Examining the Associations between Psychological Flexibility, Mindfulness, Psychosomatic Functioning, and Anxiety during the COVID-19 Pandemic: A Path Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Psychological Measures
2.3. Procedure
3. Results
3.1. Correlations between Personal Resources and Indicators of Psychosomatic Functioning during the COVID-19 Pandemic
3.2. Stepwise Regression for Psychosomatic Functioning
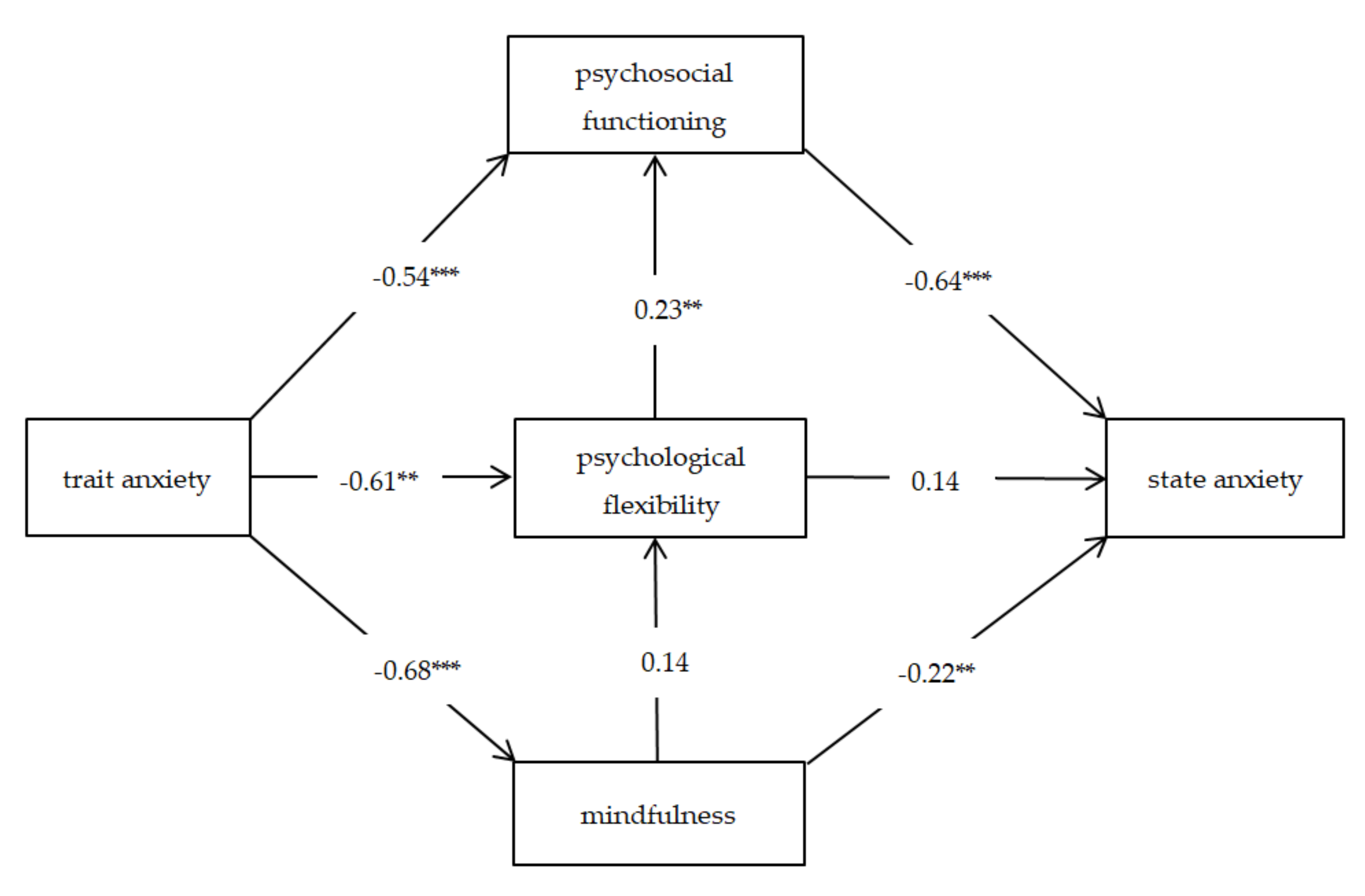
3.3. A Path Model for Pandemic Anxiety
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
References
- Lai, C.-C.; Shih, T.-P.; Ko, W.-C.; Tang, H.-J.; Hsueh, P.-R. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Corona Virus Disease-2019 (COVID-19): The Epidemic and the Challenges. Int. J. Antimicrob. Agents 2020, 55, 105924. [Google Scholar] [CrossRef] [PubMed]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R. A Novel Coronavirus from Patients with Pneumonia in China, 2019. New Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- John Hopkins University. COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). Available online: https://coronavirus.jhu.edu/map.html (accessed on 16 July 2020).
- Cascella, M.; Rajnik, M.; Cuomo, A.; Dulebohn, S.C.; Di Napoli, R. Features, Evaluation and Treatment Coronavirus (COVID-19). In Statpearls; StatPearls Publishing: Treasure Island, FL, USA, 2020. [Google Scholar]
- Sanders, J.M.; Monogue, M.L.; Jodlowski, T.Z.; Cutrell, J.B. Pharmacologic Treatments for Coronavirus Disease 2019 (COVID-19): A Review. Jama 2020, 323, 1824–1836. [Google Scholar] [CrossRef] [PubMed]
- Shang, W.; Yang, Y.; Rao, Y.; Rao, X. The Outbreak of SARS-CoV-2 Pneumonia Calls for Viral Vaccines. NPJ Vaccines 2020, 5, 18. [Google Scholar] [CrossRef]
- Young, L.-S.; Ruschel, S.; Yanchuk, S.; Pereira, T. Consequences of Delays and Imperfect Implementation of Isolation in Epidemic Control. Sci. Rep. 2019, 9, 3505. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19) Advice for the Public. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed on 24 June 2020).
- Hawryluck, L.; Gold, W.L.; Robinson, S.; Pogorski, S.; Galea, S.; Styra, R. SARS Control and Psychological Effects of Quarantine, Toronto, Canada. Emerg. Infect. Dis. 2004, 10, 1206–1212. [Google Scholar] [CrossRef]
- Jeong, H.; Yim, H.W.; Song, Y.-J.; Ki, M.; Min, J.-A.; Cho, J.; Chae, J.-H. Mental Health Status of People Isolated Due to Middle East Respiratory Syndrome. Epidemiol Health 2016, 38, e2016048. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The Psychological Impact of Quarantine and How to Reduce It: Rapid Review of the Evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Leigh-Hunt, N.; Bagguley, D.; Bash, K.; Turner, V.; Turnbull, S.; Valtorta, N.; Caan, W. An Overview of Systematic Reviews on the Public Health Consequences of Social Isolation and Loneliness. Public Health 2017, 152, 157–171. [Google Scholar] [CrossRef]
- Xyrichis, A.; Hext, G.; Clark, L.L. Beyond Restraint: Raising Awareness of Restrictive Practices in Acute Care Settings. Int. J. Nurs. Stud. 2018, 86, A1–A2. [Google Scholar] [CrossRef]
- Tasnim, S.; Hossain, M.M.; Mazumder, H. Impact of Rumors and Misinformation on COVID-19 in Social Media. J. Prev. Med. Public Health 2020, 53, 171–174. [Google Scholar] [CrossRef] [PubMed]
- Anwar, A.; Malik, M.; Raees, V.; Anwar, A. Role of Mass Media and Public Health Communications in the COVID-19 Pandemic. Cureus 2020, 12, e10453. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.; Hu, Z.; Alias, H.; Wong, L.P. Influence of Mass and Social Media on Psychobehavioral Responses Among Medical Students During the Downward Trend of COVID-19 in Fujian, China: Cross-Sectional Study. J. Med. Internet Res. 2020, 22, e19982. [Google Scholar] [CrossRef] [PubMed]
- Ayed, N.; Toner, S.; Priebe, S. Conceptualizing Resilience in Adult Mental Health Literature: A Systematic Review and Narrative Synthesis. Psychol. Psychother. Theory Res. Pract. 2019, 92, 299–341. [Google Scholar] [CrossRef] [PubMed]
- Kashdan, T.B.; Rottenberg, J. Psychological Flexibility as a Fundamental Aspect of Health. Clin. Psychol. Rev. 2010, 30, 865–878. [Google Scholar] [CrossRef]
- Bond, F.W.; Hayes, S.C.; Baer, R.A.; Carpenter, K.M.; Guenole, N.; Orcutt, H.K.; Waltz, T.; Zettle, R.D. Preliminary Psychometric Properties of the Acceptance and Action Questionnaire-II: A Revised Measure of Psychological Inflexibility and Experiential Avoidance. Behav. Ther. 2011, 42, 676–688. [Google Scholar] [CrossRef]
- Hayes, S.C.; Luoma, J.B.; Bond, F.W.; Masuda, A.; Lillis, J. Acceptance and Commitment Therapy: Model, Processes and Outcomes. Behav. Res. Ther. 2006, 44, 1–25. [Google Scholar] [CrossRef]
- Powers, M.B.; Vörding, M.B.Z.V.S.; Emmelkamp, P.M.G. Acceptance and Commitment Therapy: A Meta-Analytic Review. Psychother. Psychosom. 2009, 78, 73–80. [Google Scholar] [CrossRef]
- Corrigan, F.M. Psychotherapy as Assisted Homeostasis: Activation of Emotional Processing Mediated by the Anterior Cingulate Cortex. Med. Hypotheses 2004, 63, 968–973. [Google Scholar] [CrossRef]
- Wielgosz, J.; Goldberg, S.B.; Kral, T.R.A.; Dunne, J.D.; Davidson, R.J. Mindfulness Meditation and Psychopathology. Annu. Rev. Clin. Psychol. 2019, 15, 285–316. [Google Scholar] [CrossRef]
- Kabat-Zinn, J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness; Random House Publishing Group: New York, NY, USA, 2013. [Google Scholar]
- Segal, Z.V.; Williams, J.M.G.; Teasdale, J.D. Mindfulness-Based Cognitive Therapy for Depression, 2nd ed.; The Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Borquist-Conlon, D.S.; Maynard, B.R.; Brendel, K.E.; Farina, A.S. Mindfulness-Based Interventions for Youth with Anxiety: A Systematic Review and Meta-Analysis. Res. Soc. Work Pract. 2019, 29, 195–205. [Google Scholar] [CrossRef]
- Hofmann, S.G.; Sawyer, A.T.; Witt, A.A.; Oh, D. The Effect of Mindfulness-Based Therapy on Anxiety and Depression: A Meta-Analytic Review. J. Consult. Clinical Psychol. 2010, 78, 169–183. [Google Scholar] [CrossRef] [PubMed]
- Lv, J.; Liu, Q.; Zeng, X.; Oei, T.P.; Liu, Y.; Xu, K.; Sun, W.; Hou, H.; Liu, J. The Effect of Four Immeasurables Meditations on Depressive Symptoms: A Systematic Review and Meta-Analysis. Clin. Psychol. Rev. 2020, 76, 101814. [Google Scholar] [CrossRef] [PubMed]
- McCarney, R.W.; Schulz, J.; Grey, A.R. Effectiveness of Mindfulness-Based Therapies in Reducing Symptoms of Depression: A Meta-Analysis. Eur. J. Psychother. Couns. 2012, 14, 279–299. [Google Scholar] [CrossRef]
- Aktas, S.; Gulen, M.; Sevi, O.M. Mindfulness Therapies for Medically Unexplained Somatic Symptoms: A Systematic Review/Tibben Aciklanamayan Somatik Semptomlar Icin Bilincli Farkindalik Temelli Terapiler: Sistematik Bir Gozden Gecirme. Psikiyatr. Guncel Yaklasimlar Curr. Approaches Psychiatry 2019, 11, 271–284. [Google Scholar] [CrossRef]
- Scott-Sheldon, L.A.; Gathright, E.C.; Donahue, M.L.; Balletto, B.; Feulner, M.M.; DeCosta, J.; Cruess, D.G.; Wing, R.R.; Carey, M.P.; Salmoirago-Blotcher, E. Mindfulness-Based Interventions for Adults with Cardiovascular Disease: A Systematic Review and Meta-Analysis. Ann. Behav. Med. 2020, 54, 67–73. [Google Scholar] [CrossRef]
- Xunlin, N.G.; Lau, Y.; Klainin-Yobas, P. The Effectiveness of Mindfulness-Based Interventions among Cancer Patients and Survivors: A Systematic Review and Meta-Analysis. Support. Care Cancer 2019, 28, 1563–1578. [Google Scholar] [CrossRef]
- Gál, É.; Ștefan, S.; Cristea, I.A. The Efficacy of Mindfulness Meditation Apps in Enhancing Users’ Well-Being and Mental Health Related Outcomes: A Meta-Analysis of Randomized Controlled Trials. J. Affect. Disord. 2020. [Google Scholar] [CrossRef]
- Spijkerman, M.P.J.; Pots, W.T.M.; Bohlmeijer, E.T. Effectiveness of Online Mindfulness-Based Interventions in Improving Mental Health: A Review and Meta-Analysis of Randomised Controlled Trials. Clin. Psychol. Rev. 2016, 45, 102–114. [Google Scholar] [CrossRef]
- Khoury, B.; Sharma, M.; Rush, S.E.; Fournier, C. Mindfulness-Based Stress Reduction for Healthy Individuals: A Meta-Analysis. J. Psychosom. Res. 2015, 78, 519–528. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.E. STAI: Manual for the State–TraitAnxiety Inventory (STAI); Consulting Psychologists Pres: Palo Alto, CA, USA, 1970. [Google Scholar]
- Abel, B. Trait and State Anxiety: Assessment, Predictors and Outcomes; Nova Science Nova Science Publishers Inc.: New York, NY, USA, 2016. [Google Scholar]
- Wrześniewski, K.; Matusik, D.; Sosnowski, T. The State-Trait Anxiety Inventory; The Polish Adaptation of STAI: Warsaw, Poland, 2002. [Google Scholar]
- Kleszcz, B.; Dudek, J.E.; Bialaszek, W.; Ostaszewski, P.; Bond, F.W. The Psychometric Properties of the Polish Version of the Acceptance and Action Questionnaire-II (AAQ-II). Psychol. Stud. 2018, 56, 1–20. [Google Scholar] [CrossRef]
- Walach, H.; Buchheld, N.; Buttenmüller, V.; Kleinknecht, N.; Schmidt, S. Measuring Mindfulness—The Freiburg Mindfulness Inventory (FMI). Pers. Individ. Differ. 2006, 40, 1543–1555. [Google Scholar] [CrossRef]
- Bishop, S.R.; Lau, M.; Shapiro, S.; Carlson, L.; Anderson, N.D.; Carmody, J.; Segal, Z.V.; Abbey, S.; Speca, M.; Velting, D.; et al. Mindfulness: A Proposed Operational Definition. Clin. Psychol. Sci. Prac. 2004, 11, 230–241. [Google Scholar] [CrossRef]
- Radoń, S. Polish Adpatation and Validation of the Freiburg Mindfulness Inventory. Studia Psychol. Theor. Et Prax. 2017, 17, 85–100. [Google Scholar]
- Styła, R.; Kowalski, J. Psychometric Properties of the General Functioning Questionnaire (GFQ-58) Used for Screening for Symptoms of Psychopathologyand Overall Level of Functioning. Psychiatr. Polska 2020, 54, 83–100. [Google Scholar] [CrossRef] [PubMed]
- Balkhi, F.; Nasir, A.; Zehra, A.; Riaz, R. Psychological and Behavioral Response to the Coronavirus (COVID-19) Pandemic. Cureus 2020, 12, e7923. [Google Scholar] [CrossRef]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The Outbreak of COVID-19 Coronavirus and Its Impact on Global Mental Health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- González-Sanguino, C.; Ausín, B.; ÁngelCastellanos, M.; Saiz, J.; López-Gómez, A.; Ugidos, C.; Muñoz, M. Mental Health Consequences during the Initial Stage of the 2020 Coronavirus Pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020, 87, 172–176. [Google Scholar] [CrossRef]
- Newby, J.; O’Moore, K.; Tang, S.; Christensen, H.; Faasse, K. Acute Mental Health Responses during the COVID-19 Pandemic in Australia. medRxiv 2020, 15, e0236562. [Google Scholar] [CrossRef]
- Fonseca, S.; Trindade, I.A.; Mendes, A.L.; Ferreira, C. The Buffer Role of Psychological Flexibility against the Impact of Major Life Events on Depression Symptoms. Clin. Psychol. 2020, 24, 82–90. [Google Scholar] [CrossRef]
- Dawson, D.L.; Golijani-Moghaddam, N. COVID-19: Psychological Flexibility, Coping, Mental Health, and Wellbeing in the UK during the Pandemic. J. Context. Behav. Sci. 2020, 17, 126–134. [Google Scholar] [CrossRef] [PubMed]
- Pakenham, K.I.; Landi, G.; Boccolini, G.; Furlani, A.; Grandi, S.; Tossani, E. The Moderating Roles of Psychological Flexibility and Inflexibility on the Mental Health Impacts of COVID-19 Pandemic and Lockdown in Italy. J. Contextual Behav. Sci. 2020, 17, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Davidson, R.J. Empirical Explorations of Mindfulness: Conceptual and Methodological Conundrums. Emotion 2010, 10, 8–11. [Google Scholar] [CrossRef] [PubMed]
- Baer, R.A.; Lykins, E.L.; Peters, J.R. Mindfulness and Self-Compassion as Predictors of Psychological Wellbeing in Long-Term Meditators and Matched Nonmeditators. J. Posit. Psychol. 2012, 7, 230–238. [Google Scholar] [CrossRef]
- Spencer, N. Confirming Experience: Being Present during Reflective Conversations. Des. Princ. Pract. Ann. Int. J. 2010, 4. [Google Scholar] [CrossRef]
- Wang, Y.-Y.; Wang, F.; Zheng, W.; Zhang, L.; Ng, C.H.; Ungvari, G.S.; Xiang, Y.-T. Mindfulness-Based Interventions for Insomnia: A Meta-Analysis of Randomized Controlled Trials. Behav. Sleep Med. 2020, 18, 1–9. [Google Scholar] [CrossRef]
- Demarzo, M.M.; Montero-Marin, J.; Cuijpers, P.; Zabaleta-del-Olmo, E.; Mahtani, K.R.; Vellinga, A.; Vicens, C.; López-del-Hoyo, Y.; García-Campayo, J. The Efficacy of Mindfulness-Based Interventions in Primary Care: A Meta-Analytic Review. Ann. Fam. Med. 2015, 13, 573–582. [Google Scholar] [CrossRef]
- Manzoni, G.M.; Pagnini, F.; Castelnuovo, G.; Molinari, E. Relaxation Training for Anxiety: A Ten-Years Systematic Review with Meta-Analysis. BMC Psychiatry 2008, 8, 41. [Google Scholar] [CrossRef]
- Stetter, F.; Kupper, S. Autogenic Training: A Meta-Analysis of Clinical Outcome Studies. Appl. Psychophysiol. Biofeedback 2002, 27, 45–98. [Google Scholar] [CrossRef]
- Matiz, A.; Fabbro, F.; Paschetto, A.; Cantone, D.; Paolone, A.R.; Crescentini, C. Positive Impact of Mindfulness Meditation on Mental Health of Female Teachers during the COVID-19 Outbreak in Italy. Int. J. Environ. Res. Public Health 2020, 17, 6450. [Google Scholar] [CrossRef] [PubMed]
- Behan, C. The Benefits of Meditation and Mindfulness Practices during Times of Crisis Such as COVID-19. Ir. J. Psychol. Med. 2020, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Conversano, C.; Di Giuseppe, M.; Miccoli, M.; Ciacchini, R.; Gemignani, A.; Orrù, G. Mindfulness, Age and Gender as Protective Factors Against Psychological Distress During COVID-19 Pandemic. Front. Psychol. 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Coping and Stress. Available online: https://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/managing-stress-anxiety.html (accessed on 14 July 2020).
- Kroska, E.B.; Roche, A.I.; Adamowicz, J.L.; Stegall, M.S. Psychological Flexibility in the Context of COVID-19 Adversity: Associations with Distress. J. Contextual Behav. Sci. 2020, 18, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Boekel, W.; Hsieh, S. Cross-Sectional White Matter Microstructure Differences in Age and Trait Mindfulness. PLoS ONE 2018, 13, e0205718. [Google Scholar] [CrossRef]
- Wuhan City Health Committee. Wuhan Municipal Health and Health Commission’s briefing on the Current Pneumonia Epidemic Situation in Our City. 2019. Available online: http://wjw.wuhan.gov.cn/front/web/showDetail/2019123108989 (accessed on 14 March 2020).
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19–11 March 2020. Available online: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (accessed on 14 March 2020).
| Demographic Characteristics | N | M | SD | Range | % |
|---|---|---|---|---|---|
| Age | 27.79 | 8.157 | 18–59 | ||
| Gender | |||||
| Men | 45 | 26.47 | |||
| Women | 125 | 73.53 | |||
| Education | |||||
| Primary | 8 | 4.71 | |||
| Secondary | 38 | 22.35 | |||
| Postsecondary | 21 | 12.35 | |||
| Higher | 103 | 60.59 | |||
| Marital status | |||||
| Single | 136 | 80.00 | |||
| Married | 32 | 18.80 | |||
| Divorced | 1 | 0.60 | |||
| Widow/widower | 1 | 0.60 | |||
| Place of residence | |||||
| Village | 24 | 27.90 | |||
| Small town (less than 50 k) | 29 | 72.10 | |||
| Medium-sized town (from 50 to 150 k) | 13 | 7.65 | |||
| Big city (more than 150 k) | 104 | 6.12 |
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | M | SD |
|---|---|---|---|---|---|---|---|---|
| 1. State anxiety | - | 2.36 | 2.359 | |||||
| 2. Trait anxiety | 0.549 *** | - | 2.23 | 2.229 | ||||
| 3. Psychosomatic Functioning | −0.659 *** | −0.704 *** | - | 3.93 | 3.926 | |||
| 4. Psychological Flexibility | −0.370 *** | −0.705 *** | 0.613 *** | - | 4.52 | 4.519 | ||
| 5. Mindfulness | −0.458 *** | −0.681 *** | 0.502 *** | 0.553 *** | - | 2.47 | 2.473 | |
| 6. Somatic response to pandemic | 0.430 *** | 0.392 *** | −0.505 *** | −0.350 *** | −0.244 *** | - | 0.17 | 0.270 |
| 7. Psychological response to pandemic | 0.678 *** | 0.431 *** | −0.597 *** | −0.300 *** | −0.348 *** | 0.578 *** | 0.23 | 0.244 |
| Model 1 | F (3169) | R | R2sk | Predictors | Semipartial Correlation | % of Variance | p |
|---|---|---|---|---|---|---|---|
| General psychosomatic functioning | 60.57 | 0.72 | 0.51 | Anxiety trait | −0.329 | 10.8 | <0.001 |
| Psychological flexibility | 0.162 | 2.6 | 0.003 | ||||
| Mindfulness | 0.008 | - | 0.881 |
| Model 2 | F (3169) | R | R2sk | Predictors | Semipartial Correlation | % of Variance | p |
|---|---|---|---|---|---|---|---|
| Anxiety state | 128.65 | 0.66 | 0.43 | Psychosomatic Functioning | −0.659 | 43.4 | <0.001 |
| Path | Standardization Coefficient | SE | t | p | 95% CI (Lower, Upper) | ||
|---|---|---|---|---|---|---|---|
| Psychosomatic functioning | → | State anxiety | −0.636 | 0.075 | −8.698 | <0.001 | −0.652, −0.636 |
| Psychological flexibility | → | State anxiety | 0.139 | 0.026 | 1.826 | 0.068 | 0.048, 0.139 |
| Mindfulness | → | State anxiety | −0.216 | 0.074 | −3.115 | 0.002 | −0.231, 0.216 |
| Psychological flexibility | → | Psychosomatic functioning | 0.232 | 0.025 | 3.103 | 0.002 | 0.077, 0.232 |
| Trait anxiety | → | Psychosomatic functioning | −0.540 | 0.089 | −7.225 | <0.001 | −0.647, −0.540 |
| Mindfulness | → | Psychological flexibility | 0.136 | 0.229 | 1.848 | 0.065 | 0.424, 0.136 |
| Trait anxiety | → | Psychological flexibility | −0.613 | 0.263 | −8.345 | <0.001 | −2.199, −0.613 |
| Trait anxiety | → | Mindfulness | −0.681 | 0.065 | −12.112 | <0.001 | −0.781, −0.681 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wielgus, B.; Urban, W.; Patriak, A.; Cichocki, Ł. Examining the Associations between Psychological Flexibility, Mindfulness, Psychosomatic Functioning, and Anxiety during the COVID-19 Pandemic: A Path Analysis. Int. J. Environ. Res. Public Health 2020, 17, 8764. https://doi.org/10.3390/ijerph17238764
Wielgus B, Urban W, Patriak A, Cichocki Ł. Examining the Associations between Psychological Flexibility, Mindfulness, Psychosomatic Functioning, and Anxiety during the COVID-19 Pandemic: A Path Analysis. International Journal of Environmental Research and Public Health. 2020; 17(23):8764. https://doi.org/10.3390/ijerph17238764
Chicago/Turabian StyleWielgus, Benita, Witold Urban, Aleksandra Patriak, and Łukasz Cichocki. 2020. "Examining the Associations between Psychological Flexibility, Mindfulness, Psychosomatic Functioning, and Anxiety during the COVID-19 Pandemic: A Path Analysis" International Journal of Environmental Research and Public Health 17, no. 23: 8764. https://doi.org/10.3390/ijerph17238764
APA StyleWielgus, B., Urban, W., Patriak, A., & Cichocki, Ł. (2020). Examining the Associations between Psychological Flexibility, Mindfulness, Psychosomatic Functioning, and Anxiety during the COVID-19 Pandemic: A Path Analysis. International Journal of Environmental Research and Public Health, 17(23), 8764. https://doi.org/10.3390/ijerph17238764





