship of health beliefs with information sources and HPV vaccine acceptance among young adults in Korea. Int. J. Environ. Res. Public Health 2018, 15, 673. [Google Scholar] [CrossRef]
- Park, H. Predictors of HPV vaccination status in female nursing university students: HPV related knowledge and perception. J. Korean Soc. Sch. Health 2016, 29, 123–131. [Google Scholar] [CrossRef]
| Total | Sex of Sexual Partner 1 | p-Value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Male Only/Both | Female Only | No Partner | |||||||
| N | % | N | % | N | % | N | % | ||
| Total | 671 | 100.0 | 266 | 100.0 | 294 | 100.0 | 111 | 100.0 | |
| Age group | <0.001 | ||||||||
| 20–24 | 302 | 45.0 | 97 | 36.5 | 117 | 39.8 | 88 | 79.3 | |
| 25–29 | 194 | 28.9 | 90 | 33.8 | 89 | 30.3 | 15 | 13.5 | |
| 30–34 | 100 | 14.9 | 49 | 18.4 | 47 | 16.0 | 4 | 3.6 | |
| 35–39 | 44 | 6.6 | 16 | 6.0 | 24 | 8.2 | 4 | 3.6 | |
| 40–51 | 31 | 4.6 | 14 | 5.3 | 17 | 5.8 | 0 | 0.0 | |
| Median (Q1–Q3) | 25 (22–30) | 26 (23–30) | 26 (23–30) | 22 (21–24) | |||||
| Education level | 0.623 | ||||||||
| High school or under | 55 | 8.2 | 25 | 9.4 | 21 | 7.1 | 9 | 8.1 | |
| Above college | 616 | 91.8 | 241 | 90.6 | 273 | 92.9 | 102 | 91.9 | |
| Annual income | 0.265 | ||||||||
| <$50,000 | 476 | 70.9 | 198 | 74.4 | 201 | 68.4 | 77 | 69.4 | |
| ≥$50,000 | 195 | 29.1 | 68 | 25.6 | 93 | 31.6 | 34 | 30.6 | |
| Job | <0.001 | ||||||||
| Student | 293 | 43.7 | 95 | 35.7 | 125 | 42.5 | 73 | 65.8 | |
| Employed | 318 | 47.4 | 144 | 54.1 | 143 | 48.6 | 31 | 27.9 | |
| Unemployed | 60 | 8.9 | 27 | 10.2 | 26 | 8.8 | 7 | 6.3 | |
| Current partner | <0.001 | ||||||||
| Yes | 354 | 52.8 | 162 | 60.9 | 182 | 61.9 | 10 | 9.0 | |
| Sexual identity | <0.001 | ||||||||
| Lesbian | 355 | 52.9 | 86 | 32.3 | 228 | 77.6 | 41 | 36.9 | |
| Bisexual | 316 | 47.1 | 180 | 67.7 | 66 | 22.4 | 70 | 63.1 | |
| Medical history | |||||||||
| STI 2 treatment | 50 | 7.5 | 44 | 16.5 | 5 | 1.7 | 1 | 0.9 | <0.001 |
| Breast exam | 118 | 17.6 | 60 | 22.6 | 47 | 16.0 | 11 | 9.9 | 0.008 |
| Cervical cancer screening | <0.001 | ||||||||
| in the last 2 years | 150 | 22.4 | 102 | 38.3 | 42 | 14.3 | 6 | 5.4 | |
| HPV vaccination | 0.013 | ||||||||
| Yes | 170 | 25.3 | 83 | 31.2 | 60 | 20.4 | 27 | 24.3 | |
| Total | Outcome | Unadjusted | Adjusted 1 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||||||||||||
| N | % | OR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |||||||
| Cervical cancer screening in 2 years | ||||||||||||||||
| Total | 671 | 150 | 22.4 | |||||||||||||
| Partner 2 | Male only/both | 266 | 102 | 38.3 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Female-only | 294 | 42 | 14.3 | 0.27 | 0.18 | 0.40 | 0.24 | 0.16 | 0.37 | 0.24 | 0.15 | 0.37 | 0.32 | 0.19 | 0.52 | |
| No partner | 111 | 6 | 5.4 | 0.09 | 0.04 | 0.22 | 0.14 | 0.06 | 0.35 | 0.14 | 0.06 | 0.34 | 0.23 | 0.09 | 0.59 | |
| Total | Outcome | Unadjusted | Adjusted 1 | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | ||||||||||||||
| N | % | OR | 95% CI | AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |||||||
| HPV vaccination | ||||||||||||||||
| Total | 671 | 170 | 25.3 | |||||||||||||
| Partner 2 | Male only/both | 266 | 83 | 31.2 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Female-only | 294 | 60 | 20.4 | 0.57 | 0.39 | 0.83 | 0.57 | 0.39 | 0.84 | 0.53 | 0.36 | 0.79 | 0.58 | 0.37 | 0.91 | |
| No partner | 111 | 27 | 24.3 | 0.71 | 0.43 | 1.18 | 0.71 | 0.42 | 1.21 | 0.67 | 0.39 | 1.15 | 0.72 | 0.40 | 1.29 | |
| Socioeconomic status | ||||||||||||||||
| High education level | 616 | 161 | 26.1 | 1.63 | 0.75 | 3.54 | ||||||||||
| High annual income | 195 | 67 | 34.4 | 1.98 | 1.35 | 2.90 | ||||||||||
| Employed (ref. student) | 318 | 80 | 25.2 | 1.02 | 0.62 | 1.68 | ||||||||||
| Unemployed (ref. student) | 60 | 15 | 25.0 | 0.99 | 0.47 | 2.05 | ||||||||||
| Total | Sex of Sexual Partner 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Male Only/Both | Female Only | No Partner | ||||||
| N | % | N | % | N | % | N | % | |
| Reasons for non-screening of cervical cancer in a lifetime | ||||||||
| Total | 451 | 100.0 | 127 | 100 | 224 | 100.0 | 100 | 100.0 |
| I do not think I am the subject of the screening | 73 | 16.2 | 16 | 12.6 | 32 | 14.3 | 25 | 25.0 |
| There was no time for the screening | 141 | 31.3 | 54 | 42.5 | 58 | 25.9 | 29 | 29.0 |
| There was no interest for the screening | 167 | 37.1 | 50 | 39.4 | 86 | 38.4 | 31 | 31.0 |
| It was because of the cost | 118 | 26.2 | 56 | 44.1 | 42 | 18.8 | 20 | 20.0 |
| I am not having sex | 87 | 19.3 | 5 | 3.9 | 24 | 10.8 | 58 | 58.0 |
| I did not know about the screening | 39 | 8.7 | 9 | 7.1 | 18 | 8.1 | 12 | 12.0 |
| I think I am healthy | 97 | 21.6 | 34 | 26.8 | 47 | 21 | 16 | 16.0 |
| I have sex only with women | 132 | 29.3 | 17 | 13.4 | 111 | 49.6 | 4 | 4.0 |
| I’m afraid that the medical staff will know I’m a sexual minority | 38 | 8.5 | 4 | 3.1 | 34 | 15.2 | 0 | 0.0 |
| I think the screening will be painful | 39 | 8.7 | 15 | 11.8 | 18 | 8.1 | 6 | 6.0 |
| Screening would be embarrassing | 52 | 11.6 | 17 | 13.4 | 23 | 10.3 | 12 | 12.0 |
| I have a fear of the negative result | 23 | 5.1 | 15 | 11.8 | 7 | 3.2 | 1 | 1.0 |
| Reasons for non-vaccination against HPV | ||||||||
| Total | 493 | 100.0 | 176 | 100 | 233 | 100.0 | 84 | 100.0 |
| I don’t think I’m the subject of the vaccination | 46 | 9.4 | 13 | 7.4 | 21 | 9.1 | 12 | 14.3 |
| There was no time for the vaccination | 119 | 24.2 | 46 | 26.1 | 50 | 21.5 | 23 | 27.4 |
| There was no interest in the vaccination | 162 | 32.9 | 55 | 31.3 | 79 | 34 | 28 | 33.4 |
| It was because of the cost | 172 | 34.9 | 86 | 48.9 | 62 | 26.7 | 24 | 28.6 |
| I am not having sex | 65 | 13.2 | 3 | 1.7 | 21 | 9.1 | 41 | 48.9 |
| I did not know about vaccination | 62 | 12.6 | 24 | 13.6 | 21 | 9.1 | 17 | 20.3 |
| I think I am healthy | 88 | 17.9 | 32 | 18.2 | 43 | 18.5 | 13 | 15.5 |
| I have sex only with women | 142 | 28.9 | 29 | 16.5 | 110 | 47.3 | 3 | 3.6 |
| I’m afraid that the medical staff will know I’m a sexual minority | 16 | 3.3 | 4 | 2.3 | 12 | 5.2 | 0 | 0 |
| I think the injection will be painful | 32 | 6.5 | 14 | 8 | 13 | 5.6 | 5 | 6 |
| The effect of the vaccination is doubtful | 75 | 15.3 | 37 | 21 | 29 | 12.5 | 9 | 10.8 |
| I am worried about side effects | 110 | 22.4 | 52 | 29.5 | 45 | 19.4 | 13 | 15.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.; Lee, S.-Y.; Choi-Kwon, S. Cervical Cancer Screening and Human Papillomavirus Vaccination among Korean Sexual Minority Women by Sex of Their Sexual Partners. Int. J. Environ. Res. Public Health 2020, 17, 8924. https://doi.org/10.3390/ijerph17238924
Kim S, Lee S-Y, Choi-Kwon S. Cervical Cancer Screening and Human Papillomavirus Vaccination among Korean Sexual Minority Women by Sex of Their Sexual Partners. International Journal of Environmental Research and Public Health. 2020; 17(23):8924. https://doi.org/10.3390/ijerph17238924
Chicago/Turabian StyleKim, Ssirai, Sun-Young Lee, and Smi Choi-Kwon. 2020. "Cervical Cancer Screening and Human Papillomavirus Vaccination among Korean Sexual Minority Women by Sex of Their Sexual Partners" International Journal of Environmental Research and Public Health 17, no. 23: 8924. https://doi.org/10.3390/ijerph17238924
APA StyleKim, S., Lee, S.-Y., & Choi-Kwon, S. (2020). Cervical Cancer Screening and Human Papillomavirus Vaccination among Korean Sexual Minority Women by Sex of Their Sexual Partners. International Journal of Environmental Research and Public Health, 17(23), 8924. https://doi.org/10.3390/ijerph17238924






