Health Sciences—Evidence Based Practice Questionnaire (HS-EBP): Normative Data and Differential Profiles in Spanish Osteopathic Professionals
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Instrument
2.4. Statistical Analysis
2.5. Ethical Considerations
3. Results
3.1. Normative Data
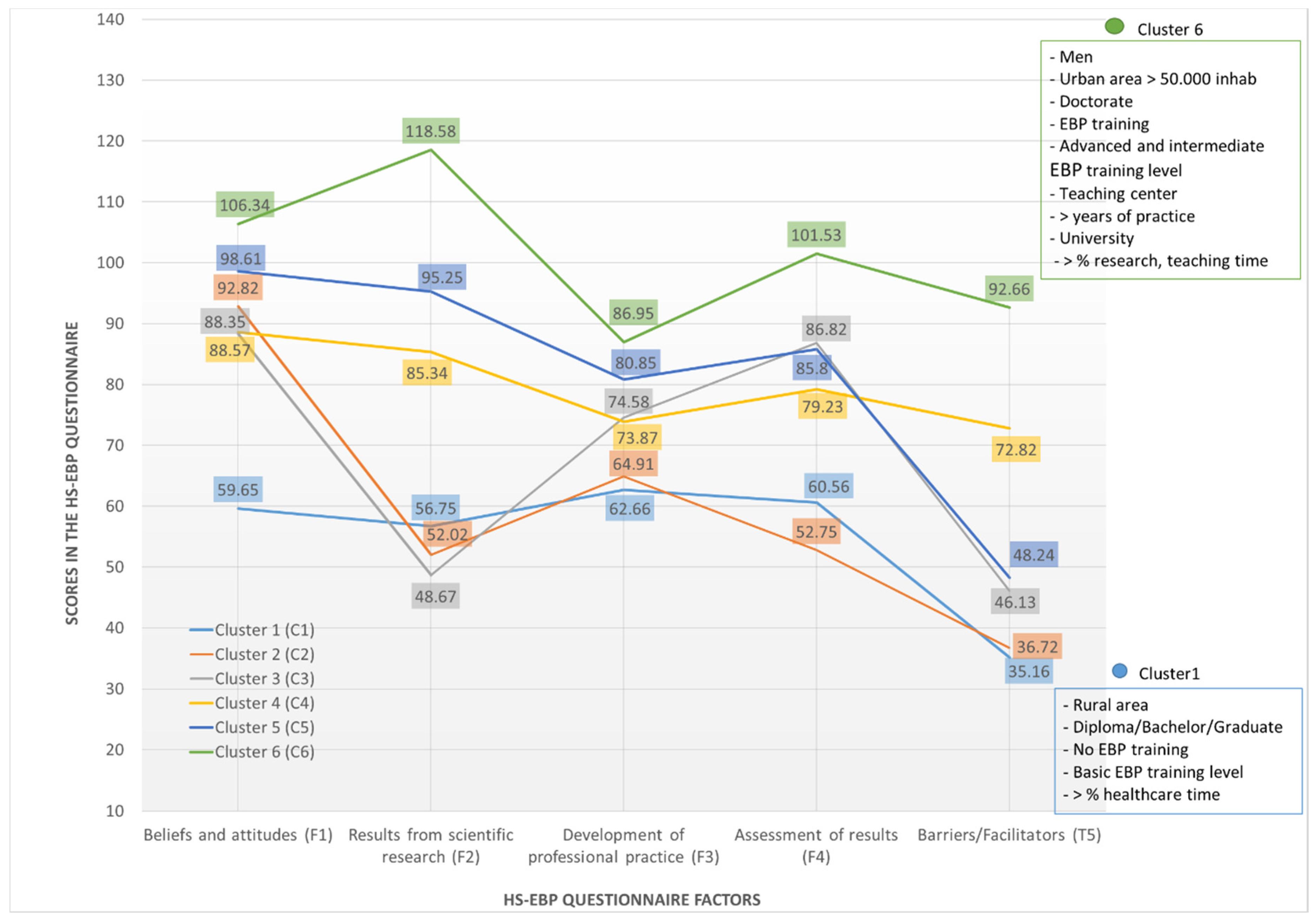
3.2. Clusters and Differential Profiles
4. Discussion
“future research should determine ideal levels of EBP activity for practicing osteopaths, and whether that might vary between different clinical settings and scopes of practice (e.g., Europe vs. US) … and further, whether different levels of EBP activity translate into poorer or improved patient outcomes” (p. 8).
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bliss-Holtz, J. Evidence-Based Practice: A Primer for Action. Issues Compr. Pediatr. Nurs. 2007, 30, 165–182. [Google Scholar] [CrossRef] [PubMed]
- Beckett, C.D.; Melnyk, B.M. Evidence-ased practice competencies and the new EBP-C credential: Keys to achieving the quadruple aim in health care. Worldviews Evid. Based Nurs. 2018, 15, 412–413. [Google Scholar] [CrossRef] [PubMed]
- Licciardone, J.C. Educating osteopaths to be researchers What role should research methods and statistics have in an undergraduate curriculum? Int. J. Osteopath. Med. 2008, 11, 62–68. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fryer, G. Teaching critical thinking in osteopathy—Integrating craft knowledge and evidence-informed approaches. Int. J. Osteopath. Med. 2008, 11, 56–61. [Google Scholar] [CrossRef]
- Thomson, O.P.; Petty, N.J.; Moore, A.P. Clinical reasoning in osteopathy—More than just principles? Int. J. Osteopath. Med. 2011, 14, 71–76. [Google Scholar] [CrossRef]
- Fawkes, C.; Ward, E.; Carnes, D. What evidence is good evidence? A master class in critical evaluation. Int. J. Osteopath. Med. 2015, 18, 116–129. [Google Scholar] [CrossRef]
- Vogel, S. Evidence, theory and variability in osteopathic practice. Int. J. Osteopath. Med. 2015, 18, 1–4. [Google Scholar] [CrossRef][Green Version]
- McGrath, M.C. A global view of osteopathic practice—Mirror or echo chamber? Int. J. Osteopath. Med. 2015, 18, 130–140. [Google Scholar] [CrossRef]
- Sundberg, T.; Leach, M.J.; Thomson, O.P.; Austin, P.; Fryer, G.; Adams, J. Attitudes, skills and use of evidence-based practice among UK osteopaths: A national cross-sectional survey. BMC Musculoskelet. Disord. 2018, 19, 439. [Google Scholar] [CrossRef]
- Leach, M.J.; Sundberg, T.; Fryer, G.; Austin, P.; Thomson, O.P.; Adams, J. An investigation of Australian osteopaths’ attitudes, skills and utilisation of evidence-based practice: A national cross-sectional survey. BMC Health Serv. Res. 2019, 19, 498. [Google Scholar] [CrossRef]
- Webber, V.; Rajendran, D. UK trained osteopaths’ relationship to evidence based practice—An analysis of influencing factors. Int. J. Osteopath. Med. 2018, 29, 15–25. [Google Scholar] [CrossRef]
- Adams, J.; Sibbritt, D.; Steel, A.; Peng, W. A workforce survey of Australian osteopathy: Analysis of a nationally-representative sample of osteopaths from the Osteopathy Research and Innovation Network (ORION) project. BMC Health Serv. Res. 2018, 18, 352. [Google Scholar] [CrossRef]
- Panczyk, M.; Belowska, J.; Zarzeka, A.; Samoliński, Ł.; Żmuda-Trzebiatowska, H.; Gotlib, J. Validation study of the Polish version of the Evidence-Based Practice Profile Questionnaire. BMC Med. Educ. 2017, 17, 1–9. [Google Scholar] [CrossRef]
- Fujimoto, S.; Kon, N.; Takasugi, J.; Nakayama, T. Attitudes, knowledge and behaviour of japanese physical therapists with regard to evidence-based practice and clinical practice guidelines: A crosssectional mail survey. J. Phys. Ther. Sci. 2017, 29, 198–208. [Google Scholar] [CrossRef] [PubMed]
- Zabaleta-Del-Olmo, E.; Subirana-Casacuberta, M.; Ara-Pérez, A.; Escuredo-Rodríguez, B.; Ríos-Rodríguez, M.Á.; Carrés-Esteve, L.; Jodar-Solà, G.; Lejardi-Estevez, Y.; Nuix-Baqué, N.; Aguas-Lluch, A.; et al. Developing Evidence-Based Practice questionnaire for community health nurses: Reliability and validity of a Spanish adaptation. J. Clin. Nurs. 2016, 25, 505–517. [Google Scholar] [CrossRef] [PubMed]
- Bierwas, D.A.; Leafman, J.; Shaw, D.K. The evidence-based practice belifs and knowledge of physical therapy clinical instructors. Internet J. Allied Health Sci. Pract. 2016, 19, 10. [Google Scholar]
- Suter, E.; Vanderheyden, L.C.; Trojan, L.S.; Verhoef, M.J.; Armitage, G.D. How Important is Research-Based Practice to Chiropractors and Massage Therapists? J. Manip. Physiol. Ther. 2007, 30, 109–115. [Google Scholar] [CrossRef]
- Walker, B.; Stomski, N.J.; Hebert, J.; French, S. Evidence-based practice in chiropractic practice: A survey of chiropractors’ knowledge, skills, use of research literature and barriers to the use of research evidence. Complement. Ther. Med. 2014, 22, 286–295. [Google Scholar] [CrossRef]
- Veziari, Y.; Leach, M.J.; Kumar, S. Barriers to the conduct and application of research in complementary and alternative medicine: A systematic review. BMC Complement. Altern. Med. 2017, 17, 166. [Google Scholar] [CrossRef]
- Bussières, A.E.; Terhorst, L.; Leach, M.; Stuber, K.; Evans, R.; Schneider, M.J. Self-reported attitudes, skills and use of evidence-based practice among Canadian doctors of chiropractic: A national survey. J. Can. Chiropr. Assoc. 2015, 59, 332–348. [Google Scholar]
- Sullivan, M.; Leach, M.J.; Snow, J.; Moonaz, S.H. Understanding North American yoga therapists’ attitudes, skills and use of evidence-based practice: A cross-national survey. Complement. Ther. Med. 2017, 32, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Alcantara, J.; Leach, M.J. Chiropractic Attitudes and Utilization of Evidence-Based Practice: The Use of the EBASE Questionnaire. Explore 2015, 11, 367–376. [Google Scholar] [CrossRef] [PubMed]
- Schneider, M.; Evans, R.; Haas, M.; Leach, M.J.; Hawk, C.; Long, C.R.; Cramer, G.D.; Walters, O.; Vihstadt, C.; Terhorst, L. US chiropractors’ attitudes, skills and use of evidence-based practice: A cross-sectional national survey. Chiropr. Man. Ther. 2015, 23, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Leach, M.J.; Gillham, D. Evaluation of the Evidence-Based practice Attitude and utilization SurvEy for complementary and alternative medicine practitioners. J. Eval. Clin. Pract. 2008, 14, 792–798. [Google Scholar] [CrossRef]
- Veziari, Y.; Kumar, S.; Leach, M.J. The development of a survey instrument to measure the barriers to the conduct and application of research in complementary and alternative medicine: A Delphi study. BMC Complement. Altern. Med. 2018, 18, 335. [Google Scholar] [CrossRef]
- Buchanan, H.; Siegfried, N.; Jelsma, J. Survey Instruments for Knowledge, Skills, Attitudes and Behaviour Related to Evidence-based Practice in Occupational Therapy: A Systematic Review. Occup. Ther. Int. 2016, 23, 59–90. [Google Scholar] [CrossRef]
- Fernández-Domínguez, J.C.; De Pedro-Gómez, J.E.; Morales-Asencio, J.M.; Bennasar-Veny, M.; Sastre-Fullana, P.; Sesé-Abad, A. Health Sciences-Evidence Based Practice questionnaire (HS-EBP) for measuring transprofessional evidence-based practice: Creation, development and psychometric validation. PLoS ONE 2017, 12, e0177172. [Google Scholar] [CrossRef]
- Fernández-Domínguez, J.C.; Sesé-Abad, A.; Morales-Asencio, J.M.; Sastre-Fullana, P.; Pol-Castañeda, S.; De Pedro-Gómez, J.E. Content validity of a health science evidence-based practice questionnaire (HS-EBP) with a web-based modified Delphi approach. Int. J. Qual. Health Care 2016, 28, 764–773. [Google Scholar] [CrossRef]
- Velez, R.R.; Del Valle, U.; Correa-Rodríguez, M.; Rodríguez, D.I.M.; Ramirez, L.; Ruiz, K.G.; Sánchez, M.A.D.; Duran-Palomino, D.; Girabent-Farrés, M.; Flórez-López, M.E.; et al. Evidence-based practice: Beliefs, attitudes, knowledge, and skills among Colombian physical therapists. Colomb. Med. 2015, 46, 33–40. [Google Scholar] [CrossRef]
- AlShehri, M.A.; Alalawi, A.; Alhasan, H.; Stokes, E. Physiotherapists’ behaviour, attitudes, awareness, knowledge and barriers in relation to evidence-based practice implementation in Saudi Arabia. Int. J. Evid.-Based Health 2017, 15, 127–141. [Google Scholar] [CrossRef]
- Lindström, A.-C.; Bernhardsson, S. Evidence-Based Practice in Primary Care Occupational Therapy: A Cross-Sectional Survey in Sweden. Occup. Ther. Int. 2018, 2018, 1–9. [Google Scholar] [CrossRef] [PubMed]
- French, B.; Thomas, L.H.; Baker, P.; Burton, C.R.; Pennington, L.; Roddam, H. What can management theories offer evidence-based practice? A comparative analysis of measurement tools for organisational context. Implement. Sci. 2009, 4, 28. [Google Scholar] [CrossRef] [PubMed]
- Tresoldi, M.; Ambrogi, F.; Favero, E.; Colombo, A.; Barillari, M.R.; Velardi, P.; Schindler, A. Reliability, validity and normative data of a quick repetition test for Italian children. Int. J. Pediatr. Otorhinolaryngol. 2015, 79, 888–894. [Google Scholar] [CrossRef] [PubMed]
- LaGuardia, J.; Campos, M.R.; Travassos, C.; Najar, A.L.; Dos Anjos, L.A.; Vasconcellos, M.M. Brazilian normative data for the Short Form 36 questionnaire, version 2. Rev. Bras. Epidemiol. 2013, 16, 889–897. [Google Scholar] [CrossRef]
- Nordin, M.; Nordin, S. Psychometric evaluation and normative data of the Swedish version of the 10-item perceived stress scale. Scand. J. Psychol. 2013, 54, 502–507. [Google Scholar] [CrossRef]
- Li, F.; Bai, X.; Wang, Y. The Scale of Positive and Negative Experience (SPANE): Psychometric Properties and Normative Data in a Large Chinese Sample. PLoS ONE 2013, 8, e61137. [Google Scholar] [CrossRef]
- Upton, D.; Upton, P.; Scurlock-Evans, L. The Reach, Transferability, and Impact of the Evidence-Based Practice Questionnaire: A Methodological and Narrative Literature Review. Worldviews Evid. Based Nurs. 2014, 11, 46–54. [Google Scholar] [CrossRef]
- Kajermo, K.N.; Bostrom, A.; Thompson, D.S.; Hutchinson, A.M.; Estabrooks, C.A.; Wallin, L. The BARRIERS scale -- the barriers to research utilization scale: A systematic review. Implement. Sci. 2010, 5, 32. [Google Scholar] [CrossRef]
- Gea-Caballero, V.; Juárez-Vela, R.; Díaz-Herrera, M.Á.; Mármol-López, M.I.; Blazquez, R.A.; Martínez-Riera, J.R. Development of a short questionnaire based on the Practice Environment Scale-Nursing Work Index in primary health care. PeerJ. 2019, 7, e7369. [Google Scholar] [CrossRef]
- Kaper, N.M.; Swennen, M.H.; Van Wijk, A.J.; Kalkman, C.J.; Van Rheenen, N.; Van Der Graaf, Y.; Van Der Heijden, G.J. The evidence-based practice inventory: Reliability and validity was demonstrated for a novel instrument to identify barriers and facilitators for Evidence Based Practice in health care. J. Clin. Epidemiol. 2015, 68, 1261–1269. [Google Scholar] [CrossRef]
- Salbach, N.M.; Jaglal, S.B.; Williams, J.I. Reliability and Validity of the Evidence-Based Practice Confidence (EPIC) Scale. J. Contin. Educ. Health Prof. 2013, 33, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Heiwe, S.; Kajermo, K.N.; Tyni-Lenné, R.; Guidetti, S.; Samuelsson, M.; Andersson, I.-L.; Wengström, Y. Evidence-based practice: Attitudes, knowledge and behaviour among allied health care professionals. Int. J. Qual. Health Care 2011, 23, 198–209. [Google Scholar] [CrossRef] [PubMed]
- McEvoy, M.P.; Williams, M.T.; Olds, T.S. Development and psychometric testing of a trans-professional evidence-based practice profile questionnaire. Med. Teach. 2010, 32, e373–e380. [Google Scholar] [CrossRef] [PubMed]
- Bustins, G.A.; Roura, S.; Cerritelli, F.; Esteves, J.E.; Verbeeck, J.; Van Dun, P.L.S. The Spanish Osteopathic Practitioners Estimates and RAtes (OPERA) study: A cross-sectional survey. PLoS ONE 2020, 15, e0234713. [Google Scholar] [CrossRef]
- Streiner, D.L.; Norman, G.; Cairney, J. Health measurement scales: A practical guide to their development and use (5th edition). Aust. N. Z. J. Public Health 2016, 40, 294–295. [Google Scholar] [CrossRef]
- IBM Corp. Released. IBM SPSS Statistics for Windows, Version 23.0; IBM Corp.: Armonk, NY, USA, 2015. [Google Scholar]
- Magdziarczyk, M. Right to Be Forgotten in Light of Regulation (Eu) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the Protection of Natural Persons with Regard to the Processing of Personal Data and on the Free Movement of Such Data, and Repealing Directive 95/46/Ec. In Proceedings of the 6th SGEM International Multidisciplinary Scientific Conferences on Social Sciences and Arts Proceedings, Modern Science, Vienna, Austria, 11–14 April 2019. [Google Scholar]
- Vaucher, P.; Macdonald, R.J.D.; Carnes, D. The role of osteopathy in the Swiss primary health care system: A practice review. BMJ Open 2018, 8, e023770. [Google Scholar] [CrossRef]
- Van Dun, P.L.S.; Nicolaie, M.A.; Van Messem, A. State of affairs of osteopathy in the Benelux: Benelux Osteosurvey 2013. Int. J. Osteopath. Med. 2016, 20, 3–17. [Google Scholar] [CrossRef]
- Fordyce, M.; Doescher, M.P.; Chen, F.M.; Hart, L.G. Osteopathic physicians and international medical graduates in the rural primary care physician workforce. Fam. Med. 2012, 44, 396–403. [Google Scholar]
- Dorfsman, M.L.; Hart, D.E.; Wolfson, A.B. Implementation of a Novel Conference Series on Clinical Practice Variations Provides an Opportunity for Constructive Discussion of Faculty Practice Patterns: Do as We Say? … or Do as We Do? AEM Educ. Train. 2017, 2, 15–19. [Google Scholar] [CrossRef]
- De la Cámara Gómez, A. Scientific evidence based medicine: Myth and reality of variability in clinical practice and its impact on health outcomes. An. Sist. Sanit. Navar. 2003, 26, 11–26. [Google Scholar]
- Waltz, T.J.; Powell, B.J.; Matthieu, M.M.; Damschroder, L.J.; Chinman, M.; Smith, J.L.; Proctor, E.; Kirchner, J.E. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: Results from the Expert Recommendations for Implementing Change (ERIC) study. Implement. Sci. 2015, 10, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Jette, D.U.; Bacon, K.; Batty, C.; Carlson, M.; Ferland, A.; Hemingway, R.D.; Hill, J.C.; Ogilvie, L.; Volk, D. Evidence-Based Practice: Beliefs, Attitudes, Knowledge, and Behaviors of Physical Therapists. Phys. Ther. 2003, 83, 786–805. [Google Scholar] [CrossRef] [PubMed]
| Variables | Statistics |
|---|---|
| Age | M = 33.95 SD = 7.10 |
| Sex | |
| Male | 200 (45.10%) |
| Female | 243 (54.90%) |
| Years of professional activity Type of work | M = 7.39 SD = 5.33 |
| Own practice | 281 (69.70%) |
| Specialised care | 62 (15.40%) |
| Social centres | 33 (8.20%) |
| Primary/home care | 17 (4.20%) |
| University academic staff | 8 (2.00%) |
| School system | 2 (0.50%) |
| Context | |
| Private | 369 (84.60%) |
| Public | 40 (9.20%) |
| Urban environment | |
| ≥50,000 inhabitants | 249 (56.70%) |
| <50,000 inhabitants | 138 (31.40%) |
| Rural | 52 (11.80%) |
| Academic degree | |
| PhD | 40 (9.00%) |
| Master | 218 (49.20%) |
| Other | 185 (41.80%) |
| EBP Training | |
| Yes | 216 (48.80%) |
| Basic | 59 (27.30%) |
| Intermediate | 89 (41.20%) |
| Advanced | 68 (31.50%) |
| No | 227 (51.20%) |
| Beliefs and Attitudes (D1) | Results from Scientific Research (D2) | Development of Professional Practice (D3) | Assessment of Results (D4) | Barriers/Facilitators (D5) | |
|---|---|---|---|---|---|
| Median (P50) | 95.00 | 86.00 | 78.00 | 84.00 | 62.00 |
| P25–P75 | 83.00–105.00 | 62.00–107.00 | 69.00–85.00 | 69.00–97.00 | 41.00–82.00 |
| Range | 12.00–120.00 | 14.00–140.00 | 10.00–100.00 | 12.00–120.00 | 12.00–120.00 |
| Asim. (EE) CI 95% | −0.71 (0.08) [−0.87; −0.55] | −0.19 (0.08) [−0.35; −0.03] | −0.70 (0.08) [−0.86; −0.54] | −0.49 (0.08) [−0.65; −0.33] | 0.10 (0.08) [−0.06; 0.26] |
| Kurtosis (EE) CI 95% | 0.68 (0.16) [0.36; 1.00] | −0.75 (0.16) [−1.07; −0.43] | 1.11 (0.16) [0.79; 1.43] | −0.16 (0.16) [−0.48; 0.16] | −0.92 (0.16) [−1.24; −0.60] |
| K-S test | p = 0.001 | p = 0.043 | p < 0.001 | p < 0.001 | p < 0.001 |
| Percentiles | D1 | D2 | D3 | D4 | D5 |
|---|---|---|---|---|---|
| 1 | 39.44 | 21.40 | 36.76 | 27.00 | 15.00 |
| 5 | 63.20 | 34.40 | 56.00 | 46.00 | 25.00 |
| 10 | 70.40 | 44.00 | 60.40 | 53.40 | 30.00 |
| 15 | 76.00 | 51.00 | 63.00 | 60.00 | 34.00 |
| 20 | 79.00 | 56.00 | 67.00 | 65.00 | 37.80 |
| 25 | 83.00 | 62.00 | 69.00 | 69.00 | 41.00 |
| 30 | 86.00 | 68.00 | 72.00 | 73.00 | 45.00 |
| 35 | 88.00 | 73.40 | 73.00 | 75.00 | 49.00 |
| 40 | 91.00 | 79.00 | 75.00 | 78.00 | 54.60 |
| 45 | 92.80 | 83.00 | 76.00 | 82.00 | 58.00 |
| 50 | 95.00 | 86.00 | 78.00 | 84.00 | 62.00 |
| 55 | 97.00 | 90.00 | 79.00 | 87.00 | 66.00 |
| 60 | 99.00 | 94.00 | 80.00 | 90.00 | 70.40 |
| 65 | 102.00 | 97.60 | 82.00 | 92.00 | 74.60 |
| 70 | 103.00 | 103.00 | 83.00 | 94.00 | 79.00 |
| 75 | 105.00 | 107.00 | 85.00 | 97.00 | 82.00 |
| 80 | 108.00 | 111.20 | 87.00 | 100.00 | 86.00 |
| 85 | 111.00 | 115.40 | 89.00 | 102.00 | 91.00 |
| 90 | 114.60 | 122.00 | 91.00 | 107.60 | 97.00 |
| 95 | 120.00 | 131.00 | 94.80 | 113.00 | 105.00 |
| 99 | 120.00 | 139.56 | 100.00 | 120.00 | 115.00 |
| Beliefs and Attitudes (D1) Range: 12–120 | Results from Scientific Research (D2) Range: 14–140 | Professional Practice Development (D3) Range: 10–100 | Assessment of Results (D4) Range: 12–120 | Barriers/Facilitators (D5) Range: 12–120 | ||
|---|---|---|---|---|---|---|
| CLUSTER 1 | Mean | 59.65 | 56.75 | 62.66 | 60.56 | 35.16 |
| SD * | 13.88 | 17.55 | 13.08 | 16.45 | 11.80 | |
| N | 32 | 32 | 32 | 32 | 32 | |
| CLUSTER 2 | Mean | 92.82 | 52.02 | 64.91 | 52.75 | 36.72 |
| SD * | 10.26 | 16.57 | 11.57 | 13.82 | 15.03 | |
| N | 57 | 57 | 57 | 57 | 57 | |
| CLUSTER 3 | Mean | 88.35 | 48.67 | 74.58 | 86.82 | 46.13 |
| SD * | 13.40 | 13.51 | 9.95 | 12.12 | 14.97 | |
| N | 55 | 55 | 55 | 55 | 55 | |
| CLUSTER 4 | Mean | 88.57 | 85.34 | 73.87 | 79.23 | 72.82 |
| SD * | 13.77 | 12.92 | 8.82 | 13.51 | 11.20 | |
| N | 110 | 110 | 110 | 110 | 110 | |
| CLUSTER 5 | Mean | 98.61 | 95.25 | 80.85 | 85.80 | 48.24 |
| SD * | 13.65 | 13.39 | 8.33 | 12.80 | 12.48 | |
| N | 80 | 80 | 80 | 80 | 80 | |
| CLUSTER 6 | Mean | 106.34 | 118.58 | 86.95 | 101.53 | 92.66 |
| SD * | 10.02 | 11.85 | 7.50 | 11.96 | 13.22 | |
| N | 109 | 109 | 109 | 109 | 109 | |
| TOTAL | Mean | 93.18 | 84.40 | 76.47 | 82.09 | 62.58 |
| SD * | 17.07 | 29.07 | 12.25 | 20.38 | 25.06 | |
| N | 443 | 443 | 443 | 443 | 443 |
| Clusters (Profiles) | |||||||
| Cluster 1 (Low) Mean (SD) | Cluster 2 Mean (SD) | Cluster 3 Mean (SD) | Cluster 4 Mean (SD) | Cluster 5 Mean (SD) | Cluster 6 (High) Mean (SD) | ||
| Work time invested in different types of professional activity (daily) | % healthcare | 76.88 a (23.28) | 75.07 b (25.23) | 79.43 c (16.73) | 71.38 d (20.03) | 73.83 e (18.23) | 58.47 abcde (22.15) |
| % research | 6.69 a (14.78) | 3.28 b (6.34) | 1.72 c (3.29) | 5.66 d (7.45) | 4.86 e (6.40) | 11.66 abcde (8.60) | |
| % teaching | 7.47 a (12.67) | 9.63 b (21.23) | 5.49 c (10.24) | 12.81 (14.81) | 10.58 d (13.89) | 17.58 abcd (15.23) | |
| Years of professional practice | 7.62 (6.67) | 5.36 a (3.96) | 5.58 b (4.66) | 7.25 c (4.66) | 6.78 d (5.17) | 9.91 abcd (5.71) | |
| Weekly Working hours | 24.71 (12.24) | 19.41 ac (13.40) | 25.00 (13.93) | 29.33 ab (13.03) | 23.54 bd (14.44) | 29.93 cd (12.67) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fernández-Domínguez, J.C.; Escobio-Prieto, I.; Sesé-Abad, A.; Jiménez-López, R.; Romero-Franco, N.; Oliva-Pascual-Vaca, Á. Health Sciences—Evidence Based Practice Questionnaire (HS-EBP): Normative Data and Differential Profiles in Spanish Osteopathic Professionals. Int. J. Environ. Res. Public Health 2020, 17, 8454. https://doi.org/10.3390/ijerph17228454
Fernández-Domínguez JC, Escobio-Prieto I, Sesé-Abad A, Jiménez-López R, Romero-Franco N, Oliva-Pascual-Vaca Á. Health Sciences—Evidence Based Practice Questionnaire (HS-EBP): Normative Data and Differential Profiles in Spanish Osteopathic Professionals. International Journal of Environmental Research and Public Health. 2020; 17(22):8454. https://doi.org/10.3390/ijerph17228454
Chicago/Turabian StyleFernández-Domínguez, Juan Carlos, Isabel Escobio-Prieto, Albert Sesé-Abad, Rafael Jiménez-López, Natalia Romero-Franco, and Ángel Oliva-Pascual-Vaca. 2020. "Health Sciences—Evidence Based Practice Questionnaire (HS-EBP): Normative Data and Differential Profiles in Spanish Osteopathic Professionals" International Journal of Environmental Research and Public Health 17, no. 22: 8454. https://doi.org/10.3390/ijerph17228454
APA StyleFernández-Domínguez, J. C., Escobio-Prieto, I., Sesé-Abad, A., Jiménez-López, R., Romero-Franco, N., & Oliva-Pascual-Vaca, Á. (2020). Health Sciences—Evidence Based Practice Questionnaire (HS-EBP): Normative Data and Differential Profiles in Spanish Osteopathic Professionals. International Journal of Environmental Research and Public Health, 17(22), 8454. https://doi.org/10.3390/ijerph17228454







