Estimates of Cancer Mortality Attributable to Carcinogenic Infections in Italy
Abstract
1. Introduction
2. Materials and Methods
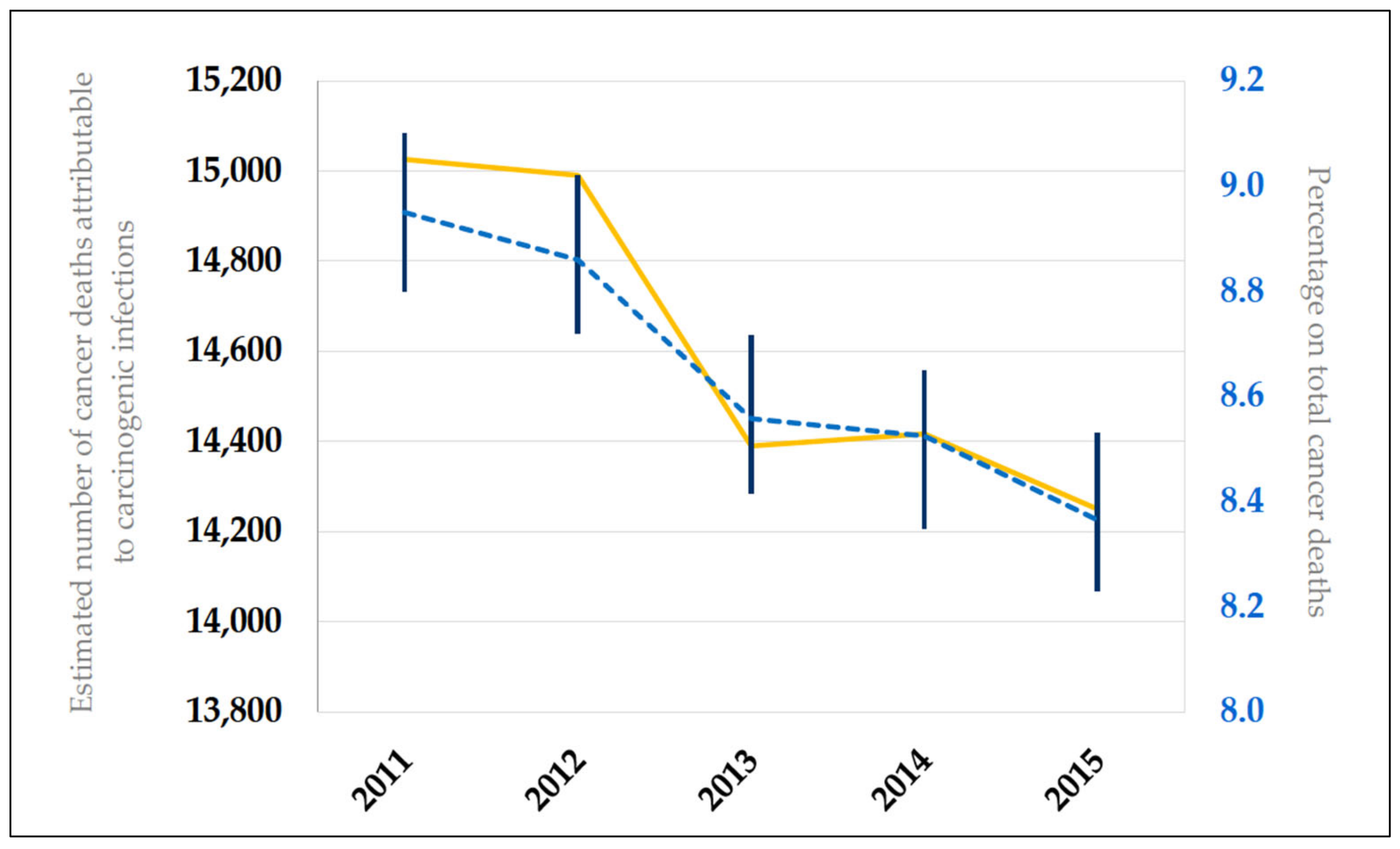
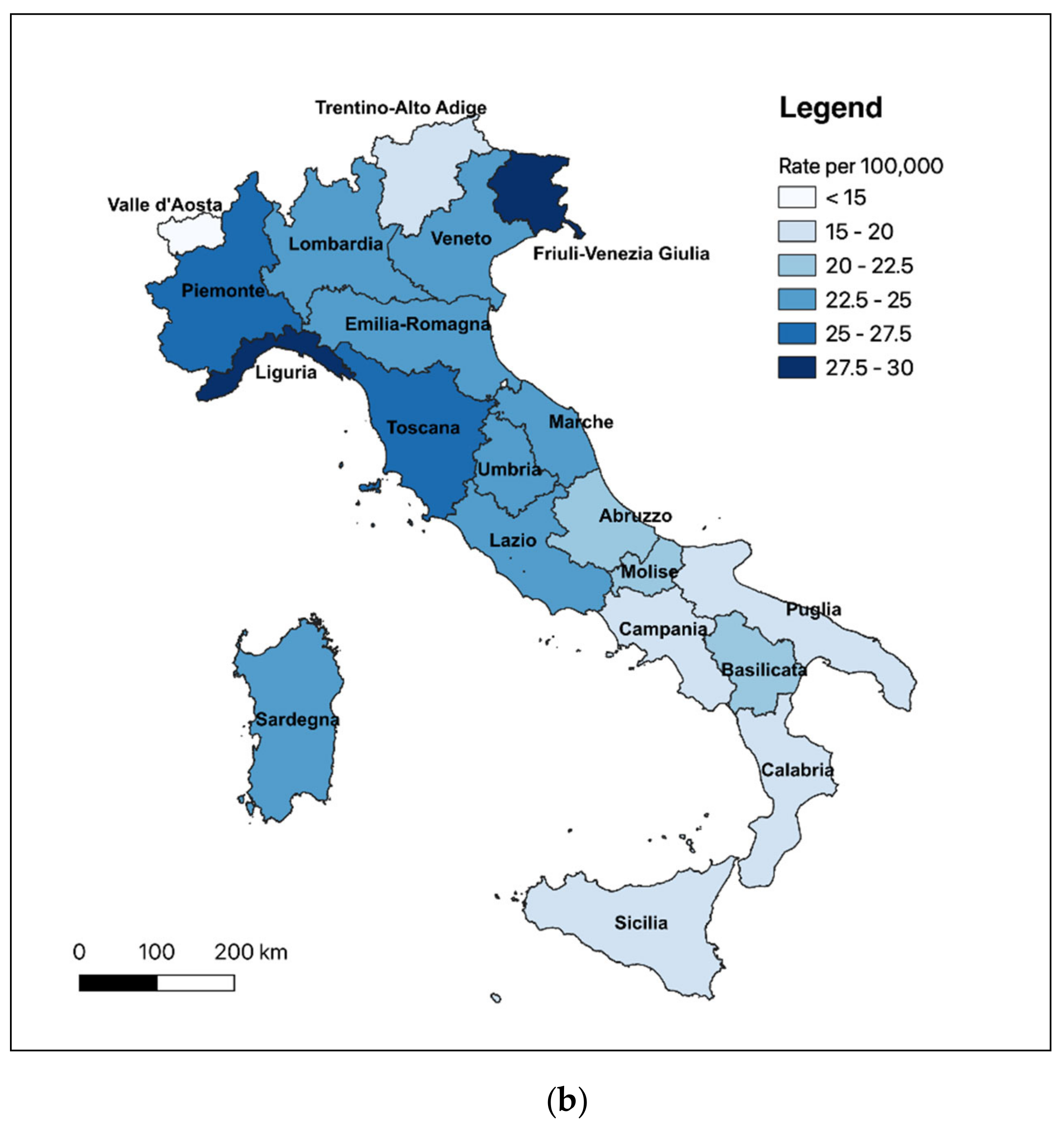
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Disclaimer
References
- Global Burden of Disease Cancer Collaboration. Global, regional, and national cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life-years for 29 cancer groups, 1990 to 2017: A systematic analysis for the global burden of disease study. JAMA Oncol. 2019, 5, 1749–1768. [Google Scholar] [CrossRef] [PubMed]
- de Martel, C.; Georges, D.; Bray, F.; Ferlay, J.; Clifford, G. Global burden of cancer attributable to infections in 2018: A worldwide incidence analysis. Lancet Glob. Health 2020, 8, e180–e190. [Google Scholar] [CrossRef]
- Rositch, A.F. Global burden of cancer attributable to infections: The critical role of implementation science. Lancet Glob. Health 2020, 8, e153–e154. [Google Scholar] [CrossRef]
- Ferrara, P.; Agüero, F.; Masuet-Aumatell, C.; Ramon-Torrell, J.M. Burden of cancer mortality attributable to carcinogenic infections in Spain. Med. Clin. 2020, 154, 394–397. [Google Scholar] [CrossRef]
- De Flora, S.; La Maestra, S.; Crocetti, E.; Mangone, L.; Bianconi, F.; Stracci, F.; Buzzoni, C. Estimates of the incidence of infection-related cancers in Italy and Italian regions in 2018. J. Prev. Med. Hyg. 2019, 60, E311–E326. [Google Scholar]
- Ferrara, P.; Agüero, F.; Conti, S.; Masuet-Aumatell, C.; Mantovani, L.; Ramon-Torrell, J.M. An exploration of cancer-related mortality attributable to infections in Italy. Eur. J. Public Health 2020, 30, ckaa1651262. [Google Scholar] [CrossRef]
- Associazione Italiana di Oncologia Medica. I Numeri del Cancro in Italia 2019. Available online: https://www.aiom.it/wp-content/uploads/2019/09/2019_Numeri_Cancro-operatori-web.pdf (accessed on 9 October 2020).
- International Agency for Research on Cancer (IARC). Cancers Attributable to Infections. Available online: gco.iarc.fr/causes/infections/home (accessed on 9 October 2020).
- Hernandez, J.B.R.; Kim, P.Y. Epidemiology Morbidity and Mortality. Available online: https://www.ncbi.nlm.nih.gov/books/NBK547668/ (accessed on 17 November 2020).
- Plummer, M.; de Martel, C.; Vignat, J.; Ferlay, J.; Bray, F.; Franceschi, S. Global burden of cancers attributable to infections in 2012: A synthetic analysis. Lancet Glob. Health 2016, 4, e609–e612. [Google Scholar] [CrossRef]
- Bucci, L.; Garuti, F.; Lenzi, B.; Pecorelli, A.; Farinati, F.; Giannini, E.G.; Granito, A.; Ciccarese, F.; Rapaccini, G.L.; Di Marco, M.; et al. The evolutionary scenario of hepatocellular carcinoma in Italy: An update. Liver Int. 2017, 37, 259–270. [Google Scholar] [CrossRef]
- Parkin, D.M. The global health burden of infection-associated cancers in the year 2002. Int J. Cancer 2006, 118, 3030–3044. [Google Scholar] [CrossRef] [PubMed]
- Istituto Nazionale di Statistica (ISTAT). I. Stat—Popolazione Residente al 1° Gennaio. Available online: http://dati.istat.it/# (accessed on 1 October 2020).
- World Health Organization (WHO). CoDQL—Cause of Death Query Online. Available online: https://apps.who.int/healthinfo/statistics/mortality/causeofdeath_query/ (accessed on 27 September 2020).
- Associazione Italiana di Oncologia Medica. I numeri del cancro in Italia 2018. Available online: https://www.aiom.it/wp-content/uploads/2018/10/2018_NumeriCancro-operatori.pdf (accessed on 1 October 2020).
- International Agency for Research on Cancer (IARC). Cancer Registration: Principles and Methods; IARC Scientific Publications: Lyon, France, 1991. [Google Scholar]
- R Foundation for Statistical Computing. Available online: www.R-project.org (accessed on 24 November 2020).
- QGIS Development Team (YEAR). QGIS Geographic Information System. Open Source Geospatial Foundation Project. Available online: https://www.osgeo.org/projects/qgis/ (accessed on 24 November 2020).
- Marcus, E.A.; Sachs, G.; Scott, D.R. Eradication of Helicobacter pylori infection. Curr. Gastroenterol. Rep. 2016, 18, 33. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.C.; Lin, J.T. Screening and treating Helicobacter pylori infection for gastric cancer prevention on the population level. J. Gastroenterol. Hepatol. 2017, 32, 1160–1169. [Google Scholar] [CrossRef]
- Dore, M.P.; Marras, G.; Rocchi, C.; Soro, S.; Loria, M.F.; Bassotti, G.; Graham, D.Y.; Malaty, H.M.; Pes, G.M. Changing prevalence of Helicobacter pylori infection and peptic ulcer among dyspeptic Sardinian patients. Intern. Emerg. Med. 2015, 10, 787–794. [Google Scholar] [CrossRef]
- Hooi, J.K.Y.; Lai, W.Y.; Ng, W.K.; Suen, M.M.Y.; Underwood, F.E.; Tanyingoh, D.; Malfertheiner, P.; Graham, D.Y.; Wong, V.W.S.; Wu, J.C.Y.; et al. Global Prevalence of Helicobacter pylori Infection: Systematic Review and Meta-Analysis. Gastroenterology 2017, 153, 420–429. [Google Scholar] [CrossRef] [PubMed]
- Gardini, I.; Bartoli, M.; Conforti, M.; Mennini, F.S.; Marcellusi, A. Estimation of the number of HCV-positive patients in Italy. PLoS ONE 2019, 14, e0223668. [Google Scholar] [CrossRef] [PubMed]
- Buonomo, A.R.; Scotto, R.; Coppola, C.; Pinchera, B.; Viceconte, G.; Rapillo, C.M.; Staiano, L.; Saturnino, M.; Scarano, F.; Portunato, F.; et al. Direct acting antivirals treatment for hepatitis C virus infection does not increase the incidence of de novo hepatocellular carcinoma occurrence: Results from an Italian real-life cohort (LINA cohort). Medicine 2020, 99, e18948. [Google Scholar] [CrossRef] [PubMed]
- Lozano, R.; Fullman, N.; Mumford, J.E.; Knight, M.; Barthelemy, C.M.; Abbafati, C.; Abbastabar, H.; Abd-Allah, F.; Abdollahi, M.; Abedi, A.; et al. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1250–1284. [Google Scholar] [CrossRef]
- Istituto Superiore di Sanità. Epidemiology of acute viral hepatitis in Italy: Results of the surveillance. Rapp. ISTISAN 2012, 12, 24. [Google Scholar]
- Peirson, L.; Fitzpatrick-Lewis, D.; Ciliska, D.; Warren, R. Screening for cervical cancer: A systematic review and meta-analysis. Syst Rev. 2013, 2, 35. [Google Scholar] [CrossRef]
- Drolet, M.; Bénard, E.; Boily, M.-C.; Ali, H.; Baandrup, L.; Bauer, H.M.; Beddows, S.; Brisson, J.; Brotherton, J.M.L.; Cummings, T.; et al. Population-level impact and herd effects following human papillomavirus vaccination programmes: A systematic review and meta-analysis. Lancet 2015, 15, 565–580. [Google Scholar] [CrossRef]
- Colamesta, V.; Grossi, A.; Barbara, A. Human Papilloma Virus (HPV) vaccination in Italy: Towards new perspectives and new challenges. Epidemiol. Biostat. Public Health 2018, 15. [Google Scholar] [CrossRef]
- Polesel, J.; Franceschi, S.; Talamini, R.; Negri, E.; Barzan, L.; Montella, M.; Libra, M.; Vaccher, E.; Franchin, G.; La Vecchia, C.; et al. Tobacco smoking, alcohol drinking, and the risk of different histological types of nasopharyngeal cancer in a low-risk population. Oral Oncol. 2011, 47, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Mesri, E.A.; Cesarman, E.; Boshoff, C. Kaposi’s sarcoma herpesvirus/Human herpesvirus-8 (KSHV/HHV8), and the oncogenesis of Kaposi’s sarcoma. Nat. Rev. Cancer 2010, 10, 707–719. [Google Scholar] [CrossRef] [PubMed]
- Cattani, P.; Capuano, M.; La Parola, I.L.; Guido, R.; Santangelo, R.; Cerimele, F.; Masini, C.; Nanni, G.; Fadda, G.; Cerimele, D. Human herpesvirus 8 in Italian HIV-Seronegative Patients with Kaposi Sarcoma. Arch. Dermatol. 1998, 134, 695–699. [Google Scholar] [CrossRef] [PubMed]
- Fondazione AIRC. Guida ai Tumori. Sarcoma di Kaposi. Available online: https://www.airc.it/cancro/informazioni-tumori/guida-ai-tumori/sarcoma-di-kaposi (accessed on 11 October 2020).
- Alessio, L.; Minichini, C.; Starace, M. Low prevalence of HTLV1/2 infection in a population of immigrants living in southern Italy. PLoS Negl. Trop. Dis. 2018, 12, e0006601. [Google Scholar] [CrossRef]
- Schiffman, J.D.; Fisher, P.G.; Gibbs, P. Early detection of cancer: Past, present, and future. Am. Soc. Clin. Oncol. Educ. Book 2015. [Google Scholar] [CrossRef] [PubMed]
- Istituto Superiore di Sanità. Basi Scientifiche per la Definizione di Linee Guida per il Carcinoma Gastrico. 2011. Available online: http://old.iss.it/binary/lgac/cont/gastricoparte1.pdf (accessed on 13 October 2020).
- Istituto Superiore di Sanità. Sistema Epidemiologico Integrato Delle Epatiti Virali Acute (Seieva)—Bollettino. Available online: https://www.epicentro.iss.it/epatite/Bollettino-Seieva (accessed on 13 October 2020).
- Spagnoli, L.; Flahault, A.; Ferrara, P. Migrant Health Burden: Where Do We Stand? Int. J. Environ. Res. Public Health 2020, 17, 3004. [Google Scholar] [CrossRef]
- Choi, K.; Park, J.; Park, S. Cancer patients’ informational needs on health promotion and related factors: A multi-institutional, cross-sectional study in Korea. Support. Care Cancer 2010, 19, 1495–1504. [Google Scholar] [CrossRef]
- Spagnoli, L.; Navaro, M.; Ferrara, P.; Del Prete, V.; Attena, F. Online information about risks and benefits of screening mammography in 10 European countries. An observational websites analysis. Medicine 2018, 97, e10957. [Google Scholar] [CrossRef]
- Murray, C.J.L.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdollahi, M.; Abedi, P.; Abedi, A.; Abolhassani, H.; et al. Five insights from the Global Burden of Disease Study 2019. Lancet 2020, 396, 1135–1159. [Google Scholar] [CrossRef]
- Botelho, M.C.; Alves, H.; Richter, J. Halting Schistosoma haematobium—Associated bladder cancer. Int. J. Cancer Manag. 2017, 10, e9430. [Google Scholar] [CrossRef]
- Kim, T.S.; Pak, J.H.; Kim, J.B.; Bahk, Y.Y. Clonorchis sinensis, an oriental liver fluke, as a human biological agent of cholangiocarcinoma: A brief review. BMB Rep. 2016, 49, 590–597. [Google Scholar] [CrossRef] [PubMed]
- Sripa, B.; Bethony, J.M.; Sithithaworn, P.; Kaewkes, S.; Mairiang, E.; Loukas, A.; Mulvenna, J.; Laha, T.; Hotez, P.J.; Brindley, P.J. Opisthorchiasis and Opisthorchis-associated cholangiocarcinoma in Thailand and Laos. Acta Trop. 2011, 120, S158–S168. [Google Scholar] [CrossRef] [PubMed]

| Total Deaths | PAF (95% CI) * | Total (N, 95% CI) § | Men (N, 95% CI) § | Women (N, 95% CI) § | |
|---|---|---|---|---|---|
| Helicobacter pylori | |||||
| Non-cardia malignant neoplasm of stomach (C16.1–9) | 8915 | 89% (79–94) | 7934 (7043–8380) | 4538 (4028–4793) | 3396 (3015–3587) |
| Gastric non-Hodgkin lymphoma (C82–85, C96) | 245 | 74% (43–86) | 182 (106–211) | 99 (57–115) | 83 (48–96) |
| Hepatitis C virus | |||||
| Liver cancer (C22) | 4064 | 94% (92–96) | 3812 (3718–3881) | 2583 (2520–2630) | 1229 (1199–1251) |
| Non-Hodgkin’s lymphoma (C82–85, C96) | 4908 | 1.7% (1.5–2.1) | 83 (74–103) | 45 (40–56) | 38 (34–47) |
| Hepatitis B virus | |||||
| Liver cancer (C22) | 801 | 70% (63–76) | 560 (502–610) | 379 (340–413) | 181 (162–197) |
| Human papillomavirus (high-risk HPV types) | |||||
| Carcinoma of the oropharynx | 599 | 24% (17–30) | 144 (102–180) | 106 (75–133) | 37 (27–47) |
| Neoplasm of base of tongue (C01) | 92 | 22 (16–28) | 17 (12–21) | 5 (4–7) | |
| Neoplasm of tonsil (C09) | 186 | 45 (32–56) | 32 (23–41) | 12 (9–15) | |
| Neoplasm of oropharynx (C10) | 321 | 77 (55–96) | 57 (40–71) | 20 (14–25) | |
| Cancer of the oral cavity | 1233 | 4.3% (3.2–5.7) | 53 (39–70) | 30 (22–39) | 23 (17–31) |
| Neoplasm of other and unspecified parts of tongue (C02) | 522 | 22 (15–30) | 13 (9–17) | 10 (7–13) | |
| Neoplasm of gum (C03) | 35 | 2 (1–2) | 1 (1–1) | 1 (1–1) | |
| Neoplasm of floor of mouth (C04) | 38 | 2 (1–2) | 1 (1–1) | 1 (1–1) | |
| Neoplasm of palate (C05) | 72 | 3 (2–4) | 2 (1–2) | 1 (1–2) | |
| Neoplasm of other and unspecified parts of mouth (C06) | 566 | 24 (18–32) | 14 (10–18) | 11 (8–14) | |
| Anal carcinoma (C21) | 278 | 88% (85–91) | 245 (236–253) | 93 (90–96) | 151 (146–157) |
| Laryngeal cancer (C32) | 1480 | 4.6% (3.3–6.1) | 68 (49–90) | 61 (44–80) | 7 (5–10) |
| Vulvar carcinoma (C51) | 497 | 16.6% (12.5–19.8) | 82 (62–98) | - | 82 (62–98) |
| Vaginal carcinoma (C52) | 93 | 78% (68–86) | 73 (63–80) | - | 73 (63–80) |
| Cervix uteri carcinoma (C53) | 442 | 100% | 442 | - | 442 |
| Penile carcinoma (C60) | 121 | 51% (47–55) | 62 (57–67) | 62 (57–67) | - |
| Epstein–Barr virus | |||||
| Nasopharyngeal carcinoma (C11) | 211 | 96.7% | 204 | 149 | 55 |
| Hodgkin’s lymphoma (C81) | 424 | 36% (32–39) | 153 (136–165) | 91 (81–99) | 61 (54–66) |
| Burkitt’s lymphoma (C83.7) | 51 | 20% | 10 | 7 | 3 |
| Human herpesvirus type 8 | |||||
| Kaposi’s sarcoma (C46) | 137 | 100% | 137 | 76 | 61 |
| Human T-cell lymphotropic virus type 1 | |||||
| Adult T-cell leukemia/lymphoma (C91.5) | 7 | 100% | 7 | 3 | 4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferrara, P.; Conti, S.; Agüero, F.; Albano, L.; Masuet-Aumatell, C.; Ramon-Torrell, J.M.; Mantovani, L.G. Estimates of Cancer Mortality Attributable to Carcinogenic Infections in Italy. Int. J. Environ. Res. Public Health 2020, 17, 8723. https://doi.org/10.3390/ijerph17238723
Ferrara P, Conti S, Agüero F, Albano L, Masuet-Aumatell C, Ramon-Torrell JM, Mantovani LG. Estimates of Cancer Mortality Attributable to Carcinogenic Infections in Italy. International Journal of Environmental Research and Public Health. 2020; 17(23):8723. https://doi.org/10.3390/ijerph17238723
Chicago/Turabian StyleFerrara, Pietro, Sara Conti, Fernando Agüero, Luciana Albano, Cristina Masuet-Aumatell, Josep Maria Ramon-Torrell, and Lorenzo Giovanni Mantovani. 2020. "Estimates of Cancer Mortality Attributable to Carcinogenic Infections in Italy" International Journal of Environmental Research and Public Health 17, no. 23: 8723. https://doi.org/10.3390/ijerph17238723
APA StyleFerrara, P., Conti, S., Agüero, F., Albano, L., Masuet-Aumatell, C., Ramon-Torrell, J. M., & Mantovani, L. G. (2020). Estimates of Cancer Mortality Attributable to Carcinogenic Infections in Italy. International Journal of Environmental Research and Public Health, 17(23), 8723. https://doi.org/10.3390/ijerph17238723







