Evaluating Health Literacy among Adolescent and Young Adult Pregnant Women from a Low-Income Area of Northeast Brazil
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Site and Design
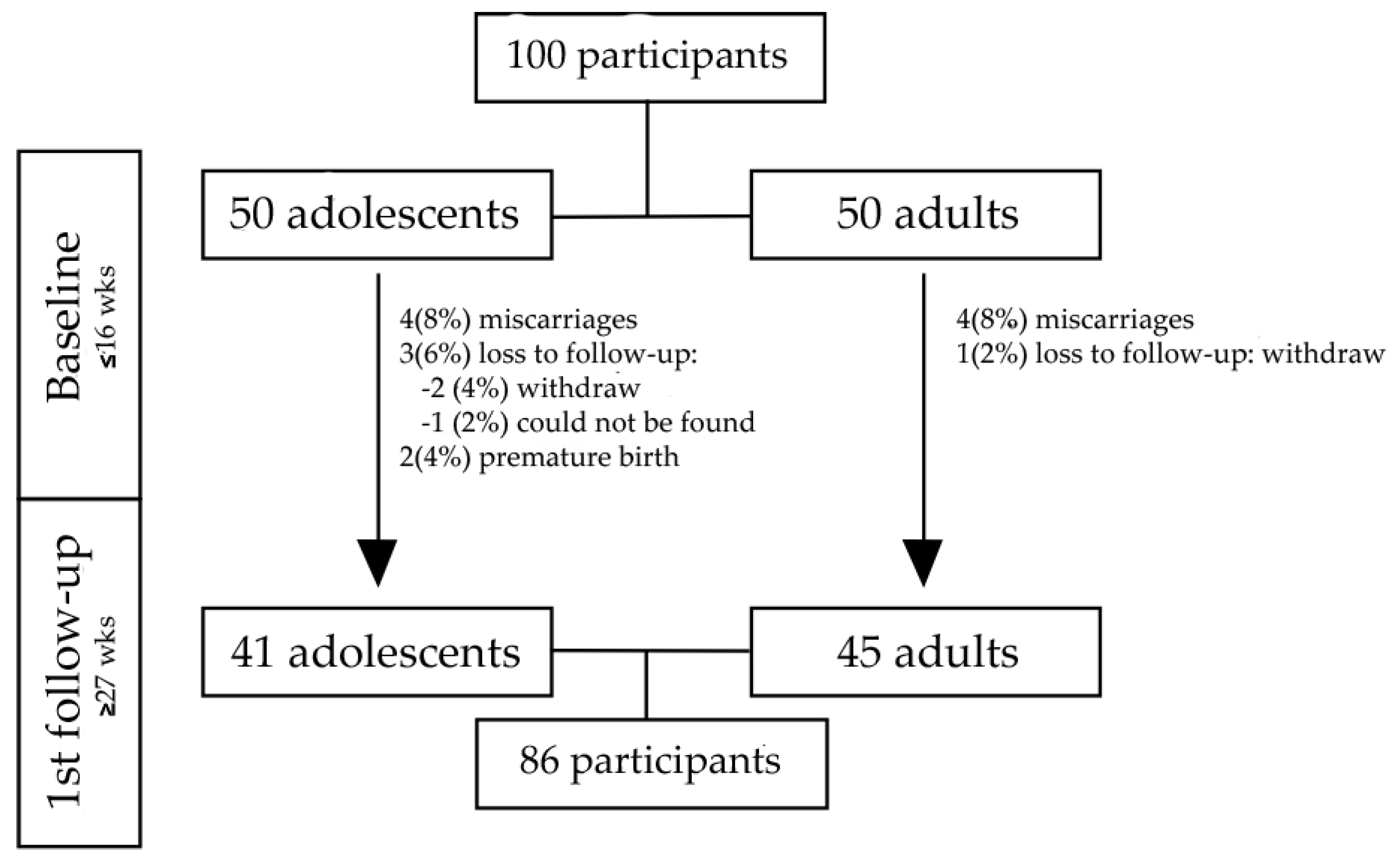
2.2. Population and Sample
2.3. Procedures
2.3.1. Socioeconomic Data
2.3.2. Prenatal Care Adequacy
2.3.3. Social Support
2.3.4. Health Literacy
2.4. Ethics
2.5. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Characteristics | SAHLPA-18 Score (Range from 0–18) | ||
|---|---|---|---|
| Median (q25–q75) | |||
| Adolescents N = 41 | Adults N = 45 | p Value a | |
| Race/color b | |||
| White | 8 (6–13) | 11.5 (8–15.3) | 0.084 |
| Mixed-race/Black | 9 (6–11) | 15.5 (10–17) | <0.001 |
| Self-perceived school performance compared to peers | |||
| Better than average | 9 (7–12) | 16 (12–17) | <0.001 |
| Average/worse | 8 (5–10.3) | 10 (7.5–15) | 0.028 |
| Income sufficiency | |||
| Very well | 6 (3–9) | 10 (9–15.3) | 0.022 |
| Suitable | 9 (7–12.5) | 15 (10.8–17) | 0.001 |
| Not well | 7 (4.5–9.5) | 13 (9–14.5) | 0.036 |
| Receiving “Bolsa Família” b | |||
| Yes | 9 (6–11) | 11 (8.5–15.5) | 0.015 |
| No | 7.5 (6.5–11.3) | 16 (13–17) | <0.001 |
| Number of prenatal consultations b | |||
| ≥6 | 9 (6.5–11) | 12.5 (10.3–16) | 0.005 |
| <6 | 8 (6–11.8) | 15 (8.3–17) | 0.001 |
| Social Support | |||
| Friends | |||
| High | 8 (5.5–10.8) | 14.5 (10–16) | <0.001 |
| Low/none | 9 (6–12) | 10 (9–17) | 0.113 |
| Grandparents | |||
| High | 9 (7–11) | 13 (8.8–16) | 0.001 |
| Low/none | 6.5 (4.5–13.3) | 14 (9–17) | 0.003 |
| Parents | |||
| High | 8 (5–11.5) | 15 (10.5–16) | <0.001 |
| Low/none | 8.5 (7–11) | 9 (7.3–12.8) | 0.787 |
| Partner | |||
| High | 8 (5–11) | 13 (9–16) | <0.001 |
| Low/none | 9 (7–13) | 15 (10.3–17) | 0.014 |
| Siblings | |||
| High | 8 (5–11.3) | 13 (10–16) | <0.001 |
| Low/none | 9 (6–11) | 13.5 (7.8–16.3) | 0.062 |
References
- Dodson, S.; Good, S.; Osborne, R.H. Health Literacy Toolkit for Lowand Middle- Income Countries: A Series of Information Sheets to Empower Communities and Strengthen Health Systems; World Health Organization, Regional Office for South-East Asia: New Delhi, India, 2015; ISBN 9789290224754. [Google Scholar]
- Sørensen, K.; Van Den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed]
- Vandenbosch, J.; Van den Broucke, S.; Vancorenland, S.; Avalosse, H.; Verniest, R.; Callens, M. Health literacy and the use of healthcare services in Belgium. J. Epidemiol. Commun. Health 2016, 70, 1032–1038. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Haun, J.N.; Patel, N.R.; French, D.D.; Campbell, R.R.; Bradham, D.D.; Lapcevic, W.A. Association between health literacy and medical care costs in an integrated healthcare system: A regional population based study. BMC Health Serv. Res. 2015, 15, 249. [Google Scholar] [CrossRef] [PubMed]
- Toci, E.; Burazeri, G.; Jerliu, N.; Sørensen, K.; Ramadani, N.; Hysa, B.; Brand, H. Health literacy, self-perceived health and self-reported chronic morbidity among older people in Kosovo. Health Promot. Int. 2015, 30, 667–674. [Google Scholar] [CrossRef]
- Mantwill, S.; Monestel-Umaña, S.; Schulz, P.J. The relationship between health literacy and health disparities: A systematic review. PLoS ONE 2015, 10. [Google Scholar] [CrossRef]
- Bröder, J.; Okan, O.; Bauer, U.; Bruland, D.; Schlupp, S.; Bollweg, T.M.; Saboga-Nunes, L.; Bond, E.; Sørensen, K.; Bitzer, E.-M.; et al. Health literacy in childhood and youth: A systematic review of definitions and models. BMC Public Health 2017, 17, 361. [Google Scholar] [CrossRef]
- Manganello, J.A. Health literacy and adolescents: A framework and agenda for future research. Health Educ. Res. 2008, 23, 840–847. [Google Scholar] [CrossRef]
- Sansom-Daly, U.M.; Lin, M.; Robertson, E.G.; Wakefield, C.E.; McGill, B.C.; Girgis, A.; Cohn, R.J. Health Literacy in Adolescents and Young Adults: An Updated Review. J. Adolesc. Young Adult Oncol. 2016, 5, 106–118. [Google Scholar] [CrossRef]
- Dongarwar, D.; Salihu, H.M. Influence of Sexual and Reproductive Health Literacy on Single and Recurrent Adolescent Pregnancy in Latin America. J. Pediatr. Adolesc. Gynecol. 2019, 32, 506–513. [Google Scholar] [CrossRef]
- WHO. Early marriages, adolescent and young pregnancies Report by the Secretariat. Sixty-Fifth World Health Assem. 2012. Available online: https://apps.who.int/iris/handle/10665/78901 (accessed on 15 March 2019).
- World Health Organization. Adolescent Pregnancy. Available online: https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy (accessed on 5 February 2020).
- Needham, H.E.; Wiemann, C.M.; Tortolero, S.R.; Chacko, M.R. Relationship Between Health Literacy, Reading Comprehension, and Risk for Sexually Transmitted Infections in Young Women. J. Adolesc. Health 2010, 46, 506–508. [Google Scholar] [CrossRef] [PubMed]
- Magnani, R.J.; Karim, A.M.; WEISS, L.A.; Bond, K.C.; Lemba, M.; Morgan, G.T. Reproductive Health Risk and Protective Factors Among Youth in Lusaka, Zambia. J. Adolesc. Health 2002, 30, 76–86. [Google Scholar] [CrossRef]
- Champion, J.D.; Harlin, B.; Collins, J.L. Sexual risk behavior and STI health literacy among ethnic minority adolescent women. Appl. Nurs. Res. 2013, 26, 204–209. [Google Scholar] [CrossRef] [PubMed]
- Govender, D.; Naidoo, S.; Taylor, M. Knowledge, attitudes and peer influences related to pregnancy, sexual and reproductive health among adolescents using maternal health services in Ugu, KwaZulu-Natal, South Africa. BMC Public Health 2019, 19, 928. [Google Scholar] [CrossRef]
- Fleary, S.A.; Joseph, P.; Pappagianopoulos, J.E. Adolescent health literacy and health behaviors: A systematic review. J. Adolesc. 2018, 62, 116–127. [Google Scholar] [CrossRef]
- IBGE—Instituto Brasileiro de Geografia e Estatística Estimativas da População. 2019. Available online: https://cidades.ibge.gov.br (accessed on 3 March 2019).
- Nunnally, J.; Bernstein, I. Psychometric Theory, 3rd ed.; McGraw-Hill: New York, NY, USA, 1994. [Google Scholar]
- Allal, N.; Sear, R.; Prentice, A.M.; Mace, R. An evolutionary model of stature, age at first birth and reproductive success in Gambian women. Proc. R. Soc. Lond. Ser. B Biol. Sci. 2004, 271, 465–470. [Google Scholar] [CrossRef]
- Gallagher, L.G.; Davis, L.B.; Ray, R.M.; Psaty, B.M.; Gao, D.L.; Checkoway, H.; Thomas, D.B. Reproductive history and mortality from cardiovascular disease among women textile workers in Shanghai, China. Int. J. Epidemiol. 2011, 40, 1510–1518. [Google Scholar] [CrossRef]
- Guo, S.; Yu, X.; Davis, E.; Armstrong, R.; Riggs, E.; Naccarella, L. Adolescent health literacy in beijing and melbourne: A cross-cultural comparison. Int. J. Environ. Res. Public Health 2020, 17, 1242. [Google Scholar] [CrossRef]
- Merritt, M.A.; Riboli, E.; Murphy, N.; Kadi, M.; Tjønneland, A.; Olsen, A.; Overvad, K.; Dossus, L.; Dartois, L.; Clavel-Chapelon, F.; et al. Reproductive factors and risk of mortality in the European Prospective Investigation into Cancer and Nutrition; a cohort study. BMC Med. 2015, 13, 252. [Google Scholar] [CrossRef]
- Câmara, S.M.; Sentell, T.; Bassani, D.G.; Domingues, M.R.; Pirkle, C.M. Strengthening health research capacity to address adolescent fertility in Northeast Brazil. J. Glob. Health 2019, 9, 10303. [Google Scholar] [CrossRef]
- Qualtrics Software 2020. Available online: www.qualtrics.com (accessed on 10 May 2017).
- Brasil Ministério da Cidadania. Secretaria Especial do Desenvolvimento Social. Available online: https://www.gov.br/cidadania/pt-br/acoes-e-programas/bolsa-familia (accessed on 3 February 2020).
- Portaria no 1.459, de 24 de junho de 2011. Institui, no âmbito do Sistema Único de Saúde—SUS—A Rede Cegonha; Diário Oficial da União: Brasília, Brasil, 2011.
- Ahmed, T.; Belanger, E.; Vafaei, A.; Koné, G.K.; Alvarado, B.; Béland, F.; Zunzunegui, M.V. Validation of a Social Networks and Support Measurement Tool for Use in International Aging Research: The International Mobility in Aging Study. J. Cross. Cult. Gerontol. 2018, 33, 101–120. [Google Scholar] [CrossRef] [PubMed]
- Apolinario, D.; de Braga, R.C.O.P.; Magaldi, R.M.; Busse, A.L.; Campora, F.; Bruc, K.S.; Lees, S.Y.D. Short assessment of health literacy for portuguese-speaking adults. Rev. Saude Publica 2012, 46, 702–711. [Google Scholar] [CrossRef] [PubMed]
- Svendsen, M.T.; Bak, C.K.; Sørensen, K.; Pelikan, J.; Riddersholm, S.J.; Skals, R.K.; Mortensen, R.N.; Maindal, H.T.; Bøggild, H.; Nielsen, G.; et al. Associations of health literacy with socioeconomic position, health risk behavior, and health status: A large national population-based survey among Danish adults. BMC Public Health 2020, 20. [Google Scholar] [CrossRef] [PubMed]
- Pelikan, J.; Ganahl, K. Measuring Health Literacy in General Populations: Primary Findings from the HLS-EU Consortium’s Health Literacy Assessment Effort. Stud. Health Technol. Inf. 2017, 240, 34–59. [Google Scholar] [CrossRef]
- Paiva, D.; Silva, S.; Severo, M.; Moura-ferreira, P.; Lunet, N.; Azevedo, A. Prevalência de Literacia em Saúde Inadequada em Portugal Medida com o Newest Vital Sign Limited Health Literacy in Portugal Assessed with the Newest Vital Sign. Acta Med. Port. 2017, 30, 861–869. [Google Scholar] [CrossRef]
- Rocha, P.C.; Rocha, D.C.; Lemos, S.M.A. Functional health literacy and quality of life of high-school adolescents in state schools in Belo Horizonte. CoDAS 2017, 29, e20160208. [Google Scholar] [CrossRef]
- Sukys, S.; Cesnaitiene, V.J.; Ossowsky, Z.M. Is health education at university associated with students’ health literacy? evidence from cross-sectional study applying HLS-EU-Q. Biomed Res. Int. 2017. [Google Scholar] [CrossRef]
- Putra, D.A.; Prihatanto, F.S.I.; Lestari, P. Health Literacy and Pre-Eclampsia Knowledge of Pregnant Mother in Primary Health Care in Surabaya. Biomol. Health Sci. J. 2020, 03, 80–82. [Google Scholar] [CrossRef]
- Akbarinejad, F.; Soleymani, M.; Shahrzadi, L. The relationship between media literacy and health literacy among pregnant women in health centers of Isfahan. J. Educ. Health Promot. 2017, 6, 17. [Google Scholar] [CrossRef]
- Castro-Sánchez, E.; Vila-Candel, R.; Soriano-Vidal, F.J.; Navarro-Illana, E.; Díez-Domingo, J. Influence of health literacy on acceptance of influenza and pertussis vaccinations: A cross-sectional study among Spanish pregnant women. BMJ Open 2018, 8, e022132. [Google Scholar] [CrossRef]
- Dadipoor, S.; Ramezankhani, A.; Alavi, A.; Aghamolaei, T.; Safari-Moradabadi, A. Pregnant Women’s Health Literacy in the South of Iran. J. Fam. Reprod. Health 2017, 11, 211–218. [Google Scholar]
- Davis, T.C.; Long, S.W.; Jackson, R.H.; Mayeaux, E.J.; George, R.B.; Murphy, P.W.; Crouch, M. Rapid estimate of adult literacy in medicine: A shortened screening instrument—PubMed. Fam. Med. 1993, 25, 391–395. [Google Scholar]
- Parker, R.M.; Baker, D.W.; Willia, M.V.; Nurss, J.R. The test of functional health literacy in adults: A new instrument for measuring patients’ literacy skills. J. Gen. Intern. Med. 1995, 10, 537–541. [Google Scholar] [CrossRef] [PubMed]
- Carthery-Goulart, M.T.; Anghinah, R.; Areza-Fegyveres, R.; Bahia, V.S.; Dozzi Brucki, S.M.; Damin, A.; Formigoni, A.P.; Frota, N.; Guariglia, C.; Jacinto, A.F.; et al. Desempenho de uma população brasileira no teste de alfabetização funcional para adultos na área de saúde. Rev. Saude Publica 2009, 43, 631–638. [Google Scholar] [CrossRef] [PubMed]
- Chisolm, D.J.; Manganello, J.A.; Kelleher, K.J.; Marshal, M.P. Health literacy, alcohol expectancies, and alcohol use behaviors in teens. Patient Educ. Couns. 2014, 97, 291–296. [Google Scholar] [CrossRef]
- Chang, L.-C. Health literacy, self-reported status and health promoting behaviours for adolescents in Taiwan. J. Clin. Nurs. 2011, 20, 190–196. [Google Scholar] [CrossRef]
- Valerio, M.A.; Peterson, E.L.; Wittich, A.R.; Joseph, C.L.M. Examining health literacy among urban African-American adolescents with asthma. J. Asthma 2016, 53, 1041–1047. [Google Scholar] [CrossRef]
- Lightfoot, M.A.; Cheng, J.W.; Hu, X.; Tschokert, M.; McCracken, C.; Kirsch, A.J.; Smith, E.A.; Cerwinka, W.H.; Arlen, A.M.; Chamberlin, D.A.; et al. Assessment of health literacy in adolescents with spina bifida and their caregivers: A multi-institutional study. J. Pediatr. Urol. 2020, 16, 167.e1–167.e6. [Google Scholar] [CrossRef]
- Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs Health literacy: Report of the Council on Scientific Affairs. Ad Hoc Committee on Health Literacy for the Council on Scientific Affairs, American Medical Association—PubMed. JAMA 1999, 281, 552–557.
- Institute of Medicine. Health Literacy: A Prescription to End Confusion; Nielsen-Bohlman, L., Panzer, A.M., Kindig, D.A., Eds.; National Academies Press: Washington, DC, USA, 2004; ISBN 978-0-309-28332-8. [Google Scholar]
- WHO. Adolescent Pregnancy Fact Sheet; WHO: Geneva, Switzerland, 2014; p. 1. [Google Scholar]
- Demirci, O.; Yılmaz, E.; Tosun, Ö.; Kumru, P.; Arınkan, A.; Mahmutoğlu, D.; Selçuk, S.; Dolgun, Z.N.; Arısoy, R.; Erdoğdu, E.; et al. Effect of young maternal age on obstetric and perinatal outcomes: Results from the tertiary center in Turkey. Balk. Med. J. 2016, 33, 344–349. [Google Scholar] [CrossRef]
- Marvin-Dowle, K.; Kilner, K.; Burley, V.J.; Soltani, H. Impact of adolescent age on maternal and neonatal outcomes in the Born in Bradford cohort. BMJ Open 2018, 8. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Why Health Literacy is Important. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/health-literacy/why-health-literacy-is-important (accessed on 8 November 2020).
- Ran, M.; Peng, L.; Liu, Q.; Pender, M.; He, F.; Wang, H. The association between quality of life(QOL) and health literacy among junior middle school students: A cross-sectional study 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Public Health 2018, 18. [Google Scholar] [CrossRef]
- Godoy, J.A.; Abrahão, R.C.; Halpern, R. Autopercepção de dificuldades escolares em alunos do ensino fundamental e médio em município do Rio Grande do Sul. Aletheia 2013, 41, 121–133. [Google Scholar]
- Beluce, A.C.; Inácio, A.L.M.; de Oliveira, K.L.; Franco, S.A.P. Reading Comprehension and Self-Perceived School Performance in Elementary School. Psico-Usf 2018, 23, 597–607. [Google Scholar] [CrossRef]
- Duong, T.V.; Aringazina, A.; Baisunova, G.; Nurjanah; Pham, T.V.; Pham, K.M.; Truong, T.Q.; Nguyen, K.T.; Oo, W.M.; Mohamad, E.; et al. Measuring health literacy in Asia: Validation of the HLS-EU-Q47 survey tool in six Asian countries. J. Epidemiol. 2017, 27, 80–86. [Google Scholar] [CrossRef]
- Cho, R.N.; Plunkett, B.A.; Wolf, M.S.; Simon, C.E.; Grobman, W.A. Health literacy and patient understanding of screening tests for aneuploidy and neural tube defects. Prenat. Diagn. 2007, 27, 463–467. [Google Scholar] [CrossRef]
- Endres, L.K.; Sharp, L.K.; Haney, E.; Dooley, S.L. Health literacy and pregnancy preparedness in pregestational diabetes. Diabetes Care. 2004, 27, 331–334. [Google Scholar] [CrossRef]
- Fry-Bowers, E.K.; Maliski, S.; Lewis, M.A.; Macabasco-O’Connell, A.; DiMatteo, R. The Association of Health Literacy, Social Support, Self-Efficacy and Interpersonal Interactions With Health Care Providers in Low-Income Latina Mothers. J. Pediatr. Nurs. 2014, 29, 309–320. [Google Scholar] [CrossRef]
- Liu, Y.; Xue, L.; Xue, H.; Hou, P. Health literacy, self-care agency, health status and social support among elderly Chinese nursing home residents. Health Educ. J. 2018, 77, 303–311. [Google Scholar] [CrossRef]
- Li, Y.; Hu, L.; Mao, X.; Shen, Y.; Xue, H.; Hou, P.; Liu, Y. Health literacy, social support, and care ability for caregivers of dementia patients: Structural equation modeling. Geriatr. Nurs. 2020, 41, 600–607. [Google Scholar] [CrossRef]
| Characteristics | Total | Adolescents (N = 41) | Adults (N = 45) | |
|---|---|---|---|---|
| N (%) or Median (q25:q75) a | p Value | |||
| Age | 23 (17:25) | 17 (16:18) | 25 (24:26) | <0.001 e |
| Race/color b | ||||
| White | 29 (34.1) | 11 (26.8) | 18 (40.9) | 0.171 c |
| Mixed-race/Black | 56 (65.9) | 30 (73.2) | 26 (59.1) | |
| Self-perceived school performance compared to peers | ||||
| Better than average | 39 (45.3) | 15 (36.6) | 24 (53.3) | 0.119 c |
| Average/worse | 47 (54.7) | 26 (63.4) | 21 (46.7) | |
| Income sufficiency | ||||
| Very well | 19 (22.1) | 7 (17.1) | 12 (26.7) | 0.101 c |
| Suitable | 55 (64.0) | 25 (61.0) | 30 (66.7) | |
| Not well | 12 (14.0) | 9 (22.0) | 3 (6.7) | |
| Receiving “Bolsa Família” b | ||||
| Yes | 56 (65.9) | 31 (75.6) | 25 (56.8) | 0.068 c |
| No | 29 (34.1) | 10 (24.4) | 19 (43.2) | |
| Number of antenatal consultations b | ||||
| ≥6 | 33 (38.8) | 17 (41.5) | 16 (36.4) | 0.630 c |
| <6 | 52 (61.2) | 24 (58.5) | 28 (63.6) | |
| Proportion of adequacy of antenatal care d | 53.84 (38.46:69.23) | 38.46 (23.08:69.23) | 61.54 (46.15:69.23) | 0.005 e |
| Social Support | ||||
| Friends | ||||
| High | 54 (62.8) | 20 (48.8) | 34 (75.6) | 0.010 c |
| Low/none | 32 (37.2) | 21 (51.2) | 11 (24.4) | |
| Grandparent | ||||
| High | 57 (66.3) | 31 (75.6) | 26 (57.8) | 0.081 c |
| Low/none | 29 (33.7) | 10 (24.4) | 19 (42.2) | |
| Parents | ||||
| High | 62 (72.1) | 25 (61.0) | 37 (82.2) | 0.028 c |
| Low/none | 24 (27.9) | 16 (39.0) | 8 (17.8) | |
| Partner | ||||
| High | 59 (68.6) | 26 (63.4) | 33 (73.3) | 0.322 c |
| Low/none | 27 (31.4) | 15 (36.6) | 12 (26.7) | |
| Siblings | ||||
| High | 61 (70.9) | 26 (63.4) | 35 (77.8) | 0.143 c |
| Low/none | 25 (29.1) | 15 (36.6) | 10 (22.2) | |
| Total | 86 (100) | 41 (47.7) | 45 (52.3) | |
| Characteristics | Health Literacy | |||||
|---|---|---|---|---|---|---|
| Adequate N = 23 | Inadequate N = 63 | p Value | SAHLPA-18 Score a (0–18) | p Value | ||
| N (%) | Median | q25–q75 | ||||
| Age categories | ||||||
| Adults | 21 (46.7) | 24 (53.3) | <0.001 b | 13 | 09–16 | <0.001 c |
| Adolescents | 2 (4.9) | 39 (95.1) | 08 | 06–11 | ||
| Race/color d | ||||||
| White | 6 (20.7) | 23 (79.3) | 0.432 b | 10 | 08–13 | 0.524 c |
| Brown/Black | 16 (28.6) | 40 (71.4) | 11 | 08–16 | ||
| Self-perceived school performance compared to peers | ||||||
| Better than average | 17 (43.6) | 22 (56.4) | 0.001 b | 13 | 09–16 | <0.001 c |
| Average/worse | 6 (12.8) | 41 (87.2) | 09 | 06–12 | ||
| Income sufficiency | ||||||
| Very well | 3 (15.8) | 16 (84.2) | 0.084 b | 09 | 06–11 | 0.023 e |
| Suitable | 19 (34.5) | 36 (65.5) | 12 | 08–16 | ||
| Not well | 1 (8.3) | 11 (91.7) | 08 | 07–12 | ||
| Receiving “Bolsa Familia” d | ||||||
| Yes | 10 (17.9) | 46 (82.1) | 0.008 b | 10 | 07–13 | 0.009 c |
| No | 13 (44.8) | 16 (55.2) | 14 | 08–17 | ||
| Number of prenatal consultations d | ||||||
| ≥6 | 7 (21.2) | 26 (78.8) | 0.334 b | 11 | 8–13 | 0.993 c |
| <6 | 16 (30.8) | 36 (69.2) | 10 | 7–16 | ||
| Social Support | ||||||
| Friends | ||||||
| High | 17 (31.5) | 37 (68.5) | 0.197 b | 12 | 08–16 | 0.200 c |
| Low/none | 6 (18.8) | 26 (81.3) | 09 | 07–14 | ||
| Grandparents | ||||||
| High | 13 (22.8) | 44 (77.2) | 0.247 b | 10 | 08–13 | 0.453 c |
| Low/none | 10 (34.5) | 19 (65.5) | 12 | 07–16 | ||
| Parents | ||||||
| High | 21 (33.9) | 41 (66.1) | 0.016 b | 12 | 08–16 | 0.052 c |
| Low/none | 2 (8.3) | 22 (91.7) | 09 | 07–11 | ||
| Partner | ||||||
| High | 14 (23.7) | 45 (76.3) | 0.350 b | 10 | 07–14 | 0.265 c |
| Low/none | 9 (33.3) | 18 (66.7) | 11 | 08–15 | ||
| Siblings | ||||||
| High | 18 (29.5) | 43 (70.5) | 0.366 b | 11 | 08–15 | 0.399 c |
| Low/none | 5 (20.0) | 20 (80.0) | 09 | 07–13 | ||
| Total | 23 (26.7) | 63 (73.3) | 10.5 | 7.8–15.0 | ||
| Variables | β | 95%CI a | p Value |
|---|---|---|---|
| Age categories | |||
| Adolescents | −3.484 | −5.006 to −1.962 | <0.001 |
| Adults | 0 | ||
| Self-perceived school performance compared to peers | |||
| Better than average | 2.843 | 1.312 to 4.375 | <0.001 |
| Average/worse | 0 | ||
| Income sufficiency | |||
| Very well | 0.498 | −2.137 to 3.132 | 0.708 |
| Suitable | 2.775 | 0.568 to 4.983 | 0.014 |
| Not well | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
França, A.S.; Pirkle, C.M.; Sentell, T.; Velez, M.P.; Domingues, M.R.; Bassani, D.G.; Câmara, S.M.A. Evaluating Health Literacy among Adolescent and Young Adult Pregnant Women from a Low-Income Area of Northeast Brazil. Int. J. Environ. Res. Public Health 2020, 17, 8806. https://doi.org/10.3390/ijerph17238806
França AS, Pirkle CM, Sentell T, Velez MP, Domingues MR, Bassani DG, Câmara SMA. Evaluating Health Literacy among Adolescent and Young Adult Pregnant Women from a Low-Income Area of Northeast Brazil. International Journal of Environmental Research and Public Health. 2020; 17(23):8806. https://doi.org/10.3390/ijerph17238806
Chicago/Turabian StyleFrança, Allen Suzane, Catherine M. Pirkle, Tetine Sentell, Maria P. Velez, Marlos R. Domingues, Diego G. Bassani, and Saionara M. A. Câmara. 2020. "Evaluating Health Literacy among Adolescent and Young Adult Pregnant Women from a Low-Income Area of Northeast Brazil" International Journal of Environmental Research and Public Health 17, no. 23: 8806. https://doi.org/10.3390/ijerph17238806
APA StyleFrança, A. S., Pirkle, C. M., Sentell, T., Velez, M. P., Domingues, M. R., Bassani, D. G., & Câmara, S. M. A. (2020). Evaluating Health Literacy among Adolescent and Young Adult Pregnant Women from a Low-Income Area of Northeast Brazil. International Journal of Environmental Research and Public Health, 17(23), 8806. https://doi.org/10.3390/ijerph17238806





