Effect of Extreme Weather Events on Mental Health: A Narrative Synthesis and Meta-Analysis for the UK
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
2.2. Data Extraction and Quality Assessment
2.3. Narrative Synthesis and Meta-Analysis
3. Results
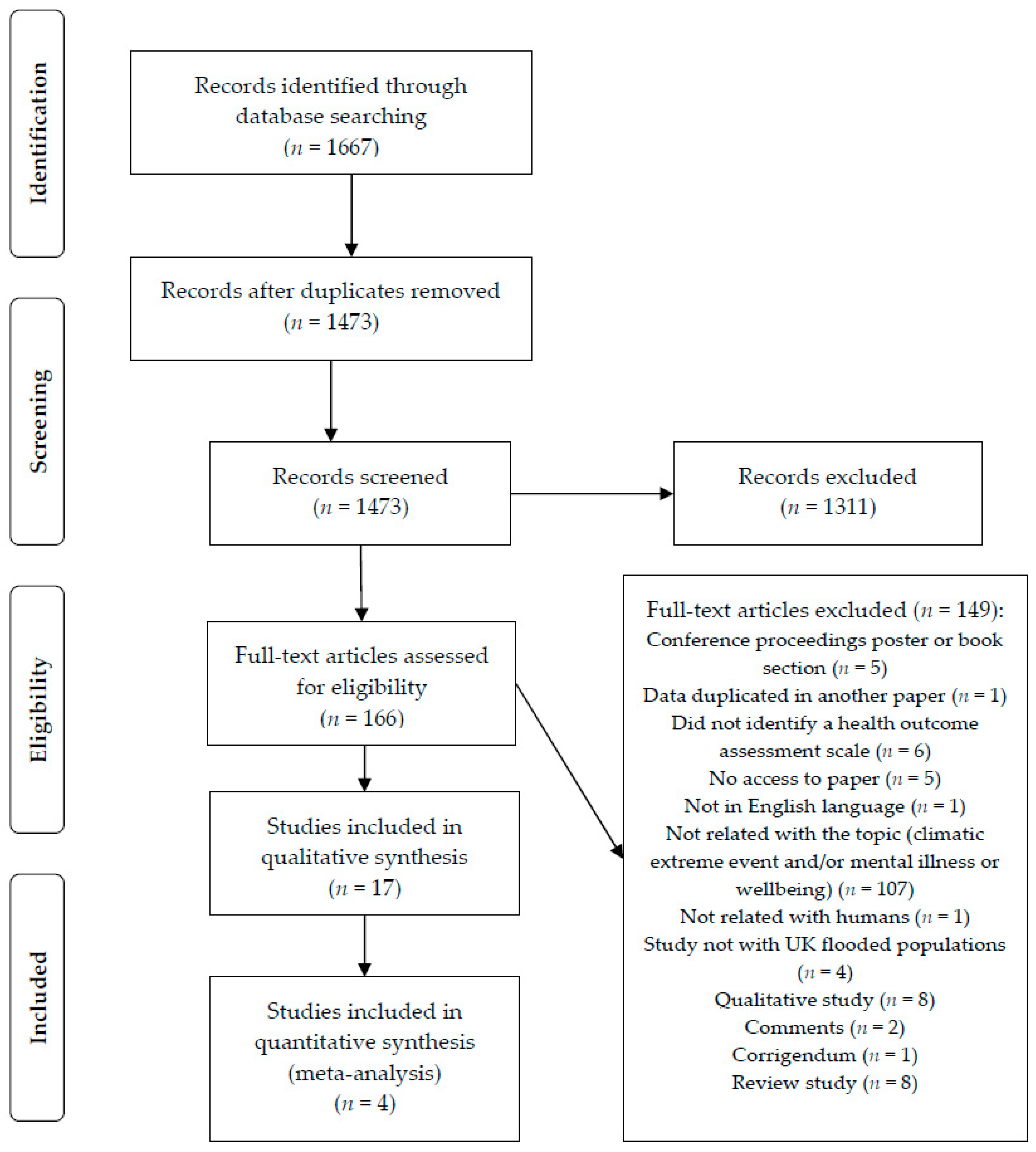
3.1. Study Selection
3.2. Study Characteristics
3.3. Narrative Analysis
3.3.1. Mental Health Morbidity
3.3.2. Physical Health and Long-Lasting Impacts on Mental Health
3.3.3. Characteristics of the Flood
3.3.4. Flood Warnings
3.3.5. Displacement and Loss of Sense of Place
3.3.6. Demographic and Socio-Economic Profile of Flood Impact
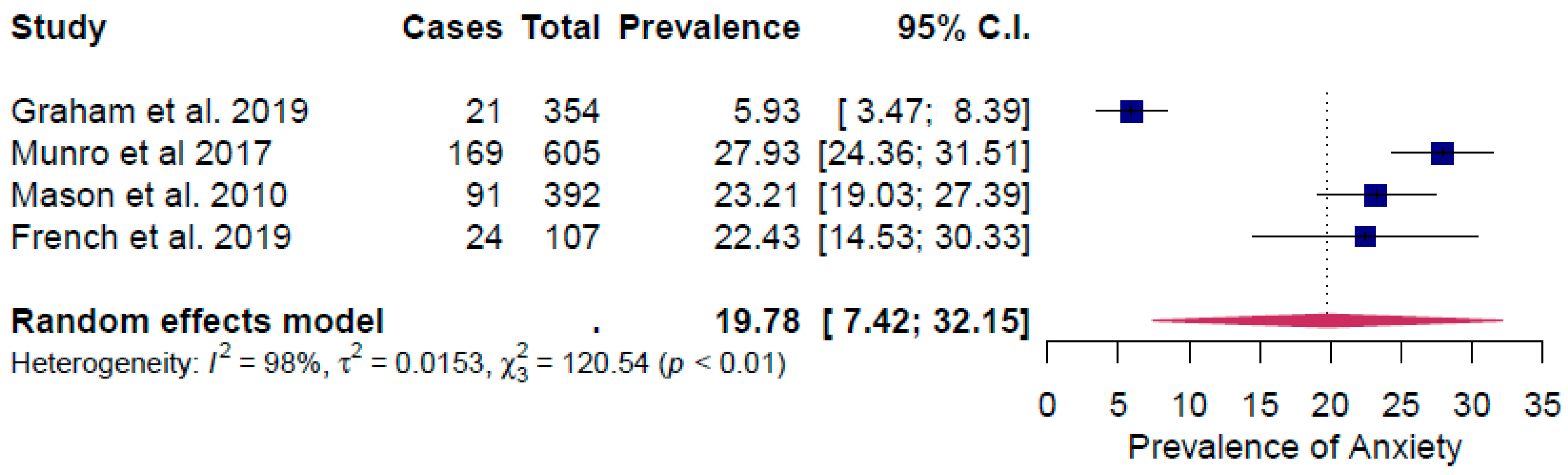
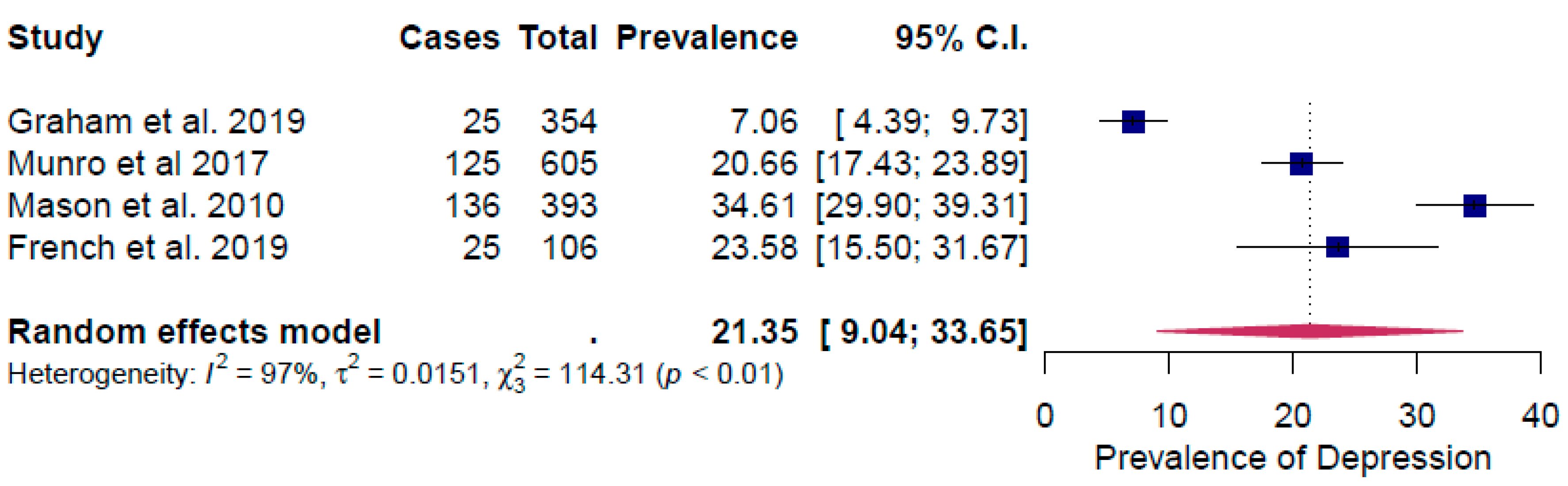
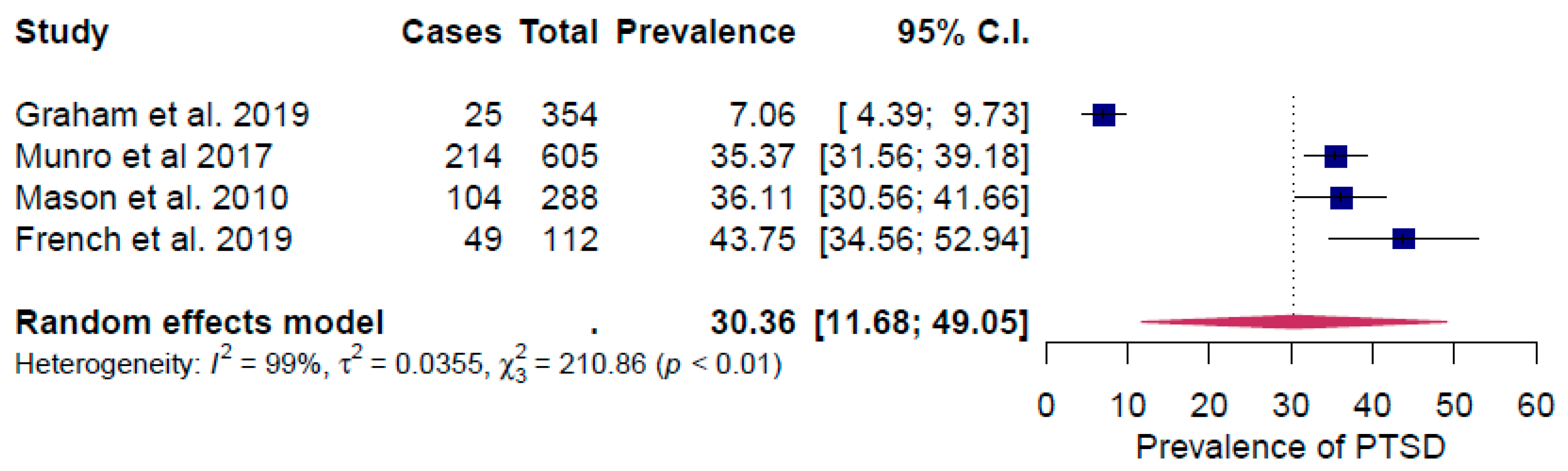
3.4. Meta-Analysis of the Prevalence of Common Mental Health Problems
4. Discussion
4.1. Implications for Research and Policy
4.2. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Whitmee, S.; Haines, A.; Beyrer, C.; Boltz, F.; Capon, A.G.; de Souza Dias, B.F.; Ezeh, A.; Frumkin, H.; Gong, P.; Head, P.; et al. Safeguarding human health in the Anthropocene epoch: Report of The Rockefeller Foundation-Lancet Commission on planetary health. Lancet 2015, 386, 1973–2028. [Google Scholar] [CrossRef]
- Elsner, J.B. Continued increases in the intensity of strong tropical cyclones. Bull. Am. Meteorol. Soc. 2020. [Google Scholar] [CrossRef]
- EASAC. Extreme Weather Events in Europe: Preparing for Climate Change Adaptation: An Update on EASAC’s 2013 Study; European Academies’ Science Advisory Council: Brussels, Belgium, 2018. [Google Scholar]
- Guerreiro, S.B.; Dawson, R.J.; Kilsby, C.; Lewis, E.; Ford, A. Future heat-waves, droughts and floods in 571 European cities. Environ. Res. Lett. 2018, 13, 034009. [Google Scholar] [CrossRef]
- McMichael, A.J.; Woodruff, R.E.; Hales, S. Climate change and human health: Present and future risks. Lancet 2006, 367, 859–869. [Google Scholar] [CrossRef]
- IPCC. Climate Change 2014: Impacts, Adaptation, and Vulnerability. Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; Cambridge University Press: Cambridge, UK, 2014. [Google Scholar]
- Clayton, S.; Devine-Wright, P.; Stern, P.C.; Whitmarsh, L.; Carrico, A.; Steg, L.; Swim, J.; Bonnes, M. Psychological research and global climate change. Nat. Clim. Chang. 2015, 5, 640–646. [Google Scholar] [CrossRef]
- Hoegh-Guldberg, O.; Jacob, D.; Bindi, M.; Brown, S.; Camilloni, I.; Diedhiou, A.; Djalante, R.; Ebi, K.; Engelbrecht, F.; Guiot, J. Global warming of 1.5 °C. In An IPCC Special Report on the Impacts of Global Warming of 1.5 °C above Pre-Industrial Levels and Related Global Greenhouse Gas Emission Pathways, in the Context of Strengthening the Global Response to the Threat of Climate Change, Sustainable Development, and Efforts to Eradicate Poverty; Masson-Delmotte, V., Pörtner, H.O., Eds.; Cambridge University Press: Cambridge, UK, 2018; pp. 175–311. [Google Scholar]
- Palinkas, L.A.; Wong, M. Global climate change and mental health. Curr. Opin. Psychol. 2020, 32, 12–16. [Google Scholar] [CrossRef]
- Haines, A.; Kovats, R.S.; Campbell-Lendrum, D.; Corvalan, C. Climate change and human health: Impacts, vulnerability, and mitigation. Lancet 2006, 367, 2101–2109. [Google Scholar] [CrossRef]
- James, S.L.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef]
- Chisholm, D.; Sweeny, K.; Sheehan, P.; Rasmussen, B.; Smit, F.; Cuijpers, P.; Saxena, S. Scaling-up treatment of depression and anxiety: A global return on investment analysis. Lancet Psychiatry 2016, 3, 415–424. [Google Scholar] [CrossRef]
- Office for National Statistics. Sickness absence in the labour market: 2018. Analysis describing sickness absence rates of workers in the UK labour market; Office for National Statistics: London, UK, 2018.
- O’Shea, N.; Bell, A. A Spending Review for Wellbeing-Briefing; Centre for Mental health: London, UK, 2020. [Google Scholar]
- Graham, H.; White, P.; Cotton, J.; McManus, S. Flood- and weather-damaged homes and mental health: An analysis using England’s Mental Health Survey. Int. J. Environ. Res. Public Health 2019, 16, 3256. [Google Scholar] [CrossRef]
- Mason, V.; Andrews, H.; Upton, D. The psychological impact of exposure to floods. Psychol. Health Med. 2010, 15, 61–73. [Google Scholar] [CrossRef] [PubMed]
- ASC UK. Climate Change Risk Assessment 2017 Synthesis Report: Priorities for the Next Five Years; Adaptation Sub-Committee of the Committee on Climate Change: London, UK, 2016. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [PubMed]
- Stephenson, D.B.; Diaz, H.; Murnane, R. Definition, diagnosis, and origin of extreme weather and climate events. In Climate extremes and society; Diaz, H.F., Murnane, R.J., Eds.; Cambridge University Press: Cambridge, UK, 2008; Volume 340, pp. 11–23. [Google Scholar]
- World Health Organization (WHO). International Statistical Classification of Diseases and Related Health Problems (ICD-10); 10th Revision; WHO: Geneva, Switzerland, 1992. [Google Scholar]
- Loney, P.L.; Chambers, L.W.; Bennett, K.J.; Roberts, J.G.; Stratford, P.W. Critical appraisal of the health research literature: Prevalence or incidence of a health problem. Chronic Dis. Can. 1998, 19, 170–176. [Google Scholar] [PubMed]
- Mays, N.; Pope, C.; Popay, J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J. Health Serv. Res. Policy 2005, 10, 6–20. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Wang, N. Conducting Meta-Analyses of Proportions in R; Research Gate: College Station, TX, USA, 2017. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2019. [Google Scholar]
- French, C.E.; Waite, T.D.; Armstrong, B.; Rubin, G.J.; Beck, C.R.; Oliver, I. Impact of repeat flooding on mental health and health-related quality of life: A cross-sectional analysis of the English National Study of Flooding and Health. BMJ Open 2019, 9, e031562. [Google Scholar] [CrossRef]
- Munro, A.; Kovats, R.S.; Rubin, G.J.; Waite, T.D.; Bone, A.; Armstrong, B.; Beck, C.R.; Amlot, R.; Leonardi, G.; Oliver, I. Effect of evacuation and displacement on the association between flooding and mental health outcomes: A cross-sectional analysis of UK survey data. Lancet Planet. Health 2017, 1, e134–e141. [Google Scholar] [CrossRef]
- Jermacane, D.; Waite, T.D.; Beck, C.R.; Bone, A.; Amlot, R.; Reacher, M.; Kovats, S.; Armstrong, B.; Leonardi, G.; James Rubin, G.; et al. The English National Cohort Study of Flooding and Health: The change in the prevalence of psychological morbidity at year two. BMC Public Health 2018, 18, 330. [Google Scholar] [CrossRef]
- Tunstall, S.; Tapsell, S.; Green, C.; Floyd, P.; George, C. The health effects of flooding: Social research results from England and Wales. J. Water Health 2006, 4, 365–380. [Google Scholar] [CrossRef]
- Reacher, M.; McKenzie, K.; Lane, C.; Nichols, T.; Kedge, I.; Iversen, A.; Hepple, P.; Walter, T.; Laxton, C.; Simpson, J. Health impacts of flooding in Lewes: A comparison of reported gastrointestinal and other illness and mental health in flooded and non-flooded households. Comm. Dis. Publ. Health 2004, 7, 39–46. [Google Scholar]
- Paranjothy, S.; Gallacher, J.; Amlot, R.; Rubin, G.J.; Page, L.; Baxter, T.; Wight, J.; Kirrage, D.; McNaught, R.; Palmer, S.R. Psychosocial impact of the summer 2007 floods in England. BMC Public Health 2011, 11, 145. [Google Scholar] [CrossRef] [PubMed]
- Tempest, E.L.; Carter, B.; Beck, C.R.; Rubin, G.J.; English Natl Study Flooding, H. Secondary stressors are associated with probable psychological morbidity after flooding: A cross-sectional analysis. Eur. J. Public Health 2017, 27, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Waite, T.D.; Chaintarli, K.; Beck, C.R.; Bone, A.; Amlot, R.; Kovats, S.; Reacher, M.; Armstrong, B.; Leonardi, G.; Rubin, G.J.; et al. The English national cohort study of flooding and health: Cross-sectional analysis of mental health outcomes at year one. BMC Public Health 2017, 17, 129. [Google Scholar] [CrossRef] [PubMed]
- Greene, G.; Paranjothy, S.; Palmer, S.R. Resilience and Vulnerability to the Psychological Harm from Flooding: The Role of Social Cohesion. Am. J. Public Health 2015, 105, 1792–1795. [Google Scholar] [CrossRef] [PubMed]
- Bennet, G. Bristol floods 1968. Controlled survey of effects on health of local community disaster. Br. Med. J. 1970, 3, 454–458. [Google Scholar] [CrossRef] [PubMed]
- Tapsell, S.M.; Tunstall, S.M. “I wish I’d never heard of Banbury”: The relationship between ‘place’ and the health impacts from flooding. Health Place 2008, 14, 133–154. [Google Scholar] [CrossRef]
- Akerkar, S.; Fordham, M. Gender, place and mental health recovery in disasters: Addressing issues of equality and difference. Int. J. Disaster Risk Reduct 2017, 23, 218–230. [Google Scholar] [CrossRef]
- Wind, T.R.; Komproe, I.H. The mechanisms that associate community social capital with post-disaster mental health: A multilevel model. Soc. Sci. Med. 2012, 75, 1715–1720. [Google Scholar] [CrossRef]
- Milojevic, A.; Armstrong, B.; Wilkinson, P. Mental health impacts of flooding: A controlled interrupted time series analysis of prescribing data in England. J. Epidemiol. Community Health 2017, 71, 970–973. [Google Scholar] [CrossRef]
- Page, L.A.; Hajat, S.; Kovats, R.S. Relationship between daily suicide counts and temperature in England and Wales. Br. J. Psychiatry 2007, 191, 106–112. [Google Scholar] [CrossRef]
- Lamond, J.E.; Joseph, R.D.; Proverbs, D.G. An exploration of factors affecting the long term psychological impact and deterioration of mental health in flooded households. Environ. Res. 2015, 140, 325–334. [Google Scholar] [CrossRef] [PubMed]
- Tapsell, S. The hidden impacts of flooding: Experiences from two English communities. In Water Resources Management; Marino, M.A., Simonovic, S.P., Eds.; IAHS Press: Wallingford, UK, 2001; pp. 319–324. [Google Scholar]
- Kessler, R.C.; Chiu, W.T.; Demler, O.; Merikangas, K.R.; Walters, E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Hasin, D.S.; Sarvet, A.L.; Meyers, J.L.; Saha, T.D.; Ruan, W.J.; Stohl, M.; Grant, B.F. Epidemiology of Adult DSM-5 Major Depressive Disorder and Its Specifiers in the United States. JAMA Psychiatry 2018, 75, 336–346. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef]
- Heo, J.H.; Kim, M.H.; Koh, S.B.; Noh, S.; Park, J.H.; Ahn, J.S.; Park, K.C.; Shin, J.; Min, S. A prospective study on changes in health status following flood disaster. Psychiatry Investig. 2008, 5, 186–192. [Google Scholar] [CrossRef]
- Liu, A.; Tan, H.; Zhou, J.; Li, S.; Yang, T.; Wang, J.; Liu, J.; Tang, X.; Sun, Z.; Wen, S.W. An epidemiologic study of posttraumatic stress disorder in flood victims in Hunan China. Can. J. Psychiatry 2006, 51, 350–354. [Google Scholar] [CrossRef]
- Charlson, F.; van Ommeren, M.; Flaxman, A.; Cornett, J.; Whiteford, H.; Saxena, S. New WHO prevalence estimates of mental disorders in conflict settings: A systematic review and meta-analysis. Lancet 2019, 394, 240–248. [Google Scholar] [CrossRef]
- Stedman, R.C. Toward a Social Psychology of Place:Predicting Behavior from Place-Based Cognitions, Attitude, and Identity. Environ. Behav. 2002, 34, 561–581. [Google Scholar] [CrossRef]
- Rose, S.; Bisson, J.; Churchill, R.; Wessely, S. Psychological debriefing for preventing post traumatic stress disorder (PTSD). Cochrane Database Syst. Rev. 2002, CD000560. [Google Scholar] [CrossRef]
- Suka, M.; Yamauchi, T.; Sugimori, H. Help-seeking intentions for early signs of mental illness and their associated factors: Comparison across four kinds of health problems. BMC Public Health 2016, 16, 301. [Google Scholar] [CrossRef]
- Hadlaczky, G.; Hokby, S.; Mkrtchian, A.; Carli, V.; Wasserman, D. Mental Health First Aid is an effective public health intervention for improving knowledge, attitudes, and behaviour: A meta-analysis. Int. Rev. Psychiatry 2014, 26, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Morgan, A.J.; Ross, A.; Reavley, N.J. Systematic review and meta-analysis of Mental Health First Aid training: Effects on knowledge, stigma, and helping behaviour. PLoS ONE 2018, 13, e0197102. [Google Scholar] [CrossRef] [PubMed]
- Richardson, R.; Dale, H.E.; Wellby, G.; McMillan, D.; Churchill, R. Mental Health First Aid as a tool for improving mental health and well-being. Cochrane Database Syst. Rev. 2018. [Google Scholar] [CrossRef]
- The Lancet Psychiatry. Send in the therapists? Lancet Psychiatry 2020, 7, 291. [Google Scholar] [CrossRef]
- Berry, H.L.; Waite, T.D.; Dear, K.B.G.; Capon, A.G.; Murray, V. The case for systems thinking about climate change and mental health. Nat. Clim. Change 2018, 8, 282–290. [Google Scholar] [CrossRef]
- Bradford, R.A.; O’Sullivan, J.J.; van der Craats, I.M.; Krywkow, J.; Rotko, P.; Aaltonen, J.; Bonaiuto, M.; De Dominicis, S.; Waylen, K.; Schelfaut, K. Risk perception–issues for flood management in Europe. Nat. Hazard Earth Sys. Sci. 2012, 12, 2299–2309. [Google Scholar] [CrossRef]
- Zevenbergen, C.; Veerbeek, W.; Gersonius, B.; van Herk, S. Challenges in urban flood management: Travelling across spatial and temporal scales. J. Flood Risk Manag. 2008, 1, 81–88. [Google Scholar] [CrossRef]
- Allwood, L. Our Place: Local Authorities and the Public’s Mental Health; Centre for Mental Health: London, UK, 2020. [Google Scholar]
| Study | Event | Location (Year of Event) | Months after the Event | Respondents’ Characteristics | Health Outcome | Health Outcome Measurement | Included in Meta-Analysis (Y/N) | Quality Score (0–8) |
|---|---|---|---|---|---|---|---|---|
| French et al. [26] | Flood | Cumbria (2015/16) | 6 | Flooded: 119; Gender: 59%; Ethnicity: 100% white; Marital status: 64% married/civil partners or cohabiting; Housing tenure: 82% owned house; Employment: 52% employed and 40% retired; Education level: 45% with degree or above, 32% below degree; English deprivation quintile: 1.7% in least deprived quintile; 6% in quintile 4 and 5 (most deprived); Long-term illness: 72% yes | Depression; Anxiety; Post-traumatic stress disorder (PTSD); Health-related quality of life | Patient Health Questionnaire (PHQ-2) depression sub-scale; Generalized Anxiety Disorder scale (GAD-2); short-form PTSD checklist (PCL-6); 5 level EQ-5D (EQ-5D-5L) | Y | 5 |
| Graham et al. [15] | Flood | England (2013/2014) | 6 | Flooded: 354; Age: 26% aged 16–34, 39% aged 35–54; 27% aged 55–74 and 8% 75+; Ethnicity: 89% white, 1% black, 7% Asian; Education level: 31% with degree, 14% teaching, HND and nursing, 14% A level, 26% GCSE or equivalent, 13% no qualifications; Housing tenure: 76% owned house; Employment: 69% employed, 28% economically inactive and 3% unemployed; English deprivation quintile: 29% in least deprived quintile, 34% in quintile 4 and 5 (most deprived) | Depression; Anxiety; Obsessive compulsive disorder; Panic disorder; Phobias; PTSD; Suicide ideation | Clinical Interview Schedule–Revised (CIS–R); PTSD Checklist Civilian Version (PCL–C) | Y | 7 |
| Mason et al. [16] | Flood | Anonymized | 6 | Gender: 182 males and 262 females; Mean Age: 57 years (SD = ±15 years); Employment: 46% employed, 0.9% unemployed and 33.6% retired | Depression; Anxiety; PTSD; | Hopkins Symptoms Checklist; Harvard Trauma Questionnaire | Y | 6 |
| Munro et al. [27] | Flood | Counties of Gloucestershire, Wiltshire, Surrey, Somerset, and Kent (2013/2014) | 12 | Flooded: 605 Age: 6.3% aged 18–35, 54% 36–64; 28.8% aged 65–79 and 8% 80+; Marital status: 69.3% married/civil partners or cohabiting; Housing tenure: 90.4% owned house; Employment: 49.8% employed and 3.8% retired; Education level: 37.0% with degree or above, 39.2% below degree; English deprivation quintile: 26.2% in least deprived quintile; 2.6% in quintile 4 and 5 (most deprived); Long-term illness: 22% yes | Depression; Anxiety; PTSD | Patient Health Questionnaire (PHQ-2) depression sub-scale; Generalized Anxiety Disorder scale (GAD-2); short-form PTSD checklist (PCL-6) | Y | 6 |
| Jermacane et al. [28] | Flood | England (2013/2014) | 24 | Flooded: 339 | Anxiety; Depression; PTSD | Patient Health Questionnaire (PHQ-2) depression sub-scale; Generalized Anxiety Disorder scale (GAD-2); short-form PTSD checklist (PCL-6) | N | 6 |
| Tunstall et al. [29] | Flood | England and Wales (1998) | 60 | Flooded: 982 respondents | Anxiety; Depression; PTSD; Psychological distress; Suicide ideation | General Health Questionnaire (GHQ-12); Post-Traumatic Stress Scale (PTSS) | N | 5 |
| Reacher et al. [30] | Flood | Lewes (2000) | 9 | Flooded: 227; Gender: 123 females; Age: 22% aged 0–17, 24% 18–39; 17% aged 40–49, 22% aged 50–64 and 15% 65+ | Psychological distress | General Health Questionnaire (GHQ-12) | N | 7 |
| Paranjothy et al. [31] | Flood | South Yorkshire and Worcestershire (2007) | South Yorkshire: 3 Worcestershire: 6 | Gender: 72% females in South Yorkshire and 57% females in Worcestershire; Mean age: 50 years (SD = ±17 years) in South Yorkshire and 57 years (SD = ±17 years) in Worcestershire; Employment: 28% unemployed and 24% retired in South Yorkshire; and 39% unemployed and 9% retired in Worcestershire | Depression; Anxiety; PTSD; Psychological distress | Patient Health Questionnaire (PHQ-9) depression sub-scale; Generalized Anxiety Disorder scale (GAD-7); short-form PTSD checklist (PCL-6); General Health Questionnaire (GHQ-12) | N | 6 |
| Tempest et al. [32] | Flood | Anonymized (2013/2014) | 12 | Flooded: 622 | Depression; Anxiety; PTSD | Patient Health Questionnaire (PHQ-2) depression sub-scale; Generalized Anxiety Disorder scale (GAD-2); short-form PTSD checklist (PCL-6); | N | 6 |
| Waite et al. [33] | Flood | Counties of Gloucestershire, Wiltshire, Surrey, Sedgemoor, South Somerset, and Tonbridge and Malling (2013/2014) | 12 | Collected but not provided | Depression; Anxiety; PTSD | Patient Health Questionnaire (PHQ-2) depression sub-scale; Generalized Anxiety Disorder scale (GAD-2); short-form PTSD checklist (PCL-6); | N | 5 |
| Greene et al. [34] | Flood | South Yorkshire and Worcestershire (2007) | 1–7 | 2029 responders (flooded and unaffected); Mean Age: South Yorkshire: 50 years (SD = ±17 years), Worcestershire: 57 years (SD = ±17 years) | Psychological distress | General Health Questionnaire (GHQ-12) | N | 5 |
| Bennet [35] | Flood | Bristol (1968) | 12 | Flooded: 88 males and 109 females | Psychiatric complaints | Self-reported | N | 3 |
| Tapsell and Tunstall [36] | Flood | Banbury and Kidlington (1998) | 7; 12; 54 | Gender: 11 males and 21 females | Anxiety; Depression; Suicide ideation; Psychological distress | General Health Questionnaire (GHQ-12) | N | 4 |
| Akerkar and Fordham [37] | Flood | Tewkesbury (2007) Morpeth (2008) | Tewkesbury: 18 Morpeth: 12 | Gender: Tewkesbury: 60 males and 76 females; Morpeth: 90 males and 146 females | Wellbeing | Mental Health Inventory (MHI-5); SF-12 Patient Questionnaire (SF-12) | N | 3 |
| Wind and Komproe [38] | Flood | Morpeth (2008) | 12 | Flooded: 231; Gender: 61% females; Age: 2.7% aged 18–24, 9% aged 25–39, 42.6% aged 40–64 and 57.4% 65+; Marital status: 38.4% married/civil partners or cohabiting; Housing tenure: 90.4% owned house; Employment: 32.3% employed and 57.3% retired; Education level: 22% with degree or above | PTSD | PTSD Checklist Civilian Version (PCL-C) | N | 5 |
| Milojevic et al. [39] | Flood | England (2011/2014) | NA | NA | Depression | Number of antidepressants prescribed | N | 4 |
| Page et al. [40] | Heat wave | England and Wales (1995 and 2003) | Suicide | Suicide counts | N | 7 |
| Mental Health Morbidity | Prevalence in Population Exposed to Flooding (%) | Prevalence in General Population (%) |
|---|---|---|
| Anxiety | 19.8 | 5.7 |
| Depression | 21.4 | 20.6 |
| PTSD | 30.4 | 7.8 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cruz, J.; White, P.C.L.; Bell, A.; Coventry, P.A. Effect of Extreme Weather Events on Mental Health: A Narrative Synthesis and Meta-Analysis for the UK. Int. J. Environ. Res. Public Health 2020, 17, 8581. https://doi.org/10.3390/ijerph17228581
Cruz J, White PCL, Bell A, Coventry PA. Effect of Extreme Weather Events on Mental Health: A Narrative Synthesis and Meta-Analysis for the UK. International Journal of Environmental Research and Public Health. 2020; 17(22):8581. https://doi.org/10.3390/ijerph17228581
Chicago/Turabian StyleCruz, Joana, Piran C. L. White, Andrew Bell, and Peter A. Coventry. 2020. "Effect of Extreme Weather Events on Mental Health: A Narrative Synthesis and Meta-Analysis for the UK" International Journal of Environmental Research and Public Health 17, no. 22: 8581. https://doi.org/10.3390/ijerph17228581
APA StyleCruz, J., White, P. C. L., Bell, A., & Coventry, P. A. (2020). Effect of Extreme Weather Events on Mental Health: A Narrative Synthesis and Meta-Analysis for the UK. International Journal of Environmental Research and Public Health, 17(22), 8581. https://doi.org/10.3390/ijerph17228581






