Coronavirus Lockdown as a Major Life Stressor: Does It Affect TMD Symptoms?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sociodemographic Items
2.2. Axis II of the RDC/TMD
2.3. PSS (Perceived Stress Scale)
2.4. Additional Items
2.5. Statistical Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rugh, J.; Woods, B.; Dahlström, L. Temporomandibular Disorders: Assessment of Psychological Factors. Adv. Dent. Res. 1993, 7, 127–136. [Google Scholar] [CrossRef] [PubMed]
- Rollman, G.B.; Gillespie, J.M. The role of psychosocial factors in temporomandibular disorders. Curr. Rev. Pain 2000, 4, 71–81. [Google Scholar] [CrossRef] [PubMed]
- Auerbach, S.M.; Laskin, D.M.; Frantsve, L.M.E.; Orr, T. Depression, pain, exposure to stressful life events, and long-term outcomes in temporomandibular disorder patients. J. Oral Maxillofac. Surg. 2001, 59, 628–633. [Google Scholar] [CrossRef] [PubMed]
- Callahan, C.D. Stress, coping, and personality hardiness in patients with temporomandibular disorders. Rehabil. Psychol. 2000, 45, 38–48. [Google Scholar] [CrossRef]
- De Leeuw, R.; Bertoli, E.; Schmidt, J.E.; Carlson, C.R. Prevalence of traumatic stressors in patients with temporomandibular disorders. J. Oral Maxillofac. Surg. 2005, 63, 42–50. [Google Scholar] [CrossRef]
- Gameiro, G.H.; Andrade, A.D.S.; Nouer, D.F.; Veiga, M.C.F.D.A. How may stressful experiences contribute to the development of temporomandibular disorders? Clin. Oral Investig. 2006, 10, 261–268. [Google Scholar] [CrossRef]
- Chisnoiu, A.M.; Picos, A.M.; Popa, S.; Chisnoiu, P.D.; Lascu, L.; Picos, A.; Chisnoiu, R. Factors involved in the etiology of temporomandibular disorders—A literature review. Med. Pharm. Rep. 2015, 88, 473–478. [Google Scholar] [CrossRef]
- Monteiro, D.R.; Zuim, P.R.J.; Pesqueira, A.A.; Ribeiro, P.D.P.; Garcia, A.R. Relationship between anxiety and chronic orofacial pain of temporomandibular disorder in a group of university students. J. Prosthodont. Res. 2011, 55, 154–158. [Google Scholar] [CrossRef]
- Lajnert, V.; Francisković, T.; Grzic, R.; Pavicic, D.K.; Bakarbić, D.; Buković, D.; Celebić, A.; Braut, V.; Fugosić, V. Depression, somatization and anxiety in female patients with temporomandibular disorders (TMD). Coll. Antropol. 2010, 34, 1415–1419. [Google Scholar]
- Tosato, J.D.P.; Caria, P.H.F.; Gomes, C.A.F.D.P.; Berzin, F.; Politti, F.; Gonzalez, T.D.O.; Biasotto-Gonzalez, D.A. Correlation of stress and muscle activity of patients with different degrees of temporomandibular disorder. J. Phys. Ther. Sci. 2015, 27, 1227–1231. [Google Scholar] [CrossRef]
- Brown, F.F.; Robinson, M.E.; Riley, J.L.; Gremillion, H.A. Pain Severity, Negative Affect, and Microstressers as Predictors of Life Interference in TMD Patients. CRANIO® 1996, 14, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Wade, J.B.; Dougherty, L.M.; Hart, R.P.; Rafii, A.; Price, D.D. A canonical correlation analysis of the influence of neuroticism and extraversion on chronic pain, suffering, and pain behavior. Pain 1992, 51, 67–73. [Google Scholar] [CrossRef]
- Guarda-Nardini, L.; Pavan, C.; Arveda, N.; Ferronato, G.; Manfredini, D. Psychometric features of temporomandibular disorders patients in relation to pain diffusion, location, intensity and duration. J. Oral Rehabil. 2012, 39, 737–743. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.; Oleszek-Listopad, J.; Marczak, M.; Szymanska, J. Psychological aspects of temporomandibular disorders—Literature review. Curr. Issues Pharm. Med. Sci. 2015, 28, 55–59. [Google Scholar] [CrossRef] [Green Version]
- Moody, P.M.; Kemper, J.T.; Okeson, J.P.; Calhoun, T.C.; Packer, M.W. Recent life changes and myofascial pain syndrome. J. Prosthet. Dent. 1982, 48, 328–330. [Google Scholar] [CrossRef]
- Lundeen, T.F.; Sturdevant, J.R.; George, J.M. Stress as a factor in muscle and temporomandibular joint pain. J. Oral Rehabil. 1987, 14, 447–456. [Google Scholar] [CrossRef] [PubMed]
- Rugh, J.D.; Solberg, W.K. Psychological implications in temporomandibular pain and dysfunction. Oral Sci. Rev. 1976, 7, 3–30. [Google Scholar]
- Speculand, B.; Hughes, A.O.; Goss, A.N. Role of recent stressful life events experience in the onset of TMJ dysfunction pain. Community Dent. Oral Epidemiol. 1984, 12, 197–202. [Google Scholar] [CrossRef]
- Dahlström, L. Psychometrics in Temporomandibular Disorders: An overview. Acta Odontol. Scand. 1993, 51, 339–352. [Google Scholar] [CrossRef]
- Uhač, I.; Kovač, Z.; Valentić-Peruzović, M.; Juretić, M.; Moro, L.J.; Gržić, R. The influence of war stress on the prevalence of signs and symptoms of temporomandibular disorders. J. Oral Rehabil. 2003, 30, 211–217. [Google Scholar] [CrossRef]
- Suvinen, T.I.; Hanes, K.R.; Gerschman, J.A.; Reade, P.C. Psychophysical subtypes of temporomandibular disorders. J. Orofac. Pain 1997, 11, 3. [Google Scholar]
- Ferreira, D.M.A.O.; Vaz, C.C.D.O.; Stuginski-Barbosa, J.; Conti, P.C.R. Post-traumatic stress disorder and temporomandibular dysfunction: A review and clinical implications. Braz. J. Pain 2018, 1, 55–59. [Google Scholar] [CrossRef]
- Tanti, I.; Himawan, L.S.; Kusdhany, L.; Bachtiar, A.; Ismail, R.I. Validation of stress screening questionnaire in temporomandibular disorders patient. J. Int. Dent. Med. Res. 2016, 9, 272. [Google Scholar]
- Sherman, J.J.; Carlson, C.R.; Wilson, J.F.; Okeson, J.P.; McCubbin, J.A. Post-traumatic stress disorder among patients with orofacial pain. J. Orofac. Pain 2005, 19, 309–317. [Google Scholar] [CrossRef] [PubMed]
- Afari, N.; Wen, Y.; Buchwald, D.; Goldberg, J.; Plesh, O. Are post-traumatic stress disorder symptoms and temporomandibular pain associated? A twin study. J. Orofac. Pain 2008, 22, 41. [Google Scholar]
- Schiffman, E.L.; Fricton, J.R.; Haley, D. The relationship of occlusion, parafunctional habits and recent life events to mandibular dysfunction in a non-patient population. J. Oral Rehabil. 1992, 19, 201–223. [Google Scholar] [CrossRef]
- Abu-Raisi, S.S.; Ibrahim, S.A.; Ajina, M.A.; Ibrahim, E.A.; Almulhim, A.Y.; Aljalal, M.A.; Almajed, Z.S. Temporomandibular Disorder among Women Who Experienced Posttraumatic Stress Disorder after a Miscarriage. J. Int. Soc. Prev. Community Dent. 2019, 9, 445–452. [Google Scholar]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.H.; Ho, R.C.M. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- Dworkin, S.F.; LeResche, L. Research diagnostic criteria for temporomandibular disorders: Review, criteria, examinations and specifications, critique. J. Craniomandib. Disord. 1992, 6, 301–355. [Google Scholar]
- Manfredini, D.; Winocur, E.; Ahlberg, J.; Guarda-Nardini, L.; Lobbezoo, F. Psychosocial impairment in temporomandibular disorders patients. RDC/TMD axis II findings from a multicentre study. J. Dent. 2010, 38, 765–772. [Google Scholar] [CrossRef]
- Ohrbach, R.; Turner, J.A.; Sherman, J.J.; Mancl, L.A.; Truelove, E.L.; Schiffman, E.L.; Dworkin, S.F. The Research Diagnostic Criteria for Temporomandibular Disorders. IV: Evaluation of psychometric properties of the Axis II measures. J. Orofac. Pain 2010, 24, 48–62. [Google Scholar]
- Von Korff, M.; Dworkin, S.F.; Le Resche, L. Graded chronic pain status: An epidemiologic evaluation. Pain 1990, 40, 279–291. [Google Scholar] [CrossRef]
- Von Korff, M.; Ormel, J.; Keefe, F.J.; Dworkin, S.F. Grading the severity of chronic pain. Pain 1992, 50, 133–149. [Google Scholar] [CrossRef]
- Derogatis, L.R. Symptom Checklist-90-R (SCL-90-R); Computer Systems: Minneapolis, MN, USA, 1993. [Google Scholar]
- Pallegama, R.; Ranasinghe, A.W.; Weerasinghe, V.S.; Sitheeque, M.A.M. Anxiety and personality traits in patients with muscle related temporomandibular disorders. J. Oral Rehabil. 2005, 32, 701–707. [Google Scholar] [CrossRef] [PubMed]
- Akhter, R.; Hassan, N.M.; Aida, J.; Kanehira, T.; Zaman, K.U.; Morita, M. Association between experience of stressful life events and muscle-related temporomandibular disorders in patients seeking free treatment in a dental hospital. Eur. J. Med. Res. 2007, 12, 535. [Google Scholar] [PubMed]
- Yap, A.U.J.; Tan, K.B.; Prosthodont, C.; Chua, E.K.; Tan, H.H. Depression and somatization in patients with temporomandibular disorders. J. Prosthet. Dent. 2002, 88, 479–484. [Google Scholar] [CrossRef]
- Michelotti, A.; Martina, R.; Russo, M.; Romeo, R. Personality characteristics of temporomandibular disorder patients using M.M.P.I. CRANIO® 1998, 16, 119–125. [Google Scholar] [CrossRef]
- Saccomanno, S.; Quinzi, V.; Sarhan, S.; Laganà, D.; Marzo, G. Perspectives of tele-orthodontics in the COVID-19 emergency and as a future tool in daily practice. Eur. J. Paediatr. Dent. 2020, 21, 157–162. [Google Scholar]
- Rossi, R.; Socci, V.; Talevi, D.; Mensi, S.; Niolu, C.; Pacitti, F.; Di Marco, A.; Rossi, A.; Siracusano, A.; Di Lorenzo, G. COVID-19 Pandemic and Lockdown Measures Impact on Mental Health Among the General Population in Italy. Front. Psychiatry 2020, 11, 790. [Google Scholar] [CrossRef]
- De Resende, C.M.B.M.; Rocha, L.G.D.D.S.; De Paiva, R.P.; Cavalcanti, C.D.S.; De Almeida, E.O.; Roncalli, A.G.; Barbosa, G.A.S. Relationship between anxiety, quality of life, and sociodemographic characteristics and temporomandibular disorder. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2020, 129, 125–132. [Google Scholar] [CrossRef]
- De Lucena, I.M.; Rodrigues, L.L.F.R.; Teixeira, M.L.; Pozza, D.H.; Guimaraes, A.S. Prospective study of a group of pre-university students evaluating anxiety and depression relationships with temporomandibular disorders. J. Clin. Exp. Dent. 2012, 4, e102–e106. [Google Scholar] [CrossRef] [PubMed]
- Gatchel, R.J.; Garofalo, J.P.; Ellis, E.; Holt, C. Major Psychological Disorders in Acute and Chronic TMD: An Initial Examination. J. Am. Dent. Assoc. 1996, 127, 1365–1374. [Google Scholar] [CrossRef] [PubMed]
- John, M.T.; Miglioretti, D.L.; LeResche, L.; Von Korff, M.; Critchlow, C.W. Widespread pain as a risk factor for dysfunctional temporomandibular disorder pain. Pain 2003, 102, 257–263. [Google Scholar] [CrossRef]
- Dworkin, S.F.; Sherman, J.; Mancl, L.; Ohrbach, R.; LeResche, L.; Truelove, E.L. Reliability, validity, and clinical utility of the research diagnostic criteria for Temporomandibular Disorders Axis II Scales: Depression, non-specific physical symptoms, and graded chronic pain. J. Orofac. Pain 2002, 16, 207–220. [Google Scholar] [PubMed]
- Yadav, S.; Yang, Y.; Dutra, E.H.; Robinson, J.L.; Wadhwa, S. Temporomandibular Joint Disorders in Older Adults. J. Am. Geriatr. Soc. 2018, 66, 1213–1217. [Google Scholar] [CrossRef] [PubMed]
- Ciancaglini, R.; Gherlone, E.F.; Redaelli, S.; Radaelli, G. The distribution of occlusal contacts in the intercuspal position and temporomandibular disorder. J. Oral Rehabil. 2002, 29, 1082–1090. [Google Scholar] [CrossRef] [PubMed]
- Pedroni, C.R.; De Oliveira, A.S.; Guaratini, M.I. Prevalence study of signs and symptoms of temporomandibular disorders in university students. J. Oral Rehabil. 2003, 30, 283–289. [Google Scholar] [CrossRef]
- Quinzi, V.; Scibetta, E.T.; Marchetti, E.; Mummolo, S.; Gianni, A.B.; Romano, M.; Beltramini, G.; Marzo, G. Analyze my face. J. Biol. Regul. Homeost. Agents 2018, 32, 149–158. [Google Scholar]
- Scoppa, F.; Saccomanno, S.; Bianco, G.; Pirino, A. Tongue Posture, Tongue Movements, Swallowing, and Cerebral Areas Activation: A Functional Magnetic Resonance Imaging Study. Appl. Sci. 2020, 10, 6027. [Google Scholar] [CrossRef]
- Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatry 2020, 51, 102076. [Google Scholar] [CrossRef]
- Zhou, S.-J.; Zhang, L.-G.; Wang, L.-L.; Guo, Z.-C.; Wang, J.-Q.; Chen, J.-C.; Liu, M.; Chen, X.; Chen, J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Ren, Y.; Yan, F.; Li, Y.; Xu, X.; Yu, X.; Qu, W.; Wang, Z.; Tian, B.; Yang, F.; et al. Psychological Impact and Predisposing Factors of the Coronavirus Disease 2019 (COVID-19) Pandemic on General Public in China. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- Wang, Y.; Di, Y.; Ye, J.; Wei, W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 2020, 30, 1–10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alpaslan, C.; Yaman, D. Clinical evaluation and classification of patients with temporomandibular disorders using ‘Diagnostic Criteria for Temporomandibular Disorders’. Acta Odontol. Turc. 2020, 37, 1–6. [Google Scholar] [CrossRef]
- Jacobson, A. A randomized clinical trial of a tailored comprehensive care treatment program for temporomandibular disorder. Am. J. Orthod. Dentofac. Orthop. 2003, 123, 481. [Google Scholar] [CrossRef]
- Türp, J.; Jokstad, A.; Motschall, E.; Schindler, H.J.; Windecker-Gétaz, I.; Ettlin, D.A. Is there a superiority of multimodal as opposed to simple therapy in patients with temporomandibular disorders? A qualitative systematic review of the literature. Clin. Oral Implant. Res. 2007, 18, 138–150. [Google Scholar] [CrossRef]
| Age Group | Frequency |
|---|---|
| <20 | 1 (0.5%) |
| 20–30 | 28 (15.4%) |
| 30–40 | 46 (25.3%) |
| 40–50 | 44 (24.2%) |
| 50–60 | 46 (25.3%) |
| 60–70 | 17 (9.3%) |
| Sex M/F | 52/130 |
| Education | |
| Middle High | 8 (4.4%) |
| High School | 70 (38.5%) |
| College | 95 (52.2%) |
| PhD | 8 (4.4%) |
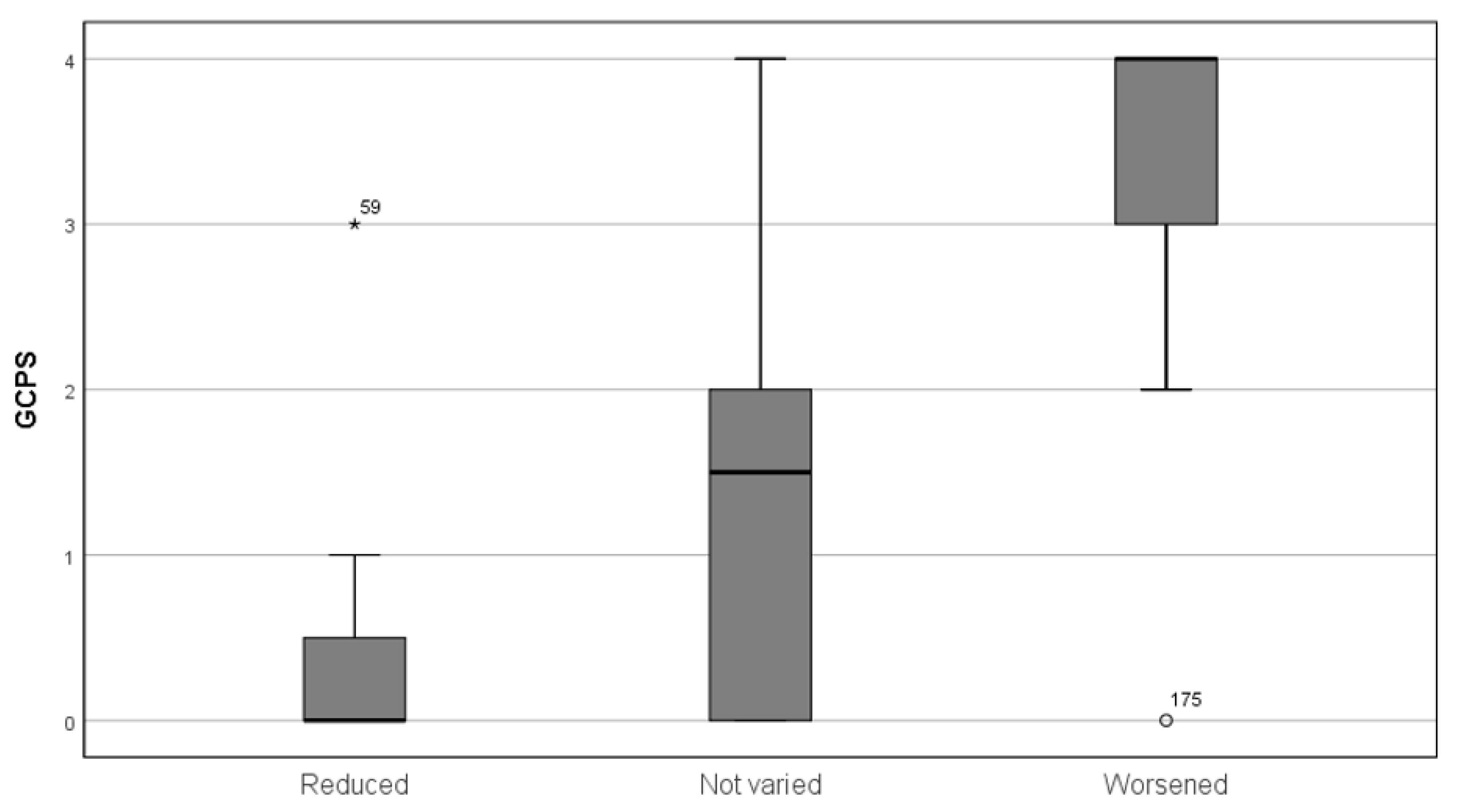
| GPCS Class | Median Perceived Stress Score (PSS) | Median Depression Score (DEP) | Median Somatization Score (SOM) |
|---|---|---|---|
| 0 | 21.0 | 1.4 | 1.5 |
| 1 | 25.0 | 1.4 | 2.0 |
| 2 | 19.5 | 0.8 | 1.2 |
| 3 | 30.0 | 2.5 | 2.3 |
| 4 | 33.0 | 2.8 | 2.33 |
| Significance | p < 0.05 | p < 0.05 | p < 0.05 |
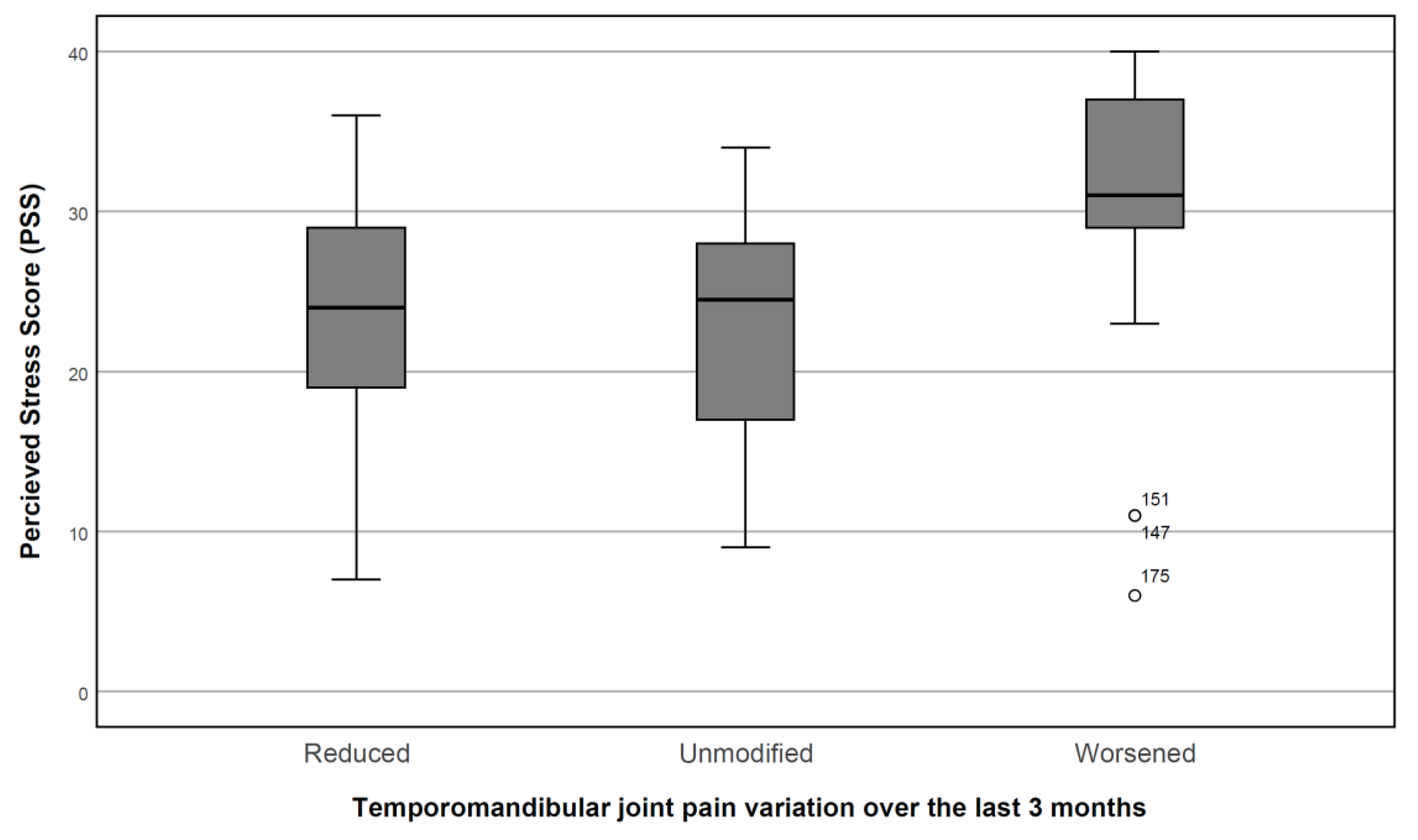
| TMJ Pain in the Last Six Months | Median Perceived Stress Score (PSS) | Median Depression Score (DEP) | Median Somatization Score (SOM) |
|---|---|---|---|
| No | 23.0 ± 9.1 | 1.3 ± 1.2 | 1.2 ± 1.4 |
| Yes | 18.0 ± 9.6 | 1.1 ± 1.4 | 0.9 ± 1.0 |
| Significance | p < 0.05 | p < 0.05 | p < 0.05 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saccomanno, S.; Bernabei, M.; Scoppa, F.; Pirino, A.; Mastrapasqua, R.; Visco, M.A. Coronavirus Lockdown as a Major Life Stressor: Does It Affect TMD Symptoms? Int. J. Environ. Res. Public Health 2020, 17, 8907. https://doi.org/10.3390/ijerph17238907
Saccomanno S, Bernabei M, Scoppa F, Pirino A, Mastrapasqua R, Visco MA. Coronavirus Lockdown as a Major Life Stressor: Does It Affect TMD Symptoms? International Journal of Environmental Research and Public Health. 2020; 17(23):8907. https://doi.org/10.3390/ijerph17238907
Chicago/Turabian StyleSaccomanno, Sabina, Mauro Bernabei, Fabio Scoppa, Alessio Pirino, Rodolfo Mastrapasqua, and Marina Angela Visco. 2020. "Coronavirus Lockdown as a Major Life Stressor: Does It Affect TMD Symptoms?" International Journal of Environmental Research and Public Health 17, no. 23: 8907. https://doi.org/10.3390/ijerph17238907
APA StyleSaccomanno, S., Bernabei, M., Scoppa, F., Pirino, A., Mastrapasqua, R., & Visco, M. A. (2020). Coronavirus Lockdown as a Major Life Stressor: Does It Affect TMD Symptoms? International Journal of Environmental Research and Public Health, 17(23), 8907. https://doi.org/10.3390/ijerph17238907







