Effect of Bioactive Glass-Based Root Canal Sealer on the Incidence of Postoperative Pain after Root Canal Obturation
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Treatment Protocol
2.3. Outcome Assessment
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Keskin, C.; Sivas, Y.Ö.; Inan, U.; Özdemir, Ö. Postoperative pain after glide path preparation using manual, reciprocating and continuous rotary instruments: A randomized clinical trial. Int. Endod. J. 2019, 52, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Sathorn, C.; Parashos, P.; Messer, H. The prevalence of postoperative pain and flare-up in single-and multiple-visit endodontic treatment: A systematic review. Int. Endod. J. 2008, 41, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Levin, L.; Amit, A.; Ashkenazi, M. Postoperative pain and use of analgesic agents following various dental procedures. Am. J. Dent. 2006, 19, 245–247. [Google Scholar] [PubMed]
- Arslan, H.; Guven, Y.; Karatas, E.; Doganay, E. Effect of the simultaneous working length control during root canal preparation on postoperative pain. J. Endod. 2017, 43, 1422–1427. [Google Scholar] [CrossRef]
- Patil, A.A.; Joshi, S.B.; Bhagwat, S.V.; Patil, S.A. Incidence of postoperative pain after single visit and two visit root canal therapy: A randomized controlled trial. J. Clin. Diagn. Res. 2016, 10, 9–12. [Google Scholar] [CrossRef]
- Pasqualini, D.; Corbella, S.; Alovisi, M.; Taschieri, S.; Del Fabbro, M.; Migliaretti, G.; Carpegna, G.C.; Scotti, N.; Berutti, E. Postoperative quality of life following single-visit root canal treatment performed by rotary or reciprocating instrumentation: A randomized clinical trial. Int. Endod. J. 2016, 49, 1030–1039. [Google Scholar] [CrossRef]
- Thakur, S.; Emil, J.; Paulaian, B. Evaluation of mineral trioxide aggregate as root canal sealer: A clinical study. Jpn. J. Conserv. Dent. 2013, 16, 494–498. [Google Scholar]
- Graunaite, I.; Skucaite, N.; Lodiene, G.; Agentiene, I.; Machiulskiene, V. Effect of Resin-based and Bioceramic Root Canal Sealers on Postoperative Pain/A Split-mouth Randomized Controlled Trial. J. Endod. 2018, 44, 689–693. [Google Scholar] [CrossRef]
- Yoshii, S.; Morotomi, T.; Fujimoto, M.; Washio, A.; Miyashita, K.; Kitamura, C. A pilot study on the effects of two types of root canal sealer on postoperative pain. J. Jpn. Endod. Associ. 2018, 39, 43–48. [Google Scholar]
- Ferreira, N.S.; Gollo, E.K.F.; Boscato, N.; Arias, A.; Silva, E.J.N.L.D. Postoperative pain after root canal filling with different endodontic sealers- a randomized clinical trial. Braz. Oral. Res. 2020, 34. [Google Scholar] [CrossRef]
- Zhang, W.; Peng, B. Tissue reactions after subcutaneous and intraosseous implantation of iRoot SP, MTA and AH Plus. Dent. Mater. J. 2015, 34, 774–780. [Google Scholar] [CrossRef] [PubMed]
- Tyagi, S.; Mishra, P.; Tyagi, P. Evolution of root canal sealers: An insight story. Eur. J. Gen. Dent. 2013, 2, 199–218. [Google Scholar] [CrossRef]
- Yesiloy, C.; Koren, L.Z.; Morse, D.R.; Kobayashi, C. A comparative tissue toxicity evaluation of established and newer root canal sealers. Oral. Surg. Oral. Med. Oral. Pathol. 1988, 65, 459–467. [Google Scholar] [CrossRef]
- Washio, A.; Morotomi, T.; Yoshii, S.; Kitamura, C. Bioactive glass-based endodontic sealer as a promising root canal filling material without semisolid core materials. Materials 2019, 12, 3967. [Google Scholar] [CrossRef]
- Williams, D.F. Definitions in Biomaterials: Proceedings of the Consensus Conference of the European Society for Biomaterials, Chester, UK, 3–5 March 1986, 1st ed. Elsevier: Amsterdam, NY, USA, 1987; 72p.
- Washio, A.; Yoshii, S.; Morotomi, T.; Maeda, H.; Kitamura, C. Effects of bioactive glass-based sealer on cell migration ability and viability of periodontal ligament cells and osteoblast-like cells. Jpn. J. Conserv. Dent. 2017, 60, 96–104. [Google Scholar]
- Washio, A.; Kitamura, C. The next-generation bioacvite glass-based root canal sealer inducing the ideal wound healing environment of periapical tissue Nishika Canal Sealer BG. Dent. Diam. 2017, 42, 178–183. [Google Scholar]
- Morotomi, T.; Hanada, K.; Washio, A.; Yoshii, S.; Matsuo, K.; Kitamura, C. Effect of newly-developed bioactive glass root canal sealer on periapical tissue of rat’s molar. Jpn. J. Conserv. Dent. 2017, 60, 120–127. [Google Scholar]
- Ozawa, T.; Koshino, T.; Arai, T. Effects of 3% weak-alkaline EDTA solution on the removal of smear layer of root canal walls. Jpn. J. Conserv. Dent. 2003, 46, 435–438. [Google Scholar]
- Schwendicke, F.; Göstemeyer, G. Cost-effectiveness of single-versus multistep root canal treatment. J. Endod. 2016, 42, 1446–1452. [Google Scholar] [CrossRef]
- Ali, A.; Olivieri, J.G.; Duran-Sindreu, F.; Abella, F.; Roig, M.; Garcia-Font, M. Influence of preoperative pain intensity on postoperative pain after root canal treatment: A prospective clinical study. J. Dent. 2016, 45, 39–42. [Google Scholar] [CrossRef]
- Arias, A.; de la Macorra, J.C.; Hidalgo, J.J.; Azabal, M. Predictive models of pain following root canal treatment: A prospective clinical study. Int. Endod. J. 2013, 46, 784–793. [Google Scholar] [CrossRef] [PubMed]
- Farrar, J.T.; Berlin, J.A.; Strom, B.L. Clinically important changes in acute pain outcome measures: A validation study. J. Pain. Symptom Manag. 2003, 25, 406–411. [Google Scholar] [CrossRef]
- Boonstra, A.M.; Schiphorst Preuper, H.R.; Reneman, M.F.; Posthumus, J.B.; Stewart, R.E. Reliability and validity of the visual analogue scale for disability in patients with chronic musculoskeletal pain. Int. J. Rehabil. Res. 2008, 31, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Closs, S.J.; Barr, B.; Briggs, M.; Cash, K.; Seers, K. A comparison of five pain assessment scales for nursing home residents with varying degrees of cognitive impairment. J. Pain. Symptom Manag. 2004, 27, 196–205. [Google Scholar] [CrossRef]
- Gagliese, L.; Weizblit, N.; Ellis, W.; Chan, V.W.S. The measurement of postoperative pain: A comparison of intensity scales in younger and older surgical patients. Pain 2005, 117, 412–420. [Google Scholar] [CrossRef]
- Peters, M.L.; Patijn, J.; Lamé, I. Pain assessment in younger and older pain patients: Psychometric properties and patient preference of five commonly used measures of pain intensity. Pain. Med. 2007, 8, 601–610. [Google Scholar] [CrossRef]
- Gudlavalleti, B.; Patil, A.A. Comparative evaluation of postoperative pain after root canal treatment using three different sealers, Viz., Tubli-Seal EWT, Apexit Plus, AH Plus: An in-vivo study. J. Clin. Diagn. Res. 2020, 14, 4–9. [Google Scholar]
- Gotler, M.; Bar-Gil, B.; Ashkenazi, M. Postoperative pain after root canal treatment: A prospective cohort study. Int. J. Dent. 2012, 2012. [Google Scholar] [CrossRef]
- Ali, S.G.; Mulay, S.; Palekar, A.; Sejpal, B.; Joshi, A.; Gufran, H. Prevalence of and factors affecting post-obturation pain following single visit root canal treatment in Indian population: A prospective, randomized clinical trial. Contemp. Clin. Dent. 2012, 3, 459–463. [Google Scholar] [CrossRef]
- Shresha, R.; Shrestha, D.; Kayastha, R. Postoperative pain and associated factors in patients undergoing single visit root canal treatment on teeth with vital pulp. Kathmandu Univ. Med. J. 2018, 16, 220–223. [Google Scholar]
- Scelza, M.Z.; Coil, J.; Alves, G.G. Effect of time of extraction on the biocompatibility of endodontic sealers with primary human fibroblasts. Braz. Oral. Res. 2012, 26, 340–424. [Google Scholar] [CrossRef] [PubMed]
- Ehsani, M.; Zabihi, E.; Gharouee, H. A comparison between cytotoxicity induced by two resin-based sealers (2 Seal and AH Plus) in Saos-2 and MG-63 cell lines. Int. J. Mol. Cell. Med. 2012, 1, 197–202. [Google Scholar] [PubMed]
- Morotomi, T.; Hirata-Tsuchiya, S.; Washio, A.; Kitamura, C. Effects of 4-META/MMA- TBB resin at different. curing stages on osteoblasts and gingival epithelial cells. J. Adhes. Dent. 2016, 18, 111–118. [Google Scholar] [PubMed]
- Silva, E.J.N.L.D.; Aghazadeh, M.; Jafari, S.; Khaki, F.; Kabiri, F. In vitro Cytotoxicity Comparison of MTA Fillapex, AH-26 and Apatite Root Canal Sealer at Different Setting Times. Iran. Endod. J. 2017, 12, 162–167. [Google Scholar]
- Silva, E.J.N.L.D.; Accorsi-Mendonça, T.; Pedrosa, A.C.; Granjeiro, J.M.; Zaia, A.A. Long-term cytotoxicity, pH and dissolution rate of AH Plus and MTA Fillapex. Braz. Dent. J. 2016, 27, 419–423. [Google Scholar] [CrossRef]
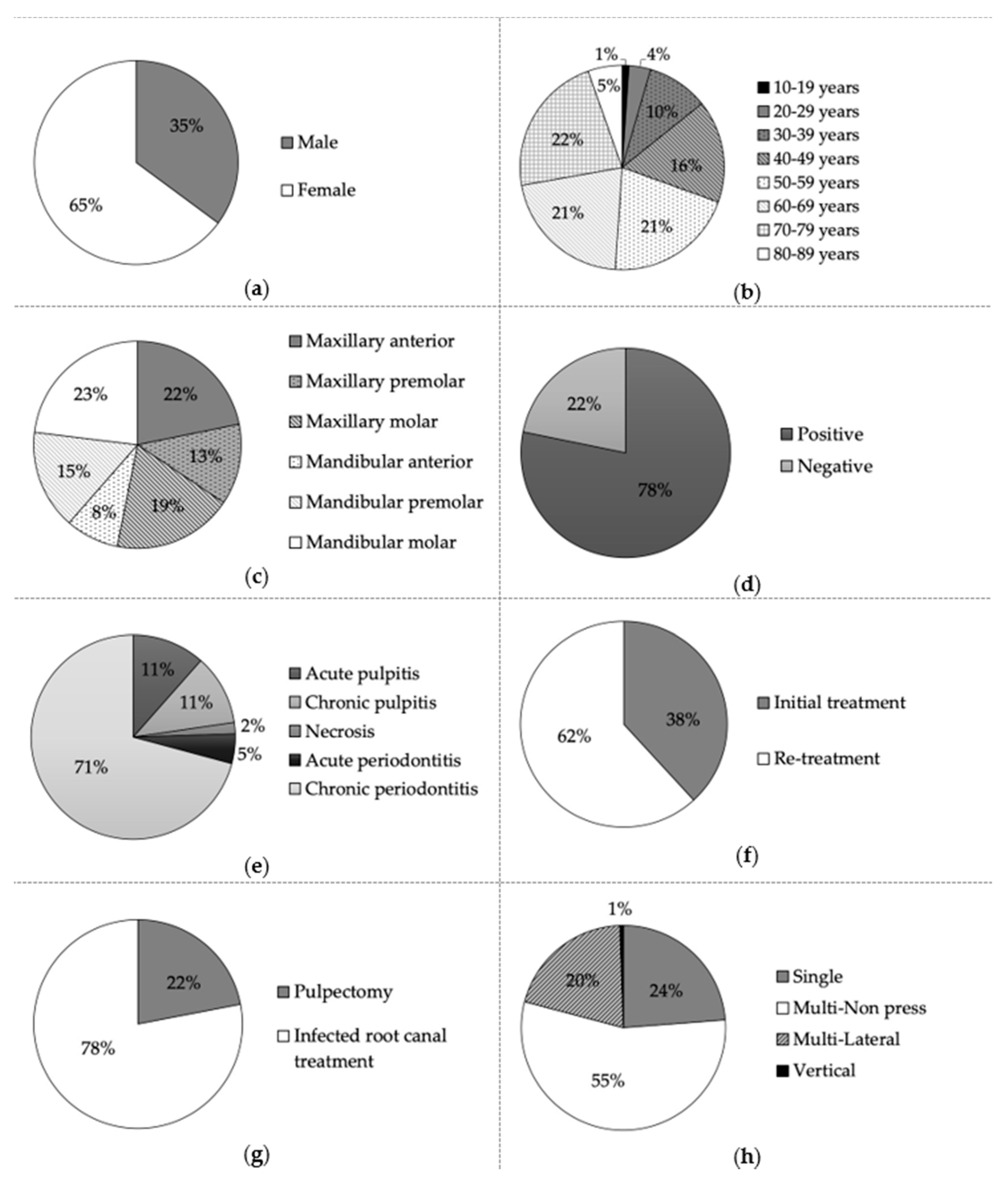
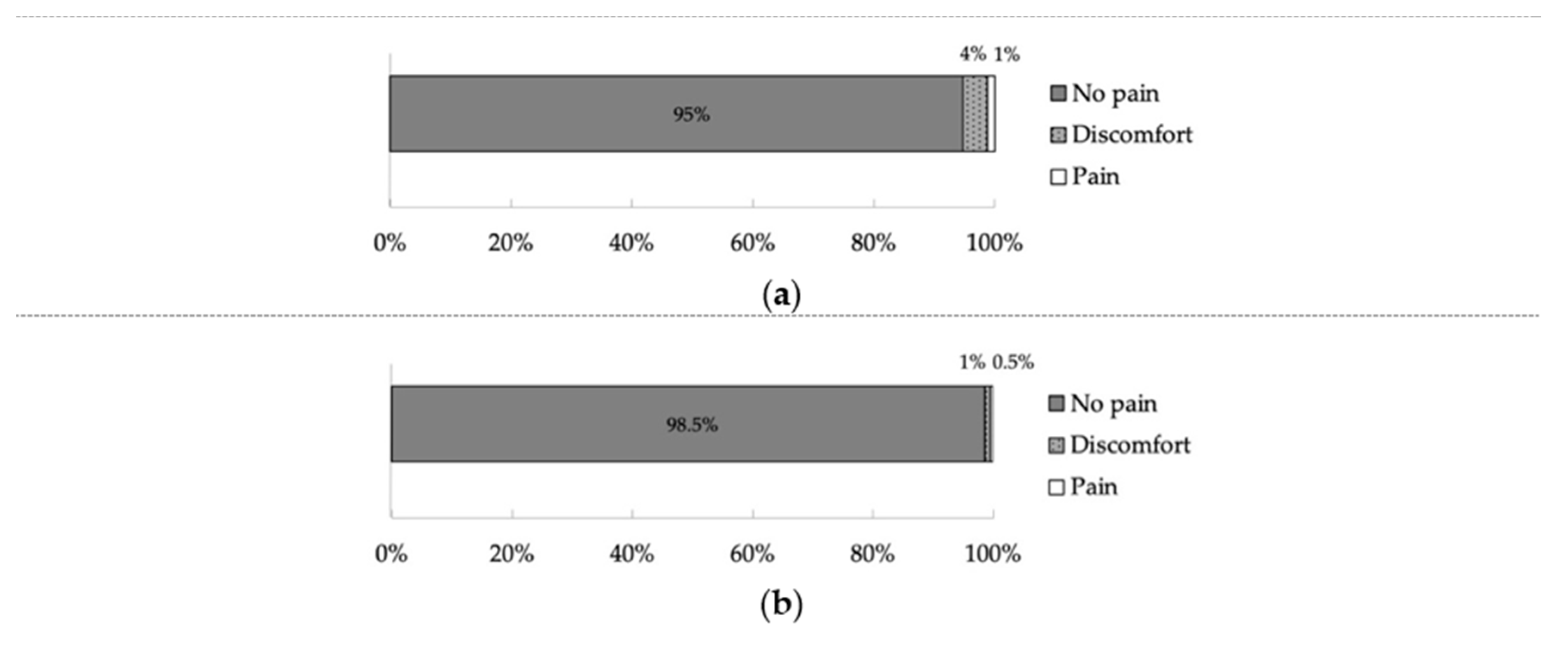
| Total, n = 555 | No Pain (n = 525) | Discomfort (n = 22) | Pain (n = 8) | p Value | |
|---|---|---|---|---|---|
| Gender | Male | 189 | 5 | 1 | 0.178 |
| Female | 336 | 17 | 7 | ||
| Age | <50 years | 164 | 2 | 3 | 0.079 |
| ≥50 years | 361 | 20 | 5 | ||
| Arch | Maxillary | 278 | 14 | 3 | 0.413 |
| Mandibular | 247 | 8 | 5 | ||
| Type of tooth | Anterior | 155 | 11 | 1 | 0.238 |
| Premolar | 148 | 5 | 3 | ||
| Molar | 222 | 6 | 4 | ||
| Symptom | Positive | 409 | 17 | 8 | 0.893 |
| Negative | 116 | 5 | 0 | ||
| Diagnosis | Acute pulpitis | 59 | 2 | 3 | 0.196 |
| Chronic pulpitis | 59 | 2 | 1 | ||
| Necrosis | 9 | 1 | 0 | ||
| Acute periodontitis | 24 | 1 | 1 | ||
| Chronic periodontitis | 385 | 16 | 3 | ||
| Initial-/Re- treatment | Initial treatment | 198 | 8 | 6 | 0.097 |
| Re-treatment | 327 | 14 | 2 | ||
| Endodontic treatments | Pulpectomy | 205 | 3 | 4 | 0.044 * |
| Infected root canal treatment | 320 | 19 | 4 | ||
| Root canal obturation techniques | Single | 125 | 4 | 3 | 0.256 |
| Multi-Non press | 285 | 17 | 5 | ||
| Multi-Lateral | 112 | 1 | 0 | ||
| Vertical | 3 | 0 | 0 | ||
| Total, n = 555 | No Pain (n = 547) | Discomfort (n = 5) | Pain (n = 3) | p Value | |
|---|---|---|---|---|---|
| Gender | Male | 193 | 3 | 0 | 0.431 |
| Female | 354 | 2 | 3 | ||
| Age | <50 years | 168 | 1 | 0 | 0.452 |
| ≥50 years | 379 | 4 | 3 | ||
| Arch | Maxillary | 289 | 4 | 2 | 0.430 |
| Mandibular | 258 | 1 | 1 | ||
| Type of tooth | Anterior | 164 | 2 | 1 | 0.507 |
| Premolar | 156 | 0 | 0 | ||
| Molar | 227 | 3 | 2 | ||
| Symptom | Positive | 426 | 5 | 3 | 0.894 |
| Negative | 121 | 0 | 0 | ||
| Diagnosis | Acute pulpitis | 64 | 0 | 0 | 0.860 |
| Chronic pulpitis | 61 | 1 | 0 | ||
| Necrosis | 10 | 0 | 0 | ||
| Acute periodontitis | 26 | 0 | 0 | ||
| Chronic periodontitis | 386 | 4 | 3 | ||
| Initial-/Re-treatment | Initial treatment | 210 | 2 | 0 | 0.393 |
| Re-treatment | 337 | 3 | 3 | ||
| Endodontic treatments | Pulpectomy | 121 | 1 | 0 | 0.650 |
| Infected root canal treatment | 426 | 4 | 3 | ||
| Root canal obturation techniques | Single | 131 | 0 | 1 | 0.556 |
| Multi-Non press | 300 | 5 | 2 | ||
| Multi-Lateral | 113 | 0 | 0 | ||
| Vertical | 3 | 0 | 0 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Washio, A.; Miura, H.; Morotomi, T.; Ichimaru-Suematsu, M.; Miyahara, H.; Hanada-Miyahara, K.; Yoshii, S.; Murata, K.; Takakura, N.; Akao, E.; et al. Effect of Bioactive Glass-Based Root Canal Sealer on the Incidence of Postoperative Pain after Root Canal Obturation. Int. J. Environ. Res. Public Health 2020, 17, 8857. https://doi.org/10.3390/ijerph17238857
Washio A, Miura H, Morotomi T, Ichimaru-Suematsu M, Miyahara H, Hanada-Miyahara K, Yoshii S, Murata K, Takakura N, Akao E, et al. Effect of Bioactive Glass-Based Root Canal Sealer on the Incidence of Postoperative Pain after Root Canal Obturation. International Journal of Environmental Research and Public Health. 2020; 17(23):8857. https://doi.org/10.3390/ijerph17238857
Chicago/Turabian StyleWashio, Ayako, Hiroki Miura, Takahiko Morotomi, Miki Ichimaru-Suematsu, Hirotake Miyahara, Kaori Hanada-Miyahara, Shinji Yoshii, Kazumasa Murata, Nana Takakura, Eiichi Akao, and et al. 2020. "Effect of Bioactive Glass-Based Root Canal Sealer on the Incidence of Postoperative Pain after Root Canal Obturation" International Journal of Environmental Research and Public Health 17, no. 23: 8857. https://doi.org/10.3390/ijerph17238857
APA StyleWashio, A., Miura, H., Morotomi, T., Ichimaru-Suematsu, M., Miyahara, H., Hanada-Miyahara, K., Yoshii, S., Murata, K., Takakura, N., Akao, E., Fujimoto, M., Matsuyama, A., & Kitamura, C. (2020). Effect of Bioactive Glass-Based Root Canal Sealer on the Incidence of Postoperative Pain after Root Canal Obturation. International Journal of Environmental Research and Public Health, 17(23), 8857. https://doi.org/10.3390/ijerph17238857




