Social Capital, Income Loss, and Psychobehavioral Responses amid COVID-19: A Population-Based Analysis
Abstract
1. Introduction
1.1. Social Capital, Mental Health, and Preventive Behaviors
1.2. Resource Loss as the Moderator
1.3. The Present Study
2. Materials and Methods
2.1. Respondents and Procedure
2.2. Measures
2.2.1. Demographics
2.2.2. Social Capital
2.2.3. Probable Depression
2.2.4. Preventive Behaviors
2.3. Statistical Analysis
3. Results
3.1. Sample and Prevalence
3.2. Multivariable Logistic Regressions
3.2.1. Social Capital and Probable Depression
3.2.2. Social Capital and Preventive Behaviors
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Outcomes | Interaction Terms | p-Value |
|---|---|---|
| Probable depression | ||
| Interpersonal trust × Income change | 0.856 | |
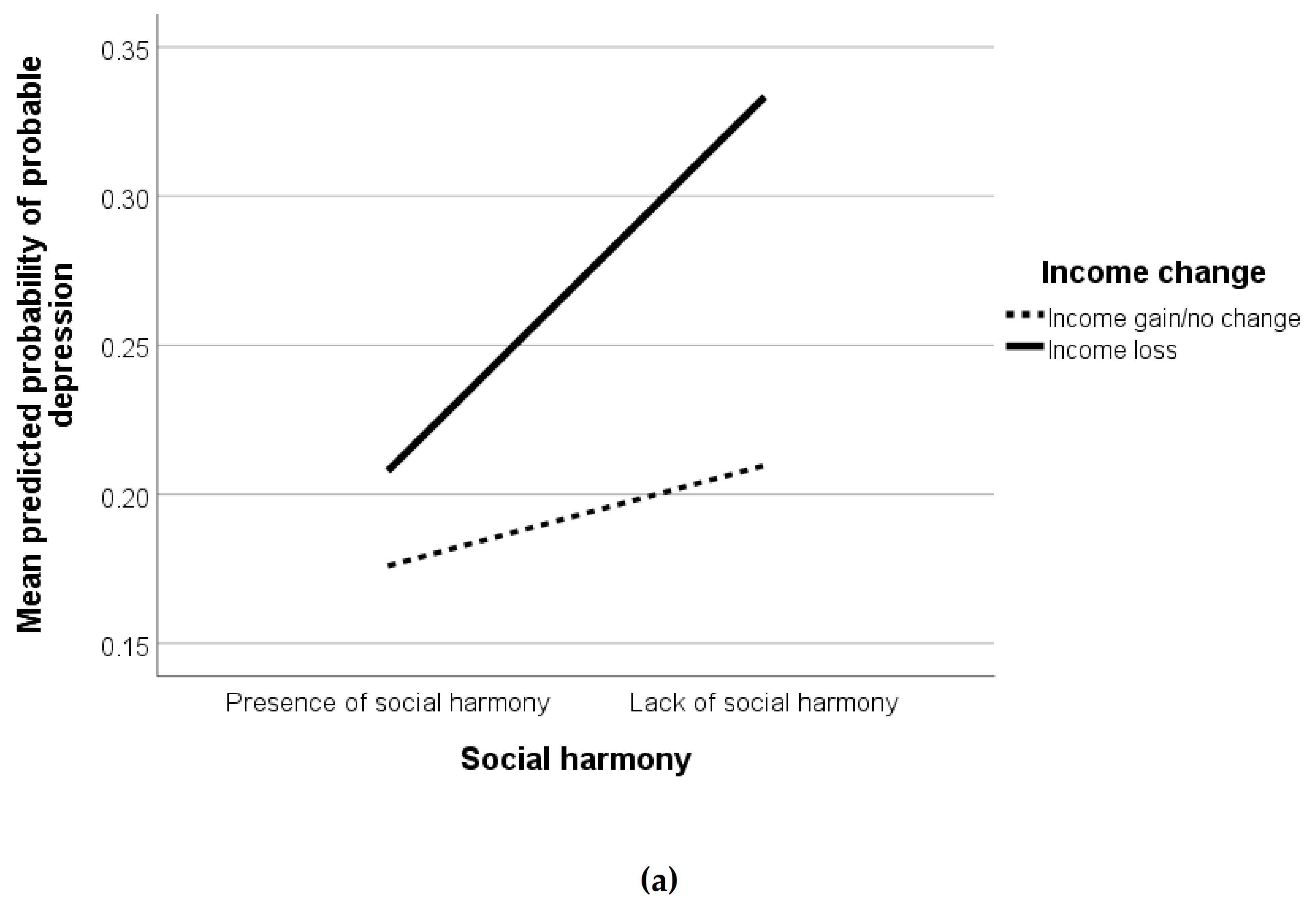
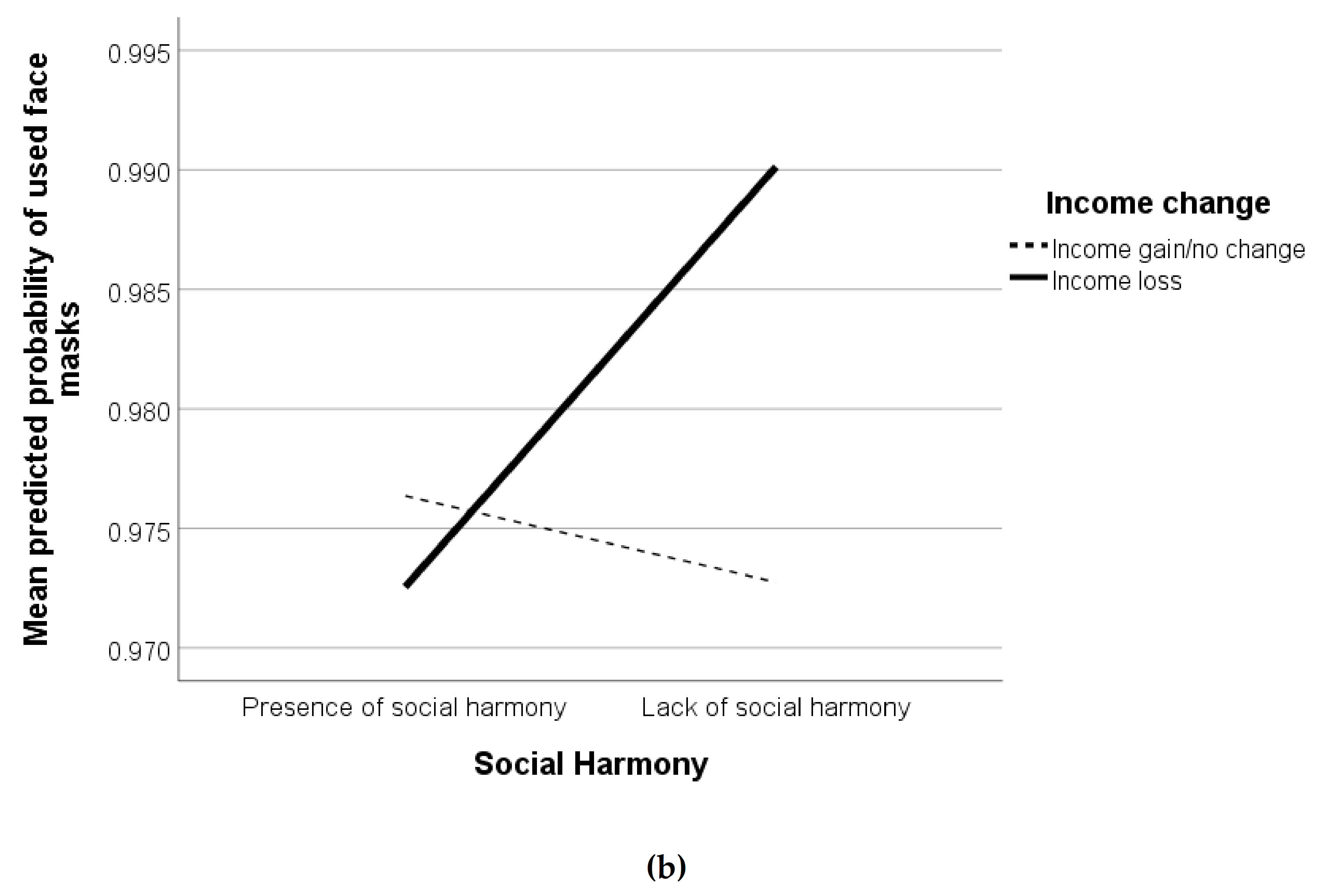
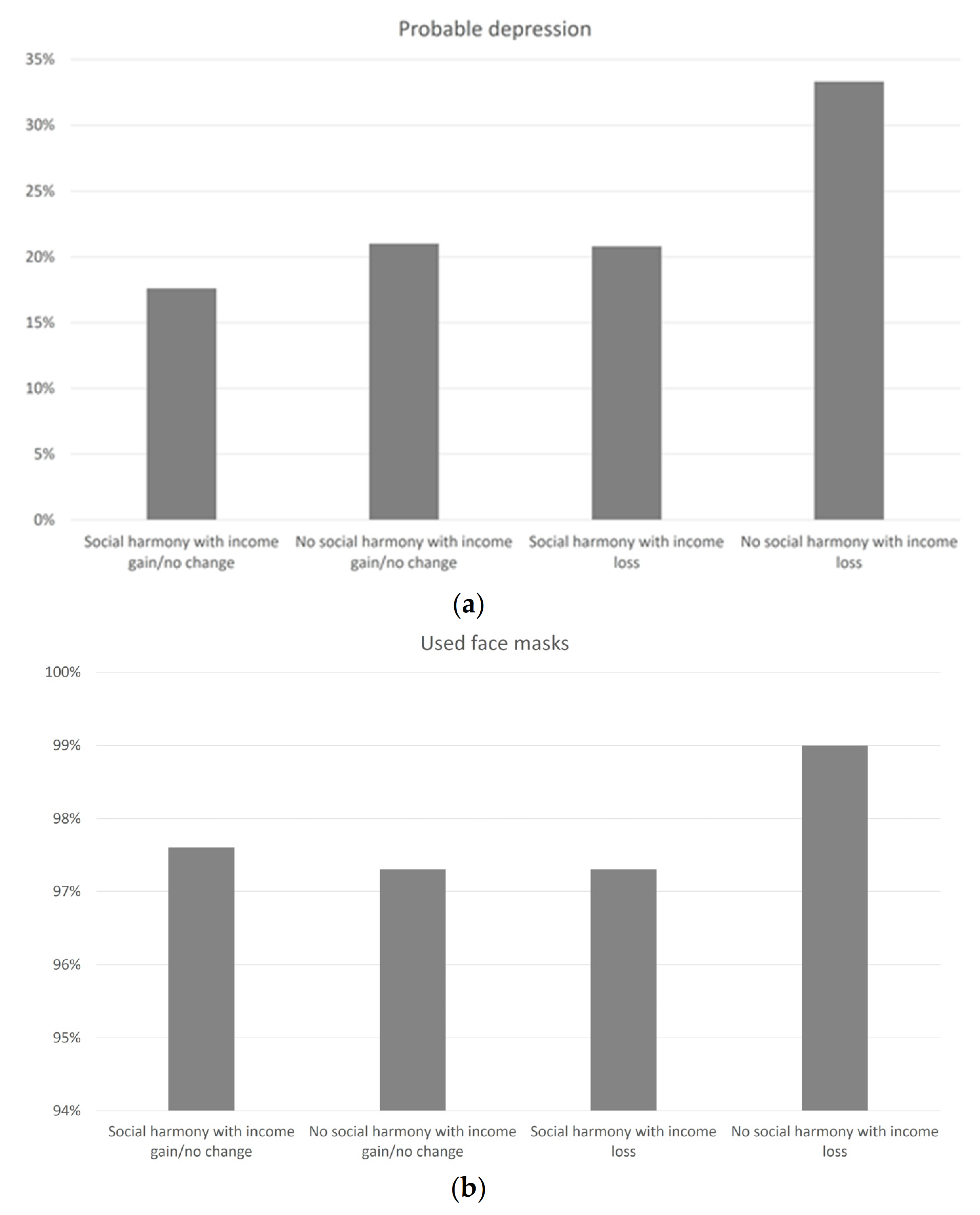
| Social harmony × Income change | 0.026 | |
| Sense of belonging × Income change | 0.300 | |
| Used face masks | ||
| Interpersonal trust × Income change | 0.336 | |
| Social harmony × Income change | 0.043 | |
| Sense of belonging × Income change | 0.335 | |
| Washed hands more often | ||
| Interpersonal trust × Income change | 0.086 | |
| Social harmony × Income change | 0.363 | |
| Sense of belonging × Income change | 0.311 | |
| Avoided contact with people with respiratory symptoms | ||
| Interpersonal trust × Income change | 0.088 | |
| Social harmony × Income change | 0.903 | |
| Sense of belonging × Income change | 0.647 | |
| Avoided going to crowded places | ||
| Interpersonal trust × Income change | 0.880 | |
| Social harmony × Income change | 0.368 | |
| Sense of belonging × Income change | 0.603 |
References
- Spinelli, A.; Pellino, G. COVID-19 pandemic: Perspectives on an unfolding crisis. Br. J. Surg. 2020, 107, 785–787. [Google Scholar] [CrossRef] [PubMed]
- Pfefferbaum, B.; North, C.S. Mental Health and the Covid-19 Pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef] [PubMed]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatr. 2020, 33, e100213. [Google Scholar] [CrossRef] [PubMed]
- González-Sanguino, C.; Ausín, B.; Castellanos, M.Á.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Hou, W.K.; Lee, T.M.C.; Liang, L.; Li, T.W.; Liu, H.; Tong, H.; Ben-Ezra, M.; Goodwin, R. Psychiatric symptoms and behavioral adjustment during the COVID-19 pandemic: Evidence from two population-representative cohorts. Transl. Psychiatry. in press.
- Dong, L.; Bouey, J. Public mental health crisis during COVID-19 pandemic, China. Emerg. Infect. Dis. 2020, 26, 1616–1618. [Google Scholar] [CrossRef]
- Variation in Government Responses to COVID-19. Available online: https://www.bsg.ox.ac.uk/sites/default/files/2020-05/BSG-WP-2020-032-v6.0.pdf (accessed on 1 August 2020).
- Hou, W.K.; Lai, F.T.T.; Ben-Ezra, M.; Goodwin, R. Regularizing daily routines for mental health during and after the COVID-19 pandemic. J. Glob. Health 2020, 10, 020315. [Google Scholar] [CrossRef]
- Putnam, R.D. Bowling alone: America’s declining social capital. J. Democr. 1995, 6, 65–78. [Google Scholar] [CrossRef]
- Aida, J.; Kawachi, I.; Subramanian, S.V.; Kondo, K. Disaster, social capital, and health. In Global Perspectives on Social Capital and Health, 1st ed.; Kawachi, I., Takao, S., Subramanian, S.V., Eds.; Springer: New York, NY, USA, 2013; pp. 167–187. [Google Scholar]
- Cowling, B.J.; Ali, S.T.; Ng, T.W.Y.; Tsang, T.K.; Li, J.C.M.; Fong, M.W.; Liao, Q.; Kwan, M.Y.W.; Lee, S.L.; Chiu, S.S.; et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study. Lancet Public Health 2020, 5, e279–e288. [Google Scholar] [CrossRef]
- Ng, S.H.; Cheung, S.Y.L.; Prakash, B. Social Capital in Hong Kong: Connectivities and Social Enterprise; City University of Hong Kong Press: Hong Kong, 2010. [Google Scholar]
- Lau, P.Y.F. Fighting COVID-19: Social capital and community mobilisation in Hong Kong. Int. J. Sociol. Soc. Policy 2020. [Google Scholar] [CrossRef]
- Lai, F.T.T.; Hall, B.J.; Liang, L.; Galea, S.; Hou, W.K. Socioeconomic gradient of mental health amid the anti-extradition bill protests in Hong Kong: The mediating role of daily routine disruptions. J. Epidemiol. Community Health 2020, 74, 988–994. [Google Scholar] [CrossRef] [PubMed]
- Ehsan, A.M.; De Silva, M.J. Social capital and common mental disorder: A systematic review. J. Epidemiol. Community Health 2015, 69, 1021–1028. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Cline, H.; Beresford, S.A.A.; Barrington, W.; Matsueda, R.; Wakefield, J.; Duncan, G.E. Associations between social capital and depression: A study of adult twins. Health Place 2018, 50, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Saeri, A.K.; Cruwys, T.; Barlow, F.K.; Stronge, S.; Sibley, C.G. Social connectedness improves public mental health: Investigating bidirectional relationships in the New Zealand attitudes and values survey. Aust. N. Z. J. Psychiatry 2018, 52, 365–374. [Google Scholar] [CrossRef]
- Szreter, S.; Woolcock, M. Health by association? Social capital, social theory, and the political economy of public health. Int. J. Epidemiol. 2004, 33, 650–667. [Google Scholar] [CrossRef]
- Iwasaki, K.; Sawada, Y.; Aldrich, D.P. Social capital as a shield against anxiety among displaced residents from Fukushima. Nat. Hazards 2017, 89, 405–421. [Google Scholar] [CrossRef]
- Rung, A.L.; Gaston, S.; Robinson, W.T.; Trapido, E.J.; Peters, E.S. Untangling the disaster-depression knot: The role of social ties after deepwater horizon. Soc. Sci. Med. 2017, 177, 19–26. [Google Scholar] [CrossRef]
- Kim, E.S.; Kawachi, I. Perceived Neighborhood Social Cohesion and Preventive Healthcare Use. Am. J. Prev. Med. 2017, 53, e35–e40. [Google Scholar] [CrossRef]
- Asma, P.; Javad, A.B.M.; Behzad, M.; Reza, R.M. The role of social capital on the health promotion behaviors in women teachers at bam girls’ schools. J. Med. Life 2019, 12, 442–448. [Google Scholar] [CrossRef]
- Chuang, Y.C.; Huang, Y.L.; Tseng, K.C.; Yen, C.H.; Yang, L.H. Social capital and health-protective behavior intentions in an influenza pandemic. PLoS ONE 2015, 10, e0122970. [Google Scholar] [CrossRef]
- Jung, M.; Lin, L.; Viswanath, K. Associations between health communication behaviors, neighborhood social capital, vaccine knowledge, and parents’ H1N1 vaccination of their children. Vaccine 2013, 31, 4860–4866. [Google Scholar] [CrossRef] [PubMed]
- Rönnerstrand, B. Contextual generalized trust and immunization against the 2009 A (H1N1) pandemic in the American states: A multilevel approach. SSM Popul. Health 2016, 2, 632–639. [Google Scholar] [CrossRef] [PubMed]
- Bourdieu, P. The forms of capital. In Handbook of Theory and Research for the Sociology of Education, 1st ed.; Richardson, J.G., Ed.; Greenwood Press: New York, NY, USA, 1986; pp. 241–258. [Google Scholar]
- Wright, L.; Steptoe, A.; Fancourt, D. Are we all in this together? Longitudinal assessment of cumulative adversities by socioeconomic position in the first 3 weeks of lockdown in the UK. J. Epidemiol. Community Health 2020, 74, 683–688. [Google Scholar] [CrossRef] [PubMed]
- Global Economic Prospects. Available online: https://www.worldbank.org/en/publication/global-economic-prospects (accessed on 1 August 2020).
- Hobfoll, S.E. Stress, Culture, and Community: The Psychology and Philosophy of Stress, 1st ed.; Plenum Press: New York, NY, USA, 1998. [Google Scholar]
- Hobfoll, S.E. Conservation of resources theory: Its implication for stress, health, and resilience. In The Oxford Handbook of Stress, Health, and Coping, 1st ed.; Folkman, S., Ed.; Oxford University Press: New York, NY, USA, 2010; pp. 127–147. [Google Scholar]
- Hou, W.K.; Hall, B.J.; Canetti, D.; Lau, K.M.; Ng, S.M.; Hobfoll, S.E. Threat to democracy: Physical and mental health impact of democracy movement in Hong Kong. J. Affect. Disord. 2015, 186, 74–82. [Google Scholar] [CrossRef]
- Rhodes, J.; Chan, C.; Paxson, C.; Rousse, C.E.; Waters, M.; Fussell, E. The impact of Hurricane Katrina on the mental and physical health of low-income parents in New Orleans. Am. J. Orthopsychiatry 2010, 80, 237–247. [Google Scholar] [CrossRef]
- Nagai, M.; Ohira, T.; Zhang, W.; Nakano, H.; Maeda, M.; Yasumura, S.; Abe, M.; Fukushima Health Management Survey. Lifestyle-related factors that explain disaster-induced changes in socioeconomic status and poor subjective health: A cross-sectional study from the Fukushima health management survey. BMC Public Health 2017, 17, 340. [Google Scholar] [CrossRef]
- Local Situation Dashboard (Desktop Version). Available online: https://chp-dashboard.geodata.gov.hk/covid-19/en.html (accessed on 9 November 2020).
- Wong, S.Y.S.; Kwok, K.O.; Chan, F.K.L. What can countries learn from Hong Kong’s response to the COVID-19 pandemic? CMAJ 2020, 192, E511–E515. [Google Scholar] [CrossRef]
- Galea, S.; Tracy, M. Participation rates in epidemiologic studies. Ann. Epidemiol. 2007, 17, 643–653. [Google Scholar] [CrossRef]
- Leung, G.M.; Ho, L.M.; Chan, S.K.K.; Ho, S.Y.; Bacon-Shone, J.; Choy, R.Y.L.; Hedley, A.J.; Lam, T.H.; Fielding, R. Longitudinal assessment of community psychobehavioral responses during and after the 2003 outbreak of severe acute respiratory syndrome in Hong Kong. Clin. Infect. Dis. 2005, 40, 1713–1720. [Google Scholar] [CrossRef]
- Harpham, T.; Grant, E.; Thomas, E. Measuring social capital within health surveys: Key issues. Health Policy Plan. 2002, 17, 106–111. [Google Scholar] [CrossRef]
- De Silva, M.J.; Harpham, T.; Tuan, T.; Bartolini, R.; Penny, M.E.; Huttly, S.R. Psychometric and cognitive validation of a social capital measurement tool in Peru and Vietnam. Soc. Sci. Med. 2006, 62, 941–953. [Google Scholar] [CrossRef] [PubMed]
- Yeung, A.; Fung, F.; Yu, S.C.; Vorono, S.; Ly, M.; Wu, S.; Fava, M. Validation of the Patient Health Questionnaire-9 for depression screening among Chinese Americans. Compr. Psychiatry 2008, 49, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Nan, H.; Lee, P.H.; Ni, M.Y.; Chan, B.H.Y.; Lam, T.H. Effects of depressive symptoms and family satisfaction on health related quality of life: The Hong Kong FAMILY study. PLoS ONE 2013, 8, e58436. [Google Scholar] [CrossRef] [PubMed]
- Guidelines on Prevention of Coronavirus Disease 2019 (COVID-19) for the General Public. Available online: https://www.chp.gov.hk/files/pdf/nid_guideline_general_public_en.pdf (accessed on 1 June 2020).
- Hong Kong in Figures. Available online: https://www.statistics.gov.hk/pub/B10100062020AN20B0100.pdf (accessed on 1 June 2020).
- Kingsbury, M.; Clayborne, Z.; Colman, I.; Kirkbride, J.B. The protective effect of neighbourhood social cohesion on adolescent mental health following stressful life events. Psychol. Med. 2019, 50, 1292–1299. [Google Scholar] [CrossRef]
- Prior, T.; Eriksen, C. Wildfire preparedness, community cohesion and social–ecological systems. Glob. Environ. Chang. 2013, 23, 1575–1586. [Google Scholar] [CrossRef]
- Han, Z.; Wang, L.; Cui, K. Trust in stakeholders and social support: Risk perception and preparedness by the Wenchuan earthquake survivors. Environ. Hazards. 2020. [Google Scholar] [CrossRef]
- Yıldırım, M.; Geçer, E.; Akgül, Ö. The impacts of vulnerability, perceived risk, and fear on preventive behaviours against COVID-19. Psychol. Health Med. 2020. [Google Scholar] [CrossRef]
- Galea, S.; Abdalla, S.M. COVID-19 pandemic, unemployment, and civil unrest: Underlying deep racial and socioeconomic divides. JAMA 2020, 324, 227–228. [Google Scholar] [CrossRef]
- Patel, J.; Nielsen, F.; Badiani, A.; Assi, S.; Unadkat, V.; Patel, B.; Ravindrane, R.; Wardle, H. Poverty, inequality and COVID-19: The forgotten vulnerable. Public Health 2020, 183, 110–111. [Google Scholar] [CrossRef]
- Banks, J.; Karjalainen, H.; Propper, C. Recessions and Health: The Long-Term Health Consequences of Responses to the Coronavirus. Fisc. Stud. 2020, 41, 337–344. [Google Scholar] [CrossRef]
- Hou, W.K.; Hall, B.J.; Liang, L.; Li, T.W.; Liu, H.; Galea, S. Probable depression and suicidal ideation in Hong Kong amid massive civil unrest. Ann. Epidemiol. 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- McKee, M.; Stuckler, D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nat. Med. 2020, 26, 640–642. [Google Scholar] [CrossRef]
- Amburgey, A.; Birinci, S. Which earnings groups have been most affected by the COVID-19 Crisis? Econ. Synop. 2020, 37. [Google Scholar] [CrossRef]
- Napolitano, F.; Napolitano, P.; Angelillo, I.F. Seasonal influenza vaccination in pregnant women: Knowledge, attitudes, and behaviors in Italy. BMC Infect. Dis. 2017, 17, 48. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Schmid, M.B.; Czypionka, T.; Bassler, D.; Gruer, L. Face masks for the public during the covid-19 crisis. BMJ 2020, 369, m1435. [Google Scholar] [CrossRef]
- Pitas, N.; Ehmer, C. Social Capital in the Response to COVID-19. Am. J. Health Promot. 2020, 1–3. [Google Scholar] [CrossRef] [PubMed]
| Variable | Overall (n = 3011) | |
|---|---|---|
| n | % | |
| Gender | ||
| Male | 1359 | 45.1 |
| Female | 1652 | 54.9 |
| Age | ||
| 15–24 | 441 | 14.6 |
| 25–34 | 552 | 18.3 |
| 35–44 | 554 | 18.4 |
| 45–54 | 535 | 17.8 |
| 55–65 | 455 | 15.1 |
| 65 or above | 474 | 15.7 |
| Marital status | ||
| Married | 1653 | 54.9 |
| Unmarried/divorced/widowed | 1358 | 45.1 |
| Education level | ||
| Tertiary or above | 1485 | 49.3 |
| Secondary | 1289 | 42.8 |
| Primary or below | 237 | 7.9 |
| Employment | ||
| Employed | 1781 | 59.1 |
| Dependent | 1106 | 36.7 |
| Unemployed | 124 | 4.1 |
| Monthly household income (HK$) | ||
| $80,000 or above | 445 | 14.8 |
| $60,000–$79,999 | 263 | 8.7 |
| $40,000–$59,999 | 648 | 21.5 |
| $20,000–$39,999 | 886 | 29.4 |
| $19,999 or below | 769 | 25.5 |
| Income change | ||
| Gain/No change | 2096 | 69.6 |
| Loss | 915 | 30.4 |
| Variable | Overall (n = 3011) |
|---|---|
| Social Capital 1 | |
| Interpersonal trust | 2012 (66.8%, 65.1–68.5%) |
| Social harmony | 1652 (54.9%, 53.1–56.6%) |
| Sense of belonging | 2908 (96.6%, 95.9–97.2%) |
| Probable depression 2,3 | 642 (21.3%, 19.9–22.8%) |
| Adoption of preventive behaviors 4 | |
| Used face masks | 2940 (97.6%, 97–98%) |
| Washed hands more often | 2778 (92.3%, 91–93%) |
| Avoided contact with people with respiratory symptoms | 2171 (72.1%, 70–74%) |
| Avoided going to crowded places | 2399 (79.7%, 78–81%) |
| Variable | Probable Depression 1 | Used Face Masks | Washed Hands More Often | Avoided Contact with People with Respiratory Symptoms | Avoided Going to Crowded Places |
|---|---|---|---|---|---|
| aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | aOR (95% CI) | |
| Gender | |||||
| Male | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Female | 1.55 (1.28–1.87) *** | 1.70 (1.03–2.81) * | 2.35 (1.76–3.15) *** | 1.57 (1.32–1.87) *** | 1.76 (1.46–2.12) *** |
| Age | |||||
| 15–24 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 25–34 | 1.20 (0.85–1.70) | 0.13 (0.03–0.61) * | 1.00 (0.56–1.77) | 0.91 (0.64–1.31) | 1.30 (0.91–1.85) |
| 35–44 | 1.15 (0.79–1.67) | 0.30 (0.05–1.69) | 1.10 (0.60–2.01) | 0.66 (0.45–0.95) * | 1.63 (1.11–2.41) * |
| 45–54 | 0.91 (0.62–1.33) | 0.14 (0.03–0.70) * | 1.19 (0.65–2.19) | 0.49 (0.34–0.71) *** | 1.39 (0.95–2.04) |
| 55–64 | 0.87 (0.60–1.27) | 0.10 (0.02–0.46) ** | 0.74 (0.43–1.28) | 0.42 (0.30–0.60) *** | 1.26 (0.86–1.84) |
| 65 or above | 1.03 (0.70–1.51) | 0.08 (0.02–0.37) ** | 0.92 (0.52–1.62) | 0.44 (0.31–0.64) *** | 1.28 (0.86–1.90) |
| Marital status | |||||
| Married | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Unmarried/divorced/widowed | 1.37 (1.11–1.69) ** | 0.82 (0.48–1.40) | 0.81 (0.58–1.12) | 0.81 (0.67–0.99) * | 0.90 (0.72–1.12) |
| Education level | |||||
| Tertiary or above | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Secondary | 1.28 (1.04–1.59) * | 0.66 (0.36–1.21) | 0.37 (0.26–0.52) *** | 0.61 (0.50–0.74) *** | 0.67 (0.54–0.83) *** |
| Primary or below | 1.56 (1.06–2.31) * | 0.64 (0.27–1.52) | 0.28 (0.16–0.48) *** | 0.40 (0.29–0.57) *** | 0.40 (0.27–0.59) *** |
| Employment | |||||
| Employed | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Dependent | 1.09 (0.85–1.41) | 0.53 (0.26–1.06) | 0.88 (0.60–1.29) | 1.13 (0.89–1.42) | 1.61 (1.24–2.09) *** |
| Unemployed | 1.80 (1.20–2.71) ** | 0.35 (0.13–0.92) * | 0.94 (0.48–1.84) | 1.18 (0.76–1.82) | 1.21 (0.76–1.93) |
| Monthly household income (HK$) | |||||
| $80,000 or above | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| $60,000–$79,999 | 0.92 (0.58–1.44) | 0.84 (0.26–2.71) | 0.74 (0.36–1.49) | 0.80 (0.55–1.17) | 0.66 (0.44–0.99) * |
| $40,000–$59,999 | 1.66 (1.18–2.33) ** | 0.74 (0.29–1.86) | 0.65 (0.37–1.15) | 0.80 (0.59–1.09) | 0.64 (0.46–0.90) * |
| $20,000–$39,999 | 1.64 (1.18–2.27) ** | 0.95 (0.38–2.37) | 0.68 (0.39–1.18) | 0.62 (0.46–0.83) ** | 0.58 (0.42–0.80) ** |
| $19,999 or below | 1.52 (1.07–2.16) * | 0.98 (0.39–2.46) | 0.63 (0.35–1.10) | 0.64 (0.47–0.87) ** | 0.60 (0.42–0.86) ** |
| Income change | |||||
| Gain/No change | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Loss | 1.35 (1.11–1.64) ** | 1.25 (0.71–2.20) | 1.09 (0.80–1.48) | 1.25 (1.04–1.51) * | 1.26 (1.02–1.54) * |
| Social capital | |||||
| Presence of interpersonal trust | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Lack of interpersonal trust | 1.58 (1.29–1.93) *** | 0.66 (0.38–1.15) | 0.87 (0.64–1.19) | 1.28 (1.06–1.56) * | 0.95 (0.77–1.16) |
| Presence of social harmony | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Lack of social harmony | 1.17 (0.96–1.43) | 1.40 (0.81–2.42) | 1.03 (0.76–1.40) | 0.92 (0.76–1.10) | 0.95 (0.78–1.16) |
| Presence of sense of belonging | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Lack of sense of belonging | 2.53 (1.66–3.84) *** | 0.31 (0.13–0.74) ** | 0.44 (0.25–0.80) ** | 0.47 (0.31–0.73) *** | 0.58 (0.37–0.91) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, T.W.; Lee, T.M.-c.; Goodwin, R.; Ben-Ezra, M.; Liang, L.; Liu, H.; Hou, W.K. Social Capital, Income Loss, and Psychobehavioral Responses amid COVID-19: A Population-Based Analysis. Int. J. Environ. Res. Public Health 2020, 17, 8888. https://doi.org/10.3390/ijerph17238888
Li TW, Lee TM-c, Goodwin R, Ben-Ezra M, Liang L, Liu H, Hou WK. Social Capital, Income Loss, and Psychobehavioral Responses amid COVID-19: A Population-Based Analysis. International Journal of Environmental Research and Public Health. 2020; 17(23):8888. https://doi.org/10.3390/ijerph17238888
Chicago/Turabian StyleLi, Tsz Wai, Tatia Mei-chun Lee, Robin Goodwin, Menachem Ben-Ezra, Li Liang, Huinan Liu, and Wai Kai Hou. 2020. "Social Capital, Income Loss, and Psychobehavioral Responses amid COVID-19: A Population-Based Analysis" International Journal of Environmental Research and Public Health 17, no. 23: 8888. https://doi.org/10.3390/ijerph17238888
APA StyleLi, T. W., Lee, T. M.-c., Goodwin, R., Ben-Ezra, M., Liang, L., Liu, H., & Hou, W. K. (2020). Social Capital, Income Loss, and Psychobehavioral Responses amid COVID-19: A Population-Based Analysis. International Journal of Environmental Research and Public Health, 17(23), 8888. https://doi.org/10.3390/ijerph17238888





